Osteogenesis Imperfecta: Difference between revisions
No edit summary |
No edit summary |
||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
[[File:1024px-X ray for osteogenesis imperfecta.jpeg|alt=|Figure 1. X-ray of osteogenesis imperfecta.|thumb]] | [[File:1024px-X ray for osteogenesis imperfecta.jpeg|alt=|Figure 1. X-ray of osteogenesis imperfecta.|thumb]] | ||
Osteogenesis imperfecta (OI) is a "heterogeneous group of [[Congenital and Acquired Neuromuscular and Genetic Disorders|congenital]], non-sex-linked, [[Genetic Disorders|genetic disorders]]".<ref name=":0" /> It affects the production or processing of type 1 collagen, and therefore, impacts [[Connective Tissue Disorders|connective tissue]] and [[bone]].<ref name=":0" /><ref name=":2" /> | Osteogenesis imperfecta (OI) is a "heterogeneous group of [[Congenital and Acquired Neuromuscular and Genetic Disorders|congenital]], non-sex-linked, [[Genetic Disorders|genetic disorders]]".<ref name=":0" /> It affects the production or processing of type 1 collagen, and therefore, impacts [[Connective Tissue Disorders|connective tissue]] and [[bone]].<ref name=":0" /><ref name=":2">Subramanian S. StatPearls Publishing LLC.; Treasure Island, FL, USA: 2021. Osteogenesis Imperfecta.</ref> | ||
It is also referred to as "brittle bone disease". Individuals with OI are susceptible to fractures and reduced bone density.<ref name=":2" /> They may present with [[osteoporosis]] and blue sclera (i.e. the white part of the eye), and their teeth and hearing can be affected.<ref name=":0">Osteogenesisi Imperfecta. Available from: https://radiopaedia.org/articles/osteogenesis-imperfecta-1 (Accessed, 15/10/ 2021).</ref> It can also impact mobility and an individual's ability to perform activities of daily living. | It is also referred to as "brittle bone disease". Individuals with OI are susceptible to fractures and reduced bone density.<ref name=":2" /> They may present with [[osteoporosis]] and blue sclera (i.e. the white part of the eye), and their teeth and hearing can be affected.<ref name=":0">Osteogenesisi Imperfecta. Available from: https://radiopaedia.org/articles/osteogenesis-imperfecta-1 (Accessed, 15/10/ 2021).</ref> It can also impact mobility and an individual's ability to perform activities of daily living. | ||
OI can | OI can have a negative effect on the social and emotional well-being of young people with this condition and their families. Adopting a coordinated, [[Multidisciplinary Team|multidisciplinary team]] approach helps to ensure that children with OI can "fulfill their potential, maximizing function, independence, and well-being."<ref>Marr C, Seasman A, Bishop N. Managing the patient with osteogenesis imperfecta: a multidisciplinary approach. Journal of multidisciplinary healthcare. 2017; 10:145.</ref> | ||
== Epidemiology == | |||
OI is a rare condition. The estimated incidence is approximately 1 in every 15,000 to 20,000 births.<ref name=":2" /> It affects males and females equally, and there are no differences in terms of race / ethnic group.<ref name=":0" /> | |||
== Aetiology == | |||
OI usually occurs secondary to mutations in the ''COL1A1'' and ''COL1A2'' genes, but there have been diverse mutations related to OI identified more recently.<ref name=":2" /> | |||
== Pathology == | |||
In OI, the synthesis of type I collagen is affected. Type I collagen forms the main protein of the extracellular matrix of many of our tissues, including our skin, bones, tendons, skin and sclerae.<ref name=":0" /><ref name=":2" /> | |||
== Types of OI == | == Types of OI == | ||
There are at least eight different types of OI, but three types are said to be easily distinguished.<ref name=":0" /> | There are at least eight different types of OI, but three types are said to be easily distinguished.<ref name=":0" /> | ||
| Line 16: | Line 24: | ||
* Type I:<ref name=":1" /> | * Type I:<ref name=":1" /> | ||
** The most common and mildest type of OI | ** The most common and mildest type of OI | ||
** Around 50% of children with OI have Type 1 OI | ** Around 50% of children with OI have Type 1 OI | ||
** Individuals have few fractures / deformities | ** Individuals have few fractures / deformities | ||
* Type II:<ref name=":1" /><ref name=":2" /> | * Type II:<ref name=":1" /><ref name=":2" /> | ||
** The most severe type of OI - it is a lethal condition, usually within weeks of birth | ** The most severe type of OI - it is a lethal condition, usually within weeks of birth | ||
** Causes severe disruption of "qualitative function" of the collagen molecule<ref name=":2" /> | ** Causes severe disruption of the "qualitative function" of the collagen molecule<ref name=":2" /> | ||
** Infants with Type II OI present with very short arms and legs, small chest and they have delayed ossification of the skull | ** Infants with Type II OI present with very short arms and legs, small chest and they have delayed ossification of the skull | ||
** There may be fractures at birth, low birth weight | ** There may be fractures at birth, low birth weight and under-developed lungs | ||
* Type III:<ref name=":1" /> | * Type III:<ref name=":1" /> | ||
** Children who have severe clinical signs tend to have Type III OI | ** Children who have severe clinical signs tend to have Type III OI | ||
** | ** They tend to present with moderate to severe fragility of bones, coxa vera, they may have slightly shorter arms and legs, and have arm, leg, and rib fractures | ||
** Infants may have a larger head, a triangular-shaped face, changes in their chest and spine (scoliosis), difficulties with breathing and swallowing | ** Infants may have a larger head, a triangular-shaped face, changes in their chest and spine (scoliosis), and difficulties with breathing and swallowing | ||
** May also have frontal bossing (i.e. prominent forehead), basilar invagination, short stature | ** May also have frontal bossing (i.e. prominent forehead), basilar invagination, short stature | ||
** Symptoms vary in each infant<ref name=":1">Osteogenesis Imperfecta. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/osteogenesis-imperfecta (Accessed, 15/10/2021). | ** Symptoms vary in each infant<ref name=":1">Osteogenesis Imperfecta. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/osteogenesis-imperfecta (Accessed, 15/10/2021). | ||
| Line 35: | Line 42: | ||
== Epidemiology == | == Epidemiology == | ||
OI is a rare condition. The estimated incidence is approximately 1 in every 15,000 to 20,000 births.<ref name=":2" /> It affects males and females equally, and there are no | OI is a rare condition. The estimated incidence is approximately 1 in every 15,000 to 20,000 births.<ref name=":2" /> It affects males and females equally, and there are no differences in terms of race / ethnic group. | ||
== Clinical presentation == | == Clinical presentation == | ||
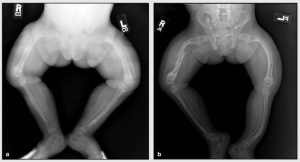
[[Image:X-ray OI.jpg|This picture is included courtesy of gghjournal.com.|alt=| | [[Image:X-ray OI.jpg|Image of OI X-ray. This picture is included courtesy of gghjournal.com.|alt=|thumb]]In general, four major clinical features characterise osteogenesis imperfecta.<ref name=":0" /><ref name=":1" /> | ||
In general, four major clinical features characterise osteogenesis imperfecta: | |||
# Osteoporosis | # Osteoporosis / bone fragility | ||
#* | #* fractures | ||
#* | #* bone deformities | ||
# Discoloration of the sclera (white of the eye) | # Discoloration of the sclera (white of the eye) | ||
#* may be blue or gray in | #* may be blue or gray in colour | ||
# Dentinogenesis imperfecta | # Dentinogenesis imperfecta | ||
#* | #* discolouration of teeth (e.g. blue-gray / yellow-brown colour) | ||
#* teeth | #* translucent teeth | ||
#* can affect | #* weaker teeth | ||
# Hearing impairment | #* can affect baby and adult teeth<ref>Dentiogenesis Imperfecta. Available from: https://medlineplus.gov/genetics/condition/dentinogenesis-imperfecta/ (Accessed, 15/10/2021).</ref> | ||
# Hearing impairment | |||
Can also cause laxity of ligamentous, joint [[Hypermobility Syndrome|hypermobility]], short stature and individuals are prone to bruising.<ref name=":0" /> | |||
== Diagnosis == | == Diagnosis == | ||
The | The following diagnostic tests may be recommended: | ||
# [[X-Rays|X-rays]] | # [[X-Rays|X-rays]]: able to show weakened / deformed bones, fractures | ||
# [[Laboratory Tests|Lab tests]] | # [[Laboratory Tests|Lab tests]]: including blood, saliva, skin and gene testing | ||
# Dual Energy X-ray Absorptiometry scan (DXA or DEXA scan) | # Dual Energy X-ray Absorptiometry scan (DXA or DEXA scan): to investigate softening of bone | ||
# Bone biopsy | # Bone biopsy (taken at the hip)<ref name=":1" /> | ||
== Treatment == | == Treatment == | ||
Treatment focuses on the prevention of deformities and fractures and the maintenance of independence.<ref name=":1" /> | |||
Management options include: | Management options include:<ref name=":0" /> | ||
* | * Surgery to help prevent fractures and to correct deformities | ||
** Intramedullary rods with osteotomy | ** Intramedullary rods with osteotomy for severe bowing of the long bones | ||
** Intramedullary rods | ** Intramedullary rods for children with frequent fractures of long bones | ||
** Different types of rods (surgical nails) are available to address issues related to surgery, bone size, and the prospect for growth; the two major categories of rods are telescopic and non-telescopic. | ** Different types of rods (surgical nails) are available to address issues related to surgery, bone size, and the prospect for growth; the two major categories of rods are telescopic and non-telescopic. | ||
| Line 91: | Line 86: | ||
== Prognosis == | == Prognosis == | ||
Prognosis is variable depending on the type of OI.<ref name=":2" /> | |||
# Age of onset of long bone fractures | # Age of onset of long bone fractures is a prognostic indicator for ambulatory ability. | ||
# Survival: The most significant indicators include the location of fractures, the severity of fractures and general radiographic appearance of the skeleton. | # Survival: The most significant indicators include the location of fractures, the severity of fractures and general radiographic appearance of the skeleton. | ||
# Engelbert et al. demonstrated that: children who achieved independent sitting or standing or both by 12 years of age, were finally able to ambulate; children who could achieve independent sitting or standing, or both, by the age of 12 months were likely to be able to walk<ref name=":2" /> | # Engelbert et al. demonstrated that: children who achieved independent sitting or standing or both by 12 years of age, were finally able to ambulate; children who could achieve independent sitting or standing, or both, by the age of 12 months were likely to be able to walk<ref name=":2" /> | ||
Revision as of 22:59, 22 April 2023
Genetic_DisordersOriginal Editors - Barrett Mattingly from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Barrett Mattingly, Lucinda hampton, Jess Bell, Admin, Uchechukwu Chukwuemeka, Kim Jackson, Robin Tacchetti, Dave Pariser, Kirenga Bamurange Liliane, WikiSysop, Heidi Johnson Eigsti, Elaine Lonnemann, Wendy Walker, Meaghan Rieke, Anna Fuhrmann and 127.0.0.1
Introduction[edit | edit source]
Osteogenesis imperfecta (OI) is a "heterogeneous group of congenital, non-sex-linked, genetic disorders".[1] It affects the production or processing of type 1 collagen, and therefore, impacts connective tissue and bone.[1][2]
It is also referred to as "brittle bone disease". Individuals with OI are susceptible to fractures and reduced bone density.[2] They may present with osteoporosis and blue sclera (i.e. the white part of the eye), and their teeth and hearing can be affected.[1] It can also impact mobility and an individual's ability to perform activities of daily living.
OI can have a negative effect on the social and emotional well-being of young people with this condition and their families. Adopting a coordinated, multidisciplinary team approach helps to ensure that children with OI can "fulfill their potential, maximizing function, independence, and well-being."[3]
Epidemiology[edit | edit source]
OI is a rare condition. The estimated incidence is approximately 1 in every 15,000 to 20,000 births.[2] It affects males and females equally, and there are no differences in terms of race / ethnic group.[1]
Aetiology[edit | edit source]
OI usually occurs secondary to mutations in the COL1A1 and COL1A2 genes, but there have been diverse mutations related to OI identified more recently.[2]
Pathology[edit | edit source]
In OI, the synthesis of type I collagen is affected. Type I collagen forms the main protein of the extracellular matrix of many of our tissues, including our skin, bones, tendons, skin and sclerae.[1][2]
Types of OI[edit | edit source]
There are at least eight different types of OI, but three types are said to be easily distinguished.[1]
- Type I:[4]
- The most common and mildest type of OI
- Around 50% of children with OI have Type 1 OI
- Individuals have few fractures / deformities
- Type II:[4][2]
- The most severe type of OI - it is a lethal condition, usually within weeks of birth
- Causes severe disruption of the "qualitative function" of the collagen molecule[2]
- Infants with Type II OI present with very short arms and legs, small chest and they have delayed ossification of the skull
- There may be fractures at birth, low birth weight and under-developed lungs
- Type III:[4]
- Children who have severe clinical signs tend to have Type III OI
- They tend to present with moderate to severe fragility of bones, coxa vera, they may have slightly shorter arms and legs, and have arm, leg, and rib fractures
- Infants may have a larger head, a triangular-shaped face, changes in their chest and spine (scoliosis), and difficulties with breathing and swallowing
- May also have frontal bossing (i.e. prominent forehead), basilar invagination, short stature
- Symptoms vary in each infant[4]
- Types IV to VIII are not common and vary in terms of their severity.[1]
Epidemiology[edit | edit source]
OI is a rare condition. The estimated incidence is approximately 1 in every 15,000 to 20,000 births.[2] It affects males and females equally, and there are no differences in terms of race / ethnic group.
Clinical presentation[edit | edit source]
In general, four major clinical features characterise osteogenesis imperfecta.[1][4]
- Osteoporosis / bone fragility
- fractures
- bone deformities
- Discoloration of the sclera (white of the eye)
- may be blue or gray in colour
- Dentinogenesis imperfecta
- discolouration of teeth (e.g. blue-gray / yellow-brown colour)
- translucent teeth
- weaker teeth
- can affect baby and adult teeth[5]
- Hearing impairment
Can also cause laxity of ligamentous, joint hypermobility, short stature and individuals are prone to bruising.[1]
Diagnosis[edit | edit source]
The following diagnostic tests may be recommended:
- X-rays: able to show weakened / deformed bones, fractures
- Lab tests: including blood, saliva, skin and gene testing
- Dual Energy X-ray Absorptiometry scan (DXA or DEXA scan): to investigate softening of bone
- Bone biopsy (taken at the hip)[4]
Treatment[edit | edit source]
Treatment focuses on the prevention of deformities and fractures and the maintenance of independence.[4]
Management options include:[1]
- Surgery to help prevent fractures and to correct deformities
- Intramedullary rods with osteotomy for severe bowing of the long bones
- Intramedullary rods for children with frequent fractures of long bones
- Different types of rods (surgical nails) are available to address issues related to surgery, bone size, and the prospect for growth; the two major categories of rods are telescopic and non-telescopic.
- Care of fractures. The lightest possible materials are used to cast fractured bones. To prevent further problems, it is recommended that a child begin moving or using the affected area as soon as possible.
- Bisphosphonates
- Growth hormone therapy[1]
- Dental procedures: Treatments including capping teeth, braces, and surgery may be needed.
- Physical and occupational therapy are both very important in babies and children with OI.
- Assistive devices. Wheelchairs and other custom-made equipment may be needed as babies get older[4].
Prognosis[edit | edit source]
Prognosis is variable depending on the type of OI.[2]
- Age of onset of long bone fractures is a prognostic indicator for ambulatory ability.
- Survival: The most significant indicators include the location of fractures, the severity of fractures and general radiographic appearance of the skeleton.
- Engelbert et al. demonstrated that: children who achieved independent sitting or standing or both by 12 years of age, were finally able to ambulate; children who could achieve independent sitting or standing, or both, by the age of 12 months were likely to be able to walk[2]
Complications[edit | edit source]
Complications may affect most body systems in a baby or child with OI. The risk of developing complications depends on the type and severity of your baby's OI. Complications may include the following:
- Respiratory infections eg. COVID 19, pneumonia
- Heart problems eg. poor cardiac valve defects
- Kidney stones
- Joint problems
- Hearing loss
- Eye conditions and vision loss
Team Approach[edit | edit source]
Physical and occupational therapy are part of an interdisciplinary approach to treatment. The medical team may also include a primary care physician, orthopedist, geneticist, nutritionist, social worker, and psychologist. Children and adults with OI, especially those with spine curves which may affect pulmonary status, may regularly see a pulmonologist. Ideally planning ahead for rehabilitation is included in the preparation for surgery. [6]
Physiotherapy[edit | edit source]
When working with individuals and families living with OI, therapists should keep these principles in mind:
- Listen: It is essential to listen to individuals with OI and their families and respect their input.
- Set Goals: Make goals incremental, realistic and achievable.
- Fear of Fractures is another serious constraint to movement: Establishing safe movement procedures, encouraging self-confidence and optimizing strength are strategies that can help resolve this issue. Passive range of motion is not recommended with new clients.
- Expect Success. With the proper environment and equipment, the majority of children and adults with OI can function well in many or most areas of daily life including but not limited to self-care, school and work.
Maximizing a person’s strength and function not only improves overall health and wellbeing, but also improves bone health, as mechanical stresses and muscle tension on bone help increase bone density. eg, deformities such as a flattened skull, a lordotic back, or tight hip flexor muscles can be prevented or minimized through therapy.
Approaches include:
- Exercise including weight bearing activities (braces may be needed), and recreational activities low-impact activities such as swimming, once precautions are defined.
- Encouraging different body positions and postures during the day and safe handling to strengthen muscle groups and prevent deformities.
- Adaptive equipment. Depending on the environment, a variety of mobility aides may be needed (cane, walker, manual or power wheelchair).
- Environmental adaptations in the home, school or workplace.[6]
Circumstances requiring intermittent or long-term physical therapy:
- When a child with OI has delays or weakness in motor skills
- When a child or adult with OI is recovering from a fracture, surgery or injury
- When a person with OI experiences fear of movement and trying new skills and activities.
- When a person with OI reaches a transition point in life, they must adapt to a new environment or require ADL training.[6]
Key Principles of Therapeutic Strategies
Patience and task analysis are both necessary to develop a successful therapy program. Developmental concepts and specific skills need to be analyzed closely, so that many small improvements can lead to achieving a particular therapy goal.
Key therapeutic strategies include the following:
1. Skill Progression - gross motor skills may be delayed or difficult for those with moderate to severe OI; In order to learn person care skills, basic gross motor skills need to be developed (reaching, sitting, etc.)
2. Preventive positioning, protective handling and active movement with gradual progression facilitate safe development of motor skills
3. Water therapy - allows for reduced gravity environment and a great starting place in the face of fear of movement; Adults often use water therapy to maintain or relearn motor skills.
4. Equipment - various equipment from wheelchairs to pillows can contribute to achieving personal and motor goals
5. Encouraging healthy living and participation in recreational activities to promote general health and prevent obesity [6]
Children of Glass[edit | edit source]
Excerpts from the Discovery Health documentary on the genetic brittle bone disorder "Osteogenesis Imperfecta", courtesy of Youtube.com.
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Osteogenesisi Imperfecta. Available from: https://radiopaedia.org/articles/osteogenesis-imperfecta-1 (Accessed, 15/10/ 2021).
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Subramanian S. StatPearls Publishing LLC.; Treasure Island, FL, USA: 2021. Osteogenesis Imperfecta.
- ↑ Marr C, Seasman A, Bishop N. Managing the patient with osteogenesis imperfecta: a multidisciplinary approach. Journal of multidisciplinary healthcare. 2017; 10:145.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 Osteogenesis Imperfecta. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/osteogenesis-imperfecta (Accessed, 15/10/2021).
- ↑ Dentiogenesis Imperfecta. Available from: https://medlineplus.gov/genetics/condition/dentinogenesis-imperfecta/ (Accessed, 15/10/2021).
- ↑ 6.0 6.1 6.2 6.3 OI foundation Physical and Occupational Therapists Guide to Treating Osteogenesis Imperfecta Available:https://oif.org/wp-content/uploads/2019/08/PT_guide_final.pdf (accessed 15.10.2021)
- ↑ Bublitz Videos. Children of Glass - (Part 1 of 4). Available from: http://www.youtube.com/watch?v=TpAMTOud3bw [last accessed 27/8/2020]
- ↑ Bublitz Videos. Children of Glass - (Part 2 of 4). Available from: http://www.youtube.com/watch?v=GTpSxlPzC8k [last accessed 37/8/2020]
- ↑ Bublitz Videos. Children of Glass - (Part 3 of 4). Available from: http://www.youtube.com/watch?v=L2f8fz6vzoI [last accessed 27/8/2020]
- ↑ Bublitz Videos. Children of Glass - (Part 4 of 4). Available from: http://www.youtube.com/watch?v=QvbY7XqyMz8 [last accessed 27/8/2020]