Bone Stress Injuries
Original Editor - Puja Gaikwad
Top Contributors - Puja Gaikwad, Rucha Gadgil, Lucinda hampton, Kim Jackson and Vidya Acharya
Introduction[edit | edit source]
Bone Stress Injuries (BSI) are overuse injuries associated with repeated loading of bone by strenuous weight-bearing activities (such as running, jogging, marching) and inadequate recovery periods. BSI’s represent the failure of the skeleton bone to withstand repetitive loading, leading to structural fatigue, localized bone pain, and tenderness around the area.[1] Bone Stress Injuries (BSI) are commonly seen in avid runners, track and field athletes, endurance athletes, military recruits, gymnasts, dancers, but also among otherwise healthy people who have recently started the new or intensive physical activity [2]accounting for 10% of all sports-related injuries.[3] BSI differs in severity, with initial findings of periosteal edema and marrow edema. In more severe conditions, stress fractures with distinct fracture lines are present. Stress fractures account for > 10% of total sports-related injuries and it could be as high as 30% in running. [4]
Pathophysiology[edit | edit source]
When the bone is subjected to mechanical forces the forces cause adaptive changes in the trabecular (i.e internal architecture of bone), followed by secondary adaptive changes in the bone cortex (i.e external architecture of bone). In trabecular bone (also known as cancellous bone), the initial response to mechanical forces is the microdamage of the trabecular which is repaired by a microcallus. In cortical bone, the initial response to an increase in mechanical forces is osteoclastic activity (bone break down) which leads to resorption of bone. Osteoblastic cellular activity fills the resorption cavities with a lamellar bone. However, bone formation is slower than bone resorption.[5]
In normal healthy bone, new activities or prolonged amounts loading stimulate turn-over of bone cells. First, the body breaks down selected portions of the bone, temporarily weakening it, and then within 1-2 weeks, new bone tissue is laid down. Once established, the new bone is stronger, denser, and better accustomed to the new activity or increase load. However, if we continue high loading or impact activities during this turn-over period if we don’t give our bones adequate time to recover. Over time, the overloaded bone will accumulate micro-fractures and eventually break down, developing into what we call a bone stress injury.[6]
Bone Stress Continuum[edit | edit source]
There is a continuum of bone stress injury varying from "normal to bone strain/stress response to stress reaction to the ultimate progression of a stress fracture. These injuries sit on a continuum whereby they start with a stress reaction (often called a ‘hot spot) which can progress towards a stress fracture and finally towards a complete bone fracture. Essentially, as the BSI progresses along the continuum, the longer it takes to recover.[8] Therefore, an understanding and early recognition of these injuries are critical to any athlete and their sports-specific goals.
On the continuum, bone is accruing microdamage following mechanical forces from loading, for example from running. Microdamage accrues proportionate to the number of loading cycles, rate of loading, and strain magnitude of the skeleton bone. When the bone is given adequate time between loading cycles to recover the rate of bone resorption is met by the rate of bone repair and remodeling. However, when insufficient time is given for the bone to adapt to external mechanical forces, an imbalance may occur between bone remodeling and microdamage to the bone resulting in structural deformation of bone and fatigue This accumulative microdamage can continue to progress and result in further pathology. It can progress from the bone being in a state of stress reaction through to stress fracture and at times even frank cortical fracture. [9]
Stages of Bone Stress Injuries[edit | edit source]
There are three progressive stages of bone stress injuries:
- Bone strain/stress response: There are signs of bone stress on medical imaging but an athlete is not yet experiencing symptoms.
- Stress reaction: Bone stress injury is severe enough to cause localized pain on the bone, which aggravates with sporting activities. Athletes will often also experience tenderness to the touch.
- Stress fracture: The final stage of the bone stress continuum when a fracture or break in the bone develops, which can be seen on medical imaging. Typically pain is very pronounced in a clear localized area, and often bearing weight on the limb is enough to provoke pain.[5]
Common Locations[edit | edit source]
Common sites for bone stress injuries and bone stress fractures are primarily seen in the lower limbs. Common locations of Bone Stress Injuries are as follows:
- The front or inside of the tibia (shin bone)
- Fibula
- Metatarsal or carpal bones of the foot
- Medial malleolus of the ankle
- Neck or shaft of the femur
- Calcaneus[4]
Risk Factors[edit | edit source]
Bone stress injury risk factors could be grouped into two categories:
- Biomechanical factors- factors that modify and affect the load applied to a bone/skeleton
- Biological factors- factors that modify how bone resists strain and the resultant accumulation of damage.[10][11] (see Table 1)
| Biomechanical Factors | Biological Factors |
|---|---|
| Training errors: sudden increases in training loads (not allowing the bone sufficient time to adapt) | Athletic/physical activity history: previous history of BSI |
| Faulty biomechanics: Poor running form, and techniques | Medical history: Family history of BSI or osteoporosis/osteopenia, history of medications like the use of oral steroids, hormone therapies, cancer medications, antidepressants, antacids, anticonvulsants, etc. |
| Footwear: for example, wearing the wrong shoes | Low Energy availability/RED-S |
| Rigid training surface | Bone health: Lower bone mineral density |
| Poor muscle strength and endurance | Insufficient calcium and Vit D |
| Misalignment or anatomical problems like lean body mass, leg length discrepancy, small calf circumference, pes cavus, or pes planus, etc. | Poor diet and nutrition |
| Dynamic loading patterns: for example, greater vertical loading, peak hip adduction, and rearfoot eversion, etc. during gait. | Stress |
Table 1: Risk factors as proposed by Warden[12]
Classification[edit | edit source]
Injury classification systems may help to grade severity, choose treatment options, and determine prognosis. In athletes who show imaging changes compatible with the symptoms of BSIs, the anatomical location and imaging findings of the lesion are important factors. Based on the understanding of the biological healing process, knowledge of blood supply to the bone in different areas of the body, and the direction of loading on the bone, these locations have been classified into low, medium, and high risk of fracture [13](see Table 2 below). Low-risk BSIs are susceptible to compressive forces and normally heal well with activity modification, in which case normal weight-bearing is likewise possible. High-risk BSIs, on the other hand, are vulnerable to tensile forces and occur in areas with decreased blood flow. They are susceptible to delayed union or nonunion and are more likely to advance to complete fractures in a later stage.[14]
| Low | Medium | High |
|---|---|---|
| Posteromedial tibia | Pelvis (sacrum and pubic rami) | Femoral neck |
| Fibula/lateral malleolus | Femoral shaft | Patella |
| Calcaneus | Proximal tibia | Anterior tibial diaphysis |
| Diaphysis of second to fourth metatarsals | Cuboid | Medial malleolus |
| Cuneiform | Talus (lateral process) | |
| Great toe sesamoid | ||
| Navicular |
Table 2: Anatomical Location and Risk of BSI
In addition to risk classification by anatomical location, BSIs can be graded as per imaging findings (Table 3). In the grading system, grades 1& 2 are low-grade BSIs, whereas grades 3 and 4 can be classified as high-grade BSIs.[15] After low and high-grade BSIs, return-to-sport time was reported to be 13.1 weeks and 23.6 weeks, respectively.[16]
To sum it up, low-grade BSIs at low-risk sites having the best prognosis and the shortest return to sport. High-grade BSIs at low-risk sites must be identified, as they will need more time to return to play. Because BSIs at high-risk sites take a longer period to recover, careful treatment is required regardless of grade.[13]
Evaluation and Diagnosis[edit | edit source]
History taking and physical examination[edit | edit source]
Bone stress injuries are an overuse injury that is typified by a gradual onset of pain with activity. A thorough review of the athlete's training history is essential, looking for a spike, or rapid change in training load. In female athletes, evaluation of female athlete triads is vital, and dietary restriction behaviors, daily intake of calcium and vitamin D, and menstrual irregularities should be reviewed. The previous fractures and family history of low bone mineral density (BMD) should also be investigated.[17] Hormonal use, like oral contraceptives, and the use of drugs like steroids and antacids, which can affect bone health, should be reported.[18] In the early stages of the continuum, pain can be a mild diffuse ache during running that settles on rest. As the stress reaction progresses, pain may be significant during loading and in the late stages, pain can be present even at rest or with low load tasks like walking or at night.
On physical examination, Pain is usually localized and will be tender to palpate. Because direct palpation of deep areas is difficult at deeper sites, a single-leg hop test or fulcrum test of the femur shaft can be performed to provoke pain.[19] In more severe cases, changes in skin color and local edema can be visible.[18]
Assessment of bone health[edit | edit source]
For athletes with diagnosed BSIs, clinicians must measure BMD and perform an endocrine function assessment. According to the American College of Sports Medicine, Z-scores less than −1 are considered to be low bone mass in female athletes who take part in weight-bearing sports.[20] For male athletes, no criteria have yet been established. Z-scores less than −2 in both genders are considered as low bone density by the International Society for Clinical Densitometry.[21]
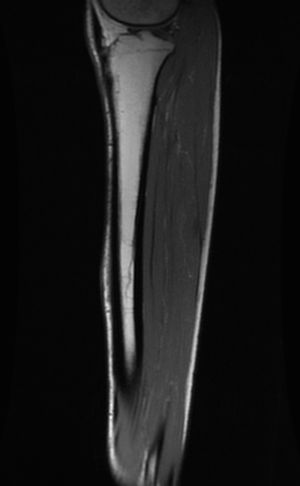
Imaging[edit | edit source]
Ultimately the gold standard method for identifying and diagnosing bone stress injuries (BSIs) is using Magnetic Resonance Imaging (MRI). MRIs are the most sensitive and specific imaging modality as compared to normal radiographic images (x-rays) as these images can look normal for the first few months despite clinical signs and symptoms of a bone stress injury. It typically takes a BSI to fully progress to a bone stress fracture to notice changes on an x-ray. With early imaging via an MRI, a bone stress injury can be detected, which can guide to appropriate intervention in efforts to avoid a full-blown bone stress fracture and delayed recovery period.[2] A stress reaction will show swelling (bone edema) on MRI. Recently, the use of diagnostic ultrasound is increasing and may be used in the field, enabling early detection of BSIs and continued use in the follow-up.[22][23]
| MRI Grade | Nattiv et al.[16] | Fredericson et al.[24] |
|---|---|---|
| 1 | Mild marrow or periosteal edema on T2; T1 normal | Mild to moderate periosteal edema on T2; normal marrow on T2 and T1 |
| 2 | Moderate marrow or periosteal edema plus positive T2 | Moderate to severe periosteal edema on T2; marrow edema on T2 but not T1 |
| 3 | Severe marrow or periosteal edema on T2 and T1 | Moderate to severe periosteal edema on T2; marrow edema on T2 and T1 |
| 4 | Severe marrow or periosteal edema on T2 and T1 plus fracture line on T2 or T1 | Moderate to severe periosteal edema on T2; marrow edema on T2 and T1; Fracture line present. |
Table 3: MRI grading scale
Management[edit | edit source]
The cornerstone of treatment involves understanding and correcting the factors that caused the injury, and a two-phase approach consisting of modifying activities and resuming gradual return to sport is used.[25] The rehabilitation time for a low-risk bone stress injury may vary depending on whether it is a simple stress reaction versus an advanced stress fracture, but the average healing time is 6-8 weeks.[13]
Phase I: Pain control[edit | edit source]
begins with pain control using analgesics along with physiotherapy treatment. Nonsteroidal anti-inflammatory drugs should not be used due to their potential negative effect on bone healing.[26] Tolerable weight-bearing is possible for daily activities, but temporary discontinuation of playing a particular sport and modification of activities are needed in the initial management of low-risk BSIs to allow for tissue healing and to limit pathological progression.
Phase II: Conditioning[edit | edit source]
- Cardiovascular Endurance Training: Maintaining conditioning while recovering from a BSI is important for a smooth return to sport. Since endurance training athletes experience cardiovascular insufficiency within 2 weeks after the discontinuance of training, conditioning exercises must be introduced early.[27] There are many ways to sustain cardiovascular fitness while recovering from a BSI, like swimming, cycling, deep-water running, and antigravity treadmill training[28][29], etc.
- Dietary Modifications to improve bone health: Ensure Sufficient Intake of Calcium and Vitamin D. All athletes with BSIs should be evaluated to ensure enough calcium and vitamin D intake, preferably through diet. Target values published by the Institute of Medicine based on age and sex are as follows:
- 600 IU of vitamin D daily is suggested for ages 9 to 70 years
- 800 IU of vitamin D daily is recommended for > 71 years or older
- 1300 mg of calcium daily for ages between 9 to 18 years.[30]
Phase III: Axial Loading Exercises[edit | edit source]
Once an athlete is pain-free for five consecutive days of usual activities, they can start a specific graduated axial loading program that has the goal of introducing controlled, progressive loads to the injured site. There are several variations of graduated loading programs and they can be individually customized; normally involves 30-minute sessions separated by rest days. These types of exercises are essential to optimally load the bone so that it can tolerate repetitive, submaximal forces that occur with high-impact activities such as running. Below are a few examples of various exercises which can be incorporated into a cross-training program.
- Marching
- single-leg squats or skater squat
- Loaded carries with the hex bar
- Biking
- POGOS: Pogos are a really nice way to introduce impact along with being easy to measure. Keep a track of total contacts with the ground, or keep track of how many rounds the athlete did and for how long. For instance, start with three rounds of the 30s and count how many times total did athlete contact the ground. The goal would be to increase volume to a few sets performed two to three times a day as bone remodeling does better with small bouts of loading dispersed throughout the day versus a lot of volumes done all at once. Allow for adequate recovery and bone remodeling to take place by taking off days as needed.
- Treadmill walking
- High-intensity resistance training (HIRT)
- Gait re-training [13]
High-risk BSIs require different management. It can vary from prolongation of activity modification to non-weight bearing, with or without a cast and/or surgical fixation.[31] Complete healing must be confirmed prior to return to play in order to prevent full fracture and other complications.[32]
Phase IV: Return to sport[edit | edit source]
The first stage begins with walking for 30 minutes and progressing to increasing durations of jogging (running at 50% of normal pace) and decreasing the duration of walking. The second stage involves progressively increasing the pace of running until running for 30 minutes at a usual pace, with the third stage consisting of running on two consecutive days followed by a rest day. The final stage includes individualized running until complete return to desired running activities.[13]
Progress through every stage of the running program is determined by pain at the site of bone stress injury. If an athlete is able to complete a session with no pain and does not encounter latent symptoms (i.e. pain later that day/night or the next morning), they can safely proceed to the next level of the program with the knowledge that the injury is tolerating the load.[2] If, however, pain is experienced at the bone stress injury site they need to immediately stop the session and, at the next session, return to the previous level they were able to successfully complete. Progress is through the program is often linear; nevertheless, setbacks do occur, particularly early in the rehabilitation program when the pathology can be a little more finicky. The key is to progress only as fast as the pathology will allow by giving attention to pain provocation.[13]
Approximate return to sport timelines for male and female track and cross-country runners have been stated as follows:
- Grade 1: 11.4 weeks ( 4.5 weeks)
- Grade 2: 13.5 weeks ( 2.1 weeks)
- Grade 3: 18.8 weeks ( 2.9 weeks)
- Grade 4: 31.7 weeks ( 3.7 weeks)[16]
Prevention[edit | edit source]
- Ball sports participation during adolescence: Engaging in ball sports such as soccer and basketball during adolescence for two years has been stated to reduce the risk of BSI.[34]
- Sufficient intake of calcium and vitamin D: Getting enough calcium and vitamin D may reduce the risk of BSIs. Female runners consuming 800 mg of calcium daily are 6 times more prone to acquire stress fractures than those who consume 1,500 mg daily.[35]
- Identification and prevention of female athlete triad: In female athletes, identification and correction of energy imbalance, and recovery of menstrual function may be the best way to maintain proper bone health during adolescence.[36]
- Preparticipation screening: Some behavior and activity patterns must be examined for all athletes at the pre-participation screening.[36] This includes drinking more than ten bottles per week, smoking, participation in excessive physical activity with insufficient rest time, a sudden increase in physical activity, and running mainly on hard surfaces.[37][38]
References[edit | edit source]
- ↑ Song SH, Koo JH. Bone Stress Injuries in Runners: a Review for Raising Interest in Stress Fractures in Korea. Journal of Korean medical science. 2020 Mar 2;35(8).
- ↑ 2.0 2.1 2.2 Pegrum J, Crisp T, Padhiar N. Diagnosis and management of bone stress injuries of the lower limb in athletes. Bmj. 2012 Apr 24;344.
- ↑ Spitz DJ, Newberg AH. Imaging of stress fractures in the athlete. Radiologic Clinics. 2002 Mar 1;40(2):313-31.
- ↑ 4.0 4.1 Robertson GA, Wood AM. Lower limb stress fractures in sport: optimizing their management and outcome. World journal of orthopedics. 2017 Mar 18;8(3):242.
- ↑ 5.0 5.1 Kiuru MJ, Pihlajamäki HK, Ahovuo JA. Bone stress injuries. Acta Radiologica. 2004 May;45(3):000-.
- ↑ Warden SJ, Burr DB. Bone Stress Injuries. Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism. 2018 Sep 25:450.
- ↑ DPT 7120 Chapter 2 Bone Stress Injuries. Available from: https://www.youtube.com/watch?v=Nw-DGdTp-u4
- ↑ Tenforde AS, Kraus E, Fredericson M. Bone stress injuries in runners. Physical Medicine and Rehabilitation Clinics. 2016 Feb 1;27(1):139-49.
- ↑ Roche M, Fredericson M, Kraus E. Bone Stress Injuries. InClinical Care of the Runner 2020 Jan 1 (pp. 141-151). Elsevier.
- ↑ Troy KL, Davis IS, Tenforde AS. A Narrative Review of Metatarsal Bone Stress Injury in Athletic Populations: Etiology, Biomechanics, and Management. PM&R. 2020 Nov 6.
- ↑ Wright AA, Taylor JB, Ford KR, Siska L, Smoliga JM. Risk factors associated with lower extremity stress fractures in runners: a systematic review with meta-analysis. British journal of sports medicine. 2015 Dec 1;49(23):1517-23.
- ↑ Warden SJ, Burr DB, Brukner PD. Stress fractures: pathophysiology, epidemiology, and risk factors. Current osteoporosis reports. 2006 Sep;4(3):103-9.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 Warden SJ, Davis IS, Fredericson M. Management and prevention of bone stress injuries in long-distance runners. journal of orthopaedic & sports physical therapy. 2014 Oct;44(10):749-65.
- ↑ Tenforde AS, Parziale AL, Popp KL, Ackerman KE. Low bone mineral density in male athletes is associated with bone stress injuries at anatomic sites with greater trabecular composition. The American journal of sports medicine. 2018 Jan;46(1):30-6.
- ↑ Chen YT, Tenforde AS, Fredericson M. Update on stress fractures in female athletes: epidemiology, treatment, and prevention. Current reviews in musculoskeletal medicine. 2013 Jun 1;6(2):173-81.
- ↑ 16.0 16.1 16.2 Nattiv A, Kennedy G, Barrack MT, Abdelkerim A, Goolsby MA, Arends JC, Seeger LL. Correlation of MRI grading of bone stress injuries with clinical risk factors and return to play: a 5-year prospective study in collegiate track and field athletes. The American journal of sports medicine. 2013 Aug;41(8):1930-41.
- ↑ Tenforde AS, Carlson JL, Sainani KL, Chang AO, Kim JH, Diaz R, Golden NH, Fredericson M. Lower Trabecular Bone Score and Spine Bone Mineral Density Are Associated With Bone Stress Injuries and Triad Risk Factors in Collegiate Athletes. PM&R. 2020 Oct 10.
- ↑ 18.0 18.1 Tenforde AS, Kraus E, Fredericson M. Bone stress injuries in runners. Physical Medicine and Rehabilitation Clinics. 2016 Feb 1;27(1):139-49.
- ↑ Johnson AW, Weiss Jr CB, Wheeler DL. Stress fractures of the femoral shaft in athletes—more common than expected: a new clinical test. The American Journal of Sports Medicine. 1994 Mar;22(2):248-56.
- ↑ Deimel JF, Dunlap BJ. The female athlete triad. Clinics in sports medicine. 2012 Apr 1;31(2):247-54.
- ↑ Lewiecki EM, Gordon CM, Baim S, Leonard MB, Bishop NJ, Bianchi ML, Kalkwarf HJ, Langman CB, Plotkin H, Rauch F, Zemel BS. International Society for Clinical Densitometry 2007 adult and pediatric official positions. Bone. 2008 Dec 1;43(6):1115-21.
- ↑ Medeiros S. Clinical considerations. Fundamentals of Emergency Ultrasound. 2019 Oct 3:321.
- ↑ Papalada A, Malliaropoulos N, Tsitas K, Kiritsi O, Padhiar N, Del Buono A, Maffulli N. Ultrasound as a primary evaluation tool of bone stress injuries in elite track and field athletes. The American journal of sports medicine. 2012 Apr;40(4):915-9.
- ↑ Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial stress reaction in runners: correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. The American journal of sports medicine. 1995 Jul;23(4):472-81.
- ↑ Raasch WG, Hergan DJ. Treatment of stress fractures: the fundamentals. Clinics in sports medicine. 2006 Jan 1;25(1):29-36.
- ↑ Ziltener JL, Leal S, Fournier PE. Non-steroidal anti-inflammatory drugs for athletes: an update. Annals of physical and rehabilitation medicine. 2010 May 1;53(4):278-88.
- ↑ Coyle EF, Martin 3rd WH, Sinacore DR, Joyner MJ, Hagberg JM, Holloszy JO. Time course of loss of adaptations after stopping prolonged intense endurance training. Journal of Applied Physiology. 1984 Dec 1;57(6):1857-64.
- ↑ Donaghe HE. Physiological Response to Body Weight-Supported Treadmill Exercise in Healthy Adults. University of California, Davis; 2011.
- ↑ de Heer HD, Kline JR, Charley B. Anti-Gravity Treadmill Training for Prevention and Rehabilitation of Running Injuries. InClinical Care of the Runner 2020 Jan 1 (pp. 113-130). Elsevier.
- ↑ Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary reference intakes. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. 1997.
- ↑ Miller TL, Kaeding CC, Rodeo SA. Emerging options for biologic enhancement of stress fracture healing in athletes. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2020 Jan 1;28(1):1-9.
- ↑ Kaeding CC, Najarian RG. Stress fractures: classification and management. The Physician and sportsmedicine. 2010 Oct 1;38(3):45-54.
- ↑ Understanding and Optimizing Recovery from Bone Stress Injuries. Available from: https://www.youtube.com/watch?v=-XBU_SfdQBc
- ↑ Tenforde AS, Sainani KL, Sayres LC, Milgrom C, Fredericson M. Participation in ball sports may represent a prehabilitation strategy to prevent future stress fractures and promote bone health in young athletes.
- ↑ Nieves JW, Melsop K, Curtis M, Kelsey JL, Bachrach LK, Greendale G, Sowers MF, Sainani KL. Nutritional factors that influence change in bone density and stress fracture risk among young female cross-country runners. PM&R. 2010 Aug 1;2(8):740-50.
- ↑ 36.0 36.1 Chen YT, Tenforde AS, Fredericson M. Update on stress fractures in female athletes: epidemiology, treatment, and prevention. Current reviews in musculoskeletal medicine. 2013 Jun 1;6(2):173-81.
- ↑ Patel DS, Roth M, Kapil N. Stress fractures: diagnosis, treatment, and prevention. American family physician. 2011 Jan 1;83(1):39-46.
- ↑ Wentz L, Liu PY, Ilich JZ, Haymes EM. Dietary and training predictors of stress fractures in female runners. International journal of sport nutrition and exercise metabolism. 2012 Oct 1;22(5):374-82.