Pulmonary Hypertension
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Kim Jackson and Uchechukwu Chukwuemeka
Introduction[edit | edit source]
Pulmonary hypertension (PH) is a life-limiting disease affecting circulation to the lungs.[1]
Pulmonary hypertension (PH): an increase of blood pressure in the pulmonary circulation, characterized by remodeling of the pulmonary vasculature, with mean pulmonary arterial pressure (mPAP) > 25 mmHg.
In PH the arteries carrying blood from the right side of the heart to the lungs are constricted, When the arteries between the heart and lungs become narrowed and flow is constricted, the heart has to work extra hard to pump blood to the lungs. Over time, the heart can grow weak and proper circulation can diminish throughout the body[2]. This leads to eg, shortness of breath, exercise intolerance.
In addition to cases of idiopathic pulmonary arterial hypertension, there are numerous known causes, and these can be subdivided in many ways.[3]
It is a rare condition with an estimated prevalence in the range of 10–52 cases per million.
- PH was once viewed as an untreatable condition; however, more people than ever are living with the disease and they are living for longer.
- The primary symptom of PH is breathlessness, yet research has shown that patients with PH can exercise safely and can benefit from exercise to improve exercise capacity and maintain quality of life.
- Medical management includes PH-targeted drug therapy and optimization of underlying conditions; in some patients, surgery is an option[1]
- Physiotherapy for patients should promote physical activity, functional independence, and self-management as routine management of their PH.
Classification[edit | edit source]
It can arise from a variety of causes and is classified (Nice classification) into Five groups:
- Group 1: pulmonary arterial hypertension (PAH). This group includes idiopathic pulmonary arterial hypertension; heritable pulmonary hypertension; drug- and toxin-induced pulmonary hypertension; pulmonary hypertension associated with connective tissue disease, HIV infection (HIV-associated pulmonary arterial hypertension), portal hypertension, congenital heart disease, schistosomiasis.
- Group 2: PH due to left heart disease
- Group 3: PH due to lung diseases (eg COPD) or hypoxia or both
- Group 4: chronic thromboembolic PH (CTEPH)
- Group 5: PH with unclear multifactorial mechanisms[4].
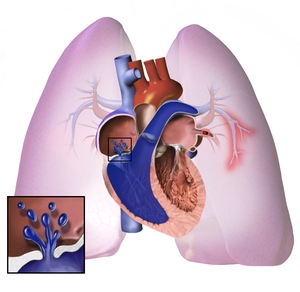
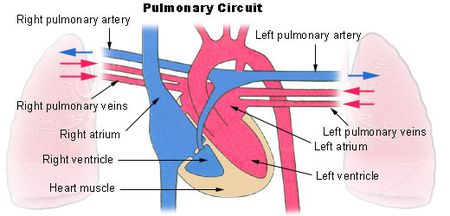
Anatomy - Pulmonary Circuit[edit | edit source]
The pulmonary circuit begins in the right atrium, where practically all the venous blood in the body reaches, passes to the right ventricle and from there it is driven to the alveolar territory through the pulmonary artery that ends in an extensive capillary network that surrounds the alveoli. The blood is separated from the alveolar air by a membrane half to one micron thick. Once arterialized, the blood is carried by the pulmonary veins to the left atrium, where it joins the greater circuit.
Epidemiology[edit | edit source]
Epidemiology varies with the underlying cause and risk factors. Overall, there is a female predilection.
Risk factors include:
- Drugs and toxins
- HIV infection - HIV-associated pulmonary arterial hypertension
- Portal hypertension and liver disease: portopulmonary hypertension
- Connective tissue disease
- Scleroderma[3]
Pathology[edit | edit source]
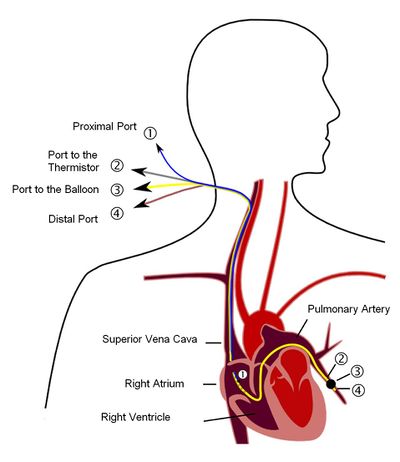
Pulmonary arterial hypertension is defined as a mean pulmonary arterial pressure >25 mmHg at rest 11 or >30 mmHg with exercise and pulmonary capillary wedge pressure ≤15 mmHg measured by cardiac catheterisation.
Image: A simple figure describing pulmonary artery catheter. Construction of a pulmonary artery catheter (Swan-Ganz catheter). The catheter has four lumens. These are the proximal canal (1), which comes to lie in the right atrium and u. a. serves to measure the central venous pressure, the channel that leads to the temperature probe and enables a cold dilution measurement (2), the channel for inflating the balloon (3) and the distal channel with which the pressure in the pulmonary artery (PAP) and the pulmonary artery occlusion pressure ( PCWP, wedge pressure) is measured (4). In this schematic diagram, the catheter is in the wedge position in which the balloon closes the pulmonary artery.
PH can result from either increased pulmonary venous resistance (most common) or increased pulmonary arterial flow, such as with a left-to-right shunt.
The main factor in generating severe pulmonary hypertension is an arteriopathy, which has four main components:
- Muscular hypertrophy
- Intimal thickening
- Adventitial thickening
- Plexiform lesions: the focal proliferation of endothelial channels
NB Plexogenic arteriopathy is a term used to describe a constellation of vascular changes occurring in those with pulmonary arterial hypertension.
The earliest change is muscular hypertrophy in muscular arteries which with time result in changes in the more proximal arteries. Eventually, fibrosis of the wall occurs, at which point the process is irreversible.[3]
Clinical presentation[edit | edit source]
Classical clinical presentation of pulmonary arterial hypertension is the combination of
- Dyspnoea (especially with exercise)
- Elevated right heart pressures, including peripheral oedema and abdominal distention.
- An ECG may demonstrate right ventricular strain and hypertrophy.[3]
Treatment and Prognosis[edit | edit source]
- Medical therapy includes: calcium channel antagonists; nitric oxide; prostanoids, e.g. epoprostenol, treprostinil, iloprost; endothelin antagonists e.g. bosentan, sitaxentran, ambrisentan; phosphodiesterase inhibitors e.g. dipyridamole
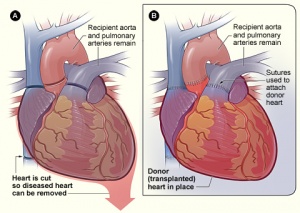
- In selected cases, combined heart and lung transplantation can be performed. Image R Heart transplantation.
- In patients with very high right heart pressures, an atrial septostomy (a procedure where a small hole is made in the wall between the left and right atria of the heart) has also been performed but is associated with high immediate mortality and reduces oxygenation due to the right-left shunt formed.
- In cases where pulmonary arterial hypertension is due to proximal pulmonary emboli, a pulmonary thromboendarterectomy is a surgical option.
Pulmonary arterial hypertension (PAH) carries a poor prognosis if not promptly diagnosed and appropriately treated. The development and approval of 14 medications over the last several decades have led to a rapidly evolving approach to therapy, and have necessitated periodic updating of evidence-based treatment guidelines[6].
Despite extensive research and recent advances in medical management prognosis remains poor, with a mean survival of only three years in untreated patients. Patients typically succumb to right heart failure or sudden death[3].
Physiotherapy[edit | edit source]
A range of common interventions that contributed to acute patient recovery and discharge by physiotherapists may include:
- Progressive walking programs
- Individualized bed- or chair-based exercise programs
- Chest treatment
- Breathing exercises
- Advice on breathlessness and pursed lip breathing
- Pacing advice re activities
- Oxygen assessments
- Providing treatment for relaxation
- Encouraging static cycling activities
- Education to client, family, and carers - patients often anxious about exercising and uncertain about how much exercise to do. They may have pre-existing negative ideas about the effects of physical activity, having been told in the past to avoid over-exertion; they may have previously experienced severe breathlessness and they felt exercise could cause them harm[1].
Pulmonary rehabilitation is a widely researched intervention for different respiratory conditions and referral for such intervention is of benefit.
Give Activity Guidelines:
- Restrict lifting, pushing, or shoving to less than 10 kg, since these activities increase the pressure in your arteries and lungs.
- Walking is important to keep muscles strong and improve circulation.
- Strenuous forms of aerobic exercise should not be done regularly since the lungs may not be able to keep up with the oxygen demands placed on the body during these activities.
- Activities that cause shortness of breath or dizziness should be avoided and pacing activities should be introduced[7].
Concluding Remarks[edit | edit source]
- Pulmonary hypertension (PH) is defined as mean pulmonary artery pressure (mPAP) 25 mmHg or greater at rest; this measurement is obtained during right heart catheterization.
- The exact prevalence of PH in the U.S. is unknown.
- Advances in hemodynamic studies of the right heart side and pulmonary circulations have helped improve our understanding of this condition. This better understanding aids the development of treatment agents aimed at improving quality of life, morbidity, and mortality.
- Awareness of this condition and understanding the classification of PH and the available treatment modalities is crucial[8].
- Physiotherapy for patients should promote physical activity, functional independence, and self-management as routine management of their PH[1]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Keen C, Fowler-Davis S, McLean S, Manson J. Physiotherapy practice in pulmonary hypertension: physiotherapist and patient perspectives. Pulmonary circulation. 2018 Jun;8(3):2045894018783738.
- ↑ Healthline PH Available from:https://www.healthline.com/health/pulmonary-hypertension-prognosis (accessed 14 August 2020)
- ↑ 3.0 3.1 3.2 3.3 3.4 Radiopedia Pulmonary Hypertension. Available from:https://radiopaedia.org/articles/pulmonary-hypertension-1 (accessed 14 August 2020)
- ↑ Radiopedia. Pulmonary hypertension (2013 classification). Available from:https://radiopaedia.org/articles/pulmonary-hypertension-2013-classification?lang=gb (accessed 14 August 2020)
- ↑ MedCram - Medical Lectures Explained CLEARLY . Pulmonary Hypertension Explained Clearly by MedCram.com. Available from: http://www.youtube.com/watch?v=V7LyWmFXuaY [last accessed 28/8/2020]
- ↑ Klinger JR, Elliott CG, Levine DJ, Bossone E, Duvall L, Fagan K, et al. Therapy for pulmonary arterial hypertension in adults: update of the CHEST guideline and expert panel report. Chest. 2019;155(3):565-86.
- ↑ Cleveland Clinic PH Available from:https://my.clevelandclinic.org/health/diseases/6530-pulmonary-hypertension-ph/management-and-treatment (accessed 14 August 2020)
- ↑ Gohar A, Shrestha A, Stys A. Pulmonary Hypertension: Brief Review Article. South Dakota Medicine. 2019;72(5).218-224.