Hip Dislocation: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (29 intermediate revisions by 5 users not shown) | |||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
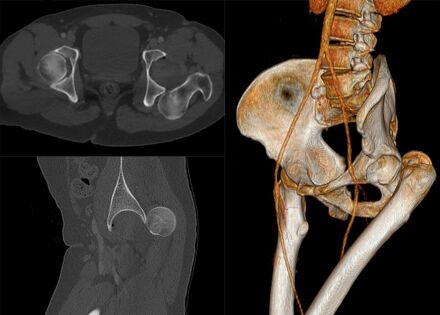
Hip dislocations are relatively rare, | [[File:Traumatic posterior hip dislocation.jpeg|thumb|440x440px|Traumatic posterior hip dislocation]] | ||
[[Hip]] dislocations are relatively rare, are be congenital or acquired and account for ~5% of all joint dislocations The native hip joint (as opposed to prosthetic hip) is inherently stable and needs a huge amount of force to cause dislocation, such as in a motor vehicle accidents.<ref name=":6">Masiewicz S, Mabrouk A, Johnson DE. [https://www.ncbi.nlm.nih.gov/books/NBK459319/ Posterior hip dislocation].Available:https://www.ncbi.nlm.nih.gov/books/NBK459319/ (accessed 7.1.2023)</ref> | |||
Hip dislocation can be classified as: | |||
# Posterior dislocation (most common ~85%). Caused by combined forces of: hip flexion, adduction, and internal rotation. | |||
# Anterior dislocation (~10%). Caused by combined forces of : hyper-abduction with the extension.<ref name=":6" /> | |||
# Central dislocation (always occurring with [[Acetabulum Fracture]])<ref name=":5">Radiopedia [https://radiopaedia.org/articles/hip-dislocation Hip dislocation] Available:https://radiopaedia.org/articles/hip-dislocation (accessed 7.1.2023)</ref> | |||
Below is a good 5 minute video on hip dislocations. | |||
{| border="0" cellspacing="1" cellpadding="1" | {| border="0" cellspacing="1" cellpadding="1" | ||
|- | |- | ||
|{{#ev:youtube|watch?v= | |{{#ev:youtube|watch?v=BLZXlVnqLs0}} | ||
|} | |||
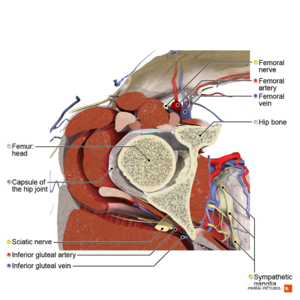
== Clinical relevant anatomy == | |||
[[File:Axial section of the hip joint Primal.png|thumb|Hip ]] | |||
The hip joint, functioning as a ball-and-socket structure, maintains inherent stability due to its well-defined bony geometry and robust ligaments. This structural resilience enables the hip to withstand substantial mechanical stress. The stability of the [[hip]] is contributed to by various anatomical components, including the depth of the acetabulum, the labrum, the joint capsule, muscular support, and surrounding ligaments. Key ligaments, such as the [[iliofemoral ligament]] located anteriorly and the [[Ischiofemoral Ligament|ischiofemoral ligament]] positioned posteriorly, play a pivotal role in stabilizing the joint against directional forces. Notably, the greater strength of the anterior ligaments often results in traumatic hip incidents presenting as posterior dislocations upon discovery, observed in approximately 90% of cases.Dynamic support is provided by muscles such as the [[Rectus Femoris]], [[Gluteal Muscles|gluteal muscles]], and short external rotators. An understanding of the hip's vasculature is crucial, as trauma to the hip can displace the femoral head and disrupt blood supply, potentially leading to avascular necrosis (AVN). Branches originating from the external iliac artery form a ring around the femoral neck, with the Lateral femoral circumflex artery extending anteriorly and the medial femoral circumflex artery extending posteriorly. The primary blood supply to the femoral head is predominantly through the medial femoral circumflex artery | |||
== Etiology == | |||
# '''Acquired Dislocation''': [[File:Dislocated hip replacement.jpeg|thumb|Dislocated hip replacement]] Motor vehicle collisions accounting for >50% of dislocations.<ref name=":5" /> Another common mechanism is falling from a height. Hip dislocations are thus rarely isolated, and often goes together with other injuries or fractures. With hip dislocations, the soft tissue around the hip, such as the muscles, ligaments and labrum are also damaged. Neural injuries may also be present. Fractures to the acetabulum and femur head is most commonly associated with traumatic hip dislocations. | |||
# [[Total Hip Replacement|Total hip replacement]] (THR) dislocation is a complication of THR usually occurring due to patient noncomplicance with [[Hip Precautions|post-operative precautions]], implant malposition, or soft-tissue deficiency. This type of dislocation normally caused by less trauma, usually falls or turning, moving into the contra-indicated positions, and putting stress on the capsule that was cut to do the replacement surgery..<ref>Orthobullets [https://www.orthobullets.com/recon/5012/tha-dislocation THA Dislocation] Available:https://www.orthobullets.com/recon/5012/tha-dislocation (accessed 7.1.2022)</ref><ref name=":5" /> For more on [[Total Hip Replacement Dislocation|THR dislocation]] see link. | |||
# '''Congenital Hip Dislocation''' have been appraised and are now viewed as part of the spectrum of [[Developmental dysplasia of the hip (DDH)|developmental dysplasia of the hip.]] See link for information on this. | |||
This page is now focused on traumatic hip dislocation | |||
== Mechanism and Classification == | |||
=== '''Mechanisms of dislocation''' === | |||
The primary mechanism involved in Traumatic Hip Dislocation is axial loading<ref>S. Sanders, N. Tejwani, and K. A. Egol, “Traumatic hip dislocation—a review,” ''Bulletin of the NYU Hospital for Joint Diseases'', vol. 68, no. 2, pp. 91–96, 2010.</ref>. The direction of the dislocation is contingent upon the position of the hip during impact and the force vector's applied direction. Specifically, when the leg is straight or the hip and knee are flexed less than 90 degrees with the hip adducted, a common outcome is posterior dislocation of the hip accompanied by a fracture of the posterior acetabular wall<ref name=":0">Obakponovwe, O., Morell, D., Ahmad, M., Nunn, T., & Giannoudis, P. V. (2011).Traumatic hip dislocation. Orthopaedics and Trauma, 25(3), 214-222.</ref>. | |||
In contrast, when the hip is abducted and externally rotated, an anterior dislocation tends to occur. This occurs when the medial aspect of the knee is impacted by external forces, such as those exerted by the steering wheel, dashboard, or front seat. | |||
'''Types of Traumatic Hip Dislocation''' | |||
Traumatic dislocations of the hip are categorically grouped into three main types: posterior, anterior, and central dislocations. This classification system is founded on the orientation and positioning of the femoral head relative to the acetabulum<ref>S. Sanders, N. Tejwani, and K. A. Egol, “Traumatic hip dislocation—a review,” ''Bulletin of the NYU Hospital for Joint Diseases'', vol. 68, no. 2, pp. 91–96, 2010.</ref>. Additionally, to provide further detail within the posterior and anterior dislocation categories, a classification system developed by Thompson and Epstein in 1951 is commonly employed for sub-classification. | |||
'''Posterior Traumatic Hip Dislocations''' constitute a significant majority, accounting for approximately 85% to 90% of all THD cases<ref>S. Sanders, N. Tejwani, and K. A. Egol, “Traumatic hip dislocation—a review,” ''Bulletin of the NYU Hospital for Joint Diseases'', vol. 68, no. 2, pp. 91–96, 2010.</ref>. Posterior dislocation, also known as dashboard injury, occurs as a result of trauma to a flexed knee, typically with the hip in varying degrees of flexion. In this scenario, the femur is thrust upwards, causing the femoral head to be forced out of its socket. This type of injury often occurs when an individual seated in a car trunk or seat during a road accident is thrown forward, leading to the knee striking against the dashboard.Within this category, further sub-classification is achieved through the Thompson-Epstein classification system, which categorizes these dislocations into five types based on the severity of associated acetabular fractures and the presence of a femoral head fracture<ref>Obakponovwe, O., Morell, D., Ahmad, M., Nunn, T., & Giannoudis, P. V. (2011).Traumatic hip dislocation. Orthopaedics and Trauma, 25(3), 214-222.</ref>. | |||
Thompson-Epstein Classification of Posterior THD<ref name=":0" /> | |||
Type I : Simple dislocation with or without an insignificant posterior wall fragment | |||
Type II Dislocation associated with a single large posterior wall fragment | |||
Type III Dislocation with a comminuted posterior wall fragment | |||
Type IV Dislocation with fracture of the acetabular floor | |||
Type V Dislocation with fracture of the femoral head | |||
'''Anterior Traumatic Hip Dislocations''' are considerably less frequent, making up around 10% of all THD cases<ref>Yang, & Cornwall, R. (2000). Initial treatment of traumatic hip dislocations in the | |||
adult. Clinical orthopaedics and related research (377), 24-31</ref>. Anterior dislocation occurs when a hyperextension force is applied against an abducted leg, causing the femoral head to be levered out of the acetabulum<ref>Pallia CS, Scott RE, Chao DJ. Traumatic hip dislocation in athletes. Curr Sports Med Rep. 2002 Dec;1(6):338-45</ref>. In instances such as road traffic accidents (RTAs), where the knee strikes the dashboard with the thigh abducted, or in cases of a violent fall from a height, or a forceful blow to the back of a patient in a squatted position, the femoral head dislocates anteriorly to the acetabulum.This subgroup is further divided into two types using the Epstein classification system<ref name=":0" />. The classification details are provided below: | |||
Epstein Classification of Anterior THD<ref name=":0" /> | |||
Type I: Superior dislocations, including pubic and subspinous. | |||
IA : No associated fractures | |||
IB: Associated fracture or impaction of the femoral head | |||
IC: Associated fracture of the acetabulum | |||
Type I: Superior dislocations, including pubic and subspinous. | |||
IA : No associated fractures | |||
IB: Associated fracture or impaction of the femoral head | |||
IC: Associated fracture of the acetabulum | |||
Type II : Inferior dislocations, including obturator and perineal | |||
IIA: No associated fractures | |||
IIB :Associated fracture or impaction of the femoral head | |||
IIC: Associated fracture of acetabulum | |||
Type I: Superior dislocations, including pubic and subspinous. | |||
IA : No associated fractures | |||
IB: Associated fracture or impaction of the femoral head | |||
IC: Associated fracture of the acetabulum | |||
Type II : Inferior dislocations, including obturator and perineal | |||
IIA: No associated fractures | |||
IIB :Associated fracture or impaction of the femoral head | |||
IIC: Associated fracture of acetabulum | |||
'''Central Traumatic Hip Dislocations''' are the least common and represents the most challenging among all hip joint dislocations. The mechanism of injury typically involves a direct impact on the greater trochanter, such as in the case of a road traffic accident (RTA) or a fall onto the sides. | |||
== Clinical Presentation == | |||
The patient's history commonly involve a description of a significant "clunk" or "popping" followed instantly by severe [[Pain Assessment|pain]]. A physical deformity with ipsilateral shortening/hip flexion, adduction and internal rotation will be visible. Inability to walk results from of pain and swelling. With the separation of the femur head from the acetabulum, surrounding muscles and tendons can be damaged as well. Subsequent knee injuries might also be present. | |||
== | * Other common features include: [[Leg Length Discrepancy|leg length discrepancy]]: hip immobility with <ref name=":1">Hung NN. [http://chinhhinhnhitw.vn/wp-content/uploads/2018/05/Full-text-5.pdf Traumatic hip dislocation in children.] Journal of Pediatric Orthopaedics B 2012;21(6):542-51.</ref> reduced hip range of motion.<ref name=":6" /><ref name=":1" /> | ||
* [[ | * Signs of possible vascular or [[Sciatic Nerve Injury|sciatic nerve injury:]] Local hematoma. Painful buttock, posterior thigh, and leg. Altered sensation in posterior leg and foot. Weakness or total loss of dorsiflexion (peroneal branch) or plantar flexion (tibial branch). Diminished or absent deep tendon [[reflexes]] at the ankle.<ref name=":6" /><sup></sup> | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
* [[X-Rays|X-rays]]: AP pelvis and lateral | * [[X-Rays|X-rays]]: AP pelvis and lateral<ref>Pallia CS, Scott RE, Chao DJ. Traumatic hip dislocation in athletes. Curr Sports Med Rep. 2002 Dec;1(6):338-45</ref> | ||
** To confirm dislocation and successful relocation | ** To confirm dislocation and successful relocation | ||
** Assess for associated fractures | ** Assess for associated fractures | ||
| Line 82: | Line 118: | ||
== Complications == | == Complications == | ||
== | # Immediate:<ref name=":4">Ortho Info. Developmental Dislocation (Dysplasia) of the Hip (DDH). Available from: https://orthoinfo.aaos.org/en/diseases--conditions/developmental-dislocation-dysplasia-of-the-hip-ddh (accessed 08/08/2020).</ref>Associated soft tissue injuries. Neural injuries, especially to the sciatic nerve in posterior dislocations (present in about 10% of traumatic dislocations). Fractures, mostly to the femur head or acetabulum (mostly posterior wall) | ||
# Long term: [[Avascular necrosis of the femoral head|Avascular necrosis]] (incidence 1.7-40% is reducable to 0-10% if relocation is done within 6 hours post traumatic) dislocation<ref>Bucholz R, Heckman JD. Rockwood e Green fraturas em adultos. In: Rockwood e Green fraturas em adultos, 2006: pp. 2263-2263.</ref>. [[Hip Osteoarthritis|Post-traumatic osteoarthritis]]. Chronic dislocations. [[Leg Length Discrepancy|Leg length discrepancy]]<ref name=":3">Lima LC, Nascimento RA, Almeida VM, Façanha Filho FA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4108698/#:~:text=The%20present%20study%20showed%20that,was%20posterior%20dislocation%20(93.3%25). Epidemiology of traumatic hip dislocation in patients treated in Ceará, Brazil.] Acta ortopedica brasileira 2014;22(3):151-4.</ref>. | |||
== Differential diagnosis == | |||
Hip pain | |||
'''Acute trauma''' | |||
* Femur fracture | |||
** Proximal | |||
*** Intracapsular | |||
**** Femoral head fracture | |||
**** Femoral neck fracture | |||
*** Extracapsular | |||
**** Intertrochanteric femur fracture | |||
**** Trochanteric femur fracture | |||
** Shaft | |||
*** Mid-shaft femur fracture (all subtrochanteric) | |||
* Pelvic fractures | |||
** Acetabular pelvic fractures | |||
** Open book pelvic fracture | |||
** Straddle pelvic fracture | |||
** Pelvic avulsion fracture | |||
'''Chronic/Atraumatic''' | |||
* Hip bursitis | |||
* Psoas abscess | |||
* Piriformis syndrome | |||
* Meralgia paresthetica | |||
* Septic arthritis | |||
** Septic arthritis of the hip (peds) | |||
* Obturator nerve entrapment | |||
* Avascular necrosis of hip | |||
== Outcome measures == | |||
[[Harris Hip Score]](HHS) serves as a specialized outcome assessment tool administered by clinicians to evaluate hip function. Originally devised by William Harris to assess hip function post total hip replacement (THR) surgery<ref name=":7">Nilsdotter, A., & Bremander, A. (2011). Measures of hip function and symptoms: | |||
Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score(HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopaedic Surgeons (AAOS) Hip and Knee Questionnaire. Arthritis Care & Research, 63(S11), 200-207.</ref>, it has since become widely employed for assessing various hip disabilities and treatments in adults, including osteoarthritis (OA)<ref name=":8">Shi, H. Y., Mau, L. W., Chang, J. K., Wang, J. W., & Chiu, H. C. (2009). | |||
Responsiveness of the Harris Hip Score and the SF-36: five years after total hip arthroplasty. Quality of Life Research, 18(8) </ref>. Comprising four domains—pain, physical function (encompassing activities of daily living and walking ability), absence of hip deformity, and range of motion (ROM) of the hip—the score consists of 10 items with a maximum of 100 points. The pain domain comprises 1 item with a scoring range of 0-44 points, the function domain consists of seven items with a range of 0-47 points, absence of deformity has 1 item with 4 points, and ROM has 2 items with 5 points<ref name=":9">Hoeksma, H., Van den Ende, C., Ronday, H., Heering, A., Breedveld, F., & Dekker,J. (2003). Comparison of the responsiveness of the Harris Hip Score with generic measures for hip function in osteoarthritis of the hip. Annals of the Rheumatic Diseases, 62(10), 935-938.</ref>. | |||
The cumulative scores from individual domains yield an overall score categorized descriptively as Excellent, Good, Fair, or Poor function<ref>Garellick, G., Herberts, P., & Malchau, H. (1999). The value of clinical data scoring | |||
systems: are traditional hip scoring systems adequate to use in evaluation after total hip surgery? The Journal of Arthroplasty, 14(8), 1024-1029.</ref>. Higher overall scores indicate better function, with less than 70 suggesting poor function, 70 to 80 indicating fair function, 80 to 90 reflecting good function, and 90 to 100 signifying excellent function. | |||
=== | Given that pain and physical function were the primary indicators for surgery in hip pathologies during the tool's development, these domains carry substantial weight in the scoring<ref name=":7" />. The HHS demonstrates excellent reliability and ease of administration without the need for formal training<ref name=":9" />. The tool demonstrated its responsiveness to be superior to the Short-Form 36 Health Survey for short-term (within 1 year) assessment of hip function<ref name=":8" />. Despite concerns raised regarding high ceiling effects in the systematic review, the tool remains deemed appropriate for studies<ref>Wamper, K. E., Sierevelt, I. N., Poolman, R. W., Bhandari, M., & Haverkamp, D. | ||
(2010). The Harris hip score: Do ceiling effects limit its usefulness in orthopaedics? Acta Orthopaedica, 81(6), 703-707.</ref>, particularly when new treatment trials are not under examination. | |||
== | == Medical Management == | ||
The management of hip dislocations may be operative and non-operative. Many studies note that time to reduction is crucial as the longer the hip is dislocated, the greater the risk of avascular necrosis in the native hip. | |||
==== Non-surgical ==== | ==== Non-surgical ==== | ||
Closed relocation of the hip is done by a traction force performed in the opposite direction of the dislocation, with the hip in 90° flexion. This should preferably be done under general or regional anesthesia and muscle relaxation to prevent greater damage to cartilage and soft tissue.<ref name=":2" /> It may also be done in under anaesthetics in theater.<ref name=":4" /> After the relocation, the stability of the hip should be tested very carefully. A period of bed rest might be recommended depending on the stability of the hip and the extent of the soft tissue injuries. | Closed relocation of the hip is done by a traction force performed in the opposite direction of the dislocation, with the hip in 90° flexion. This should preferably be done under general or regional anesthesia and muscle relaxation to prevent greater damage to cartilage and soft tissue.<ref name=":2">Medscape. Hip dislocation. Available from: https://emedicine.medscape.com/article/86930-overview (accessed 09/08/2020).</ref> It may also be done in under anaesthetics in theater.<ref name=":4" /> After the relocation, the stability of the hip should be tested very carefully. A period of bed rest might be recommended depending on the stability of the hip and the extent of the soft tissue injuries. | ||
==== Surgical ==== | ==== Surgical ==== | ||
| Line 132: | Line 188: | ||
== Physiotherapy Management == | == Physiotherapy Management == | ||
It is important to take the time frames for soft tissue healing (and bone healing in cases with associated fractures) into consideration with rehabilitation following a hip dislocation. The orthopaedic surgeon will | Individuals with hip dislocation will require extensive physical therapy. It is important to take the time frames for soft tissue healing (and bone healing in cases with associated fractures) into consideration with rehabilitation following a hip dislocation. The orthopaedic surgeon will provide guidance on eg weight bearing restrictions that might be present following the medical management of the hip. Complete rehabilitation following hip dislocation can take 3-6 months.<ref name=":4" /> | ||
* Gait re-education: Initially with mobility assistive devices (walking frame/crutches) to limit weight bearing, and progression thereof | * [[Gait]] re-education: Initially with [[Walking Aids|mobility assistive devices]] (walking frame/[[crutches]]) to limit [[weight bearing]], and progression thereof | ||
* Improve hip range of motion | * Improve hip [[Range of Motion|range of motion]] including [[Hip Mobilizations|hip mobilisations]] | ||
* Strengthening of muscles around the hip, with special focus on hip stabilizers | * Strengthening of muscles around the hip, with special focus on hip stabilizers eg [[Hip Abductors|Hip abductors]], [[Hip Adductors|adductors]], [[Hip Extensors|extensors]], [[Hip Flexors|flexors]]. | ||
* Stretching | * [[Stretching]] | ||
* Graded [[Return to Sport|return to activity/sport]] | |||
* Graded return to activity/sport | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Acquired, or traumatic hip dislocations are medical emergencies, and treatment should be sought as soon as possible. Relocation should ideally occur within 6 hours from the dislocation, in order to reduce complications. Traumatic dislocations are reduced either open or closed, and open or arthroscopy surgery might be indicated in cases with associated fractures. Physiotherapy plays an important role in the rehabilitation following a hip dislocation, in order to get the patients back to their previous level of function, and to prevent further dislocations. | |||
== References == | == References == | ||
Latest revision as of 21:03, 9 January 2024
Original Editor - Annelies Noppe
Top Contributors - Annelies Noppe, Leana Louw, Lucinda hampton, Kim Jackson, Lokiru Paul, WikiSysop, Vidya Acharya, Anas Mohamed and Kirenga Bamurange Liliane
Introduction[edit | edit source]
Hip dislocations are relatively rare, are be congenital or acquired and account for ~5% of all joint dislocations The native hip joint (as opposed to prosthetic hip) is inherently stable and needs a huge amount of force to cause dislocation, such as in a motor vehicle accidents.[1]
Hip dislocation can be classified as:
- Posterior dislocation (most common ~85%). Caused by combined forces of: hip flexion, adduction, and internal rotation.
- Anterior dislocation (~10%). Caused by combined forces of : hyper-abduction with the extension.[1]
- Central dislocation (always occurring with Acetabulum Fracture)[2]
Below is a good 5 minute video on hip dislocations.
Clinical relevant anatomy[edit | edit source]
The hip joint, functioning as a ball-and-socket structure, maintains inherent stability due to its well-defined bony geometry and robust ligaments. This structural resilience enables the hip to withstand substantial mechanical stress. The stability of the hip is contributed to by various anatomical components, including the depth of the acetabulum, the labrum, the joint capsule, muscular support, and surrounding ligaments. Key ligaments, such as the iliofemoral ligament located anteriorly and the ischiofemoral ligament positioned posteriorly, play a pivotal role in stabilizing the joint against directional forces. Notably, the greater strength of the anterior ligaments often results in traumatic hip incidents presenting as posterior dislocations upon discovery, observed in approximately 90% of cases.Dynamic support is provided by muscles such as the Rectus Femoris, gluteal muscles, and short external rotators. An understanding of the hip's vasculature is crucial, as trauma to the hip can displace the femoral head and disrupt blood supply, potentially leading to avascular necrosis (AVN). Branches originating from the external iliac artery form a ring around the femoral neck, with the Lateral femoral circumflex artery extending anteriorly and the medial femoral circumflex artery extending posteriorly. The primary blood supply to the femoral head is predominantly through the medial femoral circumflex artery
Etiology[edit | edit source]
- Acquired Dislocation: Motor vehicle collisions accounting for >50% of dislocations.[2] Another common mechanism is falling from a height. Hip dislocations are thus rarely isolated, and often goes together with other injuries or fractures. With hip dislocations, the soft tissue around the hip, such as the muscles, ligaments and labrum are also damaged. Neural injuries may also be present. Fractures to the acetabulum and femur head is most commonly associated with traumatic hip dislocations.
- Total hip replacement (THR) dislocation is a complication of THR usually occurring due to patient noncomplicance with post-operative precautions, implant malposition, or soft-tissue deficiency. This type of dislocation normally caused by less trauma, usually falls or turning, moving into the contra-indicated positions, and putting stress on the capsule that was cut to do the replacement surgery..[3][2] For more on THR dislocation see link.
- Congenital Hip Dislocation have been appraised and are now viewed as part of the spectrum of developmental dysplasia of the hip. See link for information on this.
This page is now focused on traumatic hip dislocation
Mechanism and Classification[edit | edit source]
Mechanisms of dislocation[edit | edit source]
The primary mechanism involved in Traumatic Hip Dislocation is axial loading[4]. The direction of the dislocation is contingent upon the position of the hip during impact and the force vector's applied direction. Specifically, when the leg is straight or the hip and knee are flexed less than 90 degrees with the hip adducted, a common outcome is posterior dislocation of the hip accompanied by a fracture of the posterior acetabular wall[5].
In contrast, when the hip is abducted and externally rotated, an anterior dislocation tends to occur. This occurs when the medial aspect of the knee is impacted by external forces, such as those exerted by the steering wheel, dashboard, or front seat.
Types of Traumatic Hip Dislocation
Traumatic dislocations of the hip are categorically grouped into three main types: posterior, anterior, and central dislocations. This classification system is founded on the orientation and positioning of the femoral head relative to the acetabulum[6]. Additionally, to provide further detail within the posterior and anterior dislocation categories, a classification system developed by Thompson and Epstein in 1951 is commonly employed for sub-classification.
Posterior Traumatic Hip Dislocations constitute a significant majority, accounting for approximately 85% to 90% of all THD cases[7]. Posterior dislocation, also known as dashboard injury, occurs as a result of trauma to a flexed knee, typically with the hip in varying degrees of flexion. In this scenario, the femur is thrust upwards, causing the femoral head to be forced out of its socket. This type of injury often occurs when an individual seated in a car trunk or seat during a road accident is thrown forward, leading to the knee striking against the dashboard.Within this category, further sub-classification is achieved through the Thompson-Epstein classification system, which categorizes these dislocations into five types based on the severity of associated acetabular fractures and the presence of a femoral head fracture[8].
Thompson-Epstein Classification of Posterior THD[5]
Type I : Simple dislocation with or without an insignificant posterior wall fragment
Type II Dislocation associated with a single large posterior wall fragment
Type III Dislocation with a comminuted posterior wall fragment
Type IV Dislocation with fracture of the acetabular floor
Type V Dislocation with fracture of the femoral head
Anterior Traumatic Hip Dislocations are considerably less frequent, making up around 10% of all THD cases[9]. Anterior dislocation occurs when a hyperextension force is applied against an abducted leg, causing the femoral head to be levered out of the acetabulum[10]. In instances such as road traffic accidents (RTAs), where the knee strikes the dashboard with the thigh abducted, or in cases of a violent fall from a height, or a forceful blow to the back of a patient in a squatted position, the femoral head dislocates anteriorly to the acetabulum.This subgroup is further divided into two types using the Epstein classification system[5]. The classification details are provided below:
Epstein Classification of Anterior THD[5]
Type I: Superior dislocations, including pubic and subspinous.
IA : No associated fractures
IB: Associated fracture or impaction of the femoral head
IC: Associated fracture of the acetabulum
Type I: Superior dislocations, including pubic and subspinous.
IA : No associated fractures
IB: Associated fracture or impaction of the femoral head
IC: Associated fracture of the acetabulum
Type II : Inferior dislocations, including obturator and perineal
IIA: No associated fractures
IIB :Associated fracture or impaction of the femoral head
IIC: Associated fracture of acetabulum
Type I: Superior dislocations, including pubic and subspinous.
IA : No associated fractures
IB: Associated fracture or impaction of the femoral head
IC: Associated fracture of the acetabulum
Type II : Inferior dislocations, including obturator and perineal
IIA: No associated fractures
IIB :Associated fracture or impaction of the femoral head
IIC: Associated fracture of acetabulum
Central Traumatic Hip Dislocations are the least common and represents the most challenging among all hip joint dislocations. The mechanism of injury typically involves a direct impact on the greater trochanter, such as in the case of a road traffic accident (RTA) or a fall onto the sides.
Clinical Presentation[edit | edit source]
The patient's history commonly involve a description of a significant "clunk" or "popping" followed instantly by severe pain. A physical deformity with ipsilateral shortening/hip flexion, adduction and internal rotation will be visible. Inability to walk results from of pain and swelling. With the separation of the femur head from the acetabulum, surrounding muscles and tendons can be damaged as well. Subsequent knee injuries might also be present.
- Other common features include: leg length discrepancy: hip immobility with [11] reduced hip range of motion.[1][11]
- Signs of possible vascular or sciatic nerve injury: Local hematoma. Painful buttock, posterior thigh, and leg. Altered sensation in posterior leg and foot. Weakness or total loss of dorsiflexion (peroneal branch) or plantar flexion (tibial branch). Diminished or absent deep tendon reflexes at the ankle.[1]
Diagnostic Procedures[edit | edit source]
- X-rays: AP pelvis and lateral[12]
- To confirm dislocation and successful relocation
- Assess for associated fractures
- Progression of hip dysplasia
- CT:
- To rule out concomitant injuries in traumatic dislocations (e.g. acetabulum or femur head fractures)
- Clearance of lumbar spine[13]
Complications[edit | edit source]
- Immediate:[14]Associated soft tissue injuries. Neural injuries, especially to the sciatic nerve in posterior dislocations (present in about 10% of traumatic dislocations). Fractures, mostly to the femur head or acetabulum (mostly posterior wall)
- Long term: Avascular necrosis (incidence 1.7-40% is reducable to 0-10% if relocation is done within 6 hours post traumatic) dislocation[15]. Post-traumatic osteoarthritis. Chronic dislocations. Leg length discrepancy[16].
Differential diagnosis[edit | edit source]
Hip pain
Acute trauma
- Femur fracture
- Proximal
- Intracapsular
- Femoral head fracture
- Femoral neck fracture
- Extracapsular
- Intertrochanteric femur fracture
- Trochanteric femur fracture
- Intracapsular
- Shaft
- Mid-shaft femur fracture (all subtrochanteric)
- Proximal
- Pelvic fractures
- Acetabular pelvic fractures
- Open book pelvic fracture
- Straddle pelvic fracture
- Pelvic avulsion fracture
Chronic/Atraumatic
- Hip bursitis
- Psoas abscess
- Piriformis syndrome
- Meralgia paresthetica
- Septic arthritis
- Septic arthritis of the hip (peds)
- Obturator nerve entrapment
- Avascular necrosis of hip
Outcome measures[edit | edit source]
Harris Hip Score(HHS) serves as a specialized outcome assessment tool administered by clinicians to evaluate hip function. Originally devised by William Harris to assess hip function post total hip replacement (THR) surgery[17], it has since become widely employed for assessing various hip disabilities and treatments in adults, including osteoarthritis (OA)[18]. Comprising four domains—pain, physical function (encompassing activities of daily living and walking ability), absence of hip deformity, and range of motion (ROM) of the hip—the score consists of 10 items with a maximum of 100 points. The pain domain comprises 1 item with a scoring range of 0-44 points, the function domain consists of seven items with a range of 0-47 points, absence of deformity has 1 item with 4 points, and ROM has 2 items with 5 points[19].
The cumulative scores from individual domains yield an overall score categorized descriptively as Excellent, Good, Fair, or Poor function[20]. Higher overall scores indicate better function, with less than 70 suggesting poor function, 70 to 80 indicating fair function, 80 to 90 reflecting good function, and 90 to 100 signifying excellent function.
Given that pain and physical function were the primary indicators for surgery in hip pathologies during the tool's development, these domains carry substantial weight in the scoring[17]. The HHS demonstrates excellent reliability and ease of administration without the need for formal training[19]. The tool demonstrated its responsiveness to be superior to the Short-Form 36 Health Survey for short-term (within 1 year) assessment of hip function[18]. Despite concerns raised regarding high ceiling effects in the systematic review, the tool remains deemed appropriate for studies[21], particularly when new treatment trials are not under examination.
Medical Management[edit | edit source]
The management of hip dislocations may be operative and non-operative. Many studies note that time to reduction is crucial as the longer the hip is dislocated, the greater the risk of avascular necrosis in the native hip.
Non-surgical[edit | edit source]
Closed relocation of the hip is done by a traction force performed in the opposite direction of the dislocation, with the hip in 90° flexion. This should preferably be done under general or regional anesthesia and muscle relaxation to prevent greater damage to cartilage and soft tissue.[22] It may also be done in under anaesthetics in theater.[14] After the relocation, the stability of the hip should be tested very carefully. A period of bed rest might be recommended depending on the stability of the hip and the extent of the soft tissue injuries.
Surgical[edit | edit source]
Indications:
- Failed conservative relocation
- Instability following conservative relocation
- Associated fractures of the femur head or acetabulum
- Loose bone fragments in joint space after relocation
Hip arthroscopy can be used to evaluate intra-articular fractures and chondral injuries and to remove intra-articular fragments, Hip replacement surgery can also be considered if optimal stability is not achieved with relocation and fixation of the associated injuries.[16] Dislocation following hip replacement surgery might indicate revision surgery to ensure the stability of the hip in the long run.
Open reduction indications:[16]
- Used with challenging relocations or if any obstructions (e.g. loose fragments/soft tissue) is limiting closed reduction
- Deteriorating neurological signs following closed reduction (especially sciatic nerve function following posterior dislocation)
- Cases with proximal femur fractures, where manipulation of the leg is contra-indicated
Physiotherapy Management[edit | edit source]
Individuals with hip dislocation will require extensive physical therapy. It is important to take the time frames for soft tissue healing (and bone healing in cases with associated fractures) into consideration with rehabilitation following a hip dislocation. The orthopaedic surgeon will provide guidance on eg weight bearing restrictions that might be present following the medical management of the hip. Complete rehabilitation following hip dislocation can take 3-6 months.[14]
- Gait re-education: Initially with mobility assistive devices (walking frame/crutches) to limit weight bearing, and progression thereof
- Improve hip range of motion including hip mobilisations
- Strengthening of muscles around the hip, with special focus on hip stabilizers eg Hip abductors, adductors, extensors, flexors.
- Stretching
- Graded return to activity/sport
Clinical Bottom Line[edit | edit source]
Acquired, or traumatic hip dislocations are medical emergencies, and treatment should be sought as soon as possible. Relocation should ideally occur within 6 hours from the dislocation, in order to reduce complications. Traumatic dislocations are reduced either open or closed, and open or arthroscopy surgery might be indicated in cases with associated fractures. Physiotherapy plays an important role in the rehabilitation following a hip dislocation, in order to get the patients back to their previous level of function, and to prevent further dislocations.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Masiewicz S, Mabrouk A, Johnson DE. Posterior hip dislocation.Available:https://www.ncbi.nlm.nih.gov/books/NBK459319/ (accessed 7.1.2023)
- ↑ 2.0 2.1 2.2 Radiopedia Hip dislocation Available:https://radiopaedia.org/articles/hip-dislocation (accessed 7.1.2023)
- ↑ Orthobullets THA Dislocation Available:https://www.orthobullets.com/recon/5012/tha-dislocation (accessed 7.1.2022)
- ↑ S. Sanders, N. Tejwani, and K. A. Egol, “Traumatic hip dislocation—a review,” Bulletin of the NYU Hospital for Joint Diseases, vol. 68, no. 2, pp. 91–96, 2010.
- ↑ 5.0 5.1 5.2 5.3 Obakponovwe, O., Morell, D., Ahmad, M., Nunn, T., & Giannoudis, P. V. (2011).Traumatic hip dislocation. Orthopaedics and Trauma, 25(3), 214-222.
- ↑ S. Sanders, N. Tejwani, and K. A. Egol, “Traumatic hip dislocation—a review,” Bulletin of the NYU Hospital for Joint Diseases, vol. 68, no. 2, pp. 91–96, 2010.
- ↑ S. Sanders, N. Tejwani, and K. A. Egol, “Traumatic hip dislocation—a review,” Bulletin of the NYU Hospital for Joint Diseases, vol. 68, no. 2, pp. 91–96, 2010.
- ↑ Obakponovwe, O., Morell, D., Ahmad, M., Nunn, T., & Giannoudis, P. V. (2011).Traumatic hip dislocation. Orthopaedics and Trauma, 25(3), 214-222.
- ↑ Yang, & Cornwall, R. (2000). Initial treatment of traumatic hip dislocations in the adult. Clinical orthopaedics and related research (377), 24-31
- ↑ Pallia CS, Scott RE, Chao DJ. Traumatic hip dislocation in athletes. Curr Sports Med Rep. 2002 Dec;1(6):338-45
- ↑ 11.0 11.1 Hung NN. Traumatic hip dislocation in children. Journal of Pediatric Orthopaedics B 2012;21(6):542-51.
- ↑ Pallia CS, Scott RE, Chao DJ. Traumatic hip dislocation in athletes. Curr Sports Med Rep. 2002 Dec;1(6):338-45
- ↑ Larson DE. Gezin en gezondheid. Cambium BV:Zeewolde, 1995.
- ↑ 14.0 14.1 14.2 Ortho Info. Developmental Dislocation (Dysplasia) of the Hip (DDH). Available from: https://orthoinfo.aaos.org/en/diseases--conditions/developmental-dislocation-dysplasia-of-the-hip-ddh (accessed 08/08/2020).
- ↑ Bucholz R, Heckman JD. Rockwood e Green fraturas em adultos. In: Rockwood e Green fraturas em adultos, 2006: pp. 2263-2263.
- ↑ 16.0 16.1 16.2 Lima LC, Nascimento RA, Almeida VM, Façanha Filho FA. Epidemiology of traumatic hip dislocation in patients treated in Ceará, Brazil. Acta ortopedica brasileira 2014;22(3):151-4.
- ↑ 17.0 17.1 Nilsdotter, A., & Bremander, A. (2011). Measures of hip function and symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score(HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopaedic Surgeons (AAOS) Hip and Knee Questionnaire. Arthritis Care & Research, 63(S11), 200-207.
- ↑ 18.0 18.1 Shi, H. Y., Mau, L. W., Chang, J. K., Wang, J. W., & Chiu, H. C. (2009). Responsiveness of the Harris Hip Score and the SF-36: five years after total hip arthroplasty. Quality of Life Research, 18(8)
- ↑ 19.0 19.1 Hoeksma, H., Van den Ende, C., Ronday, H., Heering, A., Breedveld, F., & Dekker,J. (2003). Comparison of the responsiveness of the Harris Hip Score with generic measures for hip function in osteoarthritis of the hip. Annals of the Rheumatic Diseases, 62(10), 935-938.
- ↑ Garellick, G., Herberts, P., & Malchau, H. (1999). The value of clinical data scoring systems: are traditional hip scoring systems adequate to use in evaluation after total hip surgery? The Journal of Arthroplasty, 14(8), 1024-1029.
- ↑ Wamper, K. E., Sierevelt, I. N., Poolman, R. W., Bhandari, M., & Haverkamp, D. (2010). The Harris hip score: Do ceiling effects limit its usefulness in orthopaedics? Acta Orthopaedica, 81(6), 703-707.
- ↑ Medscape. Hip dislocation. Available from: https://emedicine.medscape.com/article/86930-overview (accessed 09/08/2020).