Snapping Scapula Syndrome
Definition/Description[edit | edit source]
Snapping scapula syndrome is defined as an audible or palpable clicking, grinding, or crepitus noise of the scapula during movements involving the scapulothoracic joint. It is more of a symptom of other diagnoses. It is commonly seen in younger active individuals.[1] These individuals often have a history of pain, discomfort, and weakness with overhead movements which can result from sporting activities or overuse. The symptoms of snapping scapula syndrome can be insidious, be due to a result of trauma or from excessive grinding of the scapula and the thorax with soft tissues entrapped between them, such as bursas, muscles, or tendons.[2] Pain is typically not reproducible with isometric movements. The clicking and popping, as well as pain usually decreases when crossing the arm across the chest, this causes the scapula to lift from the rib cage. This syndrome is oftentimes overlooked due to a lack of awareness about the diagnosis.
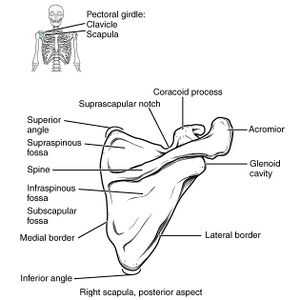
To better appreciate this condition, a preview of scapula Anatomy[3] maybe necessary. See physiopedia page on the Scapula.
Aetiology[edit | edit source]
Snapping scapula syndrome can have a variety of different causes. Typically, it is a result of overuse of the arm, such as repetitive overhead activities, however, it can also be due to trauma to the shoulder blade region. Aside from these variations, snapping scapula can be caused by anatomical variations and certain diseases. Some anatomical variations can include excessive forward curvature of the superomedial border of the scapula, whereas some diseases can include osteochondromas or scapular dyskinesis, also known as the SICK scapula.
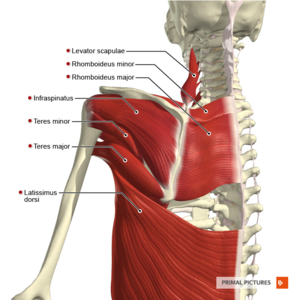
Scapular dyskinesis is defined as abnormal movements of the shoulder blade and there are a variety of causes for this, however, most are attributed to errors and are mostly dysfunctional rhythm and timing of the associated shoulder musculature. There is primary, secondary, and dynamic scapular winging. Primary scapular winging is mainly due to muscle weakness of one of the scapula stabilizers. Secondary scapular winging is when the normal movement of the scapula is altered due to glenohumeral joint pathology. Dynamic scapular winging can be due to a lesion of the long thoracic nerve which affects the serratus anterior, causes trapezius palsy, rhomboid weakness, multidirectional instability, voluntary action, and pain in the shoulder which can cause reverse scapulohumeral rhythm.
Changes in alignment to the structures, such as a fractured scapula or rib that doesn't heal or line up correctly can cause the sounds and sensations of this syndrome. Abnormal bumps and curves on the scapula’s medial border can cause bursas to form, thus leading to inflammation causing bursitis to occur. Scapulothoracic bursitis is a common cause, which is inflammation of the bursa under the shoulder blade.[4] It can occur from trauma to area, from a cause of repetitive movements of the joint, or be due to scapular dyskinesis. Another cause is from inactivity of the musculature under the scapula, causing the scapula and rib cage to grind against one another during movements.[3]
Clinical Presentation/Characteristics[edit | edit source]
Snapping Scapula Syndrome manifests in several distinct ways that can affect an individual's day-to-day activities and overall shoulder function. These manifestations, often a result of the scapula's abnormal interaction with the rib cage, can range from auditory symptoms to pain and altered movement patterns.[1] [5] Here are some of the key characteristics and presentations of this condition:
- Popping, Clicking, and Grinding: These are auditory or tactile feedback symptoms that patients often report during overhead arm movements. It's the outcome of the scapula rubbing against the ribs or thoracic spine.
- Pain with Overhead Movements: The discomfort can be triggered by activities that require lifting the arm, like reaching for an object on a high shelf or performing athletic actions.
- Nature of Pain: The pain may vary in its presentation. It can be dull and persistent, a constant achy feeling, or even sharp, sudden jabs depending on the individual and the underlying causes.
- Lack of Coordinated Movements: This pertains to an inability to smoothly and efficiently move the shoulder in its full range, often leading to restricted motion or compensatory movements.
- Weakness: Affected individuals might experience a loss of strength in the shoulder or upper arm, impacting their ability to carry out daily activities or specific tasks.
- Winging of the Scapula: One of the hallmark signs of this syndrome, it refers to the scapula protruding outwards, away from the thoracic wall. This can sometimes be visibly observed.
- Abnormal Scapular Movements: Beyond just winging, the scapula might not follow its usual movement pattern, leading to a range of other shoulder issues.
Examination[edit | edit source]
Some common questions a physical therapist may ask a patient during the evaluation process if they suspect they may have snapping scapula syndrome:
- How and when did you first notice the pain?
- With what activities do you hear or feel popping, clicking and grinding symptoms?
- Do you have any pain or stiffness in your neck?
- Does your shoulder feel weak or “tired?”[5]
Evaluation Process[edit | edit source]
The accurate diagnosis and assessment of Snapping Scapula Syndrome require a comprehensive evaluation process. This not only determines the presence of the condition but also identifies its severity, underlying causes, and associated musculoskeletal issues. From understanding the patient's pain experiences and daily life impact to meticulous physical examination and diagnostic imaging, a multifaceted approach ensures targeted and effective treatment. [6] The following components form an integral part of the evaluation procedure for this condition:
- Pain & Functional Questionnaires/ Health Assessment:
- Pain with overhead activities? Repetitious occupation? MOI? Trauma? Overuse?
- Initial Observations of the Patient:
- Bilateral asymmetry of the scapulas? Scapular winging? Poor posture? Popping, clicking, crepitus with movements?
- Structural Inspection:
- C-spine or thoracic deformities? Bony abnormalities?
- Palpation for Condition:
- Obvious bony deviations? Soft tissue atrophy? Palpable crepitus?
- Range of Motion:
- Active range of motion (AROM) quality and quantity, coordination, symptoms reproduced? Compensations? End feel?
- Passive range of motion (PROM) quality and quantity, coordination, symptoms reproduced? Compensations? End feel?
- Joint Accessory motion, joint integrity? Quantity? End feel? Dysfunction?
- Resisted Isometric Contraction:
- Painful and weak? Painful and strong? Painless and weak? Painless and strong?
- Muscle Length Testing:
- Muscle Strength:
- Weakness in upper, middle, and lower Trapezius, Rhomboids, Serratus Anterior, Latissimus Dorsi, Levator Scapulae, Rotator cuff muscles or Deltoids?
- Special Tests:
- Special testing to help rule in or out if the patient has snapping scapula or other shoulder pathologies.
- Movement/Functional Analysis:
- Assessment of scapulohumeral rhythm and functional overhead activities
- Palpation for Tenderness:
- Tenderness at the superior angle or medial border of the scapula?
- Neurovascular:
- Long thoracic nerve involvement?
- Diagnostic Imaging:
Special Tests[edit | edit source]
There are no special tests for snapping scapula syndrome specifically, but there are special tests to rule out other scapula pathologies.
- The patient will perform forward shoulder flexion
- For the involved shoulder, the physical therapist will assist the patient during forward shoulder flexion by promoting normal scapular mechanics by stabilizing the upper scapular border and assisting with upward rotation of the inferomedial border
- The physical therapist will compare the unassisted movement to the assisted movement
- If the patient feels better with assistance, this is a positive (+) test
- The patient is asked to abduct the involved arm to 0, 45 (with internal rotation), then 90 (with maximal internal rotation) degrees
- The physical therapist measures the distance from the inferior angle of the scapula to the thoracic spinous process at the same level
- The physical therapist repeats steps one and two on the uninvolved side to compare
- A positive (+) test is indicated when a side-to-side difference of 1-1.5 cm is detected
Outcome Measures:
- DASH or QuickDASH: Disabilities of the Arm, Shoulder, and Hand
- DASH is a self-reported questionnaire that consists of 30 questions asking about the difficulty level and obstruction in everyday life. QuickDash is a condensed version of DASH and consists of 11 questions.
- PSFS: Patient Specific Functional Scale
- PSFS is self-reported and allows the individual to choose 3-5 activities that are difficult. The activities chosen are then rated on their ability to be performed. The rating is done on a 0 -10 scale with 0 being unable to perform and 10 being able to perform at pre-injury level.
- UEFS: Upper Extremity Functional Scale
- UESF scale is made for individuals with a dysfunction of the shoulder, elbow, wrist, or hand. It is self-reported and asks about 20 daily activities that are rated on a 5-point scale. The 5-point scale ranges from 0-4 with 0 being extremely difficult and 4 being not difficult.
- SPADI: Shoulder Pain and Disability Index
- SPADI consists of 13 questions that are self-reported regarding the pain and disability level of daily activities. There are 5 pain questions and 8 disability questions. SPADI is scored on a 0 to 10 numerical scale.
Conservative Management[edit | edit source]
Typically when scapulothoracic popping and clicking is related to a soft tissue abnormality, poor posture or scapular dyskinesis surgical intervention will not be needed.
- Non-steroidal anti-inflammatory medications (NSAIDs)
- Cortisone injection into the space underneath the scapula where the inflammation occurs; typically repeated 3-4 times a year[8]
- Physical therapy
Preventative Measures[edit | edit source]
Prevention is a cornerstone in managing and reducing the recurrence of Snapping Scapula Syndrome. Implementing specific measures can alleviate the undue strain on the scapulothoracic joint, minimising the risk factors that contribute to the condition's onset or exacerbation. [5] Below are some important preventative measures to consider:
- Maintain an upright posture, avoiding slumping
- Maintain scapular strength and muscles surrounding the shoulder joint
- Use appropriate techniques when performing overhead arm movements
- Maintain flexibility of the musculature of the neck, shoulder and scapula
If conservative management fails to alleviate symptoms after 3 to 6 months, surgical interventions need to be considered.
Physical Therapy Management[edit | edit source]
Physical therapy plays an important role in the management of Snapping Scapula Syndrome. With a combination of modalities, therapeutic exercises, manual techniques, and education on posture and movement mechanics, physical therapists can address the underlying dysfunctions that contribute to the condition. Through individualised treatment plans, patients can experience reduced pain, improved scapular kinematics, and restored shoulder function[5]. Here are some of the primary interventions and techniques employed in the physical therapy management of this syndrome:
- Ice/Heat packs
- Ultrasound
- Diathermy
- Electrical Stimulation
- Laser Treatment
- Soft Tissue Massage of the Scapula
- Trigger Point Releases of the Chest, Neck and Shoulder
- Strengthening exercises of the Serratus Anterior, Mid and Lower Trapezius, Rhomboids and Rotator cuff muscles
- Stretching of the Pectoralis Major and Minor, Levator Scapulae, Upper Trapezius, Latissimus Dorsi, Subscapularis, Sternocleidomastoid, Rectus Capitis, and Scalene muscles
- Address postural issues to make sure the patient's head, neck, and shoulders are lined up according to the kinetic chain model
- Kinesio-taping of the Scapula
- Passive motions of the arm, neck, shoulder and scapula
Common Exercises for SSS:[edit | edit source]
- Cat-Cow
- Shoulder Rolls (forward & backward)
- Prone “Y” exercise for the Lower Trapezius
- Scapular Retractions
- External and Internal Rotation with therabands/weights
- Serratus Anterior Punches
- Gradual incorporation of functional movements and/or activities that relate directly to the patient and their goals
- Scapular mobilization exercises are shown in the video below:
Surgical Intervention[edit | edit source]
- Arthroscopic Scapulothoracic bursectomy: removal of the inflamed tissue from the scapulothoracic space
- Scapular dissection: a bony portion of the scapula that is prominent may be removed due to friction against the ribs
- A scapulothoracic bursectomy is when part of the medial angle underneath of the scapula is shaved off and the inflamed bursa between the ribs and scapula is removed. This surgery is an outpatient procedure, so the patient can return home the same day. Recovery time is usually four to six months. During the first four weeks, the patient will be required to wear a sling to limit movement and physical therapy will be started within the fifth-week post-operation.[8]
Rehabilitation Post Scapulothoracic Bursectomy per Dr. Anthony Romeo, Orthopaedic Surgeon[edit | edit source]
After undergoing a scapulothoracic bursectomy, a structured and phased rehabilitation process is crucial to ensure optimal recovery and restoration of shoulder function. Dr. Anthony Romeo, a renowned Orthopaedic Surgeon, has outlined a specific timeline and set of guidelines for postoperative care.[8] This rehabilitation protocol is designed to progressively enhance range of motion, strength, and daily activity functionality while safeguarding the surgical site. Here is a summary of the recommended post-surgery rehabilitation stages:
- Weeks 1-4:
- Wear a sling for 4 weeks
- Can do pendulums
- Advocate for shoulder ROM
- Weeks 4-6
- AAROM with isometrics for the shoulder
- ADLs without the sling
- Wear a sling in public for 6 weeks
- Weeks 6-3 months
- Continue AROM
- Theraband exercises for scapular rotators
- Expect to return to work
References[edit | edit source]
- ↑ 1.0 1.1 Merolla G, Cerciello S, Paladini P, Porcellini G. Snapping scapula syndrome: current concepts review in conservative and surgical treatment. Muscles, ligaments and tendons journal. 2013; 3(2): 80–90.
- ↑ Baldawi H, Gouveia K, Gohal C, Almana L, Paul R, Alolabi B, et al. Diagnosis and Treatment of Snapping Scapula Syndrome: A Scoping Review. Sports health. 2022;4:389–396.
- ↑ 3.0 3.1 de Carvalho SC, Castro ADAE, Rodrigues JC, Cerqueira WS, Santos DDCB, Rosemberg LA. Snapping scapula syndrome: pictorial essay. Radiol Bras. 2019;52(4):262-267. doi: 10.1590/0100-3984.2017.0226.
- ↑ Kiritsis P. A patient’s guide to snapping scapula syndrome. Available from: https://www.kneeandshouldersurgery.com/shoulder-disorders/snapping-scapula-syndrome/#:~:text=Scapulothoracic%20bursitis%20refers%20to%20inflammation,sensations%20 of%20 snapping%20 scapula%20syndrome. (accessed 22 March 2023).
- ↑ 5.0 5.1 5.2 5.3 Avruskin A. Physical therapy guide to snapping scapula syndrome. Available from: https://www.choosept.com/guide/physical-therapy-guide-snapping-scapula-syndrome (accessed 14 March 2023).
- ↑ Manske, R.C., Reiman, M.P. Nonoperative and operative management of snapping scapula. The American Journal of Sports Medicine. 2004;32:1554-1565.
- ↑ Lazar MA. Diagnosis and treatment of snapping scapula syndrome. Evidence Sport and Spine. 2009;91:2251-2262.
- ↑ 8.0 8.1 8.2 Romeo, A. Snapping scapula. Available from: https://www.anthonyromeomd.com/services/snapping-scapula/ (accessed 14 August 2023).
- ↑ Keri Henderson. Scapular Lift Mobilization. Available from: https://www.youtube.com/watch?v=cyup03gGYdE [last accessed 30/3/2023].
- ↑ Keri Henderson. Serratus Anterior Punch Exercise. Available from: https://www.youtube.com/watch?v=6WQ8cK6CTyE [last accessed 30/3/2023].