Breast Cancer Patients - Musculoskeletal Problems Experienced: Difference between revisions
Chloe Waller (talk | contribs) (Updated introduction) |
Chloe Waller (talk | contribs) (Updated post-mastectomy pain syndrome and added physiotherapy management. Added links, picture and references) |
||
| Line 5: | Line 5: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
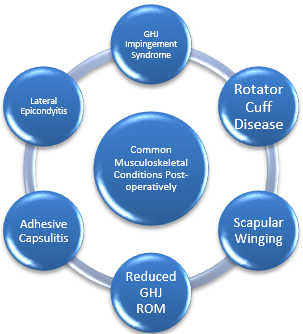
[[Breast Cancer|Breast cancer]] and its' treatment, usually localised surgery with [[Chemotherapy Side Effects and Syndromes|chemotherapy]], radiotherapy and [[Endocrine System|endocrine]] therapy, increase the risk of [[Musculoskeletal Orthopaedic Assessment|musculoskeletal]] problems, especially in the upper limb<ref>Richmond H et al, [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6006920/ PROSPER Study Group. Development of an exercise intervention for the prevention of musculoskeletal shoulder problems after breast cancer treatment: the prevention of shoulder problems trial (UK PROSPER).] BMC Health Serv Res. 2018 Jun 18;18(1):463</ref>. Research suggests 67% of women may have shoulder or arm problems up to 3 years after treatment<ref name=":1">Bruce J, Williamson E, Lait C on behalf of the PROSPER Study Group'', et al.'' [https://bmjopen.bmj.com/content/8/3/e019078 Randomised controlled trial of exercise to prevent shoulder problems in women undergoing breast cancer treatment: study protocol for the prevention of shoulder problems trial (UK PROSPER).] BMJ Open 2018;8''':'''e019078</ref>.[[File:MSK conditions group1.png|right|frameless|334x334px]] | |||
[[Breast Cancer|Breast cancer]] and its treatment, usually localised surgery with [[Chemotherapy Side Effects and Syndromes|chemotherapy]], radiotherapy and [[Endocrine System|endocrine]] therapy, increase the risk of [[Musculoskeletal Orthopaedic Assessment|musculoskeletal]] problems, especially in the upper limb<ref>Richmond H et al, [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6006920/ PROSPER Study Group. Development of an exercise intervention for the prevention of musculoskeletal shoulder problems after breast cancer treatment: the prevention of shoulder problems trial (UK PROSPER).] BMC Health Serv Res. 2018 Jun 18;18(1):463</ref>. Research suggests 67% of women may have shoulder or arm problems up to 3 years after treatment<ref name=":1">Bruce J, Williamson E, Lait C on behalf of the PROSPER Study Group'', et al.'' [https://bmjopen.bmj.com/content/8/3/e019078 Randomised controlled trial of exercise to prevent shoulder problems in women undergoing breast cancer treatment: study protocol for the prevention of shoulder problems trial (UK PROSPER).] | |||
== Musculoskeletal Conditions == | |||
* Acute or chronic [[Pain Assessment|pain]]<ref name=":2">Ballinger TJ, Thompson WR, Guise TA. [https://pubmed.ncbi.nlm.nih.gov/36419084/ The bone-muscle connection in breast cancer: implications and therapeutic strategies to preserve musculoskeletal health.] Breast Cancer Res. 2022 Nov 23;24(1):84.</ref> | * Acute or chronic [[Pain Assessment|pain]]<ref name=":2">Ballinger TJ, Thompson WR, Guise TA. [https://pubmed.ncbi.nlm.nih.gov/36419084/ The bone-muscle connection in breast cancer: implications and therapeutic strategies to preserve musculoskeletal health.] Breast Cancer Res. 2022 Nov 23;24(1):84.</ref> | ||
* [[Muscle]] weakness<ref name=":2" /> | *[[Muscle]] weakness<ref name=":2" /> | ||
* [[Osteoporosis]] and osteoporotic [[Osteoporotic Vertebral Fractures|fractures]] - certain treatments, such as aromatase inhibitors, or chemotherapy-induced [[Ovarian Cancer|ovarian]] failure, decrease [[estrogen]] and lead to [[bone]] loss<ref>Suskin J, Shapiro CL. [https://pubmed.ncbi.nlm.nih.gov/30175057/ Osteoporosis and musculoskeletal complications related to therapy of breast cancer.] Gland Surg. 2018 Aug;7(4):411-423. </ref> | * [[Osteoporosis]] and osteoporotic [[Osteoporotic Vertebral Fractures|fractures]] - certain treatments, such as aromatase inhibitors, or chemotherapy-induced [[Ovarian Cancer|ovarian]] failure, decrease [[estrogen]] and lead to [[bone]] loss<ref>Suskin J, Shapiro CL. [https://pubmed.ncbi.nlm.nih.gov/30175057/ Osteoporosis and musculoskeletal complications related to therapy of breast cancer.] Gland Surg. 2018 Aug;7(4):411-423. </ref> | ||
* Reduced | * Reduced shoulder [[Range of Motion|range of motion]]<ref name=":1" />due to pain or fear of movement leading to adapting a flexed protective [[posture]] or avoidance of use, leading to muscles shortening (especially [[pectoralis major]]) and tightening of the joint capsule.<ref name=":3">Ebaugh, D., Spinelli, B. and Schmitz, K.H. [https://www.sciencedirect.com/science/article/abs/pii/S0306987711002738 Shoulder impairments and their association with symptomatic rotator cuff disease in breast cancer survivors.] 2011. Medical Hypotheses. Vol. 77, p.481–487.</ref> | ||
* Secondary to above, there is risk of shoulder conditions such as symptomatic [[Rotator Cuff|rotator cuff]] disease | * Secondary to above, there is risk of shoulder conditions such as symptomatic [[Rotator Cuff|rotator cuff]] disease, [[Adhesive Capsulitis|adhesive capsulitis]] or shoulder [[Internal Impingement of the Shoulder|impingement]]<ref name=":3" /><ref name=":0">Pacurar R, Miclaus C, Miclaus M. [https://www.semanticscholar.org/paper/Morbidity-associated-with-breast-cancer-therapy-and-P%C4%83curar-Micl%C4%83u%C5%9F/f4430b180079722a7ad62803bb6e1f64d697cbae Morbidity associated with breast cancer therapy and the place of physiotherapy in its management.] Timisoara Physical Education & Rehabilitation Journal 2011 05;3(6):46-54.</ref> | ||
* [[Lymphoedema]]<ref>Rafn BS, Christensen J, Larsen A, Bloomquist K. [https://pubmed.ncbi.nlm.nih.gov/35077194/ Prospective Surveillance for Breast Cancer-Related Arm Lymphedema: A Systematic Review and Meta-Analysis]. J Clin Oncol. 2022 Mar 20;40(9):1009-1026.</ref> | * [[Lateral Epicondyle Tendinopathy (Tennis Elbow) Toolkit|Lateral epicondylitis]]<ref>Stubblefield MD, Custodio CM. [https://www.archives-pmr.org/article/S0003-9993(05)01487-5/fulltext Upper-extremity pain disorders in breast cancer.] Physical Medicine and Rehabiliation. 2006. 87; 3: 96-99</ref> | ||
*[[Lymphoedema]]<ref>Rafn BS, Christensen J, Larsen A, Bloomquist K. [https://pubmed.ncbi.nlm.nih.gov/35077194/ Prospective Surveillance for Breast Cancer-Related Arm Lymphedema: A Systematic Review and Meta-Analysis]. J Clin Oncol. 2022 Mar 20;40(9):1009-1026.</ref> | |||
* [[Scapular Winging|Scapula winging]] may occur as a result of exposing the [[Long Thoracic Nerve|long thoracic nerve]] during axillary surgeries<ref>Plaza Meza MP, Marín Fermín T, Maffulli N. [https://academic.oup.com/bmb/article/140/1/23/6361051?login=false Diagnosis and epidemiology of winged scapula in breast cancer patients: A systematic review and meta-analysis.] Br Med Bull. 2021 Dec 16;140(1):23-35</ref> | |||
* Increased [[Body Mass Index|body mass index]] (BMI), which can lead to or exacerbate other musculoskeletal conditions<ref>Leclerc AF et al. [https://pubmed.ncbi.nlm.nih.gov/28322035/ Multidisciplinary rehabilitation program after breast cancer: benefits on physical function, anthropometry and quality of life.] Eur J Phys Rehabil Med. 2017 Oct;53(5):633-642. doi: 10.23736/S1973-9087.17.04551-8. Epub 2017 Mar 20</ref> | * Increased [[Body Mass Index|body mass index]] (BMI), which can lead to or exacerbate other musculoskeletal conditions<ref>Leclerc AF et al. [https://pubmed.ncbi.nlm.nih.gov/28322035/ Multidisciplinary rehabilitation program after breast cancer: benefits on physical function, anthropometry and quality of life.] Eur J Phys Rehabil Med. 2017 Oct;53(5):633-642. doi: 10.23736/S1973-9087.17.04551-8. Epub 2017 Mar 20</ref> | ||
* [[Scar Management|Scar]] adhesion<ref name=":0" /> | *[[Scar Management|Scar]] adhesion<ref name=":0" /> | ||
== Post-Mastectomy Pain Syndrome (PMPS) == | == Post-Mastectomy Pain Syndrome (PMPS) == | ||
Post-mastectomy pain syndrome (PMPS) is a neuropathic condition defined as pain located in the anterior surface of the chest, arm pit, [[shoulder]] or upper half of the arm that persists for longer than 3 months after surgery. The nature of PMPS is [[Inflammation Acute and Chronic|inflammatory]] and/or [[Neuropathic Pain|neuropathic pain]], possibly due to sensitization of peripheral nociceptors, neuroma formation and fibrotic [[Nerve Entrapment|entrapment]]. <ref>Yuksel SS, Chappell AG, Jackson BT, Wescott AB, Ellis MF. [https://www.sciencedirect.com/science/article/pii/S2352587821000966?via%3Dihub "Post Mastectomy Pain Syndrome: A Systematic Review of Prevention Modalities".] JPRAS Open. 2021 Oct 30;31:32-49. </ref> | |||
Treatments include physiotherapy, mindfulness-based [[Cognitive Behavioural Therapy|cognitive therapy]], oral medications, surgical intervention (fat grafting, neuroma or lymphedema surgery as required), anesthesia, nerve blocks and neurolysis, laser, neuromodulators and topical capsaicin. <ref>Chappell AG, Yuksel S, Sasson DC, Wescott AB, Connor LM, Ellis MF. [https://www.sciencedirect.com/science/article/pii/S235258782100067X?via%3Dihub Post-Mastectomy Pain Syndrome: An Up-to-Date Review of Treatment Outcomes.] JPRAS Open. 2021 Aug 11;30:97-109.</ref> | |||
== Physiotherapy Management == | |||
[[File:Breast Cancer Exercise Classes.jpg|right|frameless]] | |||
* | Physiotherapy intervention will be patient-specific, but can include: | ||
* Upper limb stretching<ref name=":4">Bruce J et al; [https://www.bmj.com/content/375/bmj-2021-066542.long Prevention of Shoulder Problems Trial (PROSPER) Study Group. Exercise versus usual care after non-reconstructive breast cancer surgery (UK PROSPER): multicentre randomised controlled trial and economic evaluation]. BMJ. 2021 Nov 10;375:e066542</ref> | |||
* Strengthening and [[Resistance exercises|resistance training]]<ref name=":5">Lahart IM, Metsios GS, Nevill AM, Carmichael AR. [https://pubmed.ncbi.nlm.nih.gov/29376559/ Physical activity for women with breast cancer after adjuvant therapy.] Cochrane Database Syst Rev. 2018 Jan 29;1(1):CD011292</ref> | |||
* [[Aerobic Exercise|Aerobic exercise]] for cardiovascular fitness<ref name=":5" /> | |||
* [[Yoga]] and complementary/ alternative medicine<ref>Olsson Möller U, Beck I, Rydén L, Malmström M. [https://pubmed.ncbi.nlm.nih.gov/31109309/ A comprehensive approach to rehabilitation interventions following breast cancer treatment - a systematic review of systematic reviews.] BMC Cancer. 2019 May 20;19(1):472. </ref> | |||
* [[Myofascial Release|Myofascial release]] <ref>Serra-Añó P, Inglés M, Bou-Catalá C, Iraola-Lliso A, Espí-López GV. [https://pubmed.ncbi.nlm.nih.gov/30470892/ Effectiveness of myofascial release after breast cancer surgery in women undergoing conservative surgery and radiotherapy: a randomized controlled trial.] Support Care Cancer. 2019 Jul;27(7):2633-2641.</ref> | |||
* [[Kinesio Taping]] and [[Manual Lymphatic Drainage|manual lymphatic drainage]] for lymphedema<ref>Kasawara KT, Mapa JMR, Ferreira V, Added MAN, Shiwa SR, Carvas N Jr, Batista PA. [https://pubmed.ncbi.nlm.nih.gov/29308967/ Effects of Kinesio Taping on breast cancer-related lymphedema: A meta-analysis in clinical trials.] Physiother Theory Pract. 2018 May;34(5):337-345. </ref> | |||
=== Evidence === | |||
Overall, evidence supports exercise for breast cancer patients to improve physical and mental health. | |||
One controlled trial of 209 patients comparing a three-month rehabilitation program of physical training and psycho-educational sessions to usual care found improvements in [[Sit and Reach Test]], maximal incremental exercise test, [[Six Minute Walk Test / 6 Minute Walk Test|Six-Minute Walk Test]], BMI and body fat percentage and the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30.<ref>Leclerc AF et al. M[https://pubmed.ncbi.nlm.nih.gov/28322035/ ultidisciplinary rehabilitation program after breast cancer: benefits on physical function, anthropometry and quality of life.] Eur J Phys Rehabil Med. 2017 Oct;53(5):633-642. </ref> | |||
A self-completed questionnaire completed by 94 women who had had breast cancer found increased physical activity habits and physiotherapy treatments contributed for the perception of lower number of musculoskeletal disorders.<ref>Rangel J, Tomás MT, Fernandes B. [https://pubmed.ncbi.nlm.nih.gov/30361831/ Physical activity and physiotherapy: perception of women breast cancer survivors.] Breast Cancer. 2019 May;26(3):333-338.</ref> | |||
The UK PROSPER trial assessed 392 women undergoing breast cancer surgery at 17 UK NHS cancer centres, and found an exercise program to be clinically and cost effective. Patients were randomised to either usual care (information leaflets) or usual care plus a physiotherapy programme (with [[stretching]], strengthening, physical activity, and [[Behaviour Change|behaviour change]] techniques for exercise adherence). Upper limb function improved after exercise compared with usual care (mean [[DASH Outcome Measure|Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire]] 16.3 (SD 17.6) for exercise (n=132); 23.7 (22.9) usual care (n=138); adjusted mean difference 7.81, 95% confidence interval 3.17 to 12.44; P=0.001). Moreover at 12 months there was lower adjusted mean difference on [[Numeric Pain Rating Scale|numerical rating scale]] (P=0.02) and less arm disability symptoms (P=0.001). There was no increase in complications or adverse events in the exercise group.<ref name=":4" /> | |||
== References == | == References == | ||
Revision as of 14:58, 12 May 2023
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Chloe Waller and Kim Jackson
Introduction[edit | edit source]
Breast cancer and its' treatment, usually localised surgery with chemotherapy, radiotherapy and endocrine therapy, increase the risk of musculoskeletal problems, especially in the upper limb[1]. Research suggests 67% of women may have shoulder or arm problems up to 3 years after treatment[2].
Musculoskeletal Conditions[edit | edit source]
- Acute or chronic pain[3]
- Muscle weakness[3]
- Osteoporosis and osteoporotic fractures - certain treatments, such as aromatase inhibitors, or chemotherapy-induced ovarian failure, decrease estrogen and lead to bone loss[4]
- Reduced shoulder range of motion[2]due to pain or fear of movement leading to adapting a flexed protective posture or avoidance of use, leading to muscles shortening (especially pectoralis major) and tightening of the joint capsule.[5]
- Secondary to above, there is risk of shoulder conditions such as symptomatic rotator cuff disease, adhesive capsulitis or shoulder impingement[5][6]
- Lateral epicondylitis[7]
- Lymphoedema[8]
- Scapula winging may occur as a result of exposing the long thoracic nerve during axillary surgeries[9]
- Increased body mass index (BMI), which can lead to or exacerbate other musculoskeletal conditions[10]
- Scar adhesion[6]
Post-Mastectomy Pain Syndrome (PMPS)[edit | edit source]
Post-mastectomy pain syndrome (PMPS) is a neuropathic condition defined as pain located in the anterior surface of the chest, arm pit, shoulder or upper half of the arm that persists for longer than 3 months after surgery. The nature of PMPS is inflammatory and/or neuropathic pain, possibly due to sensitization of peripheral nociceptors, neuroma formation and fibrotic entrapment. [11]
Treatments include physiotherapy, mindfulness-based cognitive therapy, oral medications, surgical intervention (fat grafting, neuroma or lymphedema surgery as required), anesthesia, nerve blocks and neurolysis, laser, neuromodulators and topical capsaicin. [12]
Physiotherapy Management[edit | edit source]
Physiotherapy intervention will be patient-specific, but can include:
- Upper limb stretching[13]
- Strengthening and resistance training[14]
- Aerobic exercise for cardiovascular fitness[14]
- Yoga and complementary/ alternative medicine[15]
- Myofascial release [16]
- Kinesio Taping and manual lymphatic drainage for lymphedema[17]
Evidence[edit | edit source]
Overall, evidence supports exercise for breast cancer patients to improve physical and mental health.
One controlled trial of 209 patients comparing a three-month rehabilitation program of physical training and psycho-educational sessions to usual care found improvements in Sit and Reach Test, maximal incremental exercise test, Six-Minute Walk Test, BMI and body fat percentage and the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30.[18]
A self-completed questionnaire completed by 94 women who had had breast cancer found increased physical activity habits and physiotherapy treatments contributed for the perception of lower number of musculoskeletal disorders.[19]
The UK PROSPER trial assessed 392 women undergoing breast cancer surgery at 17 UK NHS cancer centres, and found an exercise program to be clinically and cost effective. Patients were randomised to either usual care (information leaflets) or usual care plus a physiotherapy programme (with stretching, strengthening, physical activity, and behaviour change techniques for exercise adherence). Upper limb function improved after exercise compared with usual care (mean Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire 16.3 (SD 17.6) for exercise (n=132); 23.7 (22.9) usual care (n=138); adjusted mean difference 7.81, 95% confidence interval 3.17 to 12.44; P=0.001). Moreover at 12 months there was lower adjusted mean difference on numerical rating scale (P=0.02) and less arm disability symptoms (P=0.001). There was no increase in complications or adverse events in the exercise group.[13]
References[edit | edit source]
- ↑ Richmond H et al, PROSPER Study Group. Development of an exercise intervention for the prevention of musculoskeletal shoulder problems after breast cancer treatment: the prevention of shoulder problems trial (UK PROSPER). BMC Health Serv Res. 2018 Jun 18;18(1):463
- ↑ 2.0 2.1 Bruce J, Williamson E, Lait C on behalf of the PROSPER Study Group, et al. Randomised controlled trial of exercise to prevent shoulder problems in women undergoing breast cancer treatment: study protocol for the prevention of shoulder problems trial (UK PROSPER). BMJ Open 2018;8:e019078
- ↑ 3.0 3.1 Ballinger TJ, Thompson WR, Guise TA. The bone-muscle connection in breast cancer: implications and therapeutic strategies to preserve musculoskeletal health. Breast Cancer Res. 2022 Nov 23;24(1):84.
- ↑ Suskin J, Shapiro CL. Osteoporosis and musculoskeletal complications related to therapy of breast cancer. Gland Surg. 2018 Aug;7(4):411-423.
- ↑ 5.0 5.1 Ebaugh, D., Spinelli, B. and Schmitz, K.H. Shoulder impairments and their association with symptomatic rotator cuff disease in breast cancer survivors. 2011. Medical Hypotheses. Vol. 77, p.481–487.
- ↑ 6.0 6.1 Pacurar R, Miclaus C, Miclaus M. Morbidity associated with breast cancer therapy and the place of physiotherapy in its management. Timisoara Physical Education & Rehabilitation Journal 2011 05;3(6):46-54.
- ↑ Stubblefield MD, Custodio CM. Upper-extremity pain disorders in breast cancer. Physical Medicine and Rehabiliation. 2006. 87; 3: 96-99
- ↑ Rafn BS, Christensen J, Larsen A, Bloomquist K. Prospective Surveillance for Breast Cancer-Related Arm Lymphedema: A Systematic Review and Meta-Analysis. J Clin Oncol. 2022 Mar 20;40(9):1009-1026.
- ↑ Plaza Meza MP, Marín Fermín T, Maffulli N. Diagnosis and epidemiology of winged scapula in breast cancer patients: A systematic review and meta-analysis. Br Med Bull. 2021 Dec 16;140(1):23-35
- ↑ Leclerc AF et al. Multidisciplinary rehabilitation program after breast cancer: benefits on physical function, anthropometry and quality of life. Eur J Phys Rehabil Med. 2017 Oct;53(5):633-642. doi: 10.23736/S1973-9087.17.04551-8. Epub 2017 Mar 20
- ↑ Yuksel SS, Chappell AG, Jackson BT, Wescott AB, Ellis MF. "Post Mastectomy Pain Syndrome: A Systematic Review of Prevention Modalities". JPRAS Open. 2021 Oct 30;31:32-49.
- ↑ Chappell AG, Yuksel S, Sasson DC, Wescott AB, Connor LM, Ellis MF. Post-Mastectomy Pain Syndrome: An Up-to-Date Review of Treatment Outcomes. JPRAS Open. 2021 Aug 11;30:97-109.
- ↑ 13.0 13.1 Bruce J et al; Prevention of Shoulder Problems Trial (PROSPER) Study Group. Exercise versus usual care after non-reconstructive breast cancer surgery (UK PROSPER): multicentre randomised controlled trial and economic evaluation. BMJ. 2021 Nov 10;375:e066542
- ↑ 14.0 14.1 Lahart IM, Metsios GS, Nevill AM, Carmichael AR. Physical activity for women with breast cancer after adjuvant therapy. Cochrane Database Syst Rev. 2018 Jan 29;1(1):CD011292
- ↑ Olsson Möller U, Beck I, Rydén L, Malmström M. A comprehensive approach to rehabilitation interventions following breast cancer treatment - a systematic review of systematic reviews. BMC Cancer. 2019 May 20;19(1):472.
- ↑ Serra-Añó P, Inglés M, Bou-Catalá C, Iraola-Lliso A, Espí-López GV. Effectiveness of myofascial release after breast cancer surgery in women undergoing conservative surgery and radiotherapy: a randomized controlled trial. Support Care Cancer. 2019 Jul;27(7):2633-2641.
- ↑ Kasawara KT, Mapa JMR, Ferreira V, Added MAN, Shiwa SR, Carvas N Jr, Batista PA. Effects of Kinesio Taping on breast cancer-related lymphedema: A meta-analysis in clinical trials. Physiother Theory Pract. 2018 May;34(5):337-345.
- ↑ Leclerc AF et al. Multidisciplinary rehabilitation program after breast cancer: benefits on physical function, anthropometry and quality of life. Eur J Phys Rehabil Med. 2017 Oct;53(5):633-642.
- ↑ Rangel J, Tomás MT, Fernandes B. Physical activity and physiotherapy: perception of women breast cancer survivors. Breast Cancer. 2019 May;26(3):333-338.