|
|
| (88 intermediate revisions by 5 users not shown) |
| Line 1: |
Line 1: |
| | <div class="editorbox"> '''Original Editor '''- [[User:Robin Tacchetti|Robin Tacchetti]] based on the course by [https://members.physio-pedia.com/course_tutor/daphne-xuan/ Daphne Xuan]<br> |
| | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> |
| | |
|
| |
|
| == Introduction == | | == Introduction == |
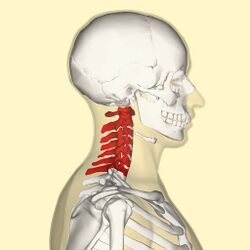
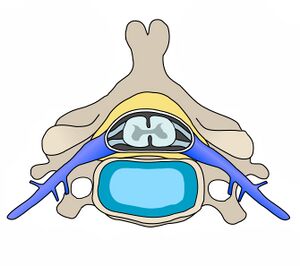
| The cervical spine supports and promotes movement of the head and neck. <ref>Frost BA, Camarero-Espinosa S, Foster EJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6356370/ Materials for the spine: anatomy, problems, and solutions]. Materials. 2019 Jan;12(2):253</ref> <ref name=":0">Kaiser JT, Lugo-Pico JG. [[Anatomy, Head and Neck, Cervical Vertebrae]]. 2019.</ref>The cervical spine is subjected to extrinsic factors such as repetitive movements, whole body vibrations and static load.<ref>Petersen JA, Brauer C, Thygesen LC, Flachs EM, Lund CB, Thomsen JF. [https://bmjopen.bmj.com/content/12/2/e053999 Prospective, population-based study of occupational movements and postures of the neck as risk factors for cervical disc herniation]. BMJ open. 2022 Feb 1;12(2):e053999.</ref> | | The cervical spine supports the weight of the head and enables head and neck movement.<ref>Frost BA, Camarero-Espinosa S, Foster EJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6356370/ Materials for the spine: anatomy, problems, and solutions]. Materials. 2019 Jan;12(2):253</ref> <ref name=":0">Kaiser JT, Reddy V, Lugo-Pico JG. Anatomy, Head and Neck: Cervical Vertebrae. [Updated 2022 Oct 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539734/</ref> Intervertebral discs maintain the spaces between the vertebrae. These discs act like shock absorbers throughout the spinal column to cushion the bones as the body moves. Ligaments hold the vertebrae in place, and tendons attach the muscles to the spinal column. The cervical spine is subjected to a range of extrinsic factors such as repetitive movements, whole-body vibrations and static load.<ref>Petersen JA, Brauer C, Thygesen LC, Flachs EM, Lund CB, Thomsen JF. [https://bmjopen.bmj.com/content/12/2/e053999 Prospective, population-based study of occupational movements and postures of the neck as risk factors for cervical disc herniation]. BMJ open. 2022 Feb 1;12(2):e053999.</ref>[[File:C-spine-picture.jpg|thumb|250x250px|Cervical spine]] |
| | |
| == Key Terms == | | == Key Terms == |
| [[Cardinal Planes and Axes of Movement|Axes]]: lines around which an object rotates. The rotation axis is a line that passes through the centre of mass. There are three axes of rotation: ''sagittal'' passing from posterior to anterior, ''frontal'' passing from left to right, and ''vertical'' passing from inferior to superior. The rotation axes of the foot joints are perpendicular to the cardinal planes. Therefore, motion at these joints results in rotations within three planes. Example: supination involves inversion, internal rotation, and plantarflexion. | | [[Cardinal Planes and Axes of Movement|Axes]]: lines around which an object rotates. The rotation axis is a line that passes through the centre of mass. There are three axes of rotation: ''sagittal'' passing from posterior to anterior, ''frontal'' passing from left to right, and ''vertical'' passing from inferior to superior. The rotation axes of the foot joints are perpendicular to the cardinal planes. Therefore, motion at these joints results in rotations within three planes. Example: supination involves inversion, internal rotation, and plantarflexion. |
|
| |
|
| [[Bursitis|Bursae]]: reduce friction between the moving parts of the body joints. A bursa is a fluid-filled sac. There are four types of bursae: adventitious, subcutaneous, [[/www.physio-pedia.com/Synovial Fluid Analysis|synovial]], and sub-muscular. | | [[Bursitis|Bursae]]: reduce friction between the moving parts of the body joints. A bursa is a fluid-filled sac. There are four types of bursae: adventitious, subcutaneous, [[Synovial Fluid Analysis|synovial]], and sub-muscular. |
|
| |
|
| [[Capsular and Non-Capsular Patterns|Capsule]]: one of the characteristics of the synovial joints. It is a fibrous connective tissue which forms a band that seals the joint space, provides passive and active stability and may even form articular surfaces for the joint. The capsular pattern is "the proportional motion restriction in range of motion during passive exercises due to tightness of the joint capsule." | | [[Capsular and Non-Capsular Patterns|Capsule]]: one of the characteristics of the synovial joints. It is a fibrous connective tissue which forms a band that seals the joint space, provides passive and active stability and may even form articular surfaces for the joint. The capsular pattern is "the proportional motion restriction in range of motion during passive exercises due to tightness of the joint capsule." |
|
| |
|
| Closed pack position: the position with the most congruency of the joint surfaces. In this position, joint stability increases. For example, the closed pack position for the interphalangeal joints is a full extension. | | Closed pack position: the position with the most congruency of the joint surfaces. In this position, joint stability increases. For example, the closed pack position for the interphalangeal joints is full extension. |
|
| |
|
| Degrees of freedom: the direction of joint movement or rotation; there is a maximum of six degrees of freedom, including three translations and three rotations. | | Degrees of freedom: the direction of joint movement or rotation; there is a maximum of six degrees of freedom, including three translations and three rotations. |
| Line 22: |
Line 24: |
| == Cervical Spine Structure == | | == Cervical Spine Structure == |
|
| |
|
| === '''Cervical vertebrae''' === | | === Cervical Vertebrae=== |
| There are seven lumbar vertebrae, which are known as C1-C7. Considering the small weight-bearing load of the cervical spine, large vertebral bodies are not required. In this section of the spine, vertebral size is not as important as range of motion. With increased range of motion and flexibility comes a heightened chance for injury of the spinal cord and its associated neurovascular structures.<ref name=":0" /> | | There are seven cervical vertebrae, which are known as C1-C7. Their role is to support the head and neck and to promote head movement. The cervical spine is only exposed to small weight-bearing loads. Therefore, the cervical vertebral bodies do not need to be large and "an increased range of motion takes priority over vertebral size and rigidity".<ref name=":0" /> However, because of this increased range of motion at the cervical spine, there is a heightened injury risk for the spinal cord and the associated neurovascular structures.<ref name=":0" /> |
|
| |
|
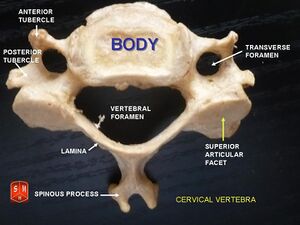
| * Vertebral body
| | The cervical vertebral bodies (C3-C6) have unique characteristics:<ref name=":0" /><ref name=":1">Teach me anatomy The cervical Spine Available from:https://teachmeanatomy.info/neck/bones/cervical-spine/</ref> |
| ** Triangular vertebral foramen
| |
| ** Bifid spinous process – spinous process splits into two distally
| |
| ** Transverse foramina – holes in the transverse processes.
| |
| *** space for vertebral artery, vein and sympathetic nerves<ref name=":1">Teach me anatomy The cervical Spine Available from:https://teachmeanatomy.info/neck/bones/cervical-spine/</ref>
| |
|
| |
|
| ==== Atlas and Axis ====
| | * vertebral bodies are smaller compared to the rest of the spine |
| The [[atlas]] and [[axis]] have additional features that mark them apart from the other cervical vertebrae.<ref name=":1" />
| | * vertebral foramen is triangular |
| | * spinous process is bifid (i..e. it splits into two distally) |
| | * there are openings in the transverse processes which allow passage for the vertebral artery, vein, and sympathetic nerves |
|
| |
|
| ==== Atlas ====
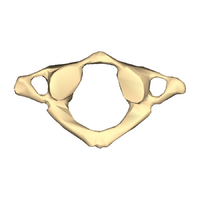
| | The Atlas (C1), Axis (C2) and C7 have further distinguishing features: |
| The atlas is the first cervical vertebra and articulates with the occiput of the head and the axis (C2). Has no vertebral body and no spinous process.
| |
|
| |
|
| * Has lateral masses which are connected by an anterior and posterior arch. Each lateral mass contains a superior articular facet (for articulation with occipital condyles), and an inferior articular facet (for articulation with C2).
| | <div class="row"> |
| * The anterior arch contains a facet for articulation with the dens of the axis. This is secured by the transverse ligament of the atlas – which attaches to the lateral masses. The posterior arch has a groove for the [[Vertebral Artery|vertebral artery]] and C1 spinal nerve. | | <div class="col-md-8 ">[[Atlas]] (C1)<br> |
| | * has no vertebral body or spinous process |
| | * instead, it has lateral masses for articulation with the occiput of the head and the second cervical vertebra (the Axis) |
| | </div> |
| | <div class="col-md-4">[[File:Cervical vertebra 1 close-up bottom (1).png|thumb|200x200px|Atlas - C1]]<br> |
| | </div> |
| | </div> |
|
| |
|
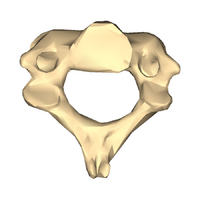
| ==== Axis ==== | | <div class="row"> |
| The axis (C2) is easily identifiable due to its dens ([[Odontoid process|odontoid]] process) which extends superiorly from the anterior portion of the vertebra.
| | <div class="col-md-8 ">[[Axis]] (C2)<br> |
| | * has a bony projection from the anterior portion called the dens, or the odontoid process, which articulates with the atlas |
| | * it is the primary weight-bearing bone of upper cervical region |
| | </div> |
| | <div class="col-md-4">[[File:Cervical vertebra 2 close-up bottom.png|thumb|200x200px|Axis - C2]]<br> |
| | </div> |
| | </div> |
|
| |
|
| The dens articulates with the anterior arch of the atlas, in doing so creating the medial atlanto-axial joint. This allows for rotation of the head independently of the torso.
| | <div class="row"> |
| | <div class="col-md-8 ">C7<br> |
| | * singular spinous process |
| | * larger spinous process |
| | * spinous process is not bifid |
| | </div> |
| | <div class="col-md-4">[[File:Cervical vertebrabifud.jpg|thumb|C3-C6]]<br> |
| | </div> |
| | </div> |
| | <nowiki>**</nowiki>In supine, it may be difficult to palpate the spinous process of C3-C6 in individuals with normal cervical lordosis. |
|
| |
|
| C7: has a much larger and singular spinous process, known as the vertebra prominens, which is similar to those in the thoracic vertebrae.<ref name=":0" />
| | === Intervertebral Discs (IVD) === |
| | The intervertebral discs make up 25% of the height of the entire spine. However, in the cervical region, they make up 40% of the height. This increased height relative to vertebral body height provides a mobility advantage.<ref name=":2">Learn muscles . Cervical spine joints. Available from: https://learnmuscles.com/blog/2017/08/01/cervical-spinal-joints/ (last accessed 29.1.2020)</ref> |
|
| |
|
| *
| | The nucleus pulposus of the cervical discs is gelatinous in children and young people. However, it dries out by the age of 30 years and becomes a firm, fibrocartilaginous plate.<ref>Peng B, Bogduk N. [https://academic.oup.com/painmedicine/article/20/3/446/5232305?login=false Cervical discs as a source of neck pain. An analysis of the evidence.] Pain Medicine. 2019 Mar 1;20(3):446-55.</ref>[[File:Cervical Vertebra Unlabeled.jpg|thumb|Intervertebral disc]] |
| *
| | The following are characteristics of the cervical spine intervertebral discs: |
| * ''Vertebral foramen''
| |
| ** ''Triangular in shape''
| |
| ** ''Larger than in the thoracic vertebrae, but smaller than in the cervical vertebrae''
| |
| * ''Two pedicles''
| |
| ** ''Posterior element of the lumbar vertebra''
| |
| ** ''Attach to the cranial half of the vertebral body''
| |
| ** ''Become shorter, broader and more lateral from L1-L5''
| |
| * ''Two laminae''
| |
| ** ''Flat and broad''
| |
| ** ''Two pedicles and two laminae form the vertebral arch''
| |
| ** ''Centrally connect to the spinous process''
| |
| * ''Spinous process''
| |
| ** ''Projects perpendicularly from the body''
| |
| ** ''Short and sturdy''
| |
| ** ''Described as "hatchet-shaped"''
| |
| ** ''Provides an attacment point for muscles and ligaments''
| |
| * ''Two transverse processes''
| |
| ** ''Located on the posterior surface''
| |
| ** ''Project laterally on each side of the vertebra''
| |
| ** ''Long and slender''
| |
| ** ''Provide attachment points for muscles and ligaments''
| |
| ** ''L1-L3 project horizontally''
| |
| ** ''L4-L5 project upward''
| |
| * ''Four articular processes''
| |
| ** ''Two superior articular facets and two inferior articular facets''
| |
| ** ''The point where two facets join is called the zygapophyseal joints''
| |
|
| |
|
| === ''Lumbar Lordosis'' ===
| | * thicker anteriorly than posteriorly |
| ''Lordosis = the natural curve for the lumbar spine. This curve defines lumbar spine alignment in the saggital plane. However, the pelvis is "the cornerstone of spinal sagittal alignment". The curve of the sacrum determines the lumbar curve.''
| | * concave superior surface |
| | * convex inferior surface |
| | * movement limited by the uncinate process |
| | * anteroposterior translation does occur |
|
| |
|
| ''The sagittal alignment of the lumbar spine offers two main benefits during locomotion:''
| | <nowiki>**</nowiki> Due to the location of the uncinate process, posterolateral disc herniations are less frequent. |
| | === Cervical Lordosis === |
| | Typically, the cervical spine has a lordotic curvature. A lordotic posture can resist large compressive loads. It also helps to decrease stress on vertebral end plates. Compressive loads are distributed differently in the cervical spine than in the thoracic and lumbar spine. In the cervical spine, the anterior column absorbs 36% of the load, and the posterior facet (zygapophyseal) joints absorb 64%.<ref>Guo GM, Li J, Diao QX, Zhu TH, Song ZX, Guo YY, Gao YZ. [https://josr-online.biomedcentral.com/articles/10.1186/s13018-018-0854-6 Cervical lordosis in asymptomatic individuals: a meta-analysis. J]ournal of orthopaedic surgery and research. 2018 Dec;13(1):1-7.</ref> |
| | == Kinematics and Joints of the Cervical Spine == |
| | [[File:Cervical spine exercises.png|thumb|Range of Motion in Cervical Spine]] |
| | The cervical spine is the most mobile part of the vertebral column. |
|
| |
|
| * ''Allows the body's centre of mass to be positioned above the hip, knee, and ankle joints''
| | '''Flexion''' range of motion is usually around 40 degrees, and extension is around 50 degrees. The largest contributors to flexion/extension are: |
| * ''Minimises the muscular force used for postural control''
| |
|
| |
|
| ''Assessment of lumbar spine alignment must include an analysis of the alignment of the lower limbs. For instance, measuring the degree of knee flexion and pelvic shift might help clinicians identify compensatory mechanisms resulting from the sagittal plane malalignment.''
| | * C4/C5 and C5/C6 in sitting |
| | * C6/C7 in supine |
|
| |
|
| == ''Abdominal Wall Structure'' ==
| | C7/T1 contributes the least to flexion/extension. |
| ''The skeletal support of the abdominal wall comes from the vertebral column and lower ribs posteriorly. Anteriorly, it connects to the thoracic cage (rib cage) superiorly and the pelvic bones inferiorly. It is defined by the following landmarks:''
| |
|
| |
|
| * ''superior border = the xiphoid process and costal cartilages of the 7th–10th ribs''
| | '''Lateral flexion''' range of motion is normally close to 30 degrees. C3/C4 and C6/C7 allow for the most movement in this plane of motion. |
| * ''inferior border = the umbilicus in the middle, and [[Inguinal Ligament|inguinal ligament]], pubic crest and [[Pubic Symphysis Dysfunction|pubic symphysis]]''
| |
|
| |
|
| ''You can read more about pelvis anatomy [[Functional Anatomy of the Pelvis#ppm251385|here]].'' | | Cervical '''rotation''' range of motion is usually close to 70 degrees. Flexibility in this plane is mainly achieved through the C1/C2 segment.<ref>Lindenmann S, Tsagkaris C, Farshad M, Widmer J. [https://link.springer.com/article/10.1007/s10439-022-03088-8 Kinematics of the Cervical Spine Under Healthy and Degenerative Conditions: A Systematic Review]. Annals of Biomedical Engineering. 2022 Dec 10:1-29.</ref> |
| | {| class="wikitable" |
| | |+'''Joints of the Cervical Spine'''<ref name=":2" /><ref>RSNA Joints of Luschka Available from: https://pubs.rsna.org/doi/10.1148/66.2.181 (last accessed 28.1.2020)</ref> |
| | !Joint |
| | !Location/Articulations |
| | !Function |
| | !Orientation/Composition |
| | |- |
| | |'''Intervertebral Disc Joint''' |
| | | |
| | * <small>Between the vertebral bodies</small> |
| | | |
| | *<small>Bear weight</small> |
| | * <small>Facilitate motion</small> |
| | * <small>Absorb shock</small> |
| | | |
| | |- |
| | |<small>'''Facet (Zygapophyseal) Joints'''</small> |
| | | |
| | * <small>Formed by articulations between the superior and inferior articular processes of adjacent vertebrae</small> |
| | | |
| | *<small>Guide motion at the segmental level</small> |
| | * <small>Determine the direction of motion</small> |
| | | |
| | * <small>Upper cervical spine = horizontal</small> |
| | * <small>Lower cervical spine = more vertical</small> |
| | |- |
| | |<small>'''Uncovertebral Joint'''</small> |
| | | |
| | *<small>Between the five lower cervical vertebral bodies</small> |
| | * <small>Anteromedially to the nerve root</small> |
| | * <small>Posteromedially to the vertebral artery</small> |
| | | |
| | * <small>Control movement</small> |
| | * <small>Limit lateral flexion</small> |
| | | |
| | |- |
| | |<small>'''Atlanto-Axial Joint'''</small> |
| | | |
| | * <small>Between the atlas and axis</small> |
| | * <small>Two lateral: interior facets of the lateral masses of C1 and superior facets of C2</small> |
| | * <small>One medial: between the dens of C2 and the articular facet of C1</small> |
| | | |
| | * <small>Cervical rotation (60% of cervical rotation occurs at this joint)</small> |
| | | |
| | * <small>Lateral: plane-type synovial joint</small> |
| | * <small>Medial: pivot-type synovial joint</small> |
| | |- |
| | |<small>'''Atlanto-Occipital Joint'''</small> |
| | | |
| | * <small>Between the spine and cranium</small> |
|
| |
|
| == ''Bones, Articulations and Kinematics of the Lumbar Spine'' ==
| | * <small>Between the superior facets of the lateral masses of the atlas and the occipital condyles</small> |
| | | |
| | * <small>Flexion and extension of the head on the neck</small> |
| | * <small>Lateral flexion</small> |
| | | |
| | * <small>Condyloid-type synovial joint</small> |
| | |} |
|
| |
|
| === ''Bones and Articulations'' === | | == Spinal Ligaments == |
| ''The lumbar spine has two types of joints located between each lumbar vertebra:''
| | Ligaments present throughout the entire vertebral column: |
|
| |
|
| # ''intervertebral disc joint'' | | # Anterior longitudinal ligament: anterior surface of the vertebral bodies; limits extension of the spine |
| # ''zygapophyseal joint or facet joint'' | | # Posterior longitudinal ligament: posterior surface of the vertebral bodies; limits flexion of the spine |
| | # Ligamentum flavum: connects the laminae of each vertebrae; series of short ligaments |
| | # Intertransverse ligament: a series of short ligaments that connect the laminae of each vertebrae; preserves upright posture and prevents hyperflexion of the spine<ref name=":3" /> |
|
| |
|
| {| class="wikitable" | | {| class="wikitable" |
| |+ | | |+'''Ligaments Unique to the Cervical Spine''' |
| !'''''Bones'''''
| | !'''<small>Ligament</small>''' |
| !'''''Articulations''''' | | !'''<small>Origin</small>''' |
| !'''''Characteristics''''' | | !'''<small>Insertion</small>''' |
| !'''''Key palpation points'''''
| | !'''<small>Role/Function</small>''' |
| | |- |
| | |<small>'''Nuchal ligament'''</small> |
| | |<small>Occiput</small> |
| | |<small>Tips of the spinous process from C1-C7</small> |
| | |<small>Limits hyperflexion</small> |
| | |- |
| | |<small>'''Transverse ligament'''</small> |
| | | |
| | |<small>Attaches to lateral masses of atlas</small> |
| | |<small>Anchors dens in place</small> |
| | |- |
| | |<small>'''Apical ligament'''</small> |
| | |<small>Dens of the axis</small> |
| | |<small>Foramen magnum</small> |
| | |Connects the dens of the axis to the foramen magnum |
| | <small>Stabilises the skull on the spine</small> |
| |- | | |- |
| |''Vertebral body'' | | |<small>'''Alar ligament'''</small> |
| |''Intervertebral disc joint''
| | |<small>Dens of the axis</small> |
| |''This joint is formed between the inferior surface of one vertebral body and the superior surface of the vertebral body that lies below (for example, the inferior surface of L1 and the superior surface of L2). An intervertebral disc separates the vertebral bodies.'' | | |<small>Occiput</small> |
| |''To find each segment of the lumbar spine, position the patient prone. The location of the spinous processes will determine the location of each segment. You can palpate the spinous processes in the centre of the patient's back.'' | | |Connects the dens of the axis to the occiput |
| ''Start with finding T12 by palpating the patient's lowest rib and following your finger along the border of the rib towards the centre of the spine. The T12 spinous process is in line with the 12th rib (which inserts into T12 spinal segment). Below T12, you can palpate L1 and continue along the spinous process of L2, L3, and L4. If you start your palpation from the distal end of the lumbar spine, you must consider the following: the spinous process of L4 "is usually determined by the position of the highest point on both sides of PSIS", but the accuracy of palpation is only 36%.''
| | <small>Limits atlanto-axial rotation</small> |
| |- | | |- |
| |''Articular processes'' | | |<small>'''Cruciform or cruciate ligament'''</small> |
| |''Zygapophyseal joint (Facet joint)''
| |
| |''Formed between the articular processes of each lumbar vertebra.''
| |
| ''Located on the left and right sides of the spine.''
| |
|
| |
|
| ''They link one vertical segment to the other. For example, the facet joint between L3 and L4 will connect L3 to L4.''
| | <small>1. Superior longitudinal band</small> |
|
| |
|
| ''The superior articular surface is vertical and concave, and the inferior is vertically convex.''
| | <small>2. Inferior longitudinal band</small> |
|
| |
|
| ''Their primary role includes the stabilisation of the spinal motion segment. They also contribute to axial compressive load transmission.''
| | <small>3. Transverse band</small> |
| |''The facet joint CANNOT be directly palpated due to overlying soft tissue. When you move your fingers two to three centimetres in the lateral direction from the spinous process, you will be on the muscles overlying the '''facet joint.''''' | | | |
| | # <small>Superior: transverse band</small> |
| | # <small>Inferior: transverse band</small> |
| | # <small>Transverse: dens of the axis</small> |
| | | |
| | # <small>Superior: foramen magnum</small> |
| | # <small>Inferior: second vertebral body</small> |
| | # <small>Transverse: between the lateral masses of the atlas</small> |
| | |<small>Holds dens in place</small> |
| |} | | |} |
| | <nowiki>**</nowiki> ligaments in spinal column |
|
| |
|
| === ''Kinematics'' === | | == Muscles of the Cervical Spine == |
| ''The lumbar spine is considered a three-joint complex or an articular triad. The zygapophyseal (facet) joints and intervertebral disc joint are part of a "spinal motion segment". The various parts of the spinal motion segment work together to allow spinal motion and to protect the spine from excessive movements.''
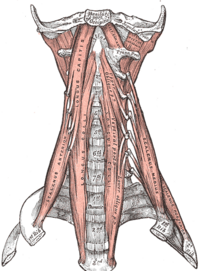
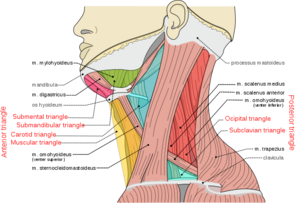
| | The muscles of the cervical spine can be divided by location or by function.[[File:Prevertebral neck muscles.png|thumb|271x271px|Anterior vertebral muscles]] |
|
| |
|
| ''The spinal motion segment has the following characteristics:''
| | === Anterior (Prevertebral) Vertebral Muscles === |
| | * [[Rectus Capitis Anterior|Rectus capitis anterior]] |
| | * [[Rectus Capitis Lateralis|Rectus capitis lateralis]] |
| | * [[Longus Capitis|Longus capitis]] |
| | * [[Longus Colli|Longus colli]]/ Longus cervicis (3 portions: superior oblique, inferior oblique, vertical) |
| | These muscles are also known as the deep cervical (neck) flexors. |
|
| |
|
| * ''The intervertebral disc joint transmits mostly vertical compressive loads''
| | === Lateral Vertebral Muscles === |
| * ''The facet joints guide and stabilise the motion segment''
| | [[Scalene|Scalenes]] |
| * ''In an erect standing position and erect sitting posture, spine load is also transmitted through the facet joints''
| |
|
| |
|
| {| class="wikitable"
| | * [[Anterior Scalene|anterior]] |
| |+ | | * [[Middle Scalene|middle]] |
| !''Joint''
| | * [[Posterior Scalene|posterior]] |
| !''Type of joint''
| | * [[Scalenus Minimus|minimus]] (not always present) |
| !''Plane of movement''
| |
| !''Motion''
| |
| !''Kinematics''
| |
| !''Closed pack position''
| |
| !''Open pack position''
| |
| |- | |
| |[[Intervertebral disc|''Intervertebral disc joint'']]
| |
| |''Cartilaginous joint, symphysis''
| |
| |''A single joint: structurally fused but allows very limited, multidirectional movements''
| |
| ''All lumbar intervertebral disc joints and zygapophyseal joints combined together: Saggital Frontal Transverse''
| |
| |''Single joint: Translating, tilting, rocking and compressing movements.''
| |
| ''All lumbar intervertebral disc joints and zygapophyseal joints combined together:''
| |
|
| |
|
| ''Flexion/extension''
| | [[File:Neck triangles.png|thumb|Lateral view of cervical muscles]] |
|
| |
|
| ''Lateral flexion''
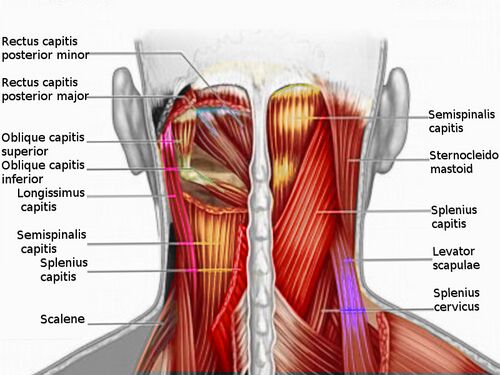
| | === Posterior Vertebral Muscles === |
| | These can be further divided into intrinsic and extrinsic muscles. |
|
| |
|
| ''Rotation''
| | ==== Extrinsic muscles ==== |
| |''All lumbar intervertebral disc joints and zygapophyseal joints combined together:''
| |
| ''Flexion 60 degrees''
| |
|
| |
|
| ''Extension 25 degrees''
| | * [[Trapezius]] |
| | * [[Levator Scapulae|Levator scapulae]] |
|
| |
|
| ''Lateral flexion 20-30 degrees''
| | ==== Intrinsic muscles ==== |
| | [[File:Cervical Spine Muscles.jpg|thumb|500x500px|Posterior muscles of the cervical spine]] |
| | * Superficial muscles : |
| | ** [[Splenius Capitis|splenius capitis]] |
| | ** [[Splenius Cervicis|splenius cervicis]] |
| | * Deep muscles: |
| | ** suboccipital group |
| | *** [[Rectus Capitis Posterior Major|rectus capitis posterior major]] |
| | *** [[Rectus Capitis Posterior Minor|rectus capitis posterior minor]] |
| | *** [[Obliquus Capitis Inferior|obliquus capitis inferior]] |
| | *** [[Obliquus Capitis Superior|obliquus capitis superior]] |
| | ** transversospinalis muscles |
| | *** [[Semispinalis Capitis|semispinalis capitis]] |
| | *** [[Semispinalis Cervicis|semispinalis cervicis]] |
| | *** rotatores cervicis |
| | *** multifidus (these are also known as deep neck extensors) |
| | ** interspinales and intertransversarii |
|
| |
|
| ''Rotation 1-5 degrees'' | | === Movement === |
| |''Full extension''
| | {| class="wikitable" |
| |''Halfway between flexion and extension''
| | |+ |
| | !<small>'''Motion'''</small> |
| | !<small>'''Flexion'''</small> |
| | !<small>'''Extension'''</small> |
| | !<small>'''Lateral Flexion'''</small> |
| | !<small>'''Rotation'''</small> |
| |- | | |- |
| |''Zygapophyseal joint (facet joint)'' | | |<small>'''Muscles'''</small> |
| |''[[Synovial Joints|Synovial]] plane joint'' | | | |
| |''Facilitate a multiplanar and multidirectional movement of the spine.'' | | * [[Longus Colli|<small>Longus colli</small>]] |
| ''Enable lumbar spine extension, lateral flexion, and rotation in the saggital, transverse and frontal planes.''
| | * <small>[[Sternocleidomastoid]]</small> |
| |''Flexion/extension'' | | * [[Scalene|<small>Scalene anterior</small>]] |
| ''Lateral flexion''
| | * [[Longus Capitis|<small>Longus capitis</small>]] |
| | | * <small>[[Rectus Capitis Anterior|Rectus capitis anterior]] (head only)</small> |
| ''Rotation''
| | | |
| |''All lumbar intervertebral disc joints and zygapophyseal joints combined together:''
| | * [[Iliocostal Cervicis|<small>Iliocostal cervicis</small>]] |
| ''Flexion:60 degrees''
| | * [[Splenius Cervicis|<small>Splenius cervicis</small>]] |
| | | * [[Splenius Capitis|<small>Splenius capitis</small>]] |
| ''Extension 25 degrees''
| | * <small>[[Trapezius]]</small> |
| | | * [[Erector Spinae|<small>Erector spinae</small>]] |
| ''Lateral flexion 20-30 degrees''
| | * <small>[[Rectus Capitis Posterior|Rectus capitis posterior,]] [[Rectus Capitis Posterior Major|major]] and [[Rectus Capitis Posterior Minor|minor]] (head only)</small> |
| | * <small>Sternocleidomastoid</small> |
| | * <small>Longissimus capitis</small> |
| | * <small>Spinalis capitis</small> |
| | | |
| | * <small>Scalene anterior, medius and posterior</small> |
| | * <small>Sternocleidomastoid</small> |
| | * <small>Splenius capitis</small> |
| | * <small>Trapezius</small> |
| | * <small>Erector spinae</small> |
| | * <small>[[Rectus Capitis Lateralis|Rectus capitis lateralis]] (head only)</small> |
| | * <small>Spinalis capitis</small> |
| | | |
| | * [[Semispinalis Cervicis|<small>Semispinalis cervicis</small>]] |
| | * <small>Multifidus</small> |
| | * <small>Scalene anterior</small> |
| | * <small>Splenius cervicis and capitis</small> |
| | * <small>Sternocleidomastoid</small> |
| | * <small>Inferior oblique (head only)</small> |
| | * <small>Rectus captitis posterior major (head only)</small> |
| | * <small>Longissius capitis</small> |
| | * <small>Spinalis capitis</small> |
| | |} |
| | <ref>Palastanga, N., & Soames, R. (2012). Anatomy and human movement (6th ed.). Edinburgh: Churchill Livingstone.</ref> |
|
| |
|
| ''Rotation 1-5 degrees''
| | The following tables identify the origin, insertion, innervation and action of key cervical muscles. Muscles with multiple functions are repeated in the relevant tables. |
| |''Full extension''
| |
| |''Halfway between flexion and extension''
| |
| |}
| |
|
| |
|
| == ''Lumbar Spine Ligaments'' == | | === Cervical Spine Flexors === |
| {| class="wikitable" | | {| class="wikitable" |
| |+ | | |+ |
| !'''''Key ligaments''''' | | !<small>'''Muscle'''</small> |
| !'''''Origin''''' | | !<small>'''Origin'''</small> |
| !'''''Insertion''''' | | !<small>'''Insertion'''</small> |
| !'''''Action/role''''' | | !<small>'''Innervation'''</small> |
| !'''''Key palpation points''''' | | !<small>'''Action'''</small> |
| |- | | |- |
| |[[Anterior longitudinal ligament|''Anterior longitudinal ligament'']] | | |<small>'''Rectus capitis anterior'''</small> |
| |''The anterior portion of the vertebral body at the base of the skull'' | | |<small>Lateral mass and transverse process of atlas (C1)</small> |
| |''The anterior portion of the vertebral body at the sacrum'' | | |<small>Basilar part of occipital bone</small> |
| |''Limits extension of the vertebral column.'' | | |<small>Anterior rami of 1st and 2nd cervical spinal nerves (C1, C2)</small> |
| ''Reinforces the intervertebral disc.''
| |
| | | | | |
| | * <small>Flexion of the head at the atlanto-occipital joint</small> |
| |- | | |- |
| |[[Posterior longitudinal ligament|''Posterior longitudinal ligament'']] | | |<small>'''Longus colli'''</small> |
| |''The body of C2''
| | |<small>Transverse processes of C3-C5 and the vertebral bodies of C5-T3</small> |
| |''Posterior surface of the sacrum'' | | |<small>Anterior tubercle of C1, the vertebral bodies of C2-C4, and the transverse processes of C5 and C6.</small> |
| |''Limits flexion of the vertebral column.'' | | |<small>Anterior rami of the 2nd to 6th cervical spinal nerves (C2-C6)</small> |
| ''Reinforces the intervertebral disc.''
| |
| | | | | |
| | * <small>Unilateral contraction: neck lateral flexion (ipsilateral), neck rotation (contralateral)</small> |
| | * <small>'''Bilateral contraction: neck flexion'''</small> |
| |- | | |- |
| |''[[Ligamentum flavum]]:'' | | |<small>'''Longus capitis'''</small> |
| ''A series of short ligaments that connect the laminae of each vertebra. There are two ligamenta flava at each vertebra.''
| | |<small>Transverse processes of C3-C6</small> |
| | | |<small>Occipital bone</small> |
| ''Each ligament is divided into:''
| | |<small>Anterior rami of 1st to 3rd cervical spinal nerves (C1-C3)</small> |
| | |
| '''''The medial portion:''' passes to the back of the next lower lamina and across the gap between the adjacent vertebrae, fusing with the [[/www.physio-pedia.com/Interspinous ligament|interspinous ligament]]''
| |
| | |
| '''''The lateral portion:''' passes in front of the [[/www.physio-pedia.com/Facet Joints|facet joint,]] attaches to the anterior aspect of the inferior and superior articular processes and forms the anterior capsule. The most lateral fibres extend beyond the superior articular process to the pedicle below.''
| |
| |''The lower half of the anterior surface of the lamina above'' | |
| |''The posterior surface and upper margin of the lamina below'' | |
| |''Their high elastin content prevents the ligament from buckling into the spinal canal.''
| |
| ''Assists with lumbar spine flexion and extension.''
| |
| | |
| ''Compresses the intervertebral discs.''
| |
| | | | | |
| | * <small>Unilateral contraction: rotation of the head (ipsilateral)</small> |
| | * <small>'''Bilateral contraction: flexion of the head and neck'''</small> |
| |- | | |- |
| |''Intertransverse ligaments'' | | |<small>'''Anterior scalene'''</small> |
| |''Transverse processes of the vertebra above'' | | |<small>Transverse processes of C3-C6</small> |
| |''Transverse processes of the vertebra below'' | | |<small>First rib</small> |
| |''Contributes to the stability of the lumbar spine.'' | | |<small>Anterior rami of 4th to 6th cervical spinal nerves (C4-C6)</small> |
| ''Limits lateral flexion.''
| | | |
| |''To palpate the '''transverse process''', position the patient in sitting. The transverse processes of the lumbar spine are most likely located directly in line with the spinous process of the corresponding vertebra. Start by palpating the spinous process of the L1 vertebra and move directly lateral to find the transverse process of L1.''
| | * <small>Unilateral contraction: neck lateral flexion (ipsilateral), neck rotation (contralateral), elevation of the first rib</small> |
| | * <small>'''Bilateral contraction: neck flexion'''</small> |
| | * Accessory muscle of respiration |
| |- | | |- |
| |''Supraspinous ligament'' | | |<small>'''Sternocleidomastoid'''</small> |
| |''Tip of spinous processes of the vertebra above from the seventh cervical vertebra to the third or fourth lumbar vertebra'' | | |<small>Manubrium and the medial portion of the clavicle</small> |
| |''Tip of spinous processes of the vertebra below'' | | |<small>Mastoid process of the temporal bone</small> |
| |''Prevents the separation of the spinous processes during forward flexion, thus limiting lumbar spine flexion'' | | |<small>Accessory nerve (CN XI), branches of cervical plexus (C2-C3)</small> |
| |''You can palpate the '''spinous processes''' in the centre of the patient's back.'' | | | |
| ''Start with finding T12 by palpating the patient's lowest rib and following your finger along the border of the rib towards the centre of the spine.T12 spinous process is in line with the 12th rib that inserts into the spinal segment. Below T12, you can palpate L1 and continue along the spinous process of L2, L3, and L4.'' | | * <small>Unilateral contraction: '''ipsilateral lateral flexion''', elevation of the chin, contralateral rotation of head</small> |
| | * <small>Bilateral contraction: '''flexes the neck''', extension of the upper vertebral joints, extension of the neck and head, elevation of the head, elevation of the sternum and clavicle, expansion of the thoracic cavity</small> |
| |- | | |- |
| |''Interspinous ligament'' | | |<small>'''Rectus capitis lateralis'''</small> |
| |''Spinous processes of the vertebra above between the ligamenta flava anteriorly and the supraspinous ligament posteriorly'' | | |<small>Transverse process of atlas (C1)</small> |
| |''Spinous processes of the vertebra below between the ligamenta flava anteriorly and the supraspinous ligament posteriorly'' | | |<small>Jugular process of occipital bone</small> |
| |''Limits forward flexion of the vertebral column.'' | | |<small>Anterior rami of 1st and 2nd cervical spinal nerves (C1-C2)</small> |
| | | | | |
| | * <small>Lateral flexion of the head (ipsilateral)</small> |
| | * <small>'''Neck flexion'''</small> |
| | * <small>Stabilisation of the atlanto-occipital joint</small> |
| |} | | |} |
|
| |
|
| == ''Muscles of the Lumbar Spine and Abdominal Wall'' == | | === '''Cervical Spine Extensors''' === |
| ''The muscles of the back can be grouped according to their function and location.'' | |
| | |
| ''When grouped according to '''function''', the muscles of the lumbar spine can be organised as follows:''
| |
| | |
| * ''Flexors: psoas major, psoas minor, internal oblique, external oblique, and rectus abdominis''
| |
| * ''Extensors: quadratus lumborum, interspinales lumborum, multifidus, and the erector spinae (iliocostalis, longissimus)''
| |
| * ''Lateral flexors: intertransversarii lumborum, psoas major, quadratus lumborum, erector spinae, internal and external obliques''
| |
| * ''Rotators: multifidus, internal and external obliques''
| |
| | |
| ''When grouped according to '''location''', the muscles of the lumbar spine can be divided as follows:''
| |
| | |
| * ''The intrinsic (deep) group:''
| |
| ** ''Superficial layer: erector spinae muscles''
| |
| ** ''Middle (deep) layer: multifidus''
| |
| ** ''Deepest layer: interspinales lumborum and intertransversarii lumborum''
| |
| * ''The abdominal wall group: transverse abdominis, the internal oblique, rectus abdominis, and the external oblique''
| |
| * ''The hip group: psoas major, psoas minor, quadratus lumborum''
| |
| | |
| ''The following tables group muscles according to their function. Please note, that when a muscle has multiple functions, it is included in all relevant tables. These tables only list muscle actions associated with the lumbar spine and abdominal wall. If a muscle acts on other joints, these actions are discussed on the relevant page. For example, psoas major is also a major hip flexor - this role is detailed on the [[Functional Anatomy of the Hip|Functional Anatomy of the Hip page]].''
| |
| | |
| === ''Lumbar Spine Flexors'' ===
| |
| {| class="wikitable" | | {| class="wikitable" |
| |+ | | |+ |
| !''Muscle'' | | !<small>'''Muscle'''</small> |
| !''Origin'' | | !<small>'''Origin'''</small> |
| !''Insertion'' | | !<small>'''Insertion'''</small> |
| !''Innervation'' | | !<small>'''Innervation'''</small> |
| !''Action'' | | !<small>'''Action'''</small> |
| | |- |
| | |<small>'''Obliquus capitis superior'''</small> |
| | |<small>Transverse process of the atlas</small> |
| | |<small>Occipital bone</small> |
| | |<small>Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1))</small> |
| | | |
| | * <small>'''Bilateral contraction: head extension'''</small> |
| | * Unilateral contraction: rotation of head to the ipsilateral side |
| | * <small>Stabilises the atlanto-occipital joint during head movements</small> |
| |- | | |- |
| |''Psoas major'' | | |<small>'''Obliquus capitis inferior'''</small> |
| |''Vertebral bodies of T12-L4'' | | |<small>Spinous process of the axis</small> |
| ''Intervertebral discs between T12-L4 Transverse processes of L1-L5 vertebrae''
| | |<small>Tansverse process of atlas</small> |
| |''Lesser trochanter of femur'' | | |<small>Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1))</small> |
| |''Anterior rami of spinal nerves L1-L3'' | | | |
| |''Contribute to lumbar spine flexion when acting bilaterally and when the insertion point is fixed.''
| | * <small>'''Bilateral contraction: head extension'''</small> |
| | * <small>Unilateral contraction: rotation of head to the ipsilateral side</small> |
| | * <small>Stabilises the atlanto-axial joint</small> |
| |- | | |- |
| |''Psoas minor'' | | |<small>'''Rectus capitis posterior major'''</small> |
| |''Vertebral bodies of T12 to L1'' | | |<small>Spinous process of C2</small> |
| |''Iliopubic eminence'' | | |<small>Occipital bone</small> |
| |''Anterior ramus of spinal nerve L1'' | | |<small>Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1))</small> |
| |''Weak trunk flexor. This muscle is absent in 40% of people.''
| | | |
| | * <small>Unilateral contraction: head rotation (ipsilateral)</small> |
| | * <small>'''Bilateral contraction: head extension'''</small> |
| |- | | |- |
| |''Internal obliques'' | | |<small>'''Rectus capitis posterior minor'''</small> |
| |''Thoracolumbar fascia''
| | |<small>Posterior tubercle of the atlas</small> |
| ''Iliac crest Inguinal ligament''
| | |<small>Occipital bone</small> |
| |''Lower four ribs'' | | |<small>Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1))</small> |
| ''Linea alba Pubic crest''
| | | |
| |''Lower intercostal nerves Branches of the lumbar plexus: iliohypogastric nerve and ilioinguinal nerve'' | | * <small>Head extension</small> |
| |''Bilateral action: lumbar flexion'' | |
| ''Assist in raising intra-abdominal pressure''
| |
| |- | | |- |
| |''External obliques'' | | |<small>'''Iliocostal cervicis'''</small> |
| |''Ribs five to twelve'' | | |<small>Ribs 3-6</small> |
| |''Linea alba'' | | |<small>Transverse process of C4-C6</small> |
| ''Pubic tubercle Iliac crest''
| | |<small>Dorsal rami of the upper thoracic and lower cervical spinal nerves</small> |
| |''Intercostal nerves T7- T11 and the T12 subcostal nerve'' | | | |
| |''Bilateral action: lumbar flexion'' | | * <small>Laterally flexes and '''extends the lower [[Cervical Anatomy|cervical region]]'''</small> |
| |- | | |- |
| |''Rectus abdominis'' | | |<small>'''Trapezius'''</small> |
| |''Pubis, pubic symphysis'' | | |<small>Occipital bone, nuchal ligament and spinous process C7-T12</small> |
| |''Xiphoid process of the sternum'' | | |<small>Lateral third of the clavicle, acromian and spine of the scapula</small> |
| ''Fifth to seventh costal cartilage''
| | |<small>Spinal [[Accessory Nerve Cranial Nerve 11|root of accessory nerve]] (CN XI) (motor)</small> |
| |''Thoracoabdominal nerves'' | |
| |''Lumbar spine flexion'' | |
| ''Assists in raising intra-abdominal pressure''
| |
| |}
| |
|
| |
|
| === ''Lumbar Spine Extensors'' ===
| | <small>Cervical nerves (C3 and C4) ([[Pain Assessment|pain]] and [[proprioception]])</small> |
| {| class="wikitable"
| | | |
| |+ | | * <small>Supports the spinal column to remain erect</small> |
| !''Muscle''
| | * '''Neck extension when scapulae are fixed''' |
| !''Origin''
| | * Ipsilateral lateral flexion of neck |
| !''Insertion''
| |
| !''Innervation''
| |
| !''Action''
| |
| |- | | |- |
| |''Quadratus lumborum'' | | |<small>'''Splenius cervicis'''</small> |
| |''Iliac crest''
| | |<small>Spinous process of T3-T6</small> |
| ''Iliolumbar ligament''
| | |<small>Transverse process of C1-C3</small> |
| |''The inferior border of the 12th rib'' | | |<small>Dorsal rami of cervical spinal nerves (C5-C8)</small> |
| ''Transverse processes of L1-L4 vertebrae''
| | | |
| |''Subcostal nerve'' | | * <small>'''Acting bilaterally: extend the neck'''</small> |
| ''Anterior rami of spinal nerves L1-L4''
| | * <small>Acting unilaterally: lateral flexion and rotation of the head and neck to the ipsilateral side</small> |
| |''Bilateral action: trunk extension'' | |
| |- | | |- |
| |''Interspinales lumborum'' | | |<small>'''Splenius capitis'''</small> |
| |''Superior aspects of spinous processes of L2-L5'' | | |<small>Spinous process of C7-T3 and nuchal ligament</small> |
| |''Inferior aspects of spinous processes of L1-L4'' | | |<small>Occipital bone</small> |
| |''Posterior rami of spinal nerves'' | | |<small>Posterior rami of the 2nd and 3rd cervical spinal nerves</small> |
| |''Stabilise the lumbar spine Extend the lumbar spine'' | | | |
| | * <small>'''Acting bilaterally: extension of the head and neck'''</small> |
| | * <small>Acting unilaterally: lateral flexion and rotation of the head and neck to the ipsilateral side</small> |
| |- | | |- |
| |''Multifidus'' | | |'''<small>Spinalis capitis</small>''' |
| |''Sacrum''
| | |<small>Spinous process of C7 and T1</small> |
| ''Posterior superior iliac spine''
| | |<small>Occipital bone</small> |
| | | |<small>Dorsal rami of spinal nerves</small> |
| ''The mammillary processes of the lumbar vertebrae''
| | | |
| | | * <small>'''Acting bilaterally: extension of the neck'''</small> |
| ''Transverse processes of T1-3 Articular processes of C4-C7''
| | * <small>Acting unilaterally: ipsilateral lateral flexion and r</small><small>otation</small> <small>of the neck</small> |
| |''Spinous processes of the vertebrae above their origin'' | |
| |''Medial branches of the posterior rami of the spinal nerves in the corresponding lumbar region'' | |
| |''Extends the lumbar spine'' | |
| ''Provides core stability''
| |
| |- | | |- |
| |''Erector spinae: Iliocostalis lumborum (ICL) Longissimus thoracis (LT)'' | | |<small>'''Longissimus capitis'''</small> |
| |''ICL: Iliac crest''
| | |<small>Transverse process of upper 4 thoracic vertebrae and articular process lower three cervical vertebrae</small> |
| ''LT : Lumbar intermuscular aponeurosis, medial part of sacropelvic surface of ilium, posterior sacroiliac ligament'' | | |<small>Mastoid process</small> |
| |''ICL: L1-L4 lumbar transverse processes, angle of 4-12 ribs and thoracolumbar fascia'' | | |<small>Posterior/dorsal rami of spinal nerves</small> |
| ''LT: Accessory and transverse processes of vertebrae L1-L5''
| | | |
| |''Dorsal rami of spinal nerves'' | | * '''<small>Acting bilaterally: extension of neck</small>''' |
| |''Bilateral action: lumbar spine extension'' | | * <small>Acting unilaterally: ipsilateral lateral flexion and rotation of the neck</small> |
| |} | | |} |
|
| |
|
| === ''Lumbar Spine Lateral Flexors'' === | | <nowiki>**</nowiki> <small>The transversospinal muscles (rotatores, multifidus, semispinalis) are the deep muscle of the spine. They attach between the transverse and spinous process of the vertebrae. They stabilise and extend the spine. The rotatores also provide rotation.</small> |
| | |
| | === Cervical Spine Lateral Flexors === |
| {| class="wikitable" | | {| class="wikitable" |
| |+ | | |+ |
| !''Muscle'' | | !<small>'''Muscle'''</small> |
| !''Origin'' | | !<small>'''Origin'''</small> |
| !''Insertion'' | | !<small>'''Insertion'''</small> |
| !''Innervation'' | | !<small>'''Innervation'''</small> |
| !''Action'' | | !<small>'''Action'''</small> |
| |- | | |- |
| |''Intertransversarii lumborum (ITL):'' | | |<small>'''Splenius cervicis'''</small> |
| ''Lateral (ITLL) Medial (ITLM)'' | | |<small>Spinous process of T3-T6</small> |
| |''ITLL: Transverse and accessory processes of L1-L4'' | | |<small>Transverse process C1-C3</small> |
| ''ITLM: Accessory processes of L1-L4''
| | |<small>Dorsal rami of cervical spinal nerves (C5-C8)</small> |
| |''ITLL: Transverse process of the following vertebra'' | | | |
| ''ITLM: Mammillary processes of the following vertebra''
| | * <small>'''Acting unilaterally: lateral flexion and rotation of the head and neck to the ipsilateral side'''</small> |
| |''Anterior rami of spinal nerves'' | | * <small>Acting bilaterally: extend the neck</small> |
| |''Assists in lateral flexion'' | |
| ''Stabilises the lumbar spine''
| |
| |- | | |- |
| |''Psoas major'' | | |<small>'''Splenius capitis'''</small> |
| |''Vertebral bodies of T12-L4''
| | |<small>Spinous process of C7-T3 and nuchal ligament</small> |
| ''Intervertebral discs between T12-L4 Transverse processes of L1-L5 vertebrae''
| | |<small>Occipital bone</small> |
| |''Lesser trochanter of femur'' | | |<small>Posterior rami of the 2nd and 3rd cervical spinal nerves</small> |
| |''Anterior rami of spinal nerves L1-L3'' | | | |
| |''Lateral flexion of the trunk'' | | * <small>'''Acting unilaterally: lateral flexion of the head and neck and rotation of the head to the ipsilateral side'''</small> |
| | * <small>Acting bilaterally: extension of the head and cervical spine</small> |
| |- | | |- |
| |''Quadratus lumborum'' | | |<small>'''Sternocleidomastoid'''</small> |
| |''Iliac crest'' | | |<small>Manubrium and the medial portion of the clavicle</small> |
| ''Iliolumbar ligament''
| | |<small>Mastoid process of the temporal bone</small> |
| |''The inferior border of the 12th rib'' | | |<small>Accessory nerve (CN XI), branches of cervical plexus (C2-C3)</small> |
| ''Transverse processes of L1-L4 vertebrae'' | | | |
| |''Subcostal nerve'' | | * <small>'''Unilateral contraction: ipsilateral lateral flexion''', elevation of the chin, contralateral rotation of head</small> |
| ''Anterior rami of spinal nerves L1-L4''
| | * <small>Bilateral contraction: flexes the neck, extension of the upper vertebral joints, extension of the neck and head, elevation of the head, elevation of the sternum and clavicle, expansion of the thoracic cavity</small> |
| |''Unilateral action: ipsilateral lumbar spine lateral flexion'' | | |- |
| | |'''Anterior scalene''' |
| | |<small>Transverse processes of C3-C6</small> |
| | |First rib |
| | |<small>Anterior rami of 4th to 6th cervical spinal nerves (C4-C6)</small> |
| | | |
| | * <small>'''Unilateral contraction: neck lateral flexion (ipsilateral)''', neck rotation (contralateral), elevation of the first rib</small> |
| | * <small>Bilateral contraction: neck flexion</small> |
| | * Accessory muscle of respiration |
| |- | | |- |
| |''Erector spinae:'' | | |<small>'''Middle scalene'''</small> |
| ''Iliocostalis (IC) Longissimus (L)''
| | |<small>Posterior tubercles of the transverse processes of C1-C7</small> |
| |''ICL: Iliac crest'' | | |<small>Scalene tubercle of the first rib</small> |
| ''LT : Lumbar intermuscular aponeurosis, medial part of sacropelvic surface of ilium, posterior sacroiliac ligament''
| | |<small>Anterior rami of C3-C8</small> |
| |''ICL: L1-L4 lumbar transverse processes, angle of 4-12 ribs and thoracolumbar fascia''
| | | |
| ''LT: Accessory and transverse processes of vertebrae L1-L5''
| | * <small>Elevation of the first rib</small> |
| |''Dorsal rami of spinal nerves'' | | * <small>'''Ipsilateral contraction causes ipsilateral lateral flexion of the neck'''</small> |
| |''Unilateral action: ipsilateral side flexion and rotation of the vertebral column'' | | * Respiration |
| |- | | |- |
| |''Internal oblique'' | | |<small>'''Posterior scalene'''</small> |
| |''Thoracolumbar fascia''
| | |<small>Posterior tubercles of the transverse processes of C4-C6</small> |
| ''Iliac crest Inguinal ligament''
| | |<small>2nd rib</small> |
| |''Lower four ribs'' | | |<small>Anterior rami of C6-C8</small> |
| ''Linea alba Pubic crest''
| | | |
| |''Lower intercostal nerves'' | | * <small>Elevation of the second rib</small> |
| ''Branches of the lumbar plexus: iliohypogastric nerve and ilioinguinal nerve.''
| | * <small>'''Ipsilateral lateral flexion of the neck'''</small> |
| |''Unilateral action: lumbar spine lateral flexion and/or rotation to the ipsilateral side''
| | * Respiration |
| ''Assists in raising intra-abdominal pressure''
| |
| |- | | |- |
| |''External oblique'' | | |<small>'''Trapezius'''</small> |
| |''Ribs five to twelve''
| | |<small>Occipital bone, nuchal ligament and spinous process C7-T12</small> |
| |''Linea alba'' | | |<small>Lateral third of the clavicle, the acromian and the spine of s scapula</small> |
| ''Pubic tubercle Iliac crest''
| | |<small>Spinal [[Accessory Nerve Cranial Nerve 11|root of accessory nerve]] (CN XI) (motor)</small> |
| |''Intercostal nerves T7- T11 and the T12 subcostal nerve''
| |
| |''Unilateral action: lumbar spine lateral flexion to the ipsilateral side and rotation to the contralateral side'' | |
| |} | |
|
| |
|
| === ''Lumbar Spine Rotators'' ===
| | <small>Cervical nerves (C3 and C4) ([[Pain Assessment|pain]] and [[proprioception]])</small> |
| {| class="wikitable"
| | | |
| |+ | | * <small>Supports the spinal column to remain erect</small> |
| !'''''Muscle'''''
| | * <small>Neck extension when scapulae are fixed</small> |
| !'''''Origin'''''
| | * <small>'''Ipsilateral lateral flexion of the neck'''</small> |
| !'''''Insertion'''''
| |
| !'''''Innervation'''''
| |
| !'''''Action'''''
| |
| |- | | |- |
| |''Multifidus'' | | |<small>'''Rectus capitis lateralis'''</small> |
| |''Sacrum''
| | |<small>Superior surface of the transverse process of atlas</small> |
| ''Posterior superior iliac spine''
| | |<small>Inferior surface of the jugular process of the occipital bone</small> |
| | | |<small>Anterior rami of C1-C2 spinal nerves</small> |
| ''The mammillary processes of the lumbar vertebrae''
| | | |
| |''Spinous processes of the vertebrae above their origin'' | | * <small>'''Lateral flexion of the head (ipsilateral)'''</small> |
| |''Medial branches of posterior rami of spinal nerves in the corresponding lumbar region.'' | | * <small>Deep neck flexion</small> |
| |''Rotates the lumbar spine away from the side of the body on which they are located'' | | * <small>Stabilisation of the atlanto-occipital joint</small> |
| ''Provides core stability''
| |
| |- | | |- |
| |''Internal oblique (IO)'' | | |'''<small>Spinalis capitis</small>''' |
| |''Thoracolumbar fascia''
| | |<small>Spinous process of C7 and T1</small> |
| ''Iliac crest''
| | |<small>Occipital bone</small> |
| | | |<small>Dorsal rami of spinal nerves</small> |
| ''Inguinal ligament''
| | | |
| |''Lower four ribs'' | | *<small>Acting bilaterally: extension of the neck</small> |
| ''Linea alba''
| | * '''<small>Acting unilaterally: ipsilateral lateral flexion and r</small><small>otation</small> <small>of the neck</small>''' |
| | |
| ''Pubic crest''
| |
| |''Lower intercostal nerves''
| |
| ''Branches of the lumbar plexus: iliohypogastric nerve and ilioinguinal nerve.''
| |
| |''Rotation to the same side''
| |
| ''Works together with opposite EO to rotate the spine - e.g. right external oblique works with left internal oblique to rotate the spine.'' | |
| |- | | |- |
| |''External oblique (EO)'' | | |<small>'''Longissimus capitis'''</small> |
| |''Ribs five to twelve''
| | |<small>Transverse process of upper 4 thoracic vertebrae and articular process lower three cervical vertebrae</small> |
| |''Linea alba Pubic tubercle'' | | |<small>Mastoid process</small> |
| ''Iliac crest''
| | |<small>Posterior/dorsal rami of spinal nerves</small> |
| |''Intercostal nerves T7- T11 and the T12 subcostal nerve'' | | | |
| |''Rotation to the opposite side'' | | *<small>Acting bilaterally: extension of the neck</small> |
| ''Works together with opposite IO to rotate the spine - e.g. right external oblique works with left internal oblique to rotate the spine.'' | | *'''<small>Acting unilaterally: ipsilateral lateral flexion and r</small><small>otation</small> <small>of the neck</small>''' |
| |} | | |} |
|
| |
|
| == ''Innervation of the Lumbar Spine and Abdominal Wall'' == | | === Cervical Spine Rotators === |
| {| class="wikitable" | | {| class="wikitable" |
| |+ | | |+ |
| !'''''Nerve''''' | | !'''<small>Muscle</small>''' |
| !'''''Origin''''' | | !'''<small>Origin</small>''' |
| !'''''Branches'''''
| | !'''<small>Insertion</small>''' |
| !'''''Motor fibres''''' | | !'''<small>Innervation</small>''' |
| !'''''Sensory fibres'''''
| | !'''<small>Action</small>''' |
| | |- |
| | |<small>'''Rectus capitis posterior major'''</small> |
| | |<small>Spinous process of C2</small> |
| | |<small>Occipital bone</small> |
| | |<small>Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1))</small> |
| | | |
| | * <small>'''Unilateral contraction: head rotation (ipsilateral)'''</small> |
| | * <small>Bilateral contraction: head extension</small> |
| |- | | |- |
| |''Intercostal'' | | |<small>'''Rectus capitis posterior major'''</small> |
| |''Lumbar plexus'' | | |<small>Spinous process of C2</small> |
| |''Muscular, collateral, lateral cutaneous, anterior cutaneous, and'' | | |<small>Occipital bone</small> |
| ''communicating branches''
| | |<small>Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1))</small> |
| |''External obliques'' | | | |
| ''Internal obliques'' | | * <small>'''Unilateral contraction: head rotation (ipsilateral)'''</small> |
| |''Skin over the anterior abdomen''
| | * <small>Bilateral contraction: head extension</small> |
| |- | | |- |
| |''Subcostal'' | | |<small>'''Sternocleidomastoid'''</small> |
| |''Anterior ramus of the spinal nerve T12'' | | |<small>Manubrium and the medial portion of the clavicle</small> |
| |''Muscular, cutaneous, communicating and collateral branches'' | | |<small>Mastoid process of the temporal bone</small> |
| |''Quadratus lumborum'' | | |<small>Accessory nerve (CN XI), branches of cervical plexus (C2-C3)</small> |
| ''External oblique'' | | | |
| |''The skin of the region under the umbilicus''
| | * <small>Unilateral contraction: ipsilateral lateral flexion, elevation of the chin, c'''ontralateral rotation of head'''</small> |
| | * <small>Bilateral contraction: flexion of the neck, extension of the upper vertebral joints, extension of the neck and head, elevation of the head, elevation of the sternum and clavicle, expansion of thoracic cavity</small> |
| |- | | |- |
| |''Iliohypogastric'' | | |<small>'''Splenius capitis'''</small> |
| |''Lumbar plexus''
| | |<small>Spinous process ofC7-T3 and nuchal ligament</small> |
| |''Lateral cutaneous branch'' | | |<small>Occipital bone</small> |
| ''Anterior cutaneous branch''
| | |<small>Posterior rami of the 2nd and 3rd cervical spinal nerves</small> |
| |''Internal oblique'' | | | |
| |''External abdominal oblique, transversus abdominis, internal abdominal oblique'' | | * <small>Acting unilaterally: lateral flexion of the head and neck and '''rotation of the head to the ipsilateral side'''</small> |
| ''The skin of the suprapubic region'' | |
| |- | | |- |
| |''Ilioinguinal'' | | |<small>'''Splenius cervicis'''</small> |
| |''Lumbar plexus''
| | |<small>Spinous process T3-T6</small> |
| |''Anterior labial nerves'' | | |<small>Transverse process C1-C3</small> |
| ''Anterior scrotal nerves''
| | |<small>Dorsal rami of cervical spinal nerves (C5-C8)</small> |
| |''Internal oblique'' | |
| | | | | |
| | * <small>Acting unilaterally: lateral flexion and '''rotation of the head and neck to the ipsilateral side'''</small> |
| |- | | |- |
| |''Dorsal (posterior) rami of spinal nerves'' | | |'''<small>Spinalis capitis</small>''' |
| |''Spinal nerves''
| | |<small>Spinous process of C7 and T1</small> |
| |''Medial'' | | |<small>Occipital bone</small> |
| ''Intermediate''
| | |<small>Dorsal rami of spinal nerves</small> |
| | | | |
| ''Lateral''
| | * <small>Acting bilaterally: extension of the neck</small> |
| |''Interspinales lumborum'' | | * <small>'''Acting unilaterally: ipsilateral lateral flexion and rotation of the neck'''</small> |
| ''Multifidus''
| |
| | |
| ''Erector spinae'' | |
| |''The skin of the back''
| |
| |- | | |- |
| |''Ventral (anterior) rami of L1-L4'' | | |<small>'''Longissimus capitis'''</small> |
| |''Spinal nerves'' | | |<small>Transverse process of upper 4 thoracic vertebrae and articular process lower three cervical vertebrae</small> |
| | |<small>Mastoid process</small> |
| | |<small>Posterior/dorsal rami of spinal nerves</small> |
| | | | | |
| |''Intertransversarii lumborum''
| | * <small>Acting bilaterally: extension of the neck</small> |
| ''Psoas major'' | | * <small>'''Acting unilaterally: ipsilateral lateral flexion and rotation of the neck'''</small> |
| | |
| ''Psoas minor''
| |
| |''Ventrolateral body surface Structures in the body wall''
| |
| |} | | |} |
|
| |
|
| == ''Vascular Supply of the Lumbar Spine and Abdominal Wall'' == | | == Innervation of the Cervical Spine == |
| | Nerves originating from the cervical plexus innervate the muscles of the neck. Each nerve root in the cervical spine exits above its corresponding nerve root. There are eight pairs of cervical nerves despite there being seven cervical vertebrae. The C8 nerve root exits below the seventh cervical vertebra. The accessory nerve, which is cranial nerve XI innervates sternocleidomastoid and trapezius.<ref name=":0" /> |
| {| class="wikitable" | | {| class="wikitable" |
| |+ | | |+ |
| !''Artery'' | | !'''<small>Nerve</small>''' |
| !''Origin'' | | !'''<small>Motor</small>''' |
| !''Branches'' | | !'''<small>Sensory</small>''' |
| !''Supply''
| | |- |
| | |'''<small>C1</small>''' |
| | |<small>Flexion of the head and neck</small> |
| | <small>Rectus capitus anterior and lateralis, longus capitis</small> |
| | | |
| | |- |
| | |'''<small>C2</small>''' |
| | |<small>Flexion of the head and neck</small> |
| | <small>Rectus capitus anterior and lateralis, longus capitus, prevertebral muscles and sternocleidomastoid</small> |
| | |<small>Lateral occiput and submandibular area</small> |
| |- | | |- |
| |''Lumbar artery (LA):'' | | |'''<small>C3</small>''' |
| ''Left (LLA)''
| | |<small>Head and neck flexion and rotation</small> |
|
| |
|
| ''Right (RLA)''
| | <small>Longus capitus, longus colli, prevertebral muscles and sternocleidomastoid, diaphragm, levator scapulae, trapezius and scalenus medius</small> |
| |''Abdominal aorta'' | | |<small>Lateral occiput and lateral neck, overlapping C2</small> |
| |''Medial'' | | |- |
| ''Middle'' | | |<small>'''C4'''</small> |
| | | |<small>Head and neck flexion and rotation</small> |
| ''Lateral'' | | <small>Longus capitus, longus colli, levator scapulae, scaleni, trapezius, diaphragm</small> |
| |''Skin and muscles of the posterior abdominal wall'' | | |<small>Lower lateral neck and medial shoulder area</small> |
| ''Joints of the lumbar spine'' | | |- |
| | | |'''<small>C5</small>''' |
| ''The lumbar portion of the deep back muscles''
| | |<small>Deltoid, biceps, bicep tendon reflex</small> |
| | | |<small>Clavicle level and lateral arm</small> |
| ''Lower two-thirds of the spinal cord'' | | |- |
| | |'''<small>C6</small>''' |
| | |<small>Biceps, wrist extensors (brachioradialis tendon reflex)</small> |
| | |<small>Lateral forearm, thumb, index and half of 2nd finger</small> |
| | |- |
| | |'''<small>C7</small>''' |
| | |<small>Wrist flexors, triceps (triceps tendon reflex)</small> |
| | |<small>Second finger</small> |
| |- | | |- |
| |''Internal thoracic artery'' | | |'''<small>C8</small>''' |
| |''Subclavian artery''
| | |<small>Finger flexors, interossei</small> |
| |''Anterior collaterals'' | | |<small>Medial forearm, ring and little finger</small> |
| ''Posterior collaterals''
| |
| | |
| ''Terminal branches''
| |
| |''The superior aspect of the abdominal wall'' | |
| |- | | |- |
| |''External iliac artery'' | | |<small>'''T1'''</small> |
| |''Common iliac artery''
| | |<small>Interossei</small> |
| |''Inferior epigastric,'' | | |<small>Medial arm</small> |
| ''Deep circumflex iliac arteries''
| |
| |''Lower abdominal wall'' | |
| |} | | |} |
|
| |
|
| == ''Clinical Relevance'' == | | == Vascular Supply of the Cervical Spine == |
| | Vertebral arteries, veins and nerves pass through the transverse foramina of the cervical vertebrae except for in C7, where the vertebral artery passes around the vertebra instead of through the transverse foramen.<ref name=":1" /> The neural components sit posterior to the vertebral artery.<ref>Joshi N, Klinger N, Halalmeh DR, Tubbs RS, Moisi MD. [https://www.cureus.com/articles/26181-the-neural-sulcus-of-the-cervical-vertebrae-a-review-of-its-anatomy-and-surgical-perspectives#!/ The Neural Sulcus of the Cervical Vertebrae: A Review of Its Anatomy and Surgical Perspectives]. Cureus. 2020 Jan 18;12(1)</ref> |
|
| |
|
| # ''Disc herniations are a common low back condition. They occur when the nucleus pulposus displaces from the intervertebral space. According to Yoon et al., when there is imaging confirmation of lumbar disc herniation that is "consistent with clinical findings, and failure to improve after six weeks of conservative care", surgical intervention may be required. You can read more about the management of disc herniation symptoms [[Disc Herniation|here.]]''
| | The cervical spine vascular supply is primarily provided by the vertebral arteries on each side of the spine. These arteries arise from the subclavian arteries, which originate directly from the arch of the [[aorta]] on the right and the brachiocephalic trunk on the left. |
| # ''Spinal stenosis is a narrowing of the spinal canal. Spinal stenosis can be caused by a range of conditions, such as tumours or bone spurs. You can learn about low back pain assessment and prognosis by taking this course.''
| |
| # ''Diastasis recti is a very common condition where the linea alba stretches and produces a gap between the two sides of the rectus abdominis muscle. Learn more about diastasis recti [[Diastasis recti abdominis|here]].''
| |
|
| |
|
| == ''Resources'' ==
| | <nowiki>**</nowiki> The common carotid artery bifurcates into the internal and external carotid arteries at the C3 segmental level. Only the external carotid artery provides any blood supply to the neck. |
|
| |
|
| # ''Inoue N, Orías AAE, Segami K. Biomechanics of the Lumbar Facet Joint. Spine Surg Relat Res. 2019 Apr 26;4(1):1-7.''
| | == Clinical Relevance == |
| # ''Kostov S, Dineva S, Kornovski Y, Slavchev S, Ivanova Y, Yordanov A. Vascular Anatomy and Variations of the Anterior Abdominal Wall - Significance in Abdominal Surgery. Prague Med Rep. 2023;124(2):108-142.''
| |
| # ''Clinical Physio. Lumbar Spine Palpation''
| |
|
| |
|
| === ''600+ accredited online courses for clinicians'' ===
| | * Atlanto-axial instability (AAI) can have serious neurological consequences: |
| ''Join the world's largest community of rehabilitation professionals''
| | ** conditions with the potential for AAI include: |
| | *** rheumatoid arthritis |
| | *** Down syndrome: |
| | **** laxity in the transverse ligament is present in 14-22% of individuals with Down syndrome. |
|
| |
|
| ''Learn more on this topic''
| | * A tight [[sternocleidomastoid]] muscle can cause torticollis. |
| | * Disc herniation: |
| | ** disc herniations in the cervical spine are a lot less common than in the lumbar spine |
| | ** typical locations: |
| | *** C5-C6 |
| | *** C6-C7 |
| | * Because the prevertebral cervical muscles stabilise the neck, dysfunction in these muscles can cause cervicogenic pain |
| | * Trigger points that develop in the suboccipital muscles can refer pain to the head, causing cervicogenic headaches<ref name=":3">Xuan D. Exploring Cervical Spine Anatomy Course. Plus, 2023.</ref> |
|
| |
|
| ''Related articles''
| | == Resources == |
|
| |
|
| ''Lumbar Anatomy - PhysiopediaIntroduction The lower back (where most back pain occurs) includes the five vertebrae in the lumbar region and supports much of the weight of the upper body. The spaces between the vertebrae are maintained by intervertebral discs that act like shock absorbers throughout the spinal column to cushion the bones as the body moves. Ligaments hold the vertebrae in place, and tendons attach the muscles to the spinal column. Thirty-one pairs of nerves are rooted to the spinal cord and they control body movements and transmit signals from the body to the brain. The spine extends from the skull to the coccyx and includes the cervical, thoracic, lumbar, and sacral regions. The lumbar spine consists of 5 moveable vertebrae (numbered L1-L5). The lumbar vertebrae, as a group, produce a lordotic curve[1] The intervertebral discs are responsible for the mobility without sacrificing the supportive strength of the vertebral column. The intervertebral discs, along with the laminae, pedicles and articular processes of adjacent vertebrae, create a space through which spinal nerves exit. The complex anatomy of the lumbar region is a remarkable combination of these strong vertebrae (with their multiple bony elements) linked by joint capsules, and flexible ligaments/tendons, large muscles, and highly sensitive nerves. It also has a complicated innervation and vascular supply. Vertebrae[edit | edit source] Typical lumbar vertebrae have several features distinct from those typical of cervical or thoracic vertebrae.[1] Presence of a large vertebral body. Spinous process is short and thick, relative to the size of the vertebra, and projects perpendicularly from the body Articular facets are markedly vertical, with the superior facets directed posteromedially and medially Facets also have the unique feature of a curved articular surface. This is one feature that differentiates lumbar vertebrae to from thoracic Addition of the mammillary process on the posterior aspect of the superior articular process. One lumbar vertebra that may be considered atypical. L5 has the largest body and transverse processes of all vertebrae. The anterior aspect of the body has a greater height compared to the posterior. This creates the lumbosacral angle between the lumbar region of the vertebrae and the sacrum. Structure a Reflection of Function[1][edit | edit source] The lumbar vertebrae have the largest bodies of the entire spine and an increase in size as the spine descends, a reflection of the responsibility of the lumbar spine of supporting the entire upper body. Due to the size of the intervertebral discs relative to the size of the vertebral body and the size and horizontal direction of the spinous processes, the lumbar spine has the greatest degree of extension of the vertebral column. The near-vertical orientation of the superior articular facets allows for flexion, extension, and lateral flexion, but prevents rotation. The mammillary processes provide a point of attachment for intertransversarii muscles and multifidus. The curvature of articular facets is thought to assist in the stabilization and weight-bearing capacity of lumbar vertebrae. Each vertebral body is more or less a cylinder with a thin cortical shell, which surrounds cancellous bone. From L1 to L5, the posterior aspect changes from slightly concave to slightly convex, and the diameter of the cylinder increases gradually because of the increasing loads each body has to carry. At the upper and lower surfaces, two distinct areas can be seen: each is a peripheral ring of compact bone – surrounding and slightly above the level of the flat and rough central zone – which originates from the apophysis and fuses with the vertebral body at the age of about 16. The central zone – the bony endplate – shows many perforations, through which blood vessels can reach the disc. A layer of cartilage covers this central zone, which is limited by the peripheral ring. This is the cartilaginous endplate, forming the transition between the cortical bone and the rest of the intervertebral disc. A sagittal cut through the vertebral body shows the endplates to be slightly concave, which consequently gives the disc a convex form[2]. Meningeal branches of spinal nerves innervate all vertebrae[1] Pedicles[edit | edit source] The two pedicles originate posteriorly and attach to the cranial half of the body. Together with the broad and flat lamina, they form the vertebral arch. From L1 to L5, the pedicles become shorter and broader, and are more lateral. This narrows the anteroposterior diameter and widens the transverse diameter of the vertebral canal from above downwards. Together with the increasing convexity of the posterior aspect of the vertebral body, these changes in the position of the pedicles alter the shape of the normal bony spinal canal from an ellipse at L1 to a triangle at L3 and more or less a trefoil at L5 (Fig. 1). Laminae[edit | edit source] Each lamina is flat and broad, blending in centrally with the similarly configured spinal process, which projects directly backwards from the lamina. The two transverse processes project laterally and slightly dorsally from the pediculolaminar junction. The superior and inferior articular processes originate directly from the lamina. The part of the lamina between the superior and inferior articular processes is called the ‘pars interlaminaris’. It runs obliquely from the lateral border of the lamina to its upper medial border. This portion of the lamina is subjected to considerable bending forces, as it lies at the junction between the vertically oriented lamina and the horizontally oriented pedicle. This ‘interlaminar part’ will therefore be susceptible to fatigue fractures or stress fractures (spondylolysis). Facet Joints[edit | edit source] The joints between the lower and upper articular processes are called zygapophyseal joints, apophyseal joints or ‘facet’ joints. They are true synovial joints, comprised of cartilaginous articular surfaces, synovial fluid, synovial tissue and a joint capsule [2] The superior articular surface is slightly concave and faces medially and posteriorly. The convex inferior articular surface points laterally and slightly anteriorly. In general terms, there is a change from a relatively sagi''ttal orientation at L1–L3, to a more coronal orientation at L5 and S1 Unlike the disc, the facet joints normally do not bear weight and during normal loads they are not subjected to compression strain. In degenerative fragmentation of the disc, however, intervertebral height diminishes and the articular surfaces are subjected to abnormal loading, setting up spondylarthrosis. The main function of the facet joints is to guide lumbar movements and keep the vertebrae in line during flexion–extension and lateral flexion. Because of the more sagittal slope of the articular surfaces, very little rotation takes place at the four upper lumbar levels. More distally, at the lumbosacral level, the joint line has a more coronal plane, which makes rotational movements potentially possible, but these are limited by the iliolumbar ligaments. The total range of rotation in the lumbar spine is therefore very limited, although not completely zero. Fibers of the medial branch of the dorsal root innervate the facet joints. The same nerve supplies the inferior aspect of the capsule and the superior aspect of the joint below. Intervertebral Discs[edit | edit source] Two adjacent vertebral bodies are linked by an intervertebral disc. Together with the corresponding facet joints, they form the ‘functional unit of Junghans’n The disc consists of an annulus fibrosus, a nucleus pulposus and two cartilaginous endplates. The distinction between annulus and nucleus can only be made in youth, because the consistency of the disc becomes more uniform in the elderly. For this reason, nuclear disc protrusions are rare after the age of 70. From a clinical point of view, it is important to consider the disc as one integrated unit, the normal function of which depends largely on the integrity of all the elements. That means that damage to one component will create adverse reactions in the others. Endplate[edit | edit source] An upper and a lower cartilaginous endplate (each about 0.6– 1 mm thick) cover the superior and inferior aspects of the disc. The endplate permits diffusion and provides the main source of nutrition for the disc. The hyaline endplate is also the last part of the disc to wear through during severe disc degeneration. Plates of cartilage that bind the disc to their respective vertebral bodies. Each endplate covers almost the entire surface of the adjacent vertebral body; only a narrow rim of bone, called the ring apophysis, around the perimeter of the vertebral body is left uncovered by cartilage. The portion of the vertebral body to which the cartilaginous endplate is applied is referred to as the vertebral endplate. The endplate covers the nucleus pulposus in its entirety; peripherally it fails to cover the entire extent of the annulus fibrosus. The collagen fibrils of the inner lamellae of the annulus enter the endplate and merge with it, resulting in all aspects of the nucleus being enclosed by a fibrous capsule. Annulus Fibrosus[edit | edit source] The annulus fibrosis is made up of 15–25 concentric fibrocartilaginous sheets or ‘lamellae’ each formed by parallel fibres, running obliquely at a 30° angle between the vertebral bodies. Because the fibers of two consecutive layers are oriented in opposite directions, they cross each other at an angle of approximately 120°. This arrangement of the annular fibers gives the normal disc great strength against shearing and rotational stresses, while angular movements remain perfectly possible. The outermost fibers are attached directly to bone, around the ring apophysis, and for that reason they are referred to as the ligamentous portion of the annulus fibrosis. The inner third merges with the cartilaginous endplate and is referred to as the capsular portion of the annulus fibrosis Nucleus Pulposus[edit | edit source] This consists of a gelatinous substance, made of a meshwork of collagen fibrils suspended in a mucoprotein base, which contains mucopolysaccharides and water. As the anterior part of the vertebral body grows faster than the posterior part, the nucleus comes to lie more posteriorly. Consequently, the anterior part of the annulus will have thicker and stronger fibres, which means that the annulus gives better protection against anterior than posterior displacements of the nucleus; this is disadvantageous with respect to the contiguous nerve roots and dura. Functions of the Disc[edit | edit source] The primary function of the disc is to join the vertebrae and allow movement between them. The other functions are typical of the erect spine: a shock absorber; a load distributor; and a separator of the posterior facets to maintain the size of the intervertebral foramen. The Weak Zone of the Disc[edit | edit source] Several anatomical, biochemical and biomechanical properties make the posterior aspect of the disc the most critical and vulnerable part of the whole intervertebral joint. The posterior annular fibers are sparser and thinner than the anterior. Because the area available for diffusion is smaller posteriorly than anteriorly, the posterior part of the nuclear–annular boundary receives less nutrition and again the posterior part of the disc is the most strained part. The posterior longitudinal ligament affords only weak reinforcement, whereas the anterior fibers are strengthened by the powerful anterior longitudinal ligament. Because of the special mechanical arrangements of the annular fibers, the tangential tensile strain on the posterior annular fibers is 4–5 times the applied external load. All these elements explain the predominance of the posterior part of the disc in the development of weakening, radiating ruptures and posterior nuclear displacements. This is unfortunate, because most nociceptive tissues responsible for backache and sciatica (nerve roots and dura mater) emerge just beyond the posterior aspect of the disc. Ligaments[edit | edit source] The broad, thick anterior longitudinal ligament originates from the anterior and basilar aspect of the occiput and ends at the upper and anterior part of the sacrum. It consists of fibers of different lengths: some extend over 4–5 vertebral bodies; the short fibers attach firmly to the fibers of the outermost annular layers and the periosteum of two adjacent vertebrae. The posterior longitudinal ligament is smaller and thinner than its anterior counterpart: 1.4 cm wide (versus 2 cm in the anterior ligament) and 1.3 mm thick (versus 2 mm). The posterior longitudinal ligament is narrow at the level of the vertebral bodies, and gives lateral expansions to the annulus fibrosis at the level of the disc, which bestow on it a denticulated appearance. Although the posterior ligament is rather narrow, it is important in preventing disc protrusion. Its resistance is the main factor in restricting posterior prolapse and accounts for the regular occurrence of spontaneous reduction in lumbago. This characteristic is also exploited in manipulative reduction, when a small central disc displacement is moved anteriorly when the ligament is tightened. The ligamentum flavum connects two consecutive laminae and has a very elastic structure with an elastin content of more than 80%. The lateral extensions form the anterior capsule of the facet joints and run further laterally to connect the posterior and inferior borders of the pedicle above with the posterior and superior borders of the pedicle below. These lateral fibers form a portion of the foraminal ring and the lateral recess. The interspinous ligament lies deeply between two consecutive spinal processes. Unlike the longitudinal ligaments, it is not a continuous fibrous band but consists of loose tissue, with the fibers running obliquely from posterosuperior to anteroinferior. This particular direction may give the ligament a function over a larger range of intervertebral motion than if the fibers were vertical. The ligament is also bifid, which allows the fibers to buckle laterally to both sides when the spinous processes approach each other during extension. The supraspinous ligament is broad, thick and cord-like. It joins the tips of two adjacent spinous processes, and merges with the insertions of the lumbodorsal muscles. Some authors consider the supraspinous ligament as not being a true ligament, as it seems to consist largely of tendinous fibers, derived from the back muscles. The effect of the supraspinous ligaments on the stability of the lumbar spine should not be underestimated. Because the ligament is positioned further away from the axis of rotation and due to its attachments to the thoracolumbar fascia, it will have more effect in resisting flexion than all the other dorsal ligaments. The intertransverse ligaments are thin membraneous structures joining two adjacent transverse processes. They are intimately connected to the deep musculature of the back. The iliolumbar ligaments are thought to be related to the upright posture. They do not exist at birth but develop gradually from the epimysium of the quadratus lumborum muscle in the first decade of life to attain full differentiation only in the second decade. The ligament consists of an anterior and a posterior part. The anterior band of the iliolumbar ligament is a well-developed, broad band. The iliolumbar ligaments play an important role in the stability of the lumbosacral junction by restricting both side flexion and rotational movement at the L5–S1 joint and forward sliding of L5 on the sacrum[2]. Muscles and Fasciae [edit | edit source] The spine is unstable without the support of the muscles that power the trunk and position the spinal segments. Back muscles can be divided into four functional groups: flexors, extensors, lateral flexors and rotators[2] Extensors, arranged in three layers Most superficial is the strong Erector Spinae or sacrospinalis muscle. Its origin is in the erector spinae aponeurosis, a broad sheet of tendinous fibers attached to the iliac crest, the median and lateral sacral crests and the spinous processes of the sacrum and lumbar spine. Middle layer is the multifidus. The fibers of the multifidus are centered on each of the lumbar spinous processes. From each spinal process, fibers radiate inferiorly to insert on the lamina, one, two or three levels below. The arrangement of the fibers is such that it pulls downwards on each spinal process, thereby causing the vertebra of origin to extend. Third layer is made up of small muscles arranged from level to level, which not only have an extension function but are also rotators and lateral flexors. Flexors intrinsic group (psoas major, psoas minor and iliacus) extrinsic group (abdominal wall muscles). Lateral flexors and rotators internal and external oblique, the intertransverse and quadratus lumborum muscles. remember that pure lateral flexion is brought about only by the quadratus lumborum. Spinal Canal[edit | edit source] The spinal canal is made up of the canals of individual vertebrae so that bony segments alternate with intervertebral and articular segments. The shape of the transverse section changes from round at L1 to triangular at L3 and slightly trefoil at L5 (Fig. 1). An anterior wall and a posterior wall, connected through pedicles and intervertebral foramina, form the margins of the canal. The anterior wall consists of the alternating posterior aspects of the vertebral bodies and the annulus of the intervertebral discs. In the midline these structures are covered by the posterior longitudinal ligament, which widens over each intervertebral disc. The posterior wall is formed by the uppermost portions of the laminae and the ligamenta flava. Because the superoinferior dimensions of the laminae tend to decrease at the L4 and L5 levels, the ligamenta flava consequently occupy a greater percentage of the posterior wall at these levels. The spinal canal contains the dural tube, the spinal nerves and the epidural tissue. Dura Mater [edit | edit source] The dura mater is a thick membranous sac, attached cranially around the greater foramen of the occiput, where its fibers blend with the inner periosteum of the skull, and anchored distally to the dorsal surface of the distal sacrum by the filum terminale. At the lumbar level, the dura contains the distal end of the spinal cord (conus medullaris, ending at L1), the cauda equina and the spinal nerves, all floating and buffered in the cerebrospinal fluid. The lumbar roots have an intra- and extrathecal course. Emerging in pairs from the spinal cord, they pass freely through the subarachnoid space before leaving the dura mater. In their extrathecal course and down to the intervertebral foramen, they remain covered by a dural investment. At the L1 and L2 levels, the nerves exit from the dural sac almost at a right angle and pass across the lower border of the vertebra to reach the intervertebral foramen above the disc. From L2 downwards, the nerves leave the dura slightly more proximally than the foramen through which they will pass, thus having a more and more oblique direction and an increasing length within the spinal canal. The dura mater has two characteristics that are of cardinal clinical importance: mobility and sensitivity.[2] Nerve Roots[edit | edit source] The radicular canal contains the intraspinal extrathecal nerve root. The nerve root consists of a sheath (dural sleeve) and fibres. Each structure has a specific behaviour and function, responsible for typical symptoms and clinical signs. This has some clinical consequences: slight pressure and inflammation only involve the sleeve and provoke pain and impaired mobility. More substantial compression of the root will also affect the nerve fibres, which leads to paraesthesia and loss of function.[2] Significant Facts[edit | edit source] Spinal nerves increase in size as the spinal cord descends, however, the intervertebral foramen decrease in size. This combination, in addition to pathology such as intervertebral disc degeneration that brings two adjacent vertebra closer together, commonly leads to spinal stenosis, a condition in which the vertebral foramen compresses the spinal nerves. This may be treated with a laminectomy, a process in which the spinous process, laminae, and pedicles are removed to create more room for the spinal cord and spinal nerves[1] The lumbar region has a lesser incidence of neurological injury due to fractures as compared to those in the thoracic region. This is due to the large size of the vertebral canal, the inferior end of the spinal cord at the level of L2, as well as the relative resilience cauda equina nerve roots. This is why spinal taps are performed inferior to L2; the roots forming the cauda equina, suspended in the cerebrospinal fluid (CSF), move out of the way of the spinal needle[1]. The valve-less vertebral venous plexuses allow for the metastasis of cancer from the pelvis, such as that of the prostatic, to the vertebral column[1] Resources[edit | edit source] Lumbar Spine Anatomy Spinal Cord AnatomyAnatomy of the Canine Spine - PhysiopediaCanine Skull Cranium[edit | edit source] Cranial skull- canine The Roof of the cranium is made up of frontal and parietal bones. The Floor is made up of sphenoid bone. The cranium consists of 5 orbital regions: Frontal Lacrimal Palatine Sphenoid Zygomatic The orbit is complete in horse and ruminants while it is incomplete in carnivores but completed by the orbital ligament. The lacrimal fossa collects tears and sends them through lacrimal canal into the nasal cavity. Joints and Ligaments of the Skull[edit | edit source] Temporo-mandibular joint:[1] A condylar joint, with an articular disc, that sits between the mandibular condyles and the mandibular fossa of the temporal bones It has a loose joint capsule with thickening, which forms a lateral ligament The temporalis muscle closes the jaw and the joint is innervated by cranial nerve V Mandibular symphysis Joints of the hyoid apparatus:[1] Tympanohyoid cartilage - skull (a syndesmosis joint) Interhyoid joints (synovial joints) Thyrohyoid bone - cranial cornu of thyroid cartilage (synovial joint) [2] Canine Spine[edit | edit source] Figure 1. The Canine Skeleton The anatomy of the canine skull and spine is quite similar to the human spine. Like in people, the canine spine supports weight and encloses the spinal cord. The spine is located along the dorsal / top side of the canine's body and runs from the base of the head to the end of the tail.[3] The canine spine is divided into five regions: cervical, thoracic, lumbar, sacral, and caudal. There are 7 cervical vertebrae, 13 thoracic vertebrae, 7 lumbar vertebrae and 3 sacral vertebrae. The number of caudal vertebrae varies according to the species.[4] Cervical vertebrae[edit | edit source] The atlas and axis are cervical vertebrae 1 and 2. Canine cervical spine The atlanto-occipital joint is a condylar modified synovial hinge joint. The capsule of the joint is strengthened by three thickenings: dorsal, ventral, and lateral.[1] The transverse process of the atlas is the wing that allows the articulation of the occipital condyles and the spine.The atlas and axis are fused in embryonic life.[4] The transverse atlantal ligament holds the dens of the axis against the ventral arch of the atlas.[1] The axis is the second and longest cervical vertebra. The atlantoaxial joint is a pivot joint and has a loose joint capsule. The dens of the axis is connected to the occipital bone through the apical ligament.[1] The cervical vertebrae are obliquely oriented in the transverse plane. The cranial articular processes face dorsomedially whereas the caudal articular processes face ventrolaterally. [1] The nuchal ligament is a paired band of connective tissue that connects the spinous processes of cervical vertebrae to the spinous processes of thoracic vertebra (from C1 to T1).[4][1] The canine ligamentum flavum, dorsal longitudinal ligament and, ventral longitudinal ligament are similar to those in people: The ligamentum flavum connects the lamina of adjacent lamina The anterior longitudinal ligament attaches to the front of each vertebra The posterior longitudinal ligament runs along the posterior aspect of spine and inside of the spinal cord[1] Muscles of the Cervical Spine[edit | edit source] Canine superficial cervical muscles Muscles of the cervical spine (table extracted from a presentation of Ansi Van Der Walt )[1] Muscle Origin Insertion Innervation Action Omotransversarius Lower spine of scapula Wing of atlas Ventral branches of local cervical spinal nerve Advances limb Moves neck laterally Brachiocephalicus [The clavicle divides the muscle into two: cleidobrachialis and cleidomastoideus] Cleidobrachialis Clavicular intersection Crest of the humerus Axillary nerve Advances limb Adducts Limb Cleidomastoideus Clavicular intersection Mastoid process of the temporal bone Ventral branch of the accessory nerve (cranial nerve XI) Forms dorsal border of jugular groove Advances limb Flexes neck Turns head Sternocephalicus (sternomandibularis) Manubrium of the sternum Mastoid part of temporal bone Nuchal crest Forms ventral border of jugular groove Flexes neck Turns head Opens mouth Omohyoideus Subscapular Fascia Lingual process of basihyoid bone Spinal nerve C1 Forms medial border of jugular groove Retracts basihyoid bone and tongue Trapezius (cervical and thoracic parts) Nuchal ligament and supraspinous ligament of C2-10 Cervical part: entire scapular spine Thoracic part: dorsal third of scapular spine Dorsal branch of accessory nerve (cranial nerve XI) Advances thoracic limb Abducts thoracic limb Elevates shoulder Rhomboiudeus muscle (cervical and thoracic) Nuchal ligament and dorsoscapular ligaments of C2-T8 Scapular cartilage Local thoracic nerve Local cervical nerve Elevates neck Draws scapula cranially and dorsally Serratus ventralis cervicis Transverse processes of C4-7 Scapular cartilage and medial scapula Ventral branches of local cervical nerve Supports trunk between forelimbs Raises neck when the limb is fixed Splenius (capitis and cervicis) Nuchal ligament and spinous processes of T3-5 via the thoracolumbar fascia Nuchal crest and the mastoid process of temporal bone Dorsal branch of accessory nerve (cranial nerve XI) and dorsal branch of local spinal nerve Extends neck Elevates neck Bends neck laterally Longissimus (cervicis,capitis, atlantis) Transverse processes of cervical and thoracic vertebrae Wing of atlas and mastoid process of temporal bone Dorsal branches of local spinal nerve Elevates head and neck Bends head and neck laterally Stabilizes and extends vertebral column Semispinalis capitis Articular processes of C2/3-7 and transverse processes of T1-6/7 Occipital bone Elevates head and neck Bends head and neck laterally Longus capitis Transverse processes of C3-5 Mastoid process Ventral branch of local spinal nerve Flexes head Bends head laterally Longus colli thoracic part Bodies of T1-6 Transverse processes of C6-7 cervical part Transverse processes of C3-7 Ventral tubercle of atlas and bodies of cervical vertebrae Flexes head Obliquus capitis caudalis Spinous process of the axis Wings of the atlas Dorsal branch of C2 Rotates atlas and head Rectus capitis dorsalis muscle minor Dorsal arch of the atlas Occipital bone Dorsal branch of C1 Elevates head major Spinous process of the axis Nuchal crest Scalenes (composed of two unequal parts and the lower one is larger) From the transverse process of the last four cervical vertebrae Into the anterior border and outer surface of the first rib Assists inspiration by drawing the first rib forward With rib fixed draws the neck downward and to one side Thoracic Vertebrae[edit | edit source] The thoracic vertebrae differ from other vertebrae in a number of ways. The thoracic vertebrae articulate with the corresponding rib (i.e. T1 to rib 1). Each thoracic vertebra has a short body, flattened extremities, short articular processes and a long spinous process. The caudal articular processes of the thoracic vertebrae face ventrally and are at the base of the spinous process. The cranial articular processes of the thoracic vertebrae are oval facets on the arch of vertebrae and face dorsally. All thoracic vertebrae have a pair of costal facets on the dorsal body (except T13) forming costal fovea. There are costal facets on the transverse processes of the vertebrae and cranial and caudal fovea on the extremities of the vertebral bodies.[5] The 11th thoracic vertebra is also known as the anticlinal vertebra. The anticlinal vertebra is the point at which vertebral anatomic features change and the spinous process becomes perpendicular to the body and the preceding vertebra incline caudally. [6] [7] The costovertebral joint has two articulations between the rib and the vertebral column. The head of the rib articulates with the cranial and costal facets of the adjacent vertebrae and is a ball and socket synovial joint. Similarly, the tubercle of the rib articulates with the transverse process of the vertebra and is a plane synovial joint. The ligaments of the costovertebral joint are the radiate ligament of the head, inter capital ligament (connects the head of the pair of opposite rib), costotransverse ligaments and ligament of the neck.[1] Lumbar spine[edit | edit source] Lumbar vertebrae are more uniform and longer in shape than the thoracic vertebrae.[4] The cranial articular process of the lumbar spine is fused with the mamillary processes and the articular processes are concave dorsally and mostly in sagittal alignment. The caudal processes are convex ventrally and correspond with the convexity of cranial articular processes. The lumbar vertebrae are differentiated from the thoracic vertebrae by their lack of costal facets. The lumbar spine allows flexion and extension of the spine. Lateral flexion and rotation are very limited, especially at the L4-L5 due to the intertransverse joints. [1] Ligaments of the thoracolumbar joint[edit | edit source] The dorsal longitudinal ligament forms a part of the floor of the vertebral canal from the axis to the sacrum and prevents hyperflexion of the spine[1] An interspinous ligament connects the spines of adjacent vertebrae from the axis to the sacrum[1] Intertransverse ligament[1] Interarcuate ligament / ligamentum flavum / yellow ligaments are the elastic ligaments filling dorsal spaces between the arches of adjacent vertebrae[1] The supraspinous ligament is made up of heavy bands of the connective tissue that run over the top of the spinous processes (T2/T3 caudally). This ligament prevents abnormal separation of spinous processes during flexion of the spine. The supraspinous ligament is a direct continuation of the funicular part of the nuchal ligament[1] The ventral longitudinal ligament runs ventrally from axis to sacrum. It widens caudally and is strongest in the lumbar spine. This prevents hyperextension of the spine[1] Sacral vertebrae[edit | edit source] The sacrum is formed by the fusion of the sacral vertebrae and articulates with the pelvic girdle. The sacrum narrows and forms a curve caudally and forms a concave surface for the pelvic cavity.[4] Caudal vertebrae[edit | edit source] The dog caudal vertebrae may vary from eighteen to twenty-five, the number differing from species to species. [4][8] Muscles of the Trunk[edit | edit source] Muscles of the trunk (table extracted from a presentation of Ansi Van Der Walt [1] Muscle Origin Insertion Innervation Action Lattisimus dorsi Supraspinous ligament from T3 and thoracolumbar fascia Teres major tuberosity of humerus Thoracodorsal nerve Flexes shoulder and draws limb caudally Draws trunk cranially when limb is flexed Serratus ventralis thoracis Ribs 1-8/9 Scapular cartilage and medial scapula Long thoracic nerve Supports trunk between forelimbs Raises neck when limb is flexed Serratus dorsalis cranialis Supraspinous ligament Cranial border of ribs 5-11 Intercostal nerve Muscle of inspiration caudalis Thoracolumbar fascia Caudal border of ribs 11-13 Muscle of expiration External intercostal muscles Muscles run caudodorsally in the intercostal spaces Muscles of inspiration Internal intercostal muscles Muscles of expiration External abdominal oblique muscle Thoracolumbar fascia and lateral aspect of ribs 4-13 Linea alba Prepubic tendon Pelvic tendon Coxal tuber Inguinal ligament Ventral branches of lumbar nerve and local intercostal nerve Abdominal press Flexes the trunk Internal abdominal oblique muscle Coxal tuber and inguinal ligament Linea alba, Prepubic tendon last rib Cartilages of ribs 14-18 Ventral branches of lumbar nerve and local intercostal nerve Abdominal press Flexes the trunk Transversus abdominis Medial surface of costal cartilages 7-18 and transverse processes of lumbar vertebrae Linea alba Ventral branches of lumbar nerve and lumbar intercostal nerve Abdominal press Flexes the trunk Rectus abdominis lateral surface of costal cartilages 4-9 Prepubic tendon and head of the femur (via accessory ligament) Ventral branches of lumbar nerve and local intercostal nerve Abdominal press Flexes the trunk Flexes lumbar spine and lumbosacral joint Longisimus thoracis and lumborum Spinous processes of thoracic, lumbar and sacral vertebrae and wings of illium Transverse processes of vertebrae and tubercles of rib Dorsal branches of lumbar nerve Stabilises and extends vertebral column Semispinalis thoracis and lumborum From the sacrum and from the articular processes of the lumbar vertebrae and from the transverse processes of the dorsal vertebrae Each slip inserts into the spinous process of the third or fourth vertebra in front of the one from which it arises Dorsal branches of local spinal nerve To fix the bones during the action of the large spinal muscles, and to assist in extending the spine Iliocostalis thoracis and lumborum Runs obliquely between the transverse processes of the vertebrae to the bodies of the adjacent vertebrae and/or the tuberosities of the rib Dorsal branches of local spinal nerves Expiration Thoracolumbar extension Cutaneous trunci Superficial trunk fascia (from the withers to the fold of the flank) Superficial shoulder fascia and medial surface of the humerus Lateral thoracic nerve and intercostobrachial nerve Moves the skin of the abdomen (and the trunk ) Longissimus thoracis and lumborum muscle are continuous from pelvis through thorax Spinous processes of thoracic, lumbar and sacral vertebrae and wings of illium Transverse processes of vertebrae and tubercles of ribs Dorsal branches of local spinal nerve Stabilises and extends vertebral column Multifidus lumborum muscle (continuous with thoracis and cervicis) Articular processes of each vertebra from C2 to sacrum Spinous process of the preceding vertebra Dorsal branches of local spinal nerve Stabilises vertebral column Rotates vertebral column Psoas major muscle Part of iliopasoas muscle Lumbar transverse processes and ventral surface of last two ribs Lesser trochanter of femur (as fused iliopsoas muscle) Ventral branches of lumbar and local intercostal nerve and lumbar plexus Rotates pelvic limb outwards Flexes hip and advances limb Stabilises vertebral column when limb is fixedEquine Spine and Head Anatomy - PhysiopediaIntroduction Equine anatomy refers to the gross and microscopic anatomy of horses and other equids (donkeys, and zebras). This page introduces the Anatomy of Equine Spine and Head. Axial Skeleton[edit | edit source] The axial skeleton consists of the skull, vertebral column, sternum, and ribs. Multiple sternebrae fuse to form one bone, attached to the 8 "true" pairs of ribs, out of a total of 18.[1] The vertebral column contains 54 bones: 7 cervical vertebrae: includes the atlas (C1) and axis (C2) 18-19 thoracic vertebrae 5-6 lumbar vertebrae 5 sacral vertebrae 15-25 caudal vertebrae[2] In certain breeds, there may be variations in these numbers.[3] Skull[edit | edit source] The skull contains the brain and the most important organs of sense. Cranium[edit | edit source] The Roof of the cranium is made up of frontal and parietal bones. The Floor is made up of sphenoid bone. The cranium consists of 5 orbital regions: Frontal Lacrimal Palatine Sphenoid Zygomatic Interparietal bone: only found in horse and cat. The orbit is complete in horse and ruminants while it is incomplete in carnivores but completed by the orbital ligament. The lacrimal fossa collects tears and sends them through lacrimal canal into the nasal cavity. Bones in the Equine Skull[edit | edit source] There are 34 bones and most of them are flat. During the birth process, these bones overlap and allow the skull to compress as much as possible to allow for parturition. The 14 major bones are:[1] Incisive bone (premaxillary): part of the upper jaw; where the incisors attach Nasal bone: covers the nasal cavity Maxillary bone: a large bone that contains the roots of the molars Mandible: lower portion of the jaw; largest bone in the skull Lacrimal bone: contains the nasolacrimal duct, which carries fluid from the surface of the eye, to the nose Frontal bone: creates the forehead of the horse Parietal bone: extends from the forehead to the back of the skull Occipital bone: forms the joint between the skull and the first vertebrae of the neck (the atlas) Temporal bone: contains the eternal acoustic meatus, which transmits sound from the ear to the cochlea (eardrum) Zygomatic bone: attaches to the temporal bone to form the zygomatic arch (cheekbone) Palatine bone: forms the back of the hard palate Sphenoid: formed by fusion of the foetal basisphenoid and presphenoid bones, at the base of the skull. Can become fractured in horses that rear over backwards Vomer: forms the top of the inside of the nasal cavity Pterygoid: small bone attached to the sphenoid that extends downward Cavities[edit | edit source] The equine skull consists of 4 cavities: The cranial cavity: Protects and encloses the brain, supports sense organs. The cranium consists of a roof made up of the frontal and parietal bones and a floor made up of the sphenoid bone The orbital cavity: Has 5 orbits: frontal, lacrimal, palatine, sphenoid and zygomatic. It protects and surrounds the eye.[4] Horses have both monocular and binocular vision: Monocular vision: The horse can see objects with one eye. This means that the brain receives two images simultaneously Binocular vision: The horse can focus with both eyes just like humans and the brain receives only one signal The oral cavity: A passage into the respiratory and digestive system The nasal cavity: Contains bone that protects the mucous membrane from inspired warm air Foramina of the Skull and the Structures Passing Through[edit | edit source] Foramina Structures passing through Infra-orbital foramen Infra-orbital nerve. CNV Maxillary foramen Cribriform foramen Olfactory nerve. CNI Optic canal Optic nerve. CNII Orbital fissure CNVII, IV, V and VI (ophthalmic division) Round foramen CNV (maxillary division) Oval foramen CNV (mandibular division) Foramen lacerum Internal carotid artery CN V3 (horse and pig) Internal acoustic meatus CNVIII Jugular foramen CNIX, X, XI Stylomastoid foramen CNVII Mandibular foramen CNV (mandibular alveolar nerve) Mental foramen Joints and Ligaments[edit | edit source] Joints and Ligaments of the Skull[edit | edit source] The temporo-mandibular joint - a condylar joint between the mandibular condyles and the mandibular fossae of the temporal bones. It has a loose joint capsule with thickenings that form a lateral ligament, as well as an articular disc[1] Mandibular symphysis Hyoid apparatus - consists of three joints: Tympanohyoid cartilage- skull (syndesmosis) Interhyoid joints (synovial) Thyrohyoid bone- cranial cornu of thyroid cartilage (synovial)[1] [5] Cervical Spine[edit | edit source] Joints[edit | edit source] Atlanto-Occipital Joint[edit | edit source] A condylar, modified synovial hinge joint. The articulating surfaces are the occipital condyles and the cranial articular surfaces of the atlas (C1). There are three thickenings that strengthen the spacious joint capsule: Dorsal, Ventral, Lateral. The transverse atlantal ligament holds the dens of the axis against the ventral arch of the atlas.[1] Atlanto-Axial Joint[edit | edit source] A pivot joint between the atlas and the saddle shaped surface of the axis (C2), which extends upon the dens. It has a loose joint capsule. The apical ligament of dens connects the apex of the dens to the occipital bone. Motion at this joint includes rotation of the atlas and head upon the axis and some accessory lateral flexion.[1] Rotation at this joint makes up 73 percent of cervical rotation.[6] Cervical Spine C3-C4[edit | edit source] A planar, extensive, oval shaped joint that is obliquely oriented in transverse plane. The cranial articular processes face dorsomedially and the caudal articular processes face ventrolaterally. Spinous process height increases caudally from C6. Lateral flexion is the primary motion at these joints (25-45 degrees each joint - C1/C2 only has 3.9 degrees of lateral flexion).[6] Ligaments[edit | edit source] Dorsal longitudinal ligament Ventral longitudinal ligament Ligamentum flavum Nuchal ligament: This ligament connects the thoracic vertebra to the head and assists in supporting its weight. It consists of two paired parts:[1] Funicular (cord) part - extends from the poll to +/- the second to the fourth thoracic spinous process Lamellar part - arises from the second and third thoracic spinous processes and the funicular part, and inserts on the C2-C6 spinous processes. The first digitation going to the axis is very strong, but it decreases in strength caudally Thoracic Spine (T1-T18)[edit | edit source] Articular processes[edit | edit source] Caudal articular processes face ventrally and are positioned at the base of the spinous process. The cranial articular processes are oval facets on the arch of the vertebra and face dorsally. Each thoracic vertebrae has a pair of costal facets on the dorsal body (except the last) forming the costal fovea.[1] Anticlinal vertebrae: This is the point in the caudal thoracic vertebral column at which the anatomic features of the vertebra start to change.[7] This usually occurs at the 13th vertebra in horses. Motion: Flexion - most flexion occurs at T17/T18; least flexion occurs at T3-T9 Extension - most extension occurs at T14-T18; least extension occurs at T2-9[1] Rib Neck[edit | edit source] Has 2 converse facets: Cranial and Caudal Rib 1 attaches to C7, T1 and the associated IV disc Motion: rotation of the rib, which is greater caudally Costovertebral Joint[edit | edit source] Joints[edit | edit source] The costovertebral joints have two distinct articulations between most ribs and the vertebral column:[1] Head of the rib: Cranial and caudal costal facets of adjacent vertebrae; a ball and socket synovial joint Tubercle of the rib: Transverse process of vertebrae; a plane synovial joint Ligaments[edit | edit source] Radiate longitudinal ligament Intercapital ligament Costotransverse ligament Ligament of the neck Lumbar Spine[edit | edit source] Joints[edit | edit source] Horses usually have 6 lumbar vertebrae (L1-L6), but some arabian horses only have 5 (L1-L5).[1] Articular processes[edit | edit source] Cranial articular processes are fused with mammillary processes. They are concave dorsally and mostly in sagittal alignment. Caudal processes are convex ventrally and correspond with the convexity of the cranial articular processes. They are differentiated from the last thoracic vertebra by the lack of costal facets.[1] Motion: The lumbar spine and caudal thoracic spine are the least mobile regions of a horse's back.[8] Lateral flexion and rotation is very limited especially at L4-L6 due to intertransverse joints.[1] Ligaments of Thoraco-Lumbar Spine[edit | edit source] Supraspinous ligament: A heavy band of connective tissue running over the top of spinous processes ( T2/T3 caudally). It prevents abnormal separation of spinous processes during flexion Ventral longitudinal ligament: Marks the ventral surface of vertebrae from the axis to the sacrum. It is strongest and widest caudally. It plays a major role in preventing overextension of the spine Dorsal longitudinal ligament: Extends from the floor of the vertebral canal from the axis to sacrum and helps to prevent spine hyper-flexion Annulus fibrosis of IVD: Thick ventrally Intertransverse ligament Interarcuate ligament/ yellow ligament/ ligamentum flavum: An elastic ligament that fills the dorsal space between the arch of the adjacent vertebra[1] Lumbosacral Joint[edit | edit source] The cranial articular process of the first sacral vertebra are concave and face dorsomedially. Motion: Flexion and Extension - 23.4 degrees[9] Sacrum[edit | edit source] The sacrum consists of fused sacral vertebrae and has dorsal and ventral sacral foramina. [10] Myology and Neurology[edit | edit source] Muscles of the Head[edit | edit source] Muscles of the Face[edit | edit source] The muscles of facial expressions are innervated by the motor fibers of CNVII (facial nerve).[1] Muscle Origin Insertion Action M. Levator labii maxillaris Lacrimal, Zygomatic and Maxillary bones The maxillary lip Elevates the Maxillary lip M. Levator nasolabialis Nasal and Frontal bones The lateral wing of nostril The maxillary lip Elevates and retracts the angle of the mouth M. Zygomaticus The fascia covering the Masseter The commissure of the lips M. Buccinator Maxilla and Mandible Flattens the cheeks and thus presses food between the teeth M. Depressor labii mandibulars The alveolar border of the Mandible The mandibular lip Depresses and retracts the mandibular lip M. Orbicularis oris The sphincter muscle of the skin and the muscles of the lips Corner of the mouth Into the lips as it surrounds the mouth Closes the mouth M. Risorius Part of M. cutaneous faciei The angle of the mouth Retracts the angle of the mouth M. Dilator naris Alar cartillage Alar cartillage Dilates the nostril M. Lateralis nasi Dorsal part Nasal bone Parietal cartilage Dilates the nostril and nasal vestibule Ventral part Nasal process of Incisive bone Lateral wall of the Nasal vestibule M. Caninus Maxilla close to the rostral extremity of the facial crest Lateral wing of the nostril Dilates the nostril laterally M. Levator nasolabialis Frontal and Nasal bones Lateral wing of the nostril Elevates the maxillary lip and the commissure of the mouth Dilates the nostril Ear[edit | edit source] The ear is an organ of hearing and balance. It consists of the outer, middle, and inner ear. Outer Ear[edit | edit source] The outer ear includes:[1] Pinna: mobile and can move independently - can hear multiple sounds at the same time[11] Ear canal Cartilage: Cartilages of the ear collect and transmit sound to the essential organ of hearing within the temporal bone. In order to achieve this, they (especially the concha) need to move.[1] The muscles of outer ear:[1] Rostral Dorsal Caudal Ventral There are 3 cartilages:[1] Conchal: Forms the framework of the portion of the ear which stands erect. It has a large vertical opening on one side to receive sound, and is attached below to the annular cartilage Annular: A small ring of gristle connected to the auditory process of the petrous temporal bone Scutiform: A small, flat and somewhat triangular cartilaginous plate situated in front of the base of concha, to which it is attached Middle Ear[edit | edit source] The middle ear includes:[1] Eardrum Small, air-filled chamber containing 3 tiny bones: the hammer, anvil, and stirrup. It also includes 2 muscles: the oval window, and the eustachian tube. Inner Ear[edit | edit source] The inner ear is a complex structure that includes the cochlea and the vestibular system.[11] Muscles of Mastication[edit | edit source] The muscles of mastication are innervated by the mandibular branch of trigeminal nerve CNV.[1] Muscle Origin Insertion Action M. Masseter The zygomatic arch and the facial crest The lateral border of the ramus of the mandible Closes the mouth M. Temporalis The temporal fossa and the temporal crest The coronoid process of the mandible Closes the mouth (to raise the mandible) M. Pterygoideus medialis The crest formed by the pterygoid processes of the basisphenoid and the palatine bones The medial surface of the ramus of the mandible M. Pterygoideus lateralis The pterygoid process of the sphenoid bone Rostral border of the condyle of the mandible Draws and moves the mandible rostrally M. Digastricus The jugular process of occipital bone Medial surface of the ventral border of the molar part of the body of the mandible Opens the mouth M. Occipitomandibularis The jugular process The caudal border of the ramus of the mandible Muscles of the Eyes[edit | edit source] M. Orbicularis oculi - innervated by palpebral branch of CN VII M. Levator palpebrae superioris - originates from the posterior orbit and inserts at orbicularis oculi fibers of the lower eyelid. It elevates the upper eyelid and is innervated by CN III (oculomotor nerve) M. Malaris - lowers the ventral eyelid. It is innervated by CN VII (facial nerve) Muller's muscle - innervated by sympathetic nerves Ciliary muscles M. Retractor anguli - retracts and anchors the lateral canthus M. Levator anguli oculi medialis and M. Frontalis - slightly elevates of the upper eyelid[12][13] Muscles of the Tongue[edit | edit source] The equine tongue is made up of twelve different muscles[14] including styloglossus, genioglossus and hyoglossus. These muscles are covered by mucosa on the sides and underneath.[1] Action: prehension, mastication (i.e. chewing) Innervation: Hypoglossus (CNXII) Muscles of Pharynx and Soft palate.[edit | edit source] [15][16] Muscle Origin Insertion Action Innervation INTRINSIC MUSCLES M. Tensor veli palatini Muscular process of the petrous part of the temporal bone, pterygoid bone, and lateral lamina of the auditory tube Palatine aponeurosis Retracts the soft palate away from the dorsal pharyngeal wall, expanding the nasopharynx and slightly depressing it ventrad during inspiration Mandibular branch of the trigeminal nerve M. Levator veli palatini Muscular process of the petrous part of the temporal bone and the lateral lamina of the Auditory tube and passes along the lateral wall of the nasopharynx Soft palate dorsal to the glandular layer Elevates the soft palate during swallowing Pharyngeal branch of the Vagus nerve M. Palatinus Caudal aspect of the palatine aponeurosis Caudal free margin of the soft palate Shortens the soft palate and depresses it towards the tongue M. Palatopharyngeus Palatine aponeurosis and from the palatine and pterygoid bones Upper edge of the thyroid cartilage M. Stylopharyngeus Rostral Medial surface of the rostral end of the Stylohyoid bone Pharyngeal raphe Pharyngeal constrictor Glossopharyngeal nerve Caudal Medial aspect of the caudal third of the Stylohyoid bone Dorsolateral wall of the pharynx Pharyngeal dilator EXTRINSIC MUSCLES M. Genioglossus Median plane of the Tongue Oral surface of the Mandible Protracts the tongue Hypoglossal nerve M. Geniohyoideus Medial surface of the Mandible Basihyoid bone Protrudes the tongue M. Thyrohyoideus Lateral lamina of the Thyroid cartilage Caudal aspect of the thyrohyoid bone Moves the larynx rostrad M. Hyoglossus Hyoid bones Median plane of the dorsum of the tongue Retracts and depresses the base of the tongue M. Hyoepiglotticus M. Styloglossus Lateral aspect of the stylohyoid bone Tip of the tongue Retraction of the tongue M. Sternohyoideus Sternal manubrium Basihyoid bone and lingual process of the hyoid apparatus Caudal traction Branches of the first and second cervical nerves M. Sternothyroideus Caudolateral aspect of the thyroid cartilage Muscles of the Hyoid Apparatus and Larynx[edit | edit source] Muscles of the hyoid apparatus and larynx are innervated by CNX. Hyoid Apparatus[edit | edit source] The hyoid apparatus has muscular connections from the throat to the forelimbs, shoulder, and sternum. Sternohyoid and omohyoid provide a direct connection from the hyoid apparatus to the shoulder of the horse via the ventral neck. The tongue connects to the hyoid apparatus. Small muscles of the hyoid apparatus connect to the TMJ and the poll and the TMJ articulates with the hyoid apparatus.[17][18] Larynx[edit | edit source] Intrinsic muscles: Cricoarytenoideus dorsalis - abduction of arytenoids and tensing of vocal cords Thyroarytenoideus - adduction of arytenoids Arytenoideus transversus - adduction of arytenoids Cricoarytenoideus lateralis - adduction of arytenoids[19] Muscles of Cervical spine[edit | edit source] [20][21] Muscle Origin Insertion Action Innervation M. Omotransversarius Fascia of shoulder Scapular cartilage and transverse processes of C2-4 Advances limb Adducts limb Moves neck laterally Ventral branch of local cervical spinal nerve M. Brachiocephalicus Mastoid process of temporal bone and first cervical vertebra Deltoid tuberosity and crest of the humerus Shoulder extension Protraction Flexion of the neck towards the side of the protracting limb Accessory nerve M. Cleidobrachialis Inscription of clavicle Crest of the humerus Advances limb Adducts limb Axillary nerve M. Cleidomastoideus Clavicular intersection Mastoid process of temporal bone Advances limb Flexes neck Turns head Ventral branch of Accessory nerve (cranial nerve XI) M. Sternocephalicus (Sternomandibularis) Manubrium of the sternum Caudal border of mandible Turns head Opens mouth M. Omohyoideus Subscapular fascia Lingual process of basihyoid bone Retracts basihyoid bone and tongue Spinal nerve C1 M. Trapezius Nuchal ligament and Supraspinous ligaments of C2-10 Cervical part: Entire scapular spine Advances thoracic limb Abducts thoracic limb Elevates shoulder Dorsal branch of Accessory nerve (cranial nerve XI) Thoracic part: Dorsal third of Scapular spine M. Rhomboideus (cervicis and thoracis) Nuchal ligament and dorsoscapular ligaments of C2-T8 Scapular cartilage Elevates neck Draws scapula cranially and dorsally Local thoracic nerve and Local cervical nerve M. Serratus ventralis (cervicis) Transverse processes of C4-7 Scapular cartilage and medial scapula Supports trunk between forelimbs Raises neck when the limb is fixed Ventral branch of local cervical nerve M. Splenius (capitus and cervicis) Nuchal ligament and spinous processes of T3-T5 Nuchal crest and mastoid process of temporal bone Extends neck Elevates neck Bends neck laterally Dorsal branch of Accessory nerve and dorsal branch of local spinal nerve M. Longissimus (cervicis, capitus, atlantis) Transverse processes of cervical and thoracic vertebrae Wing of atlas and mastoid process of temporal bone Elevates head and neck Bends head and neck laterally Stabilizes and extends vertebral column Dorsal branch of local spinal nerve M. Semispinalis capitis Articular processes of C2/3-7 and transverse processes of T1-6/7 Occipital bone Elevates head and neck Bends head and neck laterally M. Longus capitis Transverse processes of C3-5 Base of skull Bends head and neck Ventral branch of local spinal nerve M. Longus colli Cervical part Transverse processes of C3-7 Ventral tubercle of atlas and bodies of cervical vertebrae Flexes head Thoracic part Bodies of T1-6 Transverse processes of C6-7 Flexes head Bends head laterally M. Obliqus capitis caudalis Spinous process of the axis Wing of the Atlas Rotates atlas and Head Dorsal branch of C2 M. Rectus capitis dorsalis Major Nuchal crest Elevates head Dorsal branch of C1 Minor Dorsal arch of the atlas Occipital bone M. Scalenes Transverse processes of the last 4 cervical vertebrae Anterior border and Outer surface of the first rib Assists inspiration by drawing the first rib forward. With the rib fixed, draws the neck downward and to one side. Cervical nerves Muscles of Trunk[edit | edit source] Muscles Origin Insertion Action Innervation M. Latissimus dorsi Supraspinous ligaments from T3 and thoracolumbar fascia Teres major tuberosity of humerus Flexes shoulder and draws limb caudally. Draws trunk cranially when the limb is flexed. Thoracodorsal nerve M. Serratus ventralis (thoracis) Ribs 1-8/9 Scapular cartilage and Medial scapula Supports trunk between forelimbs. Raises neck when the limb is flexed. Long thoracic nerve M. Serratus dorsalis Cranialis Supraspinous ligament Cranial border of ribs 5-11 Inspiration Intercostal nerve Caudalis Thoracolumbar fascia Caudal borders of ribs 11-18 Expiration M. External intercostal Muscles run caudodorsally in the intercostal spaces Inspiration Intercostal nerve M. Internal intercostal Muscles run cranioventrally in the intercostal spaces Expiration M. External abdominal oblique Thoracolumbar fascia and lateral aspect of ribs 4-18 Linea alba Prepubic tendon Pelvic tendon Coxal tendon Inguinal ligament Flexes the trunk Ventral branch of lumbar nerve and local intercostal nerve M. Internal abdominal oblique Coxal tuber and inguinal ligament Linea alba Prepubic tendon Last rib Cartilages of ribs 14-18 Flexes the trunk Ventral branches of lumbar nerve and local intercostal nerve M. Transversus abdominis Medial surface of Costal cartilage 7-18 and transverse processes of lumbar vertebrae Linea alba M. Rectus abdominis Lateral surface of costal cartilages 4-9 Prepubic tendon and the head of the femur Flexes the trunk Flexes lumbar spine and lumbosacral joint M. Longissimus thoracis et lumborum Spinous processes of thoracic, lumbar and sacral vertebrae and wing of ilium Transverse processes of vertebrae and tubercles of ribs Stabilizes and extends vertebral column Dorsal branch of local spinal nerve M. Semispinalis thoracis and lumborum Sacrum, the articular processes of the lumbar vertebrae and the transverse processes of the dorsa vertebrae Spinous processes of third or fourth vertebra in front of the one from which it arises Fixes the bone during the action of the large spinal muscle, and assists in spine extension M. Iliocostalis thoracis and lumborum Transverse processes of vertebrae Bodies of the adjacent vertebrae and/or the tuberosities of the ribs Expiration Thoracolumbar extension M. Cutaneous trunci Superficial trunk fascia Superficial shoulder fascia and medial surface of humerus Moves the skin of the abdomen Lateral thoracic nerve and intercostobrachial nerve M. Multifidus lumborum Articular processes of each vertebra from C2 to sacrum Spinous process of the preceding vertebrae Stabilizes and rotates vertebral column Dorsal branches of local spinal nerve M. Psoas major Lumbar transverse processes and ventral surface of the last two ribs Lesser trochanter of Femur Rotates pelvic limb outward Flexed hip Advances limb Stabilizes vertebral column when limb is fixed Ventral branches of lumbar and local intercostal nerve and lumbar plexus [22]Functional Anatomy of the Thoracic Spine and Rib Cage - PhysiopediaIntroduction Key Terms[edit | edit source] Axes: lines around which an object rotates. The rotation axis is a line that passes through the centre of mass. There are three axes of rotation: sagittal passing from posterior to anterior, frontal passing from left to right, and vertical passing from inferior to superior. The rotation axes of the foot joints are perpendicular to the cardinal planes. Therefore, motion at these joints results in rotations within three planes. Example: supination involves inversion, internal rotation, and plantarflexion. Bursae: reduce friction between the moving parts of the body joints. A bursa is a fluid-filled sac. There are four types of bursae: adventitious, subcutaneous, synovial, and sub-muscular. Capsule: one of the characteristics of the synovial joints. It is a fibrous connective tissue which forms a band that seals the joint space, provides passive and active stability and may even form articular surfaces for the joint. The capsular pattern is "the proportional motion restriction in range of motion during passive exercises due to tightness of the joint capsule." Closed pack position: the position with the most congruency of the joint surfaces. In this position, joint stability increases. For example, the closed pack position for the interphalangeal joints is a full extension. Degrees of freedom: the direction of joint movement or rotation; there is a maximum of six degrees of freedom, including three translations and three rotations. Ligament: fibrous connective tissue that holds the bones together. Open (loose) pack position: position with the least joint congruency where joint stability is reduced. Planes of movement: describe how the body moves. Up and down movements (flexion/extension) occur in the sagittal plane. Sideway movements (abduction/adduction) occur in the frontal plane. The transverse plane movements are rotational (internal and external rotation). Thoracic Spine Structure[edit | edit source] Twelve thoracic vertebrae located in the middle of the spine make up the thoracic spine. Thoracic vertebrae have costal facets for articulation with the ribs and longer spinous processes that are directed posteroinferiorly. The positioning of the ribs and the spinous processes limit the amount of flexion and extension range of motion of the thoracic spine. Vertebral compression fractures where the vertebral body collapses are seen most frequently in the thoracic spine and are often related to osteoporosis. Four different movements occur in the thoracic spine: flexion, extension, lateral flexion, and rotation. Each thoracic vertebra contains the following structural elements: Vertebral body Thoracic vertebrae[edit | edit source] Thoracic Kyphosis[edit | edit source] Rib Cage Structure[edit | edit source] There are 12 pairs of ribs articulating with the thoracic spine posteriorly and the sternum, or breast bone, anteriorly to make up the rib cage. They are classified into three groups. Ribs one to seven are true ribs, which directly articulate with the sternum through their costal cartilage. Ribs eight to 10 are false ribs, which indirectly articulate with the sternum via rib seven's costal cartilage. And ribs 11 and 12 are floating ribs that do not articulate with a sternum at all. Rib fractures can be one of the causes of a pneumothorax, where air enters the pleural cavity between the lung and the chest wall, causing the lung to collapse. Bones, Articulations and Kinematics of the Thoracic Spine[edit | edit source] Bones and Articulations[edit | edit source] Kinematics[edit | edit source] Thoracic Spine Ligaments[edit | edit source] Muscles of the Thoracic Spine and Rib Cage[edit | edit source] Innervation of the Thoracic Spine and Rib Cage[edit | edit source] Vascular Supply of the Thoracic Spine and Rib Cage[edit | edit source] Resources[edit | edit source] bulleted list x or numbered list xLumbar Spine Fracture - PhysiopediaDefinition/Description The complex shape of the vertebrae, along with the interaction of the central nervous system, the relatively specialized structures of the intervertebral disks and the associated vertebral ligaments has made the description and classification of spinal fractures an ongoing pursuit for the medical community. The current system had its roots in 1963 after Holdsworth proposed classifying spinal fractures by the mechanism of injury (MOI) of compression, flexion, extension and flexion-rotation. He divided the injuries according to the involvement of the anterior weight-bearing column and the posterior “tension bearing” column of facet joints and ligament complex.[1] The 1983 Denis system revision led to a center column comprised of the posterior vertebral body, posterior vertebral disk and posterior longitudinal ligament.[2] In the Denis system, it was believed that trauma focused on the middle column was sufficient to cause instability in the spine. The instability was further categorized into three types: First degree: considered mechanical Second degree: neurological Third degree: combined mechanical/neurological This system is still currently the favoured method. The main frustration with the Denis method is that the inclusion of the middle column introduced a “virtual landmark” that isn’t really suitable for determining an injury type because it is not an anatomic entity. A recently developed system by Aebi incorporates the two-column method, combined with the method of injury, and the instability which may result in neurological compromise.[3] This method works with grades of severity, increasing from type A to type B and type C. Every type has another subdivision of grade 1 to 3, also going in increasing order of severity. In this way, we have nine basic injury types which can be even further specified into 27 subgroups of spinal fractures[3].[3] Obviously the classification of fractures is complicated and ongoing. Clinically Relevant Anatomy[edit | edit source] Lumbar spine fractures, as the name suggests, are always located in the lumbar spine. The lumbar spine is the part of the spine located in the lower back and is a common painful area in physiotherapy. It is situated in between the thoracic and the sacral part of the spine and is characterised by lordosis. The lumbar spine consists of five vertebrae that are simultaneously strong and articularly flexible to give the ability to move the body in different planes such as flexion-extension, rotation and lateral flexion. A lumbar vertebra consists of; a large anterior body which bears most of the weight that is placed on the spine massive dorsal vertebral arches which protect the neural structures (spinal cord) lying inside the vertebral foramen (space between the body and the arches) several types of processes, on which many muscles and ligaments attach the pedicle and facet joints, which are other weight-bearing structures In between the vertebrae, there are intervertebral discs, which support the weight-bearing task of the vertebral bodies and act as shock-absorbers. Another function of these discs is that they connect the vertebral bodies to each other. Epidemiology /Etiology[edit | edit source] “In 2005, osteoporosis was responsible for more than 2 million fractures; approximately 547,000 of those were vertebral fractures. Approximately one-third of osteoporotic vertebral injuries are lumbar, one-third are thoracolumbar, and one-third are thoracic in origin. Additionally, 75% of women older than 65 years who have scoliosis have at least one osteoporotic wedge fracture.”[4] The American Academy of Orthopedic Surgeons website lists fractures based on the pattern of injury and in a simpler format: The flexion pattern contains compression fractures and axial burst fractures. The extension pattern, which contains flexion/distraction (often called a chance fracture). The rotation pattern contains transverse process and fracture-dislocation.[5] Nowadays, fractures are divided into type A, B or C fractures. These are actually the same as the ones described above. Although sufficiently powerful studies about the epidemiology of lumbar spine fractures are lacking, several studies acknowledge osteoporosis as the underlying cause of many lumbar fractures, especially in postmenopausal women. Cooper et al. found an age-adjusted incidence rate of 117 per 100,000 in women that was almost twice of that in men (73 per 100,000). Of all fractures, 14% followed severe trauma, 83% followed moderate or no trauma and 3% were pathologic. Incidence rates for fractures following moderate trauma were higher in women than in men and rose steeply with age in both genders. In contrast, fractures following severe trauma were more frequent in men, and their incidence increased less with age. One should keep in mind that this study did not specify the localisation (cervical, thoracic, lumbar) and type of fracture.[6] Type A fractures- compression (flexion pattern): Failure of the anterior column to resist compression. Burst fractures (Type A3) are the most frequent and severe type of Type A fractures. They are characterised by the increase of the interpedicular distance and the loss of the height of the vertebral body. There is another subdivision of A3.1 Incomplete, A3.2 Complete and A3.3 Burst split fractures. The complete burst fracture involves both endplates, the superior one as well as the inferior one. Compression fractures are usually caused by an axial load on the anterior part of the vertebrae. Due to this vertical force, this specific part of the vertebrae will lose height and will become wedge-shaped.[5] Axial Burst fractures are also caused by an axial load on the vertebrae, but the difference with the compression fractures is that the vertebra is crushed in every direction and therefore also spreads out in every direction. This implies that this kind of fracture is far more dangerous than a compression fracture because of the risk of the bony margins injuring the spinal cord. These kinds of fractures are typically seen in motor accidents or falls from heights.[7] Burst fractures may result in some retropulsion of the vertebra into the vertebral canal.[7] Type B fractures- distraction (extension pattern): Failure from the posterior column to resist distraction B1-lesions are lesions in which the posterior ligament is disrupted but without the involvement of relevant bony elements. The B2-lesions are basically bony seat belt injuries also called Chance fractures. B3-lesions are lesions who are to be found in the anterior column, producing very typical fractures. A Chance fracture results from a flexion-distraction movement e.g an emergency car stop in which the force of the seat belt pulls the vertebrae apart. For this reason, chance fractures are also called ‘seatbelt fractures’ and are often associated with intra-abdominal injuries. Chance fractures involve all three spinal columns. The vertebral body suffers a flexion injury while the posterior elements suffer a distraction type injury.[8] If this type of injuries remain unnoticed, it may result in progressive kyphosis with pain and deformity. Type C- rotation: Results in disrupted posterior tension banding system and a disruption of the anterior column with a rotational dislocation.[3] Transverse process (TP) fractures are uncommon and result from extreme sideways bending. These do not usually affect stability. The fracture-dislocation is a fracture in which bone and its accompanying soft tissue will move off an adjacent vertebra. This type is an unstable fracture and may cause severe spinal cord compression. “C1 lesion is a rotational injury combined with a typical anterior lesion. The C2 lesion is a rotational injury with a typical B type lesion and the C3-lesion is characterised by multilevel and shear injuries with a big variety and quite rare forms in their appearance.”[3] Essential characteristics of the three injury types; Type A, compression injury of the anterior column. Type B, two-column injury with either posterior or anterior transverse disruption. Type C, two-column injury with rotation. Classification A B C (according to M. Aebi, V. Arlet, J.K. Webb, in AO-Manual of Spine Surgery, Vol. I, 2008. Thieme Publisher, Stuttgart) The analysis of a whole collective of injuries learned us that there is a dominance of the injuries at the thoracolumbar junction with the most frequent fractures at L1, second frequent at T12, third frequent at L2, fourth frequent at L3. Injuries of the T10 and L4 vertebrae are of the same frequency along with injuries of T5, 6, 7 and 8.[3][9] While the listed examples above all imply trauma for a spinal fracture, osteoporosis and conditions such as osteogenesis imperfecta are commonly implicated in vertebral fractures as well. Characteristics/Clinical Presentation[edit | edit source] Fractures of the lumbar spine and at the thoracolumbar junction are quite common. Per definition, in compression type fractures the anterior column is affected, whereas in burst fractures, anterior and middle column and sometimes the posterior column, are involved. Compression type fractures are predominately caused by indirect hyperflexion and bending forces whereas burst type fractures result from axial loading.[10] More than 65% of vertebral fractures may not cause recognizable symptoms and may be undiagnosed with radiographs.[11] Patients could have neurologic involvement, may have low back pain, movement may be impaired, or a combination of all of them. When the spinal cord is also involved, numbness, tingling, weakness, or bowel/bladder dysfunction may occur.[5] Upon inspection of the spine, the patient typically has a kyphotic posture that cannot be corrected. The kyphosis is caused by the wedge shape of the fractured vertebra; the fracture essentially turns the lateral conformation of the vertebra from a square to a triangle.[12] A useful tool for the classification of thoracolumbar injuries is ‘the Thoraco-Lumbar Injury Classification and Severity(TLICS) classification system’. Recent studies have raised concerns regarding the reliability of both the Denis and the AO systems, which have been previously mentioned. Both systems have moderate inter- and intra-observer reliability, due to the complex subtypes within each system. This shows that increased complexity of the classification system often leads to less reliability in the clinical setting. The Thoraco-Lumbar Injury Classification and Severity (TLICS) scale, developed by the Spine Trauma Study Group (STSG), works with three “primary axes”:[13] Injury morphology Integrity of the posterior ligamentous complex (PLC) Neurological status.[13] The three primary axes are further divided into a limited number of easily recognizable subgroups, further defining a particular injury from least to most significant.[14] The interpretation of the TLICS severity score is simple. Lesser point values are assigned to the less severe or less urgent injuries and greater point values are assigned to more severe or more urgent injuries. In general, severity is used to indicate the extent of injury to the bony and ligamentous elements of the spine.[15] The TLICS system has proven helpful in guiding surgical treatment. The scores of the three primary axes are summed to yield a total severity score. This score can generally predict the need for surgical intervention. Generally speaking, a total score >5 requires surgical treatment whereas a score <3 can be treated non-operatively. The reliability and the validity have been investigated extensively. Since the introduction of the classification system it underwent a series of modifications. The most recent version of the system has proven to be both valid and reliable by multiple studies, Rampersaud et al. (2006) performed a multi-center reliability study which shows that the TLISS establishes a consensus-based algorithm for treating thoracolumbar injuries.[16] Patel et al. (2007) also showed the validity of the system in a prospective study.[17] The main goal of this study was to evaluate the time-dependent changes in inter-observer reliability. They found that there was a substantial improvement at the second assessment, this suggests that the classifications system can be taught efficiently. There are even more studies analyzing the reliability and the validity and all show positive results. Therefore we can conclude this system can be incorporated in daily practice.[15] Differential Diagnosis[edit | edit source] Coccyx pain Lumbar Facet Arthropathy Mechanical Low Back Pain ( Non-Specific Low Back Pain) Lumbar Degenerative Disc Disease - process in which the intervertebral discs of the lumbar region lose height and hydration. Lumbar Spondylolysis - a uni- or bilateral bony defect in the pars interarticularis or isthmus of the vertebra Golden standard: a combination of SPECT and (CT). MRI is a valuable tool for diagnosing as well, as T1-weighted MR images have been proven useful in the early diagnosis of spondylolysis. In addition, MRI allows spondylolysis to be diagnosed without ionizing radiation Lumbar Spondylolisthesis Osteoporosis - a disease characterized by a decrease in bone density (mass and quality) Diagnostic Procedures[edit | edit source] Although historically the golden standard for diagnosing spine fractures has been plain radiography, Spiral Computed Tomography (SCT) is being used with increasing frequency. Computed Tomography is more sensitive than plain radiographs for evaluation of the Thoracolumbar spine after trauma. In addition, Computed Tomography can be performed faster.[18] According to one study by Brown et al. SCT of the spine identified 99.3% of all fractures of the cervical, thoracic and lumbar spine. Those missed by the SCT required minimal or no treatment. SCT is a sensitive diagnostic test for the identification of spinal fractures.[19] A more recent study by Ang et al[20] concluded that 3-T Magnetic Resonance Imaging (MRI) with thin-slice 3D T1 VIBE is 100% accurate in diagnosing complete pars fractures and has excellent diagnostic ability in the detection and characterisation of incomplete pars stress fractures compared to CT. MRI has the added advantages of detecting bone marrow edema and does not employ ionizing radiation. One disadvantage is that MRI may be substantially more costly than CT for some institutions.[20] Outcome measures[edit | edit source] To assess if the treatment is working or has worked one can take an x-Ray and evaluate the bone mineral density. Subjectively, a therapist notices progression with various tests that determine the ROM and strength. The measurements can also be taken by other tests. Clinical examination[edit | edit source] Whilst height loss is normal with aging due to the compression over the years on the intervertebral disks, it can also be an indicator for a fracture of the spine. Without radiographic imaging it is uncertain there is a fracture. Therefore one should take radiographic imaging to be completely certain of a fracture.[21] When confronted by an acute case of a lumbar fracture the patient needs emergency treatment because the extend of the injury is not known. A doctor should do a full body exam to make sure the fracture did not cause any other damage. It is of grave importance the doctor performs neurological tests as well as imaging tests. The neurological tests evaluate if the patient has suffered damage to the spinal cord or nerves that originate in the lumbar region. the tests consist of moving, feeling and sensing the limbs in different positions and testing of the reflexes of the patient. The imaging tests consist of X-rays, CT scans and MRI depending on the extent of the trauma that is suffered.[22] Radiologists should take a proactive role in helping to diagnose spinal fractures. The failure to diagnose vertebral fracture is a worldwide problem due in part to the lack of fracture recognition by radiologists and the use of ambiguous terminology in radiology reports.[21] Physical therapists can also be more engaged through a thorough exam that includes: A detailed history A neurological exam Palpation, especially midline along the vertebrae[12] ROM, STR, joint mobility and muscle length assessments Careful differential diagnosis Medical Management (current best evidence)[edit | edit source] Patients with burst fractures (a type of traumatic spinal injury in which a vertebra breaks from a high-energy vertical axial load) of the thoracic and lumbar spines must receive individualized case analysis before a course of therapy can be decided. A consideration of fracture stability, degree of canal compromise, and patient evaluation become significant in determining operative or nonoperative treatment. In neurologically intact patients with selected fractures, nonoperative treatment can be successful in the functional rehabilitation of the patient.[23] Operative[edit | edit source] When neurological impairments are present, surgical procedures are usually required to repair or relieve the site of injury.[24] There are several procedures determined by the degree of compromise, the spinal level of the fracture and the patient's previous health status.[25] A technique called ‘decompression’ is an example of one of these procedures. In this technique, a small portion of bone or disc material that compresses the nerve root is surgically removed to give the root more space.[26] Anterior/Posterior Approach: Often dictated by the severity of compromise or level of injury, a surgeon will make an anterior or posterior approach to the patient's spine in order to stabilize it. Rods, screws and other mechanical devices are inserted through remaining structures to fuse the affected vertebra(e). The anterior approach dominates upper lumbar (L1, L2) fractures due to involvement with the crura of the diaphragm while lower lumbar fractures (L5) are stabilized through a posterior approach method.[27][28] Kyphoplasty: A mini-invasive percutaneous procedure that relieves vertebral fracture pain through the heat discharged during bone cement coagulation. The cement also solidifies to further stabilize the site of injury.[29] During the procedure, a cannula is introduced into the vertebral body followed by a bone expander to regain some vertebral height. Kyphoplasty has been found to be similar in success rate as vertebroplasty, but with greater recovery of vertebral height.[30] A study by Wardlaw et al. suggests that Balloon Kyphoplasty (a minimally invasive procedure for the treatment of painful vertebral fractures) is an effective and safe procedure for patients with acute vertebral fractures.[31] Vertebroplasty: An effective treatment in the management of vertebral compression fractures, vertebroplasty involves injecting bone fillers such as polymethylmethacrylate (PMMA) bone cement into the fractured vertebral body. The effect of this procedure on osteoporotic vertebral compression fractures was analysed by R. Takemasa et al. and found no demonstrable clinically important benefits compared with a sham procedure. Non-operative[edit | edit source] Patients not requiring surgery receive treatments that target pain relief with bracing and rehabilitation therapy.[12][11] Those with compression type and burst type fractures involving the anterior and middle column have been described as the best candidates for non-operative management.[10] Compression Fractures A study by Stadhouder et al states that brace treatment with supplementary physical therapy is the treatment in choice for patients with compression fractures of the thoracic and lumbar spine.[32] Burst Fractures Operative treatment of patients with a stable thoracolumbar burst fracture and normal findings on a neurological examination provides no major long-term advantage compared with nonoperative treatment.[33] A prospective study by Shen et al. comparing operative and non-operative treatment of thoracolumbar burst fractures without neurological deficit acknowledges the early pain relief and partial kyphosis correction provided by operative short-segment posterior fixation, but the functional outcome at two years is similar to that of non-operative treatment.[34] Orthoses[edit | edit source] A thoracic-lumbar-sacral orthosis (TLSO) is the current brace of choice for these types of injuries. However, patients will also want to move into mobility as their pain and healing process progresses. Thus allowing them to move into weight-bearing exercises to prevent future osteoporosis and extension exercises.[12][11] Non-operative options are increasingly becoming the preferred method of fracture management as bracing and therapy methods are shown to be as clinically effective, yet much more cost-efficient than surgical options.[35] Orthoses have shown great improvements in muscle strength, posture and body height. The brace makes sure that muscles along the vertebrae get less fatigued and relief of muscle spasm. In lumbar fractures orthosis is available but can only restrict sagittal plane motion in the upper lumbar spine (L1-3). Motion between the lower segments has been proven to be increased while wearing an orthosis brace (L4-S1).[36] Pharmaceutical[edit | edit source] Medications ranging from Tylenol and NSAIDs to opioids can be taken to modulate lumbar spine fracture pain. Spinal nerve blocks at the L2 region have also been found to be effective against acute low back pain from fractures.[37] Physical Therapy Management[edit | edit source] The purpose of physical therapy management in patients with lumbar spine fracture is to decrease pain, increase mobility and prevent future occurrences.[12][11] While mobility is important, back extensor and abdominal (core) strength have been shown an effective therapeutic intervention for those with lumbar problems associated with osteoporosis. In particular, the multifidus, quadratus lumborum and transverse abdominals help support the spine. So much so that increasing strength not only relieves pain and symptoms from those patients with fractures, but also can act as a preventative to decrease future fractures. Physical therapy programs that promote exercise targeting impairments in intrinsic back strength have been shown to improve the function and quality of life in those with osteoporotic vertebral fracture.[12] [35] [38]Several suggested exercises can be seen below. Focus on transverse abdominal control, properly learn to activate the TA, reverse curl ups, hip bridging Focus on strengthening transverse abdominals. Stabilization is increased through multifidus, transverse abdominal and oblique contraction. This exercise works both the core and back muscles, hitting the TA, multifidus and quadratus lumborum. Thoracolumbar fracture therapy evidence closely parallels that of the lumbar spine and other exercises can be seen here Thoracic_Spine_Fracture. Assuming the availability of necessary nutrients, stimulus to the osteoblasts results in a net gain in bone mass. Exercise is a form of repetitive loading that facilitates osteoblastic activity, thereby helping to maintain a positive balance between bone formation and bone resorption.[39] Even the very moderate amount of exercise that is recommended for general wellness (a minimum of 30 minutes on most days) is helpful in preventing osteoporosis and maintaining bone density. Overall, physical therapy has been shown to have no clinical significant difference in outcomes when compared to surgery for appropriate spinal fracture patients. Not only does physical therapy help relieve pain and disability as well as surgery, but the overall cost to the patient is greatly reduced.[35] Clinical Bottom Line[edit | edit source] Lumbar spine fractures, whether from an acute injury or progressive in nature like osteoporosis, occur often enough to merit adequate research with regard to healing procedures. A great deal of inquiry has gone into spinal surgery options, while very little appears to exist for specific physical therapy management. Most of the present information acknowledges that physical therapy, especially that of therapy and bracing can just as effectively manage lumbar fracture pain (without neurological involvement) as that of surgery. However, no current research exists that effectively compares the most effective therapy. Current recommendations revolve around basic core and lumbar spine strengthening as with most lumbar spine injuries. It is our recommendation that more research be done in this area that focuses specifically on lumbar spine fractures and the most effective therapy treatments for these injuries. Resources[edit | edit source] Medscape. Lumbar Compression Fracture. Available from: <nowiki>http://emedicine.medscape.com/article/309615-overview</nowiki> (accessed 7 May 2022). OrthoInfo. Fractures of the Thoracic and Lumbar Spine. Available from: <nowiki>http://orthoinfo.aaos.org/topic.cfm?topic=a00368</nowiki> (accessed 7 May 2022). Wheeless' Textbook of Orthopaedics. Burst Fracture of Spine. Available from: <nowiki>http://www.wheelessonline.com/ortho/burst_frx_of_spine</nowiki> (accessed 7 May 2022). SpineUniverse. Low Lumbar Fractures at L4 and L5. Available from: <nowiki>http://www.spineuniverse.com/professional/pathology/trauma/fractures-l4-l5-low-lumbar-fractures</nowiki> (accessed 7 May 2022) Livestrong. Physical Therapy for Lumbar Compression Fractures. <nowiki>http://www.livestrong.com/article/420272-physical-therapy-for-lumbar-compression-fractures/</nowiki> (accessed 7 May 2022)
| | * [[Functional Anatomy of the Thoracic Spine and Rib Cage]] |
| | * [[Functional Anatomy of the Lumbar Spine and Abdominal Wall]] |
| | * [[Cervical Deep Neck Extensors]] |
| | * [[Cervical Deep Neck Flexors]] |
|
| |
|
| == References == | | == References == |
| | | <references /> |
| # ↑ Yan YZ, Li QP, Wu CC, Pan XX, Shao ZX, Chen SQ, Wang K, Chen XB, Wang XY. Rate of the presence of 11 thoracic vertebrae and 6 lumbar vertebrae in asymptomatic Chinese adult volunteers. J Orthop Surg Res. 2018 May 23;13(1):124.
| | [[Category:Anatomy]] |
| # ↑ Jump up to:2.0 2.1 2.2 2.3 2.4 2.5 Xuan D. Exploring Lumbar Spine and Abdominal Wall Anatomy Course. Physiopedia Plus, 2023.
| | [[Category:Cervical Spine]] |
| # ↑ Yan YZ, Wang B, Huang XQ, Ru X, Wang XY, Qu HB. Variation in Global Spinal Sagittal Parameters in Asymptomatic Adults with 11 Thoracic Vertebrae, four Lumbar Vertebrae, and six Lumbar Vertebrae. Orthop Surg. 2022 Feb;14(2):341-348.
| | [[Category:Musculoskeletal/Orthopaedics]] |
| # ↑ Waxenbaum JA, Reddy V, Williams C, Futterman B. Anatomy, Back, Lumbar Vertebrae. 2022 Aug 1. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–.
| | [[Category:Neurology]] |
| # ↑ Jump up to:5.0 5.1 Diebo BG, Varghese JJ, Lafage R, Schwab FJ, Lafage V. Sagittal alignment of the spine: What do you need to know? Clin Neurol Neurosurg. 2015 Dec;139:295-301.
| | [[Category:Course Pages]] |
| # ↑ Schwab F, Lafage V, Boyce R, Skalli W, Farcy JP. Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine (Phila Pa 1976). 2006 Dec 1;31(25):E959-67.
| | [[Category:Plus Content]] |
| # ↑ Jump up to:7.0 7.1 Feng Q, Zhang L, Zhang M, Wen Y, Zhang P, Wang Y, Zeng Y, Wang J. Morphological parameters of fourth lumbar spinous process palpation: three-dimensional reconstruction of computed tomography. J Orthop Surg Res. 2020 Jun 22;15(1):227.
| |
| # ↑ Jump up to:8.0 8.1 Kapetanakis S, Gkantsinikoudis N. Anatomy of lumbar facet joint: a comprehensive review. Folia Morphol (Warsz). 2021;80(4):799-805.
| |
| # ↑ Inoue N, Orías AAE, Segami K. Biomechanics of the Lumbar Facet Joint. Spine Surg Relat Res. 2019 Apr 26;4(1):1-7.
| |
| # ↑ Jump up to:10.0 10.1 Yoon WW, Koch J. Herniated discs: when is surgery necessary? EFORT Open Rev. 2021 Jun 28;6(6):526-530.
| |
| # ↑ Cavalli M, Aiolfi A, Bruni PG, Manfredini L, Lombardo F, Bonfanti MT, Bona D, Campanelli G. Prevalence and risk factors for diastasis recti abdominis: a review and proposal of a new anatomical variation. Hernia. 2021 Aug;25(4):883-890.
| |
| # ↑ Clinical Physio. Lumbar Spine Palpation. Available from: <nowiki>https://www.youtube.com/watch?v=XrQP3AeDjiM</nowiki> [last accessed 25/6/2023]
| |
| | |
| Get Top Tips Tuesday and The Latest Physiopedia updates
| |
| | |
| ==== Our Partners ====
| |