Anatomy of the Pelvic Girdle
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (14/11/2020)
Original Editor - User Name
Top Contributors - Wanda van Niekerk, Kim Jackson, Tarina van der Stockt, Lucinda hampton, Vidya Acharya and Olajumoke Ogunleye
Introduction[edit | edit source]
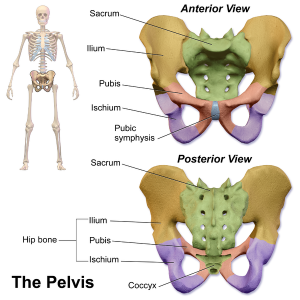
The term "pelvis" is used to identify the area between the abdomen and the lower extremities. It can be divided into the greater pelvis and the lesser pelvis.[1] The pelvis consists of the sacrum, the coccyx, the ischium, the ilium, and the pubis.[2][3] The structure of the pelvis supports the contents of the abdomen while also helping to transfer the weight from the spine to the lower limbs.[4] During gait, the joints within the pelvis work together to decrease the amount of force transferred from the ground and lower extremities to the spine and upper extremities.[4]
Osteology of the Pelvis[edit | edit source]
The pelvic bones are[1]:
- Sacrum
- Coccyx
- Two innominate bones, which consist of the:
- Ischium
- Ilium
- Pubis[2]
- The inlet to the pelvic canal is at the level of the sacral promontory and superior aspect of the pubic bones.
- The outlet is formed by the pubic arch, ischial spines, sacrotuberous ligaments, and the coccyx.
- The enclosed space between the inlet and outlet is called the true pelvis, with the plane of the inlet being at right angles to the plane of the outlet.
- The female true pelvis differs from the male in being shallower, having straighter sides, a wider angle between the pubic rami at the symphysis, and a proportionately larger pelvic outlet.
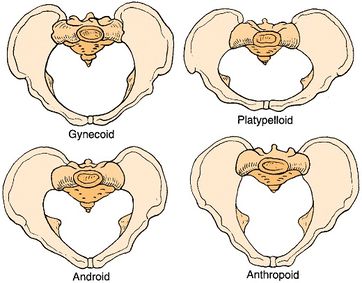
- The shape of the female bony pelvis can be classified into four broad categories: gynecoid, anthropoid, android, and platypelloid[3].
- Gynecoid/genuine pelvis
- the brim is round, more wider, and both ischial spines are less prominent this allows easy baby delivery.
- Android pelvis
- like a heart-shaped brim with narrow pelvic cavity than presented in gynecoid one, get narrower at the supra-pubic arch, and both ischial spines are prominent. During delivery, she needs to take an active role.
- Anthropoid pelvis
- oval brim, slightly narrower pelvic cavity than above with larger outlet diameter.
- Platypelloid pelvis
- shallow pelvic cavity, and decreased antero-posterior diameter, broad outlet, during labour there will be difficult for the baby to enter the pelvis at the beginning.
- Gynecoid/genuine pelvis
- In women, the pelvis houses the uterus, tubes, ovaries and vagina.
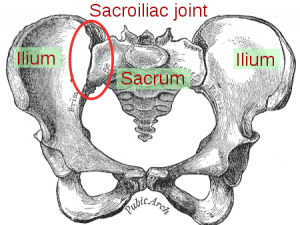
Joint Articulations[edit | edit source]
There are three articulations within the pelvis[7]:
- Inferiorly between the sacrum and the coccyx
- Posteriorly between the sacrum and each ilium (sacroiliac (SI) joint)
- Anteriorly between the pubic bodies (pubic symphysis)[3]
Other articulations:
The pelvis and femur articulate via the acetabulum[2]
Symphysis Pubis Joint[edit | edit source]
- non-synovial amphi-arthrodial joint
- inter-pubic fibrocartilage disc
- less form closure than sacro-iliac joint
Sacroiliac Joint[edit | edit source]
- diarthrodial joint[9][10]
- held together by fibrous capsule and synovial fluid[9]
- slightly moveable joint[9]
For more information on the sacroiliac joint, read this Physiopedia page: Sacroiliac Joint
[11]Sacrococcygeal Joint[edit | edit source]
- at apex of sacrum and coccyx
- amphiarthrodial joint between the base of the coccyx (concave) and the sacral apex (convex)
- Synovium present occasionally
- sacrococcygeal disc present
- slightly moveable joint, but movement decreases with age
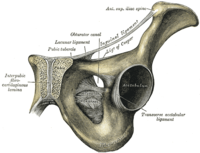
Ligaments of the Pelvis[edit | edit source]
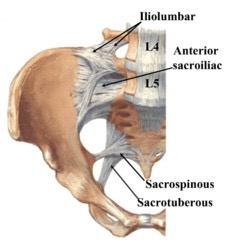
Iliolumbar Ligament[edit | edit source]
- from the tip of the transverse process of L5 to posterior aspect of the inner lip of iliac crest[7]
- 2 main bands attach to the pelvis
- Lower band - attaches to base of sacrum, contiguous with anterior sacroiliac ligament
- Upper band - attaches to iliac crest anterior to sacro-iliac articulation, contiguous with lumbodorsal fascia
- Strengthens the lumbo-sacral joint
- Anterior relationship with psoas major
- Posterior relationship with muscles in vertebral groove such a multifidus and erector spinae
- Superior relationship with quadratus lumborum
Lateral Lumbosacral Ligament[edit | edit source]
- partially continuous with lower border or iliolumbar ligament
- from the lower border of L5 transverse process to the ala of the sacrum[7]
- intermingles with anterior sacroiliac ligament
- consists of bundles of fibres of varying strength
Ischio-sacral Ligaments[edit | edit source]
- Sacrotuberous Ligament
- from sacrum to tuberosity of the ischium[7]
- PSIS to the 4th and 5th transversus tubercle of the sacrum and the lateral inferior border of the sacrum and coccyx
- free concave border is attachment for obturator fascia
- directly continuous with the long head of biceps femoris
- posterior surface of ligament is also origin of gluteus maximus
- Sacrospinous Ligament
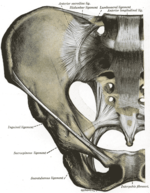
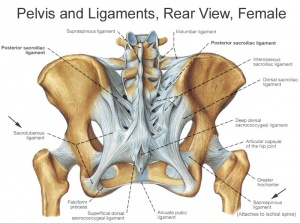
Sacroiliac Ligaments[edit | edit source]
- Ventral/Anterior sacroiliac ligament[13]
- from antero-lateral aspect of the sacrum to auricular surface of the ilium
- Dorsal/Posterior sacroiliac ligament[13]
- The upper portion (short posterior sacroiliac ligament) - from 1st and 2nd transverse tubercles of the sacrum to the tuberosity of ilium
- The lower portion (long posterior sacroiliac ligament) - from 3rd transverse tubercle of the sacrum to the posterior superior iliac spine (PSIS)
- Interosseous sacroiliac ligament- lies deep to posterior SI ligament and runs between the tuberosities of the sacrum and ilium[13]
Sacrococcygeal Ligaments[edit | edit source]
- Ventral/Anterior sacrococcygeal ligament[7]
- from the anterior surface of sacrum to the front of the coccyx; continuation of the anterior longitudinal ligament of the spine
- Dorsal sacrococcygeal ligament[7]
- Deep portion - from the inside sacral canal at the 5th sacral segment to the dorsal surface of the coccyx; continuation of the posterior longitudinal ligament of the spine
- Superficial portion - from free margin of sacral hiatus to dorsal surface of the coccyx; corresponds with the ligamentum flavum of the spine
- Lateral sacrococcygeal ligament
- from the inferior lateral angle of the sacrum to the transverse process of the 1st coccygeal vertebra
Pubic Symphysis Ligaments[edit | edit source]
- Superior pubic ligament - runs between pubic tubercles[14]
- Inferior pubic ligament (aka arcuate pubic ligament) - runs between inferior pubic rami and blends with the fibrocartilaginous disc of the pubic symphysis[14]
- Anterior pubic ligament[14]
- Posterior pubic ligament - a membranous structure which blends with periosteum[14]
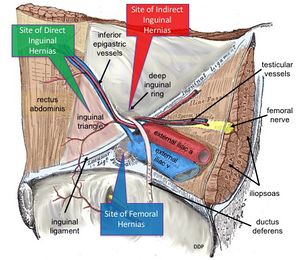
Inguinal Ligament[edit | edit source]
- runs from the ASIS to the pubic tubercle[15]
- formed by the aponeurosis of the external oblique
- continuous with fascia lata of the thigh
- Superficial inguinal ring:
- exit of the inguinal canal
- inguinal nerve
- genitofemoral nerve
- spermatic cord (males)
- round ligament (females)
- palpable under normal conditions[16]
- dilated in athletic pubalgia
- inguinal hernia - abdominal contents may protrude through ring
- exit of the inguinal canal
Muscles of the Pelvis[edit | edit source]
There are 36 muscles that attach to the sacrum or innominates. The purpose of these muscles is primarily to provide stability to the joint not to produce movement.[18]
Muscles that attach to the sacrum or innominates are:
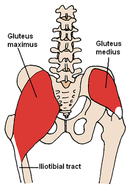
Muscles of the Hip[edit | edit source]
- Gluteus maximus
- primary stabilising muscle of the sacroiliac joint[19]
- often inhibited in people with low back pain, pelvic girdle pain or sacroiliac joint dysfunction[19][20]
- Gluteus medius
- Gluteus minimus
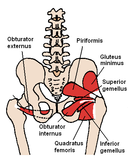
- Piriformis
- Superior gemellus
- Obturator Internus
- Inferior gemellus
- Quadratus femoris
- Iliopsoas
Pelvic Floor Myology [3][2][edit | edit source]
Layer One - Urogenital Triangle
- Bulbocavernosus
- Ischiocavernosus
- Superficial transverse perineal
- External anal sphincter
Layer Two - Urogenital Diaphragm
The urogenital diaphragm, also called the triangular ligament, is a strong, muscular membrane that occupies the area between the symphysis pubis and ischial tuberosities and stretches across the triangular anterior portion of the pelvic outlet. The urogenital diaphragm is external and inferior to the pelvic diaphragm.
- Urethral sphincter (sphincter urethrae)
- Compressor urethrae
- Sphincter urethral vaginalis
- Deep transverse perineal
- Perineal membrane
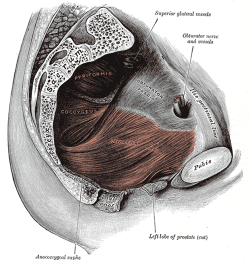
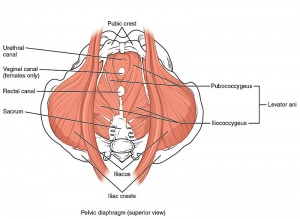
Layer Three - Pelvic Diaphragm
The pelvic diaphragm is a wide but thin muscular layer of tissue that forms the inferior border of the abdominopelvic cavity. Composed of a broad, funnel-shaped sling of fascia and muscle, it extends from the symphysis pubis to the coccyx and from one lateral sidewall to the other.
- Levator Ani Muscle (pubococcygeus aka pubovisceral, pubovaginalis, puboanalis, puborectalis, iliococcygeus)
- Coccygeus
- Piriformis
- Obturator internus
- Arcus tendinous of levator ani
- Arcus tendinous fasciae pelvis
Other muscles related to pelvic dysfunction
| [24] | [25] |
| Muscle | Origin | Insertion | Action | Innervation |
| Bulbospongiosus |
perineal body then divides to wrap around vagina |
fascia of corpus cavernosa |
empties urethra, acts as a sphincter to reduce lumen of vagina and assists erection of clitoris |
Deep branch of perineal nerve (branch of pudendal nerve) |
| Ischiocavernosus | Ischial ramus and tuberosity | Crus of penis or clitoris | Maintains erection of penis or clitoris by compression of outflow veins | Deep branch of perineal nerve (branch of pudendal nerve) |
| Superficial transverse perineal | Ischial tuberosity | Perineal body | Reinforces action of deep transverse perineal muscle to stabilize perineal body | Deep branch of perineal nerve (branch of pudendal nerve) |
| External anal sphincter | Perineal body and encircles anal canal |
Coccyx | Part of voluntary sphincter of anal canal | Inferior rectal (anal) nerve |
| Sphincter urethrae | Inferior aspect of pubic ramus and ischial tuberosity | Surrounds urethra; in females, some fibres also enclose the vagina | Controls flow of urine through urethra; also compresses vagina in females | Deep branch of perineal nerve (branch of pudendal nerve) |
|
Compressor urethrae (only in females) |
Ischiopubic ramus |
Vaginal wall |
Compresses ventral wall of the urethra |
|
|
Sphincter urethral vaginalis (only in females) |
Vaginal walls |
Ventral surface of urethra |
Compresses ventral wall of the urethra |
|
| Deep transverse perineal | Inner aspect of ischiopubic ramus | Median raphe (male), perineal body and external anal sphincter | Fixes perineal body, supports the function of levator ani and sphincter urethra |
Deep branch of perineal nerve (branch of pudendal nerve) |
| Perineal membrane (fascial thickening, not a muscle) | Fasical attachments at pubic symphysis | Fascial attachments at ischial spine | Suspensory ligament that provides extra support to prevent descent of perineal body |
|
| Levator Ani (Pubococcygeus) | Dorsal surface of pubis and fascia of obturator internus |
Anococcygeal body between tip of coccyx and the anal canal |
Voluntary spincter of the anal canal |
Nerve to levator ani (branches of S4), inferior rectal nerve (from pudendal nerve - S3, S4), coccygeal plexus |
| Levator Ani (Puborectalis) | Dorsal surface of pubis and fascia of obturator internus | Unites with its partner to make a U-shaped sling around the rectum | Controls defecation by pulling anorectal junction forward | Nerve to levator ani (branches of S4), branch of pudendal nerve (S2-4) |
| Levator Ani (Pubovaginalis) | Nerve to levator ani (branches of S4), branch of pudendal nerve (S2-4) | |||
| Levator Ani (Iliococcygeus) | Posterior aspect of arcus tendineus levator ani and the ischial spine | Anococcygeal body and the coccyx | Helps to support pelvic viscera and lateral coccyx | Nerve to levator ani (branches of S4), inferior rectal nerve (from pudendal nerve - S3, S4), coccygeal plexus |
|
Ischiococcygeus* (Coccygeus) *some consider this more of a ligament than a muscle |
Ischial Spine | Lower two sacral and upper two coccygeal spinal segments, blends with sacrospinous ligament on its external surface | Supports pelvic viscera, flexion of coccyx, stabilizes sacro-iliac joint | Anterior rami of S4 and S5 |
| Piriformis | Pelvic surface of sacrum, passes through greater sciatic foramen |
Superior border of the greater trochanter of the femur |
Hip external rotation, assist with hip abduction if hip is flexed |
Anterior rami of S1 & S2 |
| Obturator Internus | Internal or pelvic surface of the obturator foramen |
Medial surface of the greater trochanter of the femur |
Hip external rotation, assists with hip abduction if hip is flexed |
Nerve to obturator internus (L5, S1, S2) |
| Arcus tendinous levator ani (fascial thickening, not a muscle) | Fasical attachments at pubic symphysis | Fascial attachments at ischial spine | Suspensory ligament that provides extra support to prevent descent of perineal body | |
| Arcus tendinous fasciae pelvis (fascial thickening, not a muscle) | Fasical attachments at pubic symphysis | Fascial attachments at ischial spine | Suspensory ligament that provides extra support to prevent descent of perineal body |
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 Madsen C, Gordon DA. Anatomy, Neuroanatomy, and Biomechanics of the Pelvis. InPelvic Floor Dysfunction and Pelvic Surgery in the Elderly 2017 (pp. 3-26). Springer, New York, NY.
- ↑ 2.0 2.1 2.2 2.3 White TD, Black MT, Folkens PA. Human osteology. Academic press; 2011.
- ↑ 3.0 3.1 3.2 3.3 Lewis CL, Laudicina NM, Khuu A, Loverro KL. The human pelvis: Variation in structure and function during gait. The Anatomical Record 2017;300(4):633-42.
- ↑ 4.0 4.1 Magee DJ. Orthopedic physical assessment. Elsevier Health Sciences; 2013.
- ↑ Anatomy Zone. Bones of the Pelvis. Available from: https://youtu.be/3v5AsAESg1Q [last accessed 07/11/2020]
- ↑ Kenhub Learn Human Anatomy. Bones of the Pelvis. Available from https://www.youtube.com/watch?v=yK-8ZwLFarc [last accessed 07/11/2020]
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Chaudhry SR, Hulaibi FA, Nahian A, Chaudhry K. Anatomy, Abdomen and Pelvis, Pelvis. StatPearls [Internet]. 2020 May 24.
- ↑ 3D Anatomy Lyon. Arthrology of the pelvis the symphysis pubis. Available from https://www.youtube.com/watch?v=Jkw-X6zOLVI&list=PL5uEMr5n9RPGx9IX9mKc-aMe-KwJCndSj&index=8. (last accessed 14 November 2020)
- ↑ 9.0 9.1 9.2 Kiapour A, Joukar A, Elgafy H, Erbulut DU, Agarwal AK, Goel VK. Biomechanics of the sacroiliac joint: anatomy, function, biomechanics, sexual dimorphism, and causes of pain. International journal of spine surgery. 2020 Feb 1;14(s1):S3-13.
- ↑ Wong M, Kiel J. Anatomy, Abdomen and Pelvis, Sacroiliac Joint. InStatPearls [Internet] 2019 Feb 6. StatPearls Publishing.
- ↑ 3D Anatomy Lyon. Arthrology of the pelvis the sacroiliac joint. Available from https://www.youtube.com/watch?v=FTYnuXy0y1s&list=PL5uEMr5n9RPGx9IX9mKc-aMe-KwJCndSj&index=7 (last accessed 14 November 2020)
- ↑ 3D Anatomy Lyon. Arthrology of the pelvis The sacrococcygeal joint. (last accessed 14 November 2020)
- ↑ 13.0 13.1 13.2 Poilliot AJ, Zwirner J, Doyle T, Hammer N. A Systematic Review of the Normal Sacroiliac Joint Anatomy and Adjacent Tissues for Pain Physicians. Pain physician. 2019 Jul;22(4):E247-74.
- ↑ 14.0 14.1 14.2 14.3 Mahadevan V. Anatomy of the pelvis. Surgery (Oxford). 2018 Jul 1;36(7):333-8.
- ↑ Miller HJ. Inguinal hernia: mastering the anatomy. Surgical Clinics. 2018 Jun 1;98(3):607-21.
- ↑ Myers T. Fascial Palpation. Palpation and Assessment in Manual Therapy. 2017.
- ↑ Health and Medicine. Pelvis Anatomy Tutorial (Ligaments). Available from https://www.youtube.com/watch?v=pskEkYof95w&t=293s. (last accessed 14 November 2020)
- ↑ Calvillo O, Skaribas I, Turnipseed J. Anatomy and pathophysiology of the sacroiliac joint. Current review of pain 2000;4(5):356-61.
- ↑ 19.0 19.1 Buckthorpe M, Stride M, Della Villa F. Assessing and treating gluteus maximus weakness–a clinical commentary. International journal of sports physical therapy. 2019 Jul;14(4):655.
- ↑ Klahsen O. Sacroiliac joint pain: Where are we now?. SURG Journal. 2019 Jun 20;11.
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 Lifshitz L, Sela SB, Gal N, Martin R, Klar MF. Iliopsoas the Hidden Muscle: Anatomy, Diagnosis, and Treatment. Current Sports Medicine Reports. 2020 Jun 1;19(6):235-43.
- ↑ Animated Anatomy. Hip Muscles - Lateral Rotator Group & Gluteus Muscles. Available from https://www.youtube.com/watch?v=YohBVpLMZ6g. (last accessed 14 November 2020)
- ↑ KenHub Learn Human Anatomy. Iliopsoas Muscle: Action / Function, Anatomy & Innervation - Human Anatomy | Kenhub. Available from https://www.youtube.com/watch?v=cHWjpQ06-cE (last accessed 14 November 2o20)
- ↑ Anatomy Zone. Pelvic Floor Part 1 - The Pelvic Diaphragm - 3D Anatomy Tutorial. Available from: http://www.youtube.com/watch?v=P3BBAMWm2Eo [last accessed 11/04/14]
- ↑ Anatomy Zone. Pelvic Floor Part 2 - Perineal Membrane and Deep Perineal Pouch - 3D Anatomy Tutorial. Available from: http://www.youtube.com/watch?v=q0Ax3rLFc6M[last accessed 11/04/14]