Leg Length Discrepancy
Original Editor - Matthias Verlinden
Top Contributors - Vanessa Rhule, Lucinda hampton, Kim Jackson, Admin, Wanda van Niekerk, Lauren Lopez, Lucas Villalta, Lilian Ashraf, Chrysolite Jyothi Kommu, Matthias Verlinden, WikiSysop and Meaghan Rieke
Definition[edit | edit source]
Leg length discrepancy (LLD) or anisomelia, is defined as a condition in which the paired lower extremity limbs have a noticeably unequal length. Leg length discrepancy (LLD) has been a controversial issue among researchers and clinicians for many years. Its presence is accepted but there is little consensus as to its many aspects, including the extent of LLD considered to be clinically significant, the prevalence, reliability, and validity of the measuring methods, the effect of LLD on function, and its role in various neuromusculoskeletal conditions[1].
Classification of Leg Length Discrepancy[edit | edit source]
There are two types of limb length discrepancy (LDD)[2]
Anatomical[edit | edit source]
Structural limb length inequality. It’s a physical (osseous) shortening of one lower limb between the trochanter femoral major and the ankle mortise. Congenital conditions include mild developmental abnormalities found at birth or childhood, whereas acquired conditions include trauma, fractures, orthopedic degenerative diseases, and surgical disorders such as joint replacement. A systemic review evaluating the prevalence of LLD by radiographic measurements revealed that 90% of the normal population had some type of variance in bony leg length, with 20% exhibiting a difference of >9 mm.[1]
Functional[edit | edit source]
Non-structural shortening. It is a unilateral asymmetry of the lower extremity without any shortening of the osseous components of the lower limb. FLLD may be caused by an alteration of lower limb mechanics, such as joint contracture, static or dynamic mechanical axis malalignment, muscle weakness, or shortening. It is impossible to detect these faulty mechanics using a non-functional evaluation, such as radiography. FLLD can develop due to an abnormal motion of the hip, knee, ankle, or foot in any of the three planes of motion.[1]
It is clear that studies using persons with long-standing true LLD are able to cope with larger LLD than those who are subjected to artificial or induced LLD. This is reasonable since given enough time most individuals would be able to reduce the energy and mechanical costs of LLD. Also, younger persons, on the whole, are able to adapt to larger LLD than older persons (considering that it has been shown that gait patterns differ considerably between old and young individuals and that older persons have greater difficulty in mastering novel motor tasks this makes sense). The level of activity of the person also seems to play a role. Individuals who are on their feet most of the day or who are involved in sports seem to be more sensitive to LLD than those who are less active.[3]
Epidemiology[edit | edit source]
It can be found in approximately 70% to 90% of the population[1].[4] Passive structural changes – pelvic torsion, mild lumbar scoliosis, facet angulation, changes in muscle length – seem capable of compensating for anatomic LLD of up to 20 mm. Past the ~ 20 mm point, passive structural changes give way to active muscular compensatory measures[5].The final extent of a leg-length discrepancy first noted during the growing years can be estimated with predictive algorithms to within 2 cm.[6]
Some authors have tried to determine a significant LDD by quantification, others by a significant discrepancy in functional outcomes.[4] Prevalence rates for leg length difference often lack crucial information regarding demographics, examiner experience, methods to recruit patients, methods used to detect leg inequality, and yet it is often cited and used by other authors.
Etiological Factors[edit | edit source]
True LLD
- Idiopathic developmental abnormalities
- Fracture
- Trauma to the epiphyseal endplate prior to skeletal maturity
- Degenerative disorders
- Legg-Calvé- Perthes Disease
- Cancer or neoplastic changes
- Infections
Functional LLD
- Shortening of soft tissues
- Joint contractures
- Ligamentous laxity
- Axial malalignments
- Foot biomechanics (such as excessive ankle pronation)
The Role of LLD on Posture and Gait[edit | edit source]
The Role of LDD in Standing[edit | edit source]
Check for specific compensation used by the patient to level out the difference in height.
| Longer Leg | Short Leg | |
| Foot | Pronation | Supination |
| Ankle | Dorsiflexion | Plantarflexion |
| Knee | Flexion | Extension |
| Hip | Flexion and Internal Rotation | Extension and External Rotation |
| Innominate bone[7] | Posterior Rotation | Anterior Rotation |
- If the leg is left uncompensated, the anterior and posterior iliac spine on the side of the short leg can be lower which may result in a sacral base unleveling and/or scoliosis;
- Increased muscle activity in several muscle groups.
The Role of LLD in Walking[edit | edit source]
Gait asymmetries throughout the kinetic chain.
Increased vertical displacement of the center of mass resulting in increased energy consumption. Compensatory mechanisms for this include-calcaneal eversion: knee extension: toe walking: circumduction: hip or knee flexion (steppage gait).
Decreased stance time and stride length in the shorter leg.
Decreased walking velocity, increased walking cadence.
The Role of LLD in Running[edit | edit source]
Biomechanics in running is different from walking, as is the effect of LLD. In running, the vertical oscillation is greater and there is no double support so weight is not shared between legs. The stance phase is only 30% in running whereas 60% in walking. This results in stress on the lower extremity that is three times that of walking. Evidence is conflicting about the effect of running but it is suggested that the effect is also augmented threefold.[1]
Associated Musculoskeletal Disorders [edit | edit source]
Low Back Pain The current literature is very ambiguous. LLD appears to affect the lumbar spine, at least in part, by creating lumbar scoliosis. It has been shown that LLD leads to pelvic obliquity on the frontal plane inducing scoliosis.[4] Lumbosacral facet joint angles appear to be smaller on the short side, it is hypothesized that asymmetry of joint angles predisposes patients to osteoarthritic changes in the lumbosacral joints.
Further research will conclude if LLD is merely associated or an objective causal factor in low back pain (LBP), The literature at hand is contradicting and non-conclusive.
Hip Pain A longer leg might be a predisposing factor in Osteoarthritis (OA). With length increasing, femoral head contact/ weight-bearing area is decreasing. (+10mm- 5%/ +50mm - 25,1%). Combined with an increased tone in hip abductors caused by the elongated distance between origin and insertion and an increased GRF puts the longer leg at risk.
Stress Fractures Greater incidence of stress fractures in the tibia, metatarsals, and femur of the longer leg appears consistent with the greater forces emitted trough the longer leg described under hip pain.
Others There seems to be an association with trochanteric bursitis, patellar capacities, patellar joint incongruences, and myofascial pain syndrome of the peroneus longus.
Differential Diagnosis[edit | edit source]
- Pelvis shift
- Low back pain (LBP)
- Idiopathic Scoliosis
- Iliotibial band syndrome
- Foot pronation
- Stress fractures lower extremity
Examination and Outcome Measures[edit | edit source]
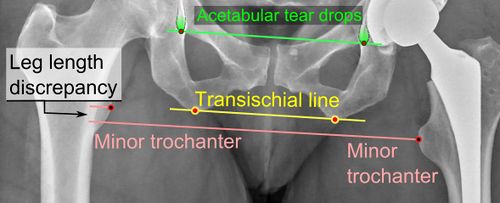
The most accurate method to identify leg (limb) length inequality (discrepancy) is through radiography. This time consumming task for radiologists that can be speed up using deep learning techniques (a computer tool to determine leg length automatically from X-rays).[9] It’s also the best way to differentiate an anatomical from a functional limb length inequality.
Medical Imaging Methods Include:
- A single exposure of the standing subject, imaging the entire lower extremity. Limitations are an inherent inaccuracy in patients with hip or knee flexion contracture and the technique is subject to a magnification error.
- Computed Tomography (CT-scan)1: It has no greater accuracy compared to the standard radiography. The increased cost for CT-scan may not be justified unless a contracture of the knee or hip has been identified or radiation exposure must be minimized.
- However, radiography has to be performed by a specialist, takes more time, and is costly. It should only be used when accuracy is critical. Therefore two general clinical methods were developed for assessing LLI.[10][11]
Direct Methods
Involves measuring limb length with a tape measure between 2 defined points, in the stand. Two common points are the anterior iliac spine and the medial malleolus or the anterior inferior iliac spine and lateral malleolus.[10][11]
Be careful, however, because there is a great deal of criticism and debate surroundings the accuracy of tape measure methods. If you choose this method, keep the following topics and possible errors in mind:
- Always use the mean of at least 2 or 3 measures
- If possible, compare measures between 2 or more clinicians
- Iliac asymmetries may mask or accentuate a limb length inequality
- Unilateral deviations in the long axis of the lower limb (eg. Genu varum,…) may mask or accentuate a limb length inequality
- Asymmetrical position of the umbilicus
- Joint contractures
Palpation of bony landmarks, most commonly the iliac crests or anterior iliac spines, in standing. These methods consist of detecting if bony landmarks are at (the horizontal) level or if limb length inequality is present.
Palpation and visual estimation of the iliac crest (or ASIS) in combination with the use of blocks or book pages of known thickness under the shorter limb to adjust the level of the iliac crests (or ASIS) appears to be the best (most accurate and precise) clinical method to asses limb inequality.
You should keep in mind that asymmetric pelvic rotations in planes other than the frontal plane may be associated with limb length inequality. A review of the literature suggests, therefore, that the greater trochanter major and as many pelvic landmarks should be palpated and compared (left trochanter with right trochanter) when the block correction method is used.
The PALM (Palpation Meter)
The PALM[14] is a reliable and valid instrument for measuring pelvic height difference. It is convenient, cost-effective, and is a good alternative to radiographic measurement!
Measurement Procedure: 2 tape strips were placed on the ground, 15cm apart. The tape strips mark the location on the floor where patients have to place their feet. The patients are asked to walk for 10 steps and align the medial borders of their feet with the outside of the tape strips. Patients have to stand fully erected (no knee or hip or spine bending). The PALM is placed on the most superior aspect of the iliac crest. The distance between caliper heads is measured to the nearest mm and the angle of inclination to the nearest half degree. The inclinometer ball is designed to move towards the side of the shorter limb.[14]
Measurement Using Blocks
The patient is standing with feet 10 cm apart, knees extended and equal weight on both feet. The clinician places his/her hands on a bilateral anatomical structure: Spina iliaca posterior superior, Spina iliaca anterior superior, or crista iliaca left and right. Now the clinician visually assesses if there is a length inequality, and if so, places a wooden board of 0,5 cm under the foot of the shorter side. Keep placing thicker planks under the shorter side until the equal length is reached, the thickness of the plank is equal to the leg length difference.
Although reliability is highly dependent on the accurate measurements of the clinician, this method has shown excellent results in inter-examination results between highly trained clinicians and medical students. Confounding variables reported by literature are pelvic asymmetry, incorrect positioning of feet, obesity, joint contractures, scoliosis, and inaccurate measurement.
Leg Length Discrepancy After Total Hip Arthroplasty[edit | edit source]
Clinical Signs[edit | edit source]
Patients can be categorized into three types according to the presentation of symptoms:
- Most commonly, patients with pain from the resultant imbalance in muscle forces around the hip and knee, as well as around the spine.
- Pain and fatigue from the longer leg’s Quadriceps and hamstring muscles (flexed knee syndrome). Patients flex their knee during gait to maintain level pelvis.
- Instability or dislocation as a result of component orientation, the pain is often a result of hip and periarticular muscle fatigue from preventing subluxations.
Correctable cause after Total Hip Arthroplasty (THA) - initial postoperative apparent LLD. The initial postoperative LLD can be described as periarticular muscle spasm, lumbosacral scoliosis, and pelvic obliquity. They can each produce this early postoperative LLD. The physical result is a tilted pelvis relative to the floor, with the surgical hemipelvis pushed inferiorly and the contralateral hemipelvis pulled superiorly, giving an apparent LLD despite equal lengths from the anterior superior iliac spines to medial malleoli.
The mainstay of treatment for this problem is patient education, reassurance, physical therapy muscle techniques, and possibly a temporary shoe lift. The patient should be reassured that most cases resolve within six months from surgery.
Medical Management[edit | edit source]
Two factors dictate if intervention is needed or not: the magnitude of the inequality and whether or not the patient is symptomatic. It has been suggested to divide limb length inequality into three categories: mild (0-30 mm), moderate (30-60mm), and severe (>60mm). In addition, it had been suggested that mild cases shouldn’t be treated surgically, except if the patient is symptomatic then a non-surgical intervention can be applied. Moderate cases should be dealt with case by case and may be dealt with surgical intervention. Severe cases should be corrected surgically. [4].
Surgical Intervention[edit | edit source]
The treatments surgically induced slowing of growth by blockade of the epiphyseal plates around the knee joint, or leg lengthening with osteotomy and subsequent distraction of the bone callus with fully implanted or external apparatus.[6]
- Consist of stopping the bone growth (in the longest leg) in adolescents and children.
- Sometimes, in patients with skeletal maturity, limb shortening by bone resection procedures is sometimes performed.
- Limb lengthening is generally reserved for LLI greater than 40-50mm. It involves cortical osteotomy followed by the extremity being fitted with an external fixation device that applies continuous longitudinal distraction across the osteotomy site.
Physical Therapy Management[edit | edit source]
The non-surgical intervention is mainly used for the functional leg length discrepancies. It is also applied to the mild category of limb length inequality.
Non-surgical Intervention[edit | edit source]
Consists of stretching the muscles of the lower extremity. This is individually different, whereby eg Tensor Fascia Latae, the adductors, the hamstring muscles, piriformis, and Iliopsoas are stretched or any muscles in the kinetic chain needing stretching or strengthening are addressed.
This non-surgical intervention belongs also to the use of shoe lifts. These shoe lifts consist of either a shoe insert (up to 10-20mm of correction) or building up the sole of the shoe on the shorter leg (up to 30-60mm of correction). This lift therapy should be implemented gradually in small increments. See section below.
Several studies have examined the treatment of low back pain patients with LLD with shoe lifts. Gofton obtained good results: the patients experienced major or complete pain relief that lasted upon follow-up ranging from 3 to 11 years. Helliwell also observed patients whereby 44% experienced complete pain relief, and 45% had moderate or substantial pain relief. Friberg found that 157 (of 211) patients with LBP, treated with shoe lifts, were symptom-free after a mean follow-up of 18 months.
A study in 2016 looking into "The Effectiveness of Specific Exercise Approach or Modifiable Heel Lift in the Treatment of Functional Leg Length Discrepancy in Early Post-surgery Inpatients after Total Hip Arthroplasty" concluded that specific exercise approach and modifiable heel lift use, during early post-operative recovery, can produce relevant changes in functional LLD after THA.[15]
However, evidence in the literature regarding the use of lift therapy is inconsistent.
LLD, Shoe Lifts and Low Back Pain[edit | edit source]
Shoe lifts can reduce low back pain if patients’ low back pain is correlated to the LLD. See Differential Diagnosis! Important is to gradually increase the corrective lift, rather than correct a fixed percentage of LLD. Shoe inserts appear to reduce (chronic) low back pain and functional disability in patients with LLDs of 10mm or less. It can be added to the treatment (low back exercises). The importance of exercises lies in the fact that (one study suggests that:) the quadratus lumborus endurance ipsilateral to the supine short leg has significantly decreased endurance compared to people with no leg-length asymmetry. However, this is only 1 small observational study, and further research about changes in muscle endurance and strength in people with LLD is needed.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Khamis S, Carmeli E. A new concept for measuring leg length discrepancy. Journal of orthopaedics. 2017 Jun;14(2):276. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5376249/ Last accessed 12.11.2019)
- ↑ D’Amico JC. Keys to recognizing and treating limb length discrepancy. Podiatry Today. 2014;27(5):66-75. Available from: https://www.podiatrytoday.com/keys-recognizing-and-treating-limb-length-discrepancy Last accessed 12.11.2019)
- ↑ Gurney B. Leg length discrepancy. Gait & posture. 2002 Apr 1;15(2):195-206. Available from: https://www.livta.com.br/material/leg-length-discrepancy.pdf (last accessed 12.11.2019)
- ↑ 4.0 4.1 4.2 4.3 Gurney B. Leg length discrepancy. Gait & Posture. 2002. 15; 2: 195-206.
- ↑ Knutson GA. Anatomic and functional leg-length inequality: a review and recommendation for clinical decision-making. Part I, anatomic leg-length inequality: prevalence, magnitude, effects and clinical significance. Chiropractic & osteopathy. 2005 Dec;13(1):11. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1232860/ Last accessed 12.11.2019
- ↑ 6.0 6.1 Björn Vogt, Dr. med., Georg Gosheger, Prof. Dr. med.,Thomas Wirth, Prof. Dr. med., Joachim Horn, MD, PhD, and Robert Rödl, Prof. Dr. med.Dtsch Arztebl Int. 2020 Jun; 117(24): 405–411.Published online 2020 Jun 12. doi: 10.3238/arztebl.2020.0405 Leg Length Discrepancy- Treatment Indications and Strategies. Duetsches Arzteblatt International.US National Library of Medicine National Institutes of Health.
- ↑ Resende RA, Kirkwood RN, Deluzio KJ, Morton AM, Fonseca ST. Mild leg length discrepancy affects lower limbs, pelvis and trunk biomechanics of individuals with knee osteoarthritis during gait. Clinger's Biomech. 2016. 38: 1–7.
- ↑ Richard Blake.Short Leg Syndrome: Limb Dominance in Walking Gait Available from:https://www.youtube.com/watch?v=hjPI7x1RHQg [last accessed 6/8/2021]
- ↑ Sastre-García B, Pérez-Pelegrí M, Martín JA, Santabárbara JM, Moratal D. Deep Learning Segmentation of Lower Extremities Radiographs for an Automatic Leg Length Discrepancy Measurement. In2023 45th Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC) 2023 Jul 24 (pp. 1-4). IEEE.Available:https://pubmed.ncbi.nlm.nih.gov/38082685/ (accessed 28.12.2023)
- ↑ 10.0 10.1 10.2 Brady RJ, Dean JB, Skinner TM, Gross MT. Limb length inequality: clinical implications for assessment and intervention. J Orthop Sports Phys Ther. 2003 May;33(5):221-34. Accessed 24 June 2019.
- ↑ 11.0 11.1 11.2 Gross MT, Burns CB, Chapman SW, Hudson CJ, Curtis HS, Lehmann JR, Renner JB. Reliability and validity of rigid lift and pelvic leveling device method in assessing functional leg length inequality. J Orthop Sports Phys Ther. 1998 Apr;27(4):285-94. Accessed 24 June 2019.
- ↑ MSK Medicine. True leg length measurement. Available from: http://www.https://www.youtube.com/watch?v=HTqifTH98K4 [last accessed 6/8/2021]
- ↑ physical therapy nation Standing Exam: Leg Length Inequality/Pelvic Symmetry Available from: https://www.youtube.com/watch?v=wmgA1pw6BAM (last accessed 12.11.2019)
- ↑ 14.0 14.1 Petrone MR, Guinn J, Reddin A, Sutlive TG, Flynn TW, Garber MP. The accuracy of the Palpation Meter (PALM) for measuring pelvic crest height difference and leg length discrepancy. J Orthop Sports Phys Ther. 2003 Jun;33(6):319-25. Accessed 24 June 2019.
- ↑ NAKANOWATARI T, SUZUKAMO Y, IZUMI SI. The Effectiveness of Specific Exercise Approach or Modifiable Heel Lift in the Treatment of Functional Leg Length Discrepancy in Early Post-surgery Inpatients after Total Hip Arthroplasty: A Randomized Controlled Trial with a PROBE design. Physical therapy research. 2016 Dec 20;19(1):39-49. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5342963/ (last accessed 12.11.2019)