Long Thoracic Nerve
Original Editor - Ankit Shah
Top Contributors - Ankit Shah, Wendy Snyders and Rahma Ahmed Ahmed Bahbah
Description[edit | edit source]
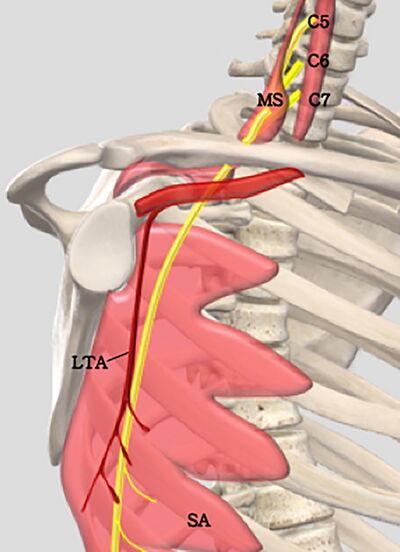
The long thoracic nerve is also known as the external respiratory nerve of Bell or the posterior thoracic nerve[1]. It originates from the superior trunk of the brachial plexus after which it descends posterior to the brachial plexus and anterior to the posterior scalene muscle. It passes over the chest wall and lies on the superficial surface of the serratus anterior muscle[1][2]. The long (22-24cm) and superficial course of this nerve makes it susceptible to various injuries[1]. The long thoracic nerve has an upper (C5 and C6 ) and lower portion (C7) which fuse in the axilla[1][2].
Root[edit | edit source]
The long thoracic nerve originates at the anterior ramii of C5, C6, C7[1][2].
In a small percentage of population the long thoracic nerve receives contributions from C4 (5%) [2]and C8 (10%)[1][2] nerve roots as well.
Function[edit | edit source]
Motor function
The long thoracic nerves solely innervates the serratus anterior muscle which is primarily responsible for shoulder protraction. It also works with trapezius to provide sustained upward rotation of scapula which is needed for overhead lifting[1].
Injury to the Long thoracic nerve[edit | edit source]
Injury to long thoracic nerve can cause weakness of the serratus anterior muscle and dynamic winging of scapula[1][2].
There are various causes for injury to long thoracic nerve but they can be mainly divided into 3 categories i.e. non-traumatic, traumatic and iatrogenic.
Non-traumatic:
- viral illness (influenza)[4]
- tonsillitis-bronchitis[4]
- poliomyelitis[4]
- allergic drug reactions[4]
- muscular dystrophy (facio-scapulohumeral dystrophy)[4]
- Parsonage-Turner syndrome[2]
Traumatic:
- clavicle or upper rib fractures[2]
- sudden scapular depression[4]
- repetitive arm movements as seen in athletes[4](especially in athletes where arm abduction and external rotation is combined with contralateral neck and neck movement e.g. javelin[2])
- house-hold activities such as digging, car washing or prolonged lying in bed with arm abducted and propping up the head to read[4]
Iatrogenic injury:
Treatment[edit | edit source]
Long thoracic nerve trauma from a direct insult to the shoulder or lateral chest wall is more severe and recovery is limited. If there was not experience recovery, the patiebt may be candidate for surgical intervention. There are reports about successful treatment with nerve transfer utilizing the thoracodorsal or medial pectoral nerves.[1]
For more information about rehabilitation, you can check nerve injury rehabilitation
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Lung K, Lui F. Anatomy, Thorax, Long Thoracic Nerve. [Updated 2020 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535396/
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 Bilfeld MF, Lapègue F, Cintas P, Acket B, Basselerie H, Bachour R, Nougarolis F, Ricard C, Gandois HC, Laumonerie P, Aprodoaei C. Ultrasonographic anatomy of the long thoracic nerve: A reappraisal using high frequency (24-MHz) probe. Diagnostic and Interventional Imaging. 2021 Apr 1;102(4):241-5.
- ↑ Bilfeld MF, Lapègue F, Cintas P, Acket B, Basselerie H, Bachour R, Nougarolis F, Ricard C, Gandois HC, Laumonerie P, Aprodoaei C. Ultrasonographic anatomy of the long thoracic nerve: A reappraisal using high frequency (24-MHz) probe. Diagnostic and Interventional Imaging. 2021 Apr 1;102(4):241-5.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 Martin RM, Fish DE. Scapular winging: anatomical review, diagnosis, and treatments. Curr Rev Musculoskelet Med. 2008;1(1):1-11. doi:10.1007/s12178-007-9000-5
- ↑ Murphy MT, Journeaux SF. Case reports: long thoracic nerve palsy after using a single axillary crutch. Clin Orthop Relat Res. 2006;447:267-269. doi:10.1097/01.blo.0000205880.27964.a3