Gait Training in Stroke: Difference between revisions
m (creation of chart from previous text for ease of reading) |
Kim Jackson (talk | contribs) No edit summary |
||
| (26 intermediate revisions by 5 users not shown) | |||
| Line 6: | Line 6: | ||
<br> | <br> | ||
== Introduction == | |||
The [[Nagi's Disability Model|functional limitations and impairments]] after a [[stroke]] are unique to each individual | [[File:AFO CVA.jpeg|thumb|359x359px|AFO (water proof dynamic)]] | ||
The [[Nagi's Disability Model|functional limitations and impairments]] after a [[stroke]] are unique to each individual and often include impairments in mobility. | |||
[[Gait]] recovery is a major objective in the rehabilitation program for persons with [[stroke]], and often a person's top goal. Restoring function after stroke is a complex process involving spontaneous recovery and the effects of therapeutic interventions. Although the majority of persons with a stroke regain the ability to walk, many do not achieve the ambulation endurance, speed, or security required to perform their [[Activities of Daily Living|daily activities]] independently and safely. [[Falls]] are a common concern for community-dwelling persons with stroke<ref name=":0" />. | |||
== Potential limitations Observed CVA Effecting Gait == | |||
Include changes in: | |||
* Muscle tone ([[spasticity]] or flaccidity) | |||
* Muscle strength | |||
* Timing of the gait cycle, resulting in an asymmetrical [[Gait Deviations|gait pattern]] | |||
* [[Walking - Muscles Used|Walking]] speed | |||
* [[Balance]] systems | |||
* [[Sensation]] | |||
* Visual scanning | |||
* [[Cognitive Deficits|Cognition]] and safety awareness | |||
* Soft tissue length (contractures) | |||
== Stroke Rehabilitation Principles == | |||
"Normal" gait is a complex activity and skilled personalized therapeutic interventions are needed for successful stroke rehabilitation. Several general principles underpin the process of stroke rehabilitation: | |||
* Good rehabilitation outcome seems to be strongly associated with high degree of motivation, and engagement of the patient and their family. | * Good rehabilitation outcome seems to be strongly associated with high degree of motivation, and engagement of the patient and their family. | ||
* Setting goals according to specific rehabilitation aims of an individual might improve the outcomes. | * Setting goals according to specific rehabilitation aims of an individual might improve the outcomes. | ||
* Cognitive function is strongly related to successful rehabilitation. Attention is a key factor for rehabilitation in persons with stroke as poorer attention performances are associated with a more negative impact of stroke disability on daily functioning<ref name=":0">Belda-Lois JM, Mena-del Horno S, Bermejo-Bosch I, Moreno JC, Pons JL, Farina D, Iosa M, Molinari M, Tamburella F, Ramos A, Caria A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3261106/ Rehabilitation of gait after stroke: a review towards a top-down approach]. Journal of neuroengineering and rehabilitation. 2011 Dec 1;8(1):66.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3261106/ (last accessed 5.2.2020)</ref> | * [[Cognitive Behavioural Therapy|Cognitive]] function is strongly related to successful rehabilitation. Attention is a key factor for rehabilitation in persons with stroke as poorer attention performances are associated with a more negative impact of stroke disability on daily functioning<ref name=":0">Belda-Lois JM, Mena-del Horno S, Bermejo-Bosch I, Moreno JC, Pons JL, Farina D, Iosa M, Molinari M, Tamburella F, Ramos A, Caria A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3261106/ Rehabilitation of gait after stroke: a review towards a top-down approach]. Journal of neuroengineering and rehabilitation. 2011 Dec 1;8(1):66.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3261106/ (last accessed 5.2.2020)</ref>. | ||
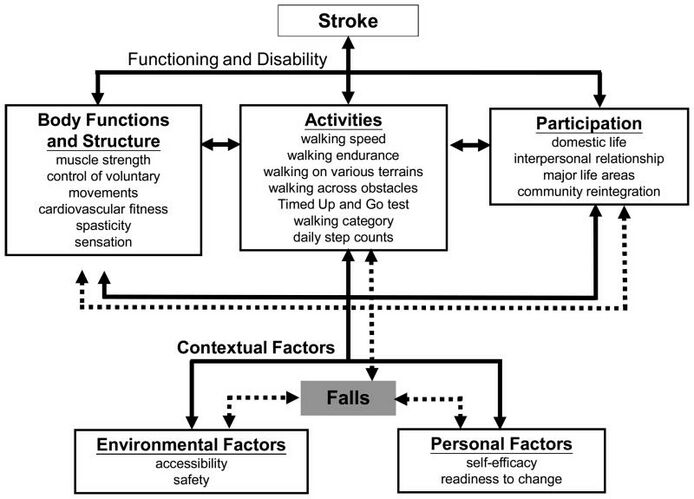
[[File:ICF_STROKE.jpg|alt=|thumb|694x694px|Stroke ICF|center]] | |||
=== Understanding Normal Gait === | |||
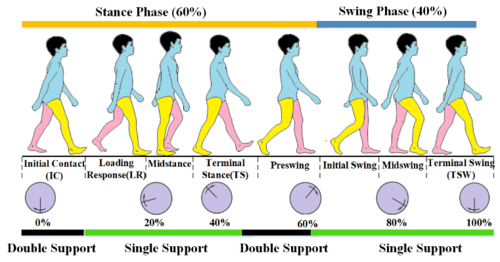
[[File:Phases of gait cycle.png|thumb|500x500px|Phases of gait cycle]] | |||
Gait training, regardless of the client's diagnosis, is based on an understanding of "normal" gait. During a therapy evaluation, it is important to gather information on the person with stroke's baseline level of activity and mobility - this data can be collected from the person themselves or reliable family members or friends. All this information is taken into account when creating a person's individualized therapy program. | Gait training, regardless of the client's diagnosis, is based on an understanding of "normal" gait. During a therapy evaluation, it is important to gather information on the person with stroke's baseline level of activity and mobility - this data can be collected from the person themselves or reliable family members or friends. All this information is taken into account when creating a person's individualized therapy program. | ||
Please visit related links as needed for background information: [[Gait Cycle|gait cycle]], [[Gait | Please visit related links as needed for background information: [[Gait Cycle|gait cycle]], [[Gait Deviations|gait disturbances]]. | ||
The ability to walk independently is a prerequisite for most daily activities, whether a person is homebound or a community distance ambulator. Think of all the skills needed to safely negotiate a community setting: cross a street in the time allotted by pedestrian lights, to step on and off a moving walkway, in and out of automatic doors, avoid obstacles, negotiate curbs, multi-task mobility with environmental scanning, understand the safety signals found in your environment. A walking velocity of 1.1-1.5 m/s is considered normal baseline speed to safely function as a community dwelling individual. It has been reported that only 7% of patients discharged from rehabilitation met the criteria for community walking, which included the ability to walk 500 m continuously at a speed that would enable them to cross a road safely<ref>Hill K, Ellis P, Bernhardt Jet al. (1997) Balance and mobility outcomes for stroke patients: a comprehensive audit. Aust J Physiother, 43, 173-180.</ref>. | The ability to walk independently is a prerequisite for most daily activities, whether a person is homebound or a community distance ambulator. Think of all the skills needed to safely negotiate a community setting: cross a street in the time allotted by pedestrian lights, to step on and off a moving walkway, in and out of automatic doors, avoid obstacles, negotiate curbs, multi-task mobility with environmental scanning, understand the safety signals found in your environment. A walking velocity of 1.1-1.5 m/s is considered normal baseline speed to safely function as a community dwelling individual. It has been reported that only 7% of patients discharged from rehabilitation met the criteria for community walking, which included the ability to walk 500 m continuously at a speed that would enable them to cross a road safely<ref>Hill K, Ellis P, Bernhardt Jet al. (1997) Balance and mobility outcomes for stroke patients: a comprehensive audit. Aust J Physiother, 43, 173-180.</ref>. | ||
| Line 36: | Line 40: | ||
''The major requirements for successful walking<ref>Forssberg H (1982) Spinal locomotion functions and descending control. In Brain Stem Control of Spinal Mechanisms (eds B Sjolund, A Bjorklund), Elsevier Biomedical Press,New York.</ref> include:'' | ''The major requirements for successful walking<ref>Forssberg H (1982) Spinal locomotion functions and descending control. In Brain Stem Control of Spinal Mechanisms (eds B Sjolund, A Bjorklund), Elsevier Biomedical Press,New York.</ref> include:'' | ||
*Support of body mass by lower limbs | *Support of [[Body Mass Index|body mass]] by lower limbs | ||
*Propulsion of the body in the intended direction | *Propulsion of the body in the intended direction | ||
*The production of a basic locomotor rhythm | *The production of a basic locomotor rhythm | ||
*Dynamic | *Dynamic balance control of the moving body | ||
*Flexibility, i.e. the ability to adapt the movement to changing environmental demands and goals. | *Flexibility, i.e. the ability to adapt the movement to changing environmental demands and goals. | ||
=== Gait after Stroke === | |||
Abnormal gait patterns are a common impairment following a stroke due to disruption of neural pathways in the motor cortex, their communication with the [[brainstem]] and its [[Spinal cord anatomy|descending pathways]] and intraspinal locomotor network. This damage results in observed muscle weakness, changes in muscle tone, and abnormal synergistic movement patterns commonly seen in persons with stroke.<ref>Li S, Francisco GE, Zhou P. [https://www.frontiersin.org/articles/10.3389/fphys.2018.01021/full Post-stroke hemiplegic gait: new perspective and insights.] Frontiers in physiology. 2018;9:1021. Available from: https://www.frontiersin.org/articles/10.3389/fphys.2018.01021/full (last accessed 29.11.2019)</ref>. Secondary impairments stemming from the cardiovascular and musculoskeletal systems stemming from disuse and physical inactivity can add to ambulation difficulty. The resulting gait pattern following stroke is often a combination of movement deviations and new compensatory movement patterns, unique to that person's injury.<ref>Balaban, Birol et al.:Gait Disturbances in Patients With Stroke : PM&R , Volume 6 , Issue 7 , 635 - 642</ref>. As with all rehabilitation programs, gait training with a person following a stroke is highly individualized. The below video shows an example of progressive intensive individualized gait training. | Abnormal gait patterns are a common impairment following a stroke due to disruption of neural pathways in the motor [[Cerebral Cortex|cortex]], their communication with the [[brainstem]] and its [[Spinal cord anatomy|descending pathways]] and intraspinal locomotor network. This damage results in observed muscle weakness, changes in muscle tone, and abnormal synergistic movement patterns commonly seen in persons with stroke.<ref>Li S, Francisco GE, Zhou P. [https://www.frontiersin.org/articles/10.3389/fphys.2018.01021/full Post-stroke hemiplegic gait: new perspective and insights.] Frontiers in physiology. 2018;9:1021. Available from: https://www.frontiersin.org/articles/10.3389/fphys.2018.01021/full (last accessed 29.11.2019)</ref>. Secondary impairments stemming from the [[Cardiovascular System|cardiovascular]] and musculoskeletal systems stemming from disuse and physical inactivity can add to ambulation difficulty. The resulting gait pattern following stroke is often a combination of movement deviations and new compensatory movement patterns, unique to that person's injury.<ref>Balaban, Birol et al.:Gait Disturbances in Patients With Stroke : PM&R , Volume 6 , Issue 7 , 635 - 642</ref>. As with all rehabilitation programs, gait training with a person following a stroke is highly individualized. The below video shows an example of progressive intensive individualized gait training. | ||
{{#ev:youtube|https://www.youtube.com/watch?v=g__BYaS9viw|width}}<ref>H Hayes Hospital Physical Therapy Restores Walking After Stroke Available from: https://www.youtube.com/watch?v=g__BYaS9viw (last accessed 29.11.2019)</ref> | {{#ev:youtube|https://www.youtube.com/watch?v=g__BYaS9viw|width}}<ref>H Hayes Hospital Physical Therapy Restores Walking After Stroke Available from: https://www.youtube.com/watch?v=g__BYaS9viw (last accessed 29.11.2019)</ref> | ||
| Line 96: | Line 100: | ||
* decreased dorsiflexor activity | * decreased dorsiflexor activity | ||
|} | |} | ||
{{#ev:youtube|ihz74Zv6D84}} | |||
{{#ev:youtube| | |||
<ref>Hemiplegic Gait – Case Study 13 Available from: <nowiki>https://www.youtube.com/watch?v=ihz74Zv6D84</nowiki> (last accessed 23.10.2021)</ref> | |||
As can be seen in the above videos, the persons with stroke demonstrated the following spatiotemporal adaptations: decreased walking speed, short and/or uneven step and stride lengths, increased stride width, increased double support phase, and dependence on assistive device through the hands<ref name="carr" />. | |||
== Gait Training == | |||
=== | ==== Therapeutic Interventions ==== | ||
Stroke rehabilitation is highly individualized to a person with stroke's needs. A physical therapy plan of care can include any or all of the following interventions to improve ambulation ability: | |||
*Preventing adaptive changes in lower limb soft tissues | |||
*Eliciting voluntary activation in key muscle groups in lower limbs | |||
*Increasing muscle strength and [[Coordination Exercises|coordination]] | |||
*Increasing walking velocity and endurance | |||
*Maximizing skill, eg increasing flexibility | |||
*Increasing static and dynamic balance | |||
*Increasing cardiovascular fitness | |||
*Increasing safety awareness | |||
*Education on proper use of assistive devices | |||
====<span>Conventional Gait Training </span>==== | |||
Conventional gait training (over ground gait training) involves breaking down parts of the gait cycle, training and improving the abnormal parts, then reintegrating them into ambulation to return to a more normal gait cycle. This can include the following: | |||
= | *Symmetrical weight bearing between lower limbs in stance | ||
*Weight shifting between lower limbs | |||
*Stepping training (swinging/clearance) over level and unloved surfaces | |||
*Heel strike/limb loading acceptance | |||
*Single leg stance with stable balance and control | |||
*Push off/initial swing of moving leg | |||
The following components of gait are key to successful ambulation: | |||
*Support of the center of gravity (COG) by the lower limbs | |||
*Propulsion of the COG by the lower limbs | |||
*[[Balance]] of the COG as it transitions between weight bearing limbs | |||
*Controlling knee and toe paths for toe clearance and foot placement | |||
*Optimizing rhythm and coordination<ref name="carr" />. | |||
Observe for abnormalities of any of these parts and develop therapeutic interventions to improve those skills. It is important to gather information on a person's normal environment during your evaluation and continued assessment. This information will help shape your gait training plan of care to include skill such as: | |||
* stair and curb negotiation | |||
* ambulation over obstacles | |||
* ambulation over carpet, tile, doorway thresholds | |||
* ambulation over changes in grades such as ramps and slopes | |||
* ambulation over uneven outdoor surfaces such as grass, loose rock, wet surfaces, sidewalks, road surfaces | |||
Special consideration for persons with stroke during gait training is the potential need for orthotics to assist with abnormalities such as drop foot. Read more about [[Stroke: Physiotherapy Treatment Approaches#sts=Orthotics|orthotics]]. | |||
==== Strength Training ==== | |||
All rehabilitation programs will involve strength training. This can be performed as a formal exercise program or through functional activities. | |||
* Circuit training | |||
* | * Strength training to improve walking ability | ||
* | * Task-specific training to improve walking ability'''<br>''' | ||
== < | ==== Neuromuscular Reeducation (NMR) ==== | ||
Neurofacilitation techniques to inhibit excessive tone, stimulate muscle activity (if hypotonia is present) and to facilitate normal movement patterns through hands-on techniques.<ref name="janice">Janice J Eng, PhD, PT/OT, Professor and Pei Fang Tang, PhD, PT ;Gait training strategies to optimize walking ability in people with stroke: A synthesis of the evidence; Expert Rev Neurother. Oct 2007; 7(10): 1417–1436.</ref> Practice based on the framework advocated by Berta [[Bobath Approach|Bobath]] remains the predominant physical therapy approach to stroke patients in the UK and is also common in many other parts of the world, including Canada, United States, Europe, Australia, Hong Kong and Taiwan. It has evolved from its original foundations, however elements still emphasize normal tone and the necessity of normal movement patterns to perform functional tasks <ref name="lennon">Lennon S, Baxter D, Ashburn A. Physiotherapy based on the Bobath concept in stroke rehabilitation: a survey within the UK. Disabil Rehabil. 2001;23(6):254–262.</ref> Examples of NMR handling techniques include: | |||
* Neuro Developmental Technique (NDT) | |||
* [[Kinesio Taping|Kinesio taping]] | |||
* Neuro-IFRAH | |||
==== Body Weight Supported Treadmill Training ==== | |||
Body Weigh Supported Treadmill Training (BWSTT) involves the use of a suspension system with harness over a treadmill for gait training. The person with stroke is secured in the harness for fall prevention, then is positioned over the treadmill and attached to the suspension system. Gait training with this modality allows for more control over the ambulation environment (level surfaces, grade of surface), control over the speed of ambulation, and allows one or more therapists to provide tactile cues or physical assist to achieve gait dynamics. The person can be unweighted by the suspension system, this reduces the amount of weight bearing through their lower limbs and gives the feeling of being lighter. Ambulation will therefore require less effort by the person during initial gait training sessions. Body weight can be slowly added back to the person's control as they progress through their BWSTT program. Skilled therapists can assist with limb advancement, heel strike, stance with knee control, and swing phases of gait with tactile cues. Upright posture can also be addressed with this treatment modality. The video below demonstrates how to setup a BSW treadmill system, handling techniques, and how to advance to suspension system to overground gait training. | |||
{{#ev:youtube|tq1_PDtTpd4}}<ref>Body Weight Supported Treadmill Available from: <nowiki>https://www.youtube.com/watch?v=tq1_PDtTpd4</nowiki> last accessed 23.10.2021)</ref> | |||
== | ==== Biofeedback ==== | ||
Forms of [[biofeedback]] have been in use in physical therapy for more than 50 years, where it is beneficial in the management of neuromuscular disorders. Biofeedback techniques have shown benefit when used as part of a physical therapy program for people with motor weakness or dysfunction after stroke. These methods are getting better at training for complex task-oriented activities like walking and grasping objects as technology continues to advance<ref>Malik K, Dua A. [https://www.ncbi.nlm.nih.gov/books/NBK553075/ Biofeedback]. [Updated 2019 Dec 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553075/</ref>. | |||
== | ==== Functional Electrical Stimulation ==== | ||
[[Functional Electrical Stimulation - Its role in upper limb recovery post-stroke|Functional Electrical Stimulation]] (FES) is a useful modality for rehabilitation after stroke, and can supplement NMR and strengthening interventions. FES is used to elicit action potentials in the peripheral nerves of axonal branches and generate muscle contractions via surface electrodes placed over a muscle group. The intensity of contraction can be controlled by adjusting the amount of stimulus given by the FES machine. Use of this modality requires a strong understanding of anatomy for proper electrode placement. FES has been used in rehabilitation of chronic hemiplegia since the 1960s<ref name=":0" />. | |||
FES can be performed using a [[Electrical Stimulation - Its role in upper limb recovery post-stroke|small handheld unit]], a wearable unit, or integrated into a upper or [[Functional Electrical Stimulation Cycling for Spinal Cord Injury|lower extremity bicycle]]. | |||
== Robotic-Assisted Training == | ==== Robotic-Assisted Training ==== | ||
Robotic devices provide safe, intensive and task-oriented rehabilitation to people with mild to severe neurologic injury. It | Stroke rehab requires hundreds of thousands of repetitions of a movement to cause permanent changes in the brain. New technology in the form of robotics can assist in achieving these numbers. Robotic devices provide safe, intensive and task-oriented rehabilitation to people with mild to severe neurologic injury. It provides: precisely controllable assistance or resistance during movements, good repeatability, objective and quantifiable measures of subject performance, and increased training motivation through the use of interactive biofeedback. Robotic-assisted training reduces the amount of physical assistance required to walk reducing health care costs, provides kinematic and kinetic data to control and quantify the intensity of practice, and measures changes and assess motor impairments with better sensitivity and reliability than standard clinical scales<ref>Juan-Manuel Belda-Lois et al; Rehabilitation of gait after stroke: a review towards a top-down approach ;Journal of NeuroEngineering and Rehabilitation 2011, 8:66</ref>. | ||
# | {{#ev:youtube|KWLgfP2ndes}}<ref>Watch a robotic exoskeleton help a stroke patient walk Available from: <nowiki>https://www.youtube.com/watch?v=KWLgfP2ndes</nowiki> last accessed 24.10.2021)</ref> | ||
=== Conclusions === | |||
Following a stroke, gait recovery is often a primary goal for our patients. It is a symbol of their independence and returning to normal. Due to the complexity of ambulation, individualized intensive rehabilitation programs are necessary to optimize recovery. Estimating rehabilitation effects on motor recovery is complex, due to the interaction of spontaneous recovery and therapeutic interventions. | |||
Treatment interventions to improve gait in persons with stroke range from physical hands-on cuing techniques, electrical stimulation, treadmill training, biofeedback, and robotics. New treatments are constantly being developed, adding to our treatment arsenal. It is often a combination of multiple treatment modalities and clinical experience and skill which lead to the best patient outcomes. | |||
== | === Additional Viewing === | ||
The video below demonstrates the phases of gait and shows an assessment of normal and common abnormal gait patterns. | |||
{{#ev:youtube|PZBiv0uSXVg}}<ref>Gait Assessment – normal gait and common abnormal gaits Available from: <nowiki>https://www.youtube.com/watch?v=PZBiv0uSXVg</nowiki> last accessed 24.10.2021)</ref> | |||
== References == | == References == | ||
Latest revision as of 12:10, 26 February 2024
Original Editor - Sheik Abdul Khadir
Top Contributors - Sheik Abdul Khadir, Stacy Schiurring, Kim Jackson, Garima Gedamkar, Lucinda hampton, Naomi O'Reilly, Vanessa Rhule, Evan Thomas, Admin, Simisola Ajeyalemi, Wanda van Niekerk, Lauren Lopez, 127.0.0.1, Aminat Abolade, WikiSysop, Adam Vallely Farrell, Vidya Acharya and Rucha Gadgil
Introduction[edit | edit source]
The functional limitations and impairments after a stroke are unique to each individual and often include impairments in mobility. Gait recovery is a major objective in the rehabilitation program for persons with stroke, and often a person's top goal. Restoring function after stroke is a complex process involving spontaneous recovery and the effects of therapeutic interventions. Although the majority of persons with a stroke regain the ability to walk, many do not achieve the ambulation endurance, speed, or security required to perform their daily activities independently and safely. Falls are a common concern for community-dwelling persons with stroke[1].
Potential limitations Observed CVA Effecting Gait[edit | edit source]
Include changes in:
- Muscle tone (spasticity or flaccidity)
- Muscle strength
- Timing of the gait cycle, resulting in an asymmetrical gait pattern
- Walking speed
- Balance systems
- Sensation
- Visual scanning
- Cognition and safety awareness
- Soft tissue length (contractures)
Stroke Rehabilitation Principles[edit | edit source]
"Normal" gait is a complex activity and skilled personalized therapeutic interventions are needed for successful stroke rehabilitation. Several general principles underpin the process of stroke rehabilitation:
- Good rehabilitation outcome seems to be strongly associated with high degree of motivation, and engagement of the patient and their family.
- Setting goals according to specific rehabilitation aims of an individual might improve the outcomes.
- Cognitive function is strongly related to successful rehabilitation. Attention is a key factor for rehabilitation in persons with stroke as poorer attention performances are associated with a more negative impact of stroke disability on daily functioning[1].
Understanding Normal Gait[edit | edit source]
Gait training, regardless of the client's diagnosis, is based on an understanding of "normal" gait. During a therapy evaluation, it is important to gather information on the person with stroke's baseline level of activity and mobility - this data can be collected from the person themselves or reliable family members or friends. All this information is taken into account when creating a person's individualized therapy program.
Please visit related links as needed for background information: gait cycle, gait disturbances.
The ability to walk independently is a prerequisite for most daily activities, whether a person is homebound or a community distance ambulator. Think of all the skills needed to safely negotiate a community setting: cross a street in the time allotted by pedestrian lights, to step on and off a moving walkway, in and out of automatic doors, avoid obstacles, negotiate curbs, multi-task mobility with environmental scanning, understand the safety signals found in your environment. A walking velocity of 1.1-1.5 m/s is considered normal baseline speed to safely function as a community dwelling individual. It has been reported that only 7% of patients discharged from rehabilitation met the criteria for community walking, which included the ability to walk 500 m continuously at a speed that would enable them to cross a road safely[2].
The major requirements for successful walking[3] include:
- Support of body mass by lower limbs
- Propulsion of the body in the intended direction
- The production of a basic locomotor rhythm
- Dynamic balance control of the moving body
- Flexibility, i.e. the ability to adapt the movement to changing environmental demands and goals.
Gait after Stroke [edit | edit source]
Abnormal gait patterns are a common impairment following a stroke due to disruption of neural pathways in the motor cortex, their communication with the brainstem and its descending pathways and intraspinal locomotor network. This damage results in observed muscle weakness, changes in muscle tone, and abnormal synergistic movement patterns commonly seen in persons with stroke.[4]. Secondary impairments stemming from the cardiovascular and musculoskeletal systems stemming from disuse and physical inactivity can add to ambulation difficulty. The resulting gait pattern following stroke is often a combination of movement deviations and new compensatory movement patterns, unique to that person's injury.[5]. As with all rehabilitation programs, gait training with a person following a stroke is highly individualized. The below video shows an example of progressive intensive individualized gait training.
Typical Kinematic Deviations seen in Gait after Stroke[edit | edit source]
| Gait Deviation | Clinical Observation | |
|---|---|---|
| Initial Stance | Limited ankle dorsiflexion |
|
| Lack of knee flexion (knee hyperextension) |
| |
| Midstance | Lack of Knee Extension (knee remains flexed 10-150 with excessive ankle dorsiflexion) |
|
| Knee Hyperextension (This interferes with preparation for push-off ) | contracture of soleus (an adaptation to fear of limb collapse due to weakness of muscles controlling the knee) | |
| Limited hip extension and ankle dorsiflexion with failure to progress body mass forward over the foot | contracture of soleus | |
| Excessive Lateral Pelvic Shift | decreased ability to activate stance hip abductors and control hip and knee extensors | |
| Late Stance (Pre-swing) | Lack of Knee Flexion and Ankle Plantar-flexion (prerequisites for push-off and preparation for swing) | weakness of calf muscles |
| Early and Mid-swing | Limited Knee Flexion normally 35-40° increasing to 60° for swing and toe clearance |
|
| Late-swing | Limited Knee Extension and Ankle Dorsiflexion jeopardising heel contact and weight-acceptance |
|
As can be seen in the above videos, the persons with stroke demonstrated the following spatiotemporal adaptations: decreased walking speed, short and/or uneven step and stride lengths, increased stride width, increased double support phase, and dependence on assistive device through the hands[7].
Gait Training [edit | edit source]
Therapeutic Interventions[edit | edit source]
Stroke rehabilitation is highly individualized to a person with stroke's needs. A physical therapy plan of care can include any or all of the following interventions to improve ambulation ability:
- Preventing adaptive changes in lower limb soft tissues
- Eliciting voluntary activation in key muscle groups in lower limbs
- Increasing muscle strength and coordination
- Increasing walking velocity and endurance
- Maximizing skill, eg increasing flexibility
- Increasing static and dynamic balance
- Increasing cardiovascular fitness
- Increasing safety awareness
- Education on proper use of assistive devices
Conventional Gait Training [edit | edit source]
Conventional gait training (over ground gait training) involves breaking down parts of the gait cycle, training and improving the abnormal parts, then reintegrating them into ambulation to return to a more normal gait cycle. This can include the following:
- Symmetrical weight bearing between lower limbs in stance
- Weight shifting between lower limbs
- Stepping training (swinging/clearance) over level and unloved surfaces
- Heel strike/limb loading acceptance
- Single leg stance with stable balance and control
- Push off/initial swing of moving leg
The following components of gait are key to successful ambulation:
- Support of the center of gravity (COG) by the lower limbs
- Propulsion of the COG by the lower limbs
- Balance of the COG as it transitions between weight bearing limbs
- Controlling knee and toe paths for toe clearance and foot placement
- Optimizing rhythm and coordination[7].
Observe for abnormalities of any of these parts and develop therapeutic interventions to improve those skills. It is important to gather information on a person's normal environment during your evaluation and continued assessment. This information will help shape your gait training plan of care to include skill such as:
- stair and curb negotiation
- ambulation over obstacles
- ambulation over carpet, tile, doorway thresholds
- ambulation over changes in grades such as ramps and slopes
- ambulation over uneven outdoor surfaces such as grass, loose rock, wet surfaces, sidewalks, road surfaces
Special consideration for persons with stroke during gait training is the potential need for orthotics to assist with abnormalities such as drop foot. Read more about orthotics.
Strength Training[edit | edit source]
All rehabilitation programs will involve strength training. This can be performed as a formal exercise program or through functional activities.
- Circuit training
- Strength training to improve walking ability
- Task-specific training to improve walking ability
Neuromuscular Reeducation (NMR)[edit | edit source]
Neurofacilitation techniques to inhibit excessive tone, stimulate muscle activity (if hypotonia is present) and to facilitate normal movement patterns through hands-on techniques.[9] Practice based on the framework advocated by Berta Bobath remains the predominant physical therapy approach to stroke patients in the UK and is also common in many other parts of the world, including Canada, United States, Europe, Australia, Hong Kong and Taiwan. It has evolved from its original foundations, however elements still emphasize normal tone and the necessity of normal movement patterns to perform functional tasks [10] Examples of NMR handling techniques include:
- Neuro Developmental Technique (NDT)
- Kinesio taping
- Neuro-IFRAH
Body Weight Supported Treadmill Training [edit | edit source]
Body Weigh Supported Treadmill Training (BWSTT) involves the use of a suspension system with harness over a treadmill for gait training. The person with stroke is secured in the harness for fall prevention, then is positioned over the treadmill and attached to the suspension system. Gait training with this modality allows for more control over the ambulation environment (level surfaces, grade of surface), control over the speed of ambulation, and allows one or more therapists to provide tactile cues or physical assist to achieve gait dynamics. The person can be unweighted by the suspension system, this reduces the amount of weight bearing through their lower limbs and gives the feeling of being lighter. Ambulation will therefore require less effort by the person during initial gait training sessions. Body weight can be slowly added back to the person's control as they progress through their BWSTT program. Skilled therapists can assist with limb advancement, heel strike, stance with knee control, and swing phases of gait with tactile cues. Upright posture can also be addressed with this treatment modality. The video below demonstrates how to setup a BSW treadmill system, handling techniques, and how to advance to suspension system to overground gait training.
Biofeedback[edit | edit source]
Forms of biofeedback have been in use in physical therapy for more than 50 years, where it is beneficial in the management of neuromuscular disorders. Biofeedback techniques have shown benefit when used as part of a physical therapy program for people with motor weakness or dysfunction after stroke. These methods are getting better at training for complex task-oriented activities like walking and grasping objects as technology continues to advance[12].
Functional Electrical Stimulation[edit | edit source]
Functional Electrical Stimulation (FES) is a useful modality for rehabilitation after stroke, and can supplement NMR and strengthening interventions. FES is used to elicit action potentials in the peripheral nerves of axonal branches and generate muscle contractions via surface electrodes placed over a muscle group. The intensity of contraction can be controlled by adjusting the amount of stimulus given by the FES machine. Use of this modality requires a strong understanding of anatomy for proper electrode placement. FES has been used in rehabilitation of chronic hemiplegia since the 1960s[1].
FES can be performed using a small handheld unit, a wearable unit, or integrated into a upper or lower extremity bicycle.
Robotic-Assisted Training[edit | edit source]
Stroke rehab requires hundreds of thousands of repetitions of a movement to cause permanent changes in the brain. New technology in the form of robotics can assist in achieving these numbers. Robotic devices provide safe, intensive and task-oriented rehabilitation to people with mild to severe neurologic injury. It provides: precisely controllable assistance or resistance during movements, good repeatability, objective and quantifiable measures of subject performance, and increased training motivation through the use of interactive biofeedback. Robotic-assisted training reduces the amount of physical assistance required to walk reducing health care costs, provides kinematic and kinetic data to control and quantify the intensity of practice, and measures changes and assess motor impairments with better sensitivity and reliability than standard clinical scales[13].
Conclusions[edit | edit source]
Following a stroke, gait recovery is often a primary goal for our patients. It is a symbol of their independence and returning to normal. Due to the complexity of ambulation, individualized intensive rehabilitation programs are necessary to optimize recovery. Estimating rehabilitation effects on motor recovery is complex, due to the interaction of spontaneous recovery and therapeutic interventions.
Treatment interventions to improve gait in persons with stroke range from physical hands-on cuing techniques, electrical stimulation, treadmill training, biofeedback, and robotics. New treatments are constantly being developed, adding to our treatment arsenal. It is often a combination of multiple treatment modalities and clinical experience and skill which lead to the best patient outcomes.
Additional Viewing[edit | edit source]
The video below demonstrates the phases of gait and shows an assessment of normal and common abnormal gait patterns.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Belda-Lois JM, Mena-del Horno S, Bermejo-Bosch I, Moreno JC, Pons JL, Farina D, Iosa M, Molinari M, Tamburella F, Ramos A, Caria A. Rehabilitation of gait after stroke: a review towards a top-down approach. Journal of neuroengineering and rehabilitation. 2011 Dec 1;8(1):66.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3261106/ (last accessed 5.2.2020)
- ↑ Hill K, Ellis P, Bernhardt Jet al. (1997) Balance and mobility outcomes for stroke patients: a comprehensive audit. Aust J Physiother, 43, 173-180.
- ↑ Forssberg H (1982) Spinal locomotion functions and descending control. In Brain Stem Control of Spinal Mechanisms (eds B Sjolund, A Bjorklund), Elsevier Biomedical Press,New York.
- ↑ Li S, Francisco GE, Zhou P. Post-stroke hemiplegic gait: new perspective and insights. Frontiers in physiology. 2018;9:1021. Available from: https://www.frontiersin.org/articles/10.3389/fphys.2018.01021/full (last accessed 29.11.2019)
- ↑ Balaban, Birol et al.:Gait Disturbances in Patients With Stroke : PM&R , Volume 6 , Issue 7 , 635 - 642
- ↑ H Hayes Hospital Physical Therapy Restores Walking After Stroke Available from: https://www.youtube.com/watch?v=g__BYaS9viw (last accessed 29.11.2019)
- ↑ 7.0 7.1 7.2 Janet H Carr EdD FACP , Roberta B Shepherd EdD FACP; Stroke Rehabilitation- Guidelil1es for Exercise and Training to Optimize Motor Skill ; First edition; 2003
- ↑ Hemiplegic Gait – Case Study 13 Available from: https://www.youtube.com/watch?v=ihz74Zv6D84 (last accessed 23.10.2021)
- ↑ Janice J Eng, PhD, PT/OT, Professor and Pei Fang Tang, PhD, PT ;Gait training strategies to optimize walking ability in people with stroke: A synthesis of the evidence; Expert Rev Neurother. Oct 2007; 7(10): 1417–1436.
- ↑ Lennon S, Baxter D, Ashburn A. Physiotherapy based on the Bobath concept in stroke rehabilitation: a survey within the UK. Disabil Rehabil. 2001;23(6):254–262.
- ↑ Body Weight Supported Treadmill Available from: https://www.youtube.com/watch?v=tq1_PDtTpd4 last accessed 23.10.2021)
- ↑ Malik K, Dua A. Biofeedback. [Updated 2019 Dec 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553075/
- ↑ Juan-Manuel Belda-Lois et al; Rehabilitation of gait after stroke: a review towards a top-down approach ;Journal of NeuroEngineering and Rehabilitation 2011, 8:66
- ↑ Watch a robotic exoskeleton help a stroke patient walk Available from: https://www.youtube.com/watch?v=KWLgfP2ndes last accessed 24.10.2021)
- ↑ Gait Assessment – normal gait and common abnormal gaits Available from: https://www.youtube.com/watch?v=PZBiv0uSXVg last accessed 24.10.2021)