Sacroiliac Joint: Difference between revisions
No edit summary |
No edit summary |
||
| Line 10: | Line 10: | ||
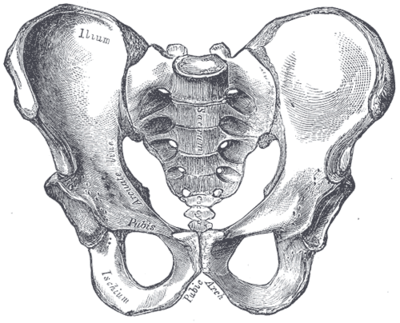
* Each innominate is formed by the fusion of the three bones of the pelvis: the ilium, ischium, and pubic [[bone]].<ref name="Dutton">Dutton M. Orthopaedic Examination, Evaluation, and Intervention. 2nd ed. New York: McGraw Hill, 2008. </ref> | * Each innominate is formed by the fusion of the three bones of the pelvis: the ilium, ischium, and pubic [[bone]].<ref name="Dutton">Dutton M. Orthopaedic Examination, Evaluation, and Intervention. 2nd ed. New York: McGraw Hill, 2008. </ref> | ||
* The sacroiliac joints are essential for [[Lumbosacral Biomechanics|effective load transfer]] between the spine and the lower extremities. | * The sacroiliac joints are essential for [[Lumbosacral Biomechanics|effective load transfer]] between the spine and the lower extremities. | ||
* It functions both as a shock absorber for the spine above and converts torque from the lower extremities into the rest of the body. | |||
* The sacrum, pelvis and spine-, are functionally interrelated through [[muscle]]<nowiki/>s, [[fascia]] and [[Ligament|ligamentous]] interconnections. | * The sacrum, pelvis and spine-, are functionally interrelated through [[muscle]]<nowiki/>s, [[fascia]] and [[Ligament|ligamentous]] interconnections. | ||
| Line 16: | Line 17: | ||
* The strong ligamentous system of the joint makes it better designed for stability and limits the amount of motion available.<ref name="Cohen">Cohen SP. Sacroiliac Joint Pain: A Comprehensive Review of Anatomy, Diagnosis, and Treatment. ''Anesth Analg'' 2005; 101:1440-1453.</ref> | * The strong ligamentous system of the joint makes it better designed for stability and limits the amount of motion available.<ref name="Cohen">Cohen SP. Sacroiliac Joint Pain: A Comprehensive Review of Anatomy, Diagnosis, and Treatment. ''Anesth Analg'' 2005; 101:1440-1453.</ref> | ||
* Nutation and Counternutation - movements that happen at the sacroiliac joint | * Nutation and Counternutation - movements that happen at the sacroiliac joint | ||
Nutation is the motion that occurs when force (weight) is absorbed at the sacroiliac joint, and occurs in the direction of gravitational forces (toward the ground). Counternutation is the body’s response, lifting the joint up against gravity.<ref>serola biomechanic [https://www.serola.net/nutation-counternutation-what-are-they-and-why-are-they-so-important/ Nutation] Available from:https://www.serola.net/nutation-counternutation-what-are-they-and-why-are-they-so-important/ (last accessed 12.6.2020)</ref> | Nutation is the motion that occurs when force (weight) is absorbed at the sacroiliac joint, and occurs in the direction of gravitational forces (toward the ground). Counternutation is the body’s response, lifting the joint up against gravity.<ref>serola biomechanic [https://www.serola.net/nutation-counternutation-what-are-they-and-why-are-they-so-important/ Nutation] Available from:https://www.serola.net/nutation-counternutation-what-are-they-and-why-are-they-so-important/ (last accessed 12.6.2020)</ref>In most individuals, this motion is limited to 2 to 4 mm of movement due to the bony architecture and ligamentous structures of the joint.<ref name=":1" /> | ||
Nutation occurs | Nutation occurs | ||
| Line 31: | Line 32: | ||
* Surrounded by a fibrous capsule containing a joint space filled with synovial fluid between the articular surfaces. | * Surrounded by a fibrous capsule containing a joint space filled with synovial fluid between the articular surfaces. | ||
* Articular surface is made up of two, strong, C-shaped layers. | * Articular surface is made up of two, strong, C-shaped layers. | ||
* It is distinguished from other synovial joints by the unusual articulation of two different types of cartilage. | * It is distinguished from other synovial joints by the unusual articulation of two different types of [[cartilage]]. | ||
* The sacral capsular surface is composed of hyaline cartilage ( Hyaline cartilage is made from type II collagen and is the weakest type of cartilage) | * The sacral capsular surface is composed of hyaline cartilage ( Hyaline cartilage is made from type II collagen and is the weakest type of cartilage) | ||
* Iliac capsular surface is composed of fibrocartilage (Fibrocartilage is made from type I collagen and is the strongest type of cartilage)<ref>Wong M, Kiel J. [https://www.ncbi.nlm.nih.gov/books/NBK507801/#:~:text=The%20SI%20joint%20is%20a,strong%2C%20C%2Dshaped%20layers. Anatomy, Abdomen and Pelvis, Sacroiliac Joint.] InStatPearls [Internet] 2019 Feb 6. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK507801/#:~:text=The%20SI%20joint%20is%20a,strong%2C%20C%2Dshaped%20layers. (last accessed 12.6.2020)</ref>. . | * Iliac capsular surface is composed of fibrocartilage (Fibrocartilage is made from type I collagen and is the strongest type of cartilage)<ref name=":1">Wong M, Kiel J. [https://www.ncbi.nlm.nih.gov/books/NBK507801/#:~:text=The%20SI%20joint%20is%20a,strong%2C%20C%2Dshaped%20layers. Anatomy, Abdomen and Pelvis, Sacroiliac Joint.] InStatPearls [Internet] 2019 Feb 6. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK507801/#:~:text=The%20SI%20joint%20is%20a,strong%2C%20C%2Dshaped%20layers. (last accessed 12.6.2020)</ref>. . | ||
'''Ligaments: '''[[Image:Gray319.png|Anterior view of the ligaments of the sacroiliac joint|right|frameless]] | '''Ligaments: ''' | ||
A strong [[Ligament|ligamentous]] architecture stabilizes the SI joint. | |||
The interosseous sacroiliac ligament forms the major connection between the sacrum and the ilium. It is the strongest ligament in the body and prevents anterior and inferior movement of the sacrum.[[Image:Gray319.png|Anterior view of the ligaments of the sacroiliac joint|right|frameless]] | |||
*<u>Anterior Sacroiliac</u> - an anteroinferior thickening of the fibrous capsule that is weak and thin when compared to the other ligaments of the joint. It connects the third sacral ligament to the lateral side of the preauricular sulcus and is better developed closer to the arcuate line and the PSIS. This ligament is injured most often and is a common source of pain because of its thinness.<br> | *<u>Anterior Sacroiliac</u> - an anteroinferior thickening of the fibrous capsule that is weak and thin when compared to the other ligaments of the joint. It connects the third sacral ligament to the lateral side of the preauricular sulcus and is better developed closer to the arcuate line and the PSIS. This ligament is injured most often and is a common source of pain because of its thinness.<br> | ||
| Line 42: | Line 47: | ||
*<u>Sacrotuberous</u> - consists of three large fibrous bands and is blended with the posterior (dorsal) sacroiliac ligament. It stabilizes against nutation of the sacrum and counteracts against posterior and superior migration of the sacrum during weight bearing.<br> | *<u>Sacrotuberous</u> - consists of three large fibrous bands and is blended with the posterior (dorsal) sacroiliac ligament. It stabilizes against nutation of the sacrum and counteracts against posterior and superior migration of the sacrum during weight bearing.<br> | ||
*<u>Sacrospinous</u> - triangular shaped and thinner than the sacrotuberous ligament and goes from the ischial spine to the lateral parts of the sacrum and coccyx and then to the ischial spine laterally. Along with the sacrotuberous ligament, it opposes forward tilting of the sacrum on the innominates during weight bearing.<ref name="Dutton" /><ref name="Levangie" /> <br> | *<u>Sacrospinous</u> - triangular shaped and thinner than the sacrotuberous ligament and goes from the ischial spine to the lateral parts of the sacrum and coccyx and then to the ischial spine laterally. Along with the sacrotuberous ligament, it opposes forward tilting of the sacrum on the innominates during weight bearing.<ref name="Dutton" /><ref name="Levangie" /> <br> | ||
== Nerves == | |||
* The sacroiliac joint is well innervated but the pattern of innervation varies among individuals. | |||
* The sacroiliac joint receives its innervation from the ventral rami of L4 and L5, superior gluteal nerve, and dorsal rami of L5-S2. | |||
* The nerve supply to the SI joint varies between individuals and innervation may be almost exclusively derived from the sacral dorsal rami (may account for the variable patterns of referred pain from the SI joint)<ref name=":1" />. | |||
== Muscles == | == Muscles == | ||
There are 35 muscles that attach to the sacrum or innominates which mainly provide stability to the joint rather than producing movements.<ref>Calvillo O., Skaribas I., Turnispeed J., Anatomy and pathophysiology of the SIJ, current science, 2000 (LOE 2A)</ref> | There are 35 muscles that attach to the sacrum or innominates which mainly provide stability to the joint rather than producing movements.<ref>Calvillo O., Skaribas I., Turnispeed J., Anatomy and pathophysiology of the SIJ, current science, 2000 (LOE 2A)</ref> | ||
== Specific Pathologies == | == Specific Pathologies == | ||
| Line 96: | Line 67: | ||
*[[Pubic Symphysis Dysfunction|Pubic symphysis dysfunction]] | *[[Pubic Symphysis Dysfunction|Pubic symphysis dysfunction]] | ||
*[[Osteoarthritis|Osteoarthritis]] | *[[Osteoarthritis|Osteoarthritis]] | ||
*[[Sacral Insufficiency Fractures|Stress fracture]] | *[[Sacral Insufficiency Fractures|Stress fracture]] | ||
== Epidemiology == | == Epidemiology == | ||
| Line 102: | Line 73: | ||
The reported prevalence of sacroiliac joint pain in cases of chronic low back and lower extremity pain is estimated to be between 10 - 27%<ref name="Sim">Simopoulos T. Manchikanti L. Singh V. Gupta S. Hameed H. Diwan S. Cohen P. A Systematic valuation of Prevalence and Diagnostic Accuracy of Sacroiliac Joint Interventions. Pain Physician 2012; 15:E305-E344 (http://www.painphysicianjournal.com/2012/may/2012;15;E305-E344.pdf)</ref>. There are several reported predisposing factors for SIJ pain such as a leg length discrepancy, age, arthritis, previous spine surgery, pregnancy and trauma. Compared with face and discogenic low back pain, SIJ pain is more likely to be reported as a specific inciting event, and present unilaterally below L5 and the pain patterns are extremely variable<ref name="Cohen" />. | The reported prevalence of sacroiliac joint pain in cases of chronic low back and lower extremity pain is estimated to be between 10 - 27%<ref name="Sim">Simopoulos T. Manchikanti L. Singh V. Gupta S. Hameed H. Diwan S. Cohen P. A Systematic valuation of Prevalence and Diagnostic Accuracy of Sacroiliac Joint Interventions. Pain Physician 2012; 15:E305-E344 (http://www.painphysicianjournal.com/2012/may/2012;15;E305-E344.pdf)</ref>. There are several reported predisposing factors for SIJ pain such as a leg length discrepancy, age, arthritis, previous spine surgery, pregnancy and trauma. Compared with face and discogenic low back pain, SIJ pain is more likely to be reported as a specific inciting event, and present unilaterally below L5 and the pain patterns are extremely variable<ref name="Cohen" />. | ||
== Special Tests<ref name=" | == Special Tests == | ||
* The potential differential diagnosis of lower back pain is extensive. | |||
<u>SI Joint Stress tests</u> | * The clinical examination of the patient with sacroiliac joint dysfunction begins with an evaluation of gait, leg-length inequality, and examination of the lower lumbar region. | ||
* During a physical examination, localization over the SI joint should be attempted using the Fortin finger test. The test is considered positive when the point of tenderness is within 2 cm inferomedial to the posterior superior iliac spine. In addition to the physical exam maneuvers above, the hip joint and spine should be properly evaluated to rule out other pathologies<ref name=":1" />. | |||
<u>SI Joint Stress tests</u><ref name="Dutton" /> | |||
* | *Anterior Gapping test | ||
*[[Distraction Test|Posterior Distraction test]] | *[[Distraction Test|Posterior Distraction test]] | ||
* | *Pubic Stress test | ||
* | *Sacrotuberous Ligament Stress test | ||
* | *Sacral Compression test | ||
*Rotational Stress test | *Rotational Stress test | ||
<u>Leg Length tests</u> | <u>Leg Length tests</u> | ||
| Line 117: | Line 90: | ||
*Prone test | *Prone test | ||
*Standing leg length test | *Standing leg length test | ||
*Functional leg length test | *Functional leg length test | ||
<u>Other Special Tests</u> | <u>Other Special Tests</u> | ||
| Line 124: | Line 97: | ||
*[[Supine Long Sitting Test|Long Sit test]] | *[[Supine Long Sitting Test|Long Sit test]] | ||
*[[Sign of the Buttock|Sign of the Buttock]] | *[[Sign of the Buttock|Sign of the Buttock]] | ||
*[[Gaenslen Test|Gaenslen's test]] | *[[Gaenslen Test|Gaenslen's test]] | ||
*[[Yeoman's Test|Yeoman's test]] | *[[Yeoman's Test|Yeoman's test]] | ||
*[[FABER Test|FABER (Figure-Four) test]] | *[[FABER Test|FABER (Figure-Four) test]] | ||
* | *Straight Leg Raise - 70-90deg<ref>Magee, DJ. Orthopedic Physical Assessment. 5th ed. St Louis:Saunders, an imprint of Elsevier INC, 2008.</ref> | ||
== | == Back Pain == | ||
* The incidence of lower back pain originating from the sacroiliac joint may be as high as 27%. | |||
* Patients often describe a specific trauma or inciting event. | |||
* Pain originating from the sacroiliac joint is likely more common than most providers realize due to difficulty in localizing symptoms and referred pain patterns. | |||
* Using a pain diagram to map out the location of the pain is often very helpful in diagnosis. | |||
* SI joint pain is commonly found 10 cm caudally and 3 cm laterally from the patient's posterior superior iliac spine. | |||
* SI joint pain is commonly referred to the buttocks, lower lumbar region, groin, and lateral thigh. Patients with sacroiliac joint dysfunction describe their pain being aggravated by getting out of a chair, prolonged standing or sitting, with climbing stairs or morning stiffness. | |||
* Numbness and tingling in the leg may also be present. Risk factors for sacroiliac joint pain include leg length discrepancy, age, arthritis, history of spine surgery, pregnancy, and trauma<ref name=":1" /> | |||
[[Image:Gray241.png|right|Sacroiliac joint|frameless|400x400px]]The SI joint goes through many changes throughout life. In early childhood, the surfaces of the joint are smooth and allow gliding motions in many directions.<ref name="Levangie" /> After puberty, the surface of the ilium becomes rougher and coated with fibrous plaques that will restrict motion significantly. These age-related changes will increase in the third and fourth decade and by the sixth decade motion may become noticeably restricted. By the eighth decade, plaque will form and erosions will be present.<ref name="Cohen" /> <br> | [[Image:Gray241.png|right|Sacroiliac joint|frameless|400x400px]]The SI joint goes through many changes throughout life. In early childhood, the surfaces of the joint are smooth and allow gliding motions in many directions.<ref name="Levangie" /> After puberty, the surface of the ilium becomes rougher and coated with fibrous plaques that will restrict motion significantly. These age-related changes will increase in the third and fourth decade and by the sixth decade motion may become noticeably restricted. By the eighth decade, plaque will form and erosions will be present.<ref name="Cohen" /> <br> | ||
Revision as of 08:05, 12 June 2020
Original Editors - Kathleen Nestor
Top Contributors - Kathleen Nestor, Admin, Lucinda hampton, Alexandra Kopelovich, Tony Lowe, Katie Sheidler, Kim Jackson, Scott Buxton, Tyler Shultz, Laura Ritchie, Evan Thomas, WikiSysop, Abbey Wright, Rachael Lowe, Yvonne Yap, 127.0.0.1 and Jenna Nodding
Description[edit | edit source]
The Sacroiliac joint (simply called the SI joint) is the joint connection between the spine and the pelvis.
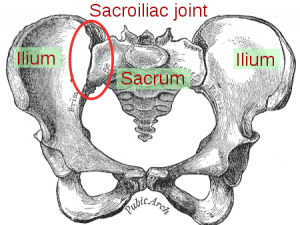
- Large diarthrodial joint[1] made up of the sacrum and the two innominates of the pelvis.
- Each innominate is formed by the fusion of the three bones of the pelvis: the ilium, ischium, and pubic bone.[2]
- The sacroiliac joints are essential for effective load transfer between the spine and the lower extremities.
- It functions both as a shock absorber for the spine above and converts torque from the lower extremities into the rest of the body.
- The sacrum, pelvis and spine-, are functionally interrelated through muscles, fascia and ligamentous interconnections.
Motions Available [edit | edit source]
- The main function of the SI joint is to provide stability and attenuate forces to the lower extremities.
- The strong ligamentous system of the joint makes it better designed for stability and limits the amount of motion available.[3]
- Nutation and Counternutation - movements that happen at the sacroiliac joint
Nutation is the motion that occurs when force (weight) is absorbed at the sacroiliac joint, and occurs in the direction of gravitational forces (toward the ground). Counternutation is the body’s response, lifting the joint up against gravity.[4]In most individuals, this motion is limited to 2 to 4 mm of movement due to the bony architecture and ligamentous structures of the joint.[5]
Nutation occurs
- when the sacrum absorbs shock; it moves down, forward, and rotates to the opposite side.
- as the sacrum moves anteriorly and inferiorly, the coccyx moves posteriorly relative to the ilium.[6]
- This motion is opposed by the wedge shape of the sacrum, the ridges and depression of the articular surfaces, the friction coefficient of the joint surface, and the integrity of the posterior, interosseous, and sacrotuberous ligaments that are also supported by muscles that insert into the ligaments.[2]
Counternutation
- the sacrum moves up, backward, and rotates to the same side that absorbs the force.[6] This motion is opposed by the posterior sacroiliac ligament that is supported by the multifidus.[2]
Ligaments & Joint Capsule[edit | edit source]
Joint
- The SI joint is a diarthrodial synovial joint.
- Surrounded by a fibrous capsule containing a joint space filled with synovial fluid between the articular surfaces.
- Articular surface is made up of two, strong, C-shaped layers.
- It is distinguished from other synovial joints by the unusual articulation of two different types of cartilage.
- The sacral capsular surface is composed of hyaline cartilage ( Hyaline cartilage is made from type II collagen and is the weakest type of cartilage)
- Iliac capsular surface is composed of fibrocartilage (Fibrocartilage is made from type I collagen and is the strongest type of cartilage)[5]. .
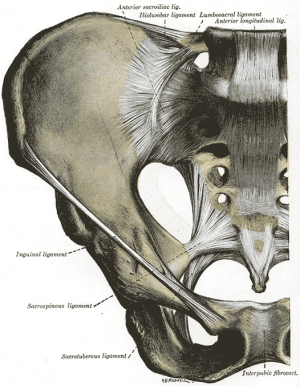
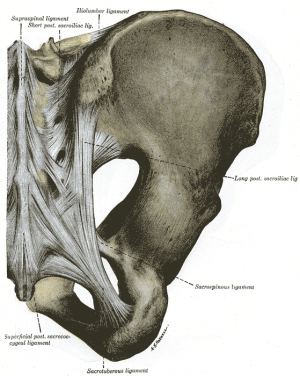
Ligaments:
A strong ligamentous architecture stabilizes the SI joint.
The interosseous sacroiliac ligament forms the major connection between the sacrum and the ilium. It is the strongest ligament in the body and prevents anterior and inferior movement of the sacrum.
- Anterior Sacroiliac - an anteroinferior thickening of the fibrous capsule that is weak and thin when compared to the other ligaments of the joint. It connects the third sacral ligament to the lateral side of the preauricular sulcus and is better developed closer to the arcuate line and the PSIS. This ligament is injured most often and is a common source of pain because of its thinness.
- Interosseus Sacroiliac - forms the major connection between the sacrum and the innominate and is a strong, short ligament deep to the posterior sacroiliac ligament. It resists anterior and inferior movement of the sacrum.
- Posterior (Dorsal) Sacroiliac - connects the PSIS with the lateral crest of the third and fourth segments of the sacrum and is very stong and tough. Nutation, which is anterior motion of the sacrum, slackens the ligament, and counternutation, which is posterior motion will make the ligament taut. It can be palpated directly below the PSIS and can often be a source of pain.[7]
- Sacrotuberous - consists of three large fibrous bands and is blended with the posterior (dorsal) sacroiliac ligament. It stabilizes against nutation of the sacrum and counteracts against posterior and superior migration of the sacrum during weight bearing.
- Sacrospinous - triangular shaped and thinner than the sacrotuberous ligament and goes from the ischial spine to the lateral parts of the sacrum and coccyx and then to the ischial spine laterally. Along with the sacrotuberous ligament, it opposes forward tilting of the sacrum on the innominates during weight bearing.[2][6]
Nerves[edit | edit source]
- The sacroiliac joint is well innervated but the pattern of innervation varies among individuals.
- The sacroiliac joint receives its innervation from the ventral rami of L4 and L5, superior gluteal nerve, and dorsal rami of L5-S2.
- The nerve supply to the SI joint varies between individuals and innervation may be almost exclusively derived from the sacral dorsal rami (may account for the variable patterns of referred pain from the SI joint)[5].
Muscles[edit | edit source]
There are 35 muscles that attach to the sacrum or innominates which mainly provide stability to the joint rather than producing movements.[8]
Specific Pathologies[edit | edit source]
There are many pathologies that could present at the site of the sacroiliac joint including:[2]
- Sacroiliac tuberculosis
- Spondyloarthropathy
- Crystal and pyogenic arthropathies
- Groin pain
- Osteitis pubis
- Pubic symphysis dysfunction
- Osteoarthritis
- Stress fracture
Epidemiology[edit | edit source]
The reported prevalence of sacroiliac joint pain in cases of chronic low back and lower extremity pain is estimated to be between 10 - 27%[9]. There are several reported predisposing factors for SIJ pain such as a leg length discrepancy, age, arthritis, previous spine surgery, pregnancy and trauma. Compared with face and discogenic low back pain, SIJ pain is more likely to be reported as a specific inciting event, and present unilaterally below L5 and the pain patterns are extremely variable[3].
Special Tests[edit | edit source]
- The potential differential diagnosis of lower back pain is extensive.
- The clinical examination of the patient with sacroiliac joint dysfunction begins with an evaluation of gait, leg-length inequality, and examination of the lower lumbar region.
- During a physical examination, localization over the SI joint should be attempted using the Fortin finger test. The test is considered positive when the point of tenderness is within 2 cm inferomedial to the posterior superior iliac spine. In addition to the physical exam maneuvers above, the hip joint and spine should be properly evaluated to rule out other pathologies[5].
SI Joint Stress tests[2]
- Anterior Gapping test
- Posterior Distraction test
- Pubic Stress test
- Sacrotuberous Ligament Stress test
- Sacral Compression test
- Rotational Stress test
Leg Length tests
- Prone test
- Standing leg length test
- Functional leg length test
Other Special Tests
- Seated Flexion test (Piedallu's Sign)
- Long Sit test
- Sign of the Buttock
- Gaenslen's test
- Yeoman's test
- FABER (Figure-Four) test
- Straight Leg Raise - 70-90deg[10]
Back Pain[edit | edit source]
- The incidence of lower back pain originating from the sacroiliac joint may be as high as 27%.
- Patients often describe a specific trauma or inciting event.
- Pain originating from the sacroiliac joint is likely more common than most providers realize due to difficulty in localizing symptoms and referred pain patterns.
- Using a pain diagram to map out the location of the pain is often very helpful in diagnosis.
- SI joint pain is commonly found 10 cm caudally and 3 cm laterally from the patient's posterior superior iliac spine.
- SI joint pain is commonly referred to the buttocks, lower lumbar region, groin, and lateral thigh. Patients with sacroiliac joint dysfunction describe their pain being aggravated by getting out of a chair, prolonged standing or sitting, with climbing stairs or morning stiffness.
- Numbness and tingling in the leg may also be present. Risk factors for sacroiliac joint pain include leg length discrepancy, age, arthritis, history of spine surgery, pregnancy, and trauma[5]
The SI joint goes through many changes throughout life. In early childhood, the surfaces of the joint are smooth and allow gliding motions in many directions.[6] After puberty, the surface of the ilium becomes rougher and coated with fibrous plaques that will restrict motion significantly. These age-related changes will increase in the third and fourth decade and by the sixth decade motion may become noticeably restricted. By the eighth decade, plaque will form and erosions will be present.[3]
The ligaments of the SI ligament complex are weaker in women than in men, allowing the ability to give birth.[11]
Related Pages[edit | edit source]
Resources[edit | edit source]
Wheeless' Textbook of Orthopaedics
References[edit | edit source]
- ↑ Cohen S., Steven P., Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis and treatment, IARS, November 2005, volume 101, issue 5, pp 1440-1453 (LOE 3A)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Dutton M. Orthopaedic Examination, Evaluation, and Intervention. 2nd ed. New York: McGraw Hill, 2008.
- ↑ 3.0 3.1 3.2 Cohen SP. Sacroiliac Joint Pain: A Comprehensive Review of Anatomy, Diagnosis, and Treatment. Anesth Analg 2005; 101:1440-1453.
- ↑ serola biomechanic Nutation Available from:https://www.serola.net/nutation-counternutation-what-are-they-and-why-are-they-so-important/ (last accessed 12.6.2020)
- ↑ 5.0 5.1 5.2 5.3 5.4 Wong M, Kiel J. Anatomy, Abdomen and Pelvis, Sacroiliac Joint. InStatPearls [Internet] 2019 Feb 6. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK507801/#:~:text=The%20SI%20joint%20is%20a,strong%2C%20C%2Dshaped%20layers. (last accessed 12.6.2020)
- ↑ 6.0 6.1 6.2 6.3 Levangie PK, Norkin CC. Joint Structure and Function: A Comprehensive Analysis. 4th ed. Philadelphia: F.A. Davis, 2005.
- ↑ Vleeming A, Pool-Goudzwaard AL, Hammudoghlu D, Stoeckart R, Snijders CJ, Mens JM. The function of the long dorsal sacroiliac ligament: its implication for understanding low back pain. Spine 1996;21:556-62 (LOE 3A)
- ↑ Calvillo O., Skaribas I., Turnispeed J., Anatomy and pathophysiology of the SIJ, current science, 2000 (LOE 2A)
- ↑ Simopoulos T. Manchikanti L. Singh V. Gupta S. Hameed H. Diwan S. Cohen P. A Systematic valuation of Prevalence and Diagnostic Accuracy of Sacroiliac Joint Interventions. Pain Physician 2012; 15:E305-E344 (http://www.painphysicianjournal.com/2012/may/2012;15;E305-E344.pdf)
- ↑ Magee, DJ. Orthopedic Physical Assessment. 5th ed. St Louis:Saunders, an imprint of Elsevier INC, 2008.
- ↑ Calvillo O., Skaribas I., Turnispeed J., Anatomy and pathophysiology of the SIJ, current science, 2000 (LOE 2A)