Physical Activity and Respiratory Conditions: Difference between revisions
No edit summary |
No edit summary |
||
| Line 105: | Line 105: | ||
For individuals who develop EIB or asthmalike symptoms with exercise, a rapid-acting β2-agonist should be taken before exercise. Individuals with asthma should also incorporate a progressive warm-up and should try to avoid exercising in the excessive cold or environments with known asthma triggers<ref name=":2" /> | For individuals who develop EIB or asthmalike symptoms with exercise, a rapid-acting β2-agonist should be taken before exercise. Individuals with asthma should also incorporate a progressive warm-up and should try to avoid exercising in the excessive cold or environments with known asthma triggers<ref name=":2" /> | ||
{| width="100%" cellspacing="1" cellpadding="1" | |||
|- | |||
|{{#ev:youtube|VR7QnSnHmBU|300}} | |||
|{{#ev:youtube|Tgy_eQs4A5w|300}} | |||
== Resources == | == Resources == | ||
The [https://gpcpd.walesdeanery.org/index.php/welcome-to-motivate-2-move Motivate2Move] website, created by Wales Deanery, has a useful section on physical activity and [https://gpcpddev.walesdeanery.org/index.php/respiratory-diseases respiratory disease]. | The [https://gpcpd.walesdeanery.org/index.php/welcome-to-motivate-2-move Motivate2Move] website, created by Wales Deanery, has a useful section on physical activity and [https://gpcpddev.walesdeanery.org/index.php/respiratory-diseases respiratory disease]. | ||
Revision as of 18:09, 18 October 2017
- Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!
- If you would like to get involved in this project and earn accreditation for your contributions, please get in touch!
Tips for writing this page:
Please consider including the following topics in this page plus other subjects that you think are appropriate:
- x
- x
A quick word on content:
When you write this page please include:
- Evidence (where appropriate and available
- References
- Images and videos
- A list of open online resources that we can link to
- Links to other pages in this project
Example content:
Original Editor - Add a link to your Physiopedia profile here.
Top Contributors - Mariam Hashem, Kim Jackson, Wendy Walker, Admin, Rachael Lowe, Tony Lowe, Evan Thomas, Michelle Lee, Tarina van der Stockt, Adam Vallely Farrell, Vidya Acharya, Rucha Gadgil and Lucinda hampton
Introduction[edit | edit source]
Chronic respiratory diseases are a group of chronic diseases affecting the airways and the other structures of the lungs. Common chronic respiratory diseases are (Asthma, Bronchiectasis, chronic obstructive pulmonary disease COPD, Chronic rhinosinusitis, Hypersensitivity pneumonitis,Lung cancer, cystic fibrosis, Adult Respiratory Distress syndrome)[1]
Physical activity (PA) is defined as any bodily movement produced by skeletal muscles which results in energy expenditure. Physical activity in daily life can be categorized into occupational, sports, conditioning, household, or other activities. Exercise is a subset of physical activity that is planned, structured, and repetitive and has as a final or an intermediate objective the improvement or maintenance of physical fitness.[2]
Why Exercise?[edit | edit source]
Increased PA is associated with enhanced psychological functioning and quality of life, improved cardiorespiratory fitness, and decreased morbidity.[3]
Increasing physical fitness may be beneficial for children with asthma by increasing exercise tolerance and capacity and, as a consequence, the threshold for inducing a condition called exercise-induced bronchoconstriction (EIB).[3] A low level of regular physical activity, in turn, leads to chronic deconditioning. It is not surprising, therefore, that some studies have found that patients with asthma tend to have lower cardiorespiratory fitness than their healthy counterparts. [4][5][6]
Physical training programs in asthma have been designed to enhance aerobic power, neuromuscular coordination, and self-confidence.[7]Reduced activity levels observed in asthmatics may also increase the incidence of obesity, with negative consequences on self-esteem .[8][9]
physical activity levels play a key role in the onset of muscle dysfunction and deconditioning and have been associated with quality of life, hospital admission, comorbidities, lung function decline and mortality.[10][11] Skeletal muscle dysfunction is now recognized as a major problem for COPD patients[12] , and, as such, the use of strength training as a modality to reverse the deleterious effects of the disease is now recommended[13] . A recent systematic review demonstrated strength training could improve skeletal muscle strength in COPD patients, and these improvements were associated with increased activities of daily living [14]
Gardiner et al. showed that a strength training program can decrease the atrophy and strength loss associated with steroid use. They also demonstrated that the extent of fast-twitch muscle atrophy resulting from chronic glucocorticoid treatment can be lessened by mild weight-lifting exercise. [15]
Key Evidence:[edit | edit source]
Barriers/ Limitations to Physical Activities[edit | edit source]
There are many barriers that could limit the participation of a chronic respiratory condition patient in exercises.
Children and adolescents with asthma may experience frustration, embarrassment and low self confidence because of their disease-related limitations.[16] [17]They may also withdraw from PA because of their parents’ fear and protectiveness.[18]
the fear of breathlessness (Dyspnoea) inhibits many patients from taking part in PA.[19]
cardiovascular disease, peripheral vascular disease, lung cancer, diabetes, dyslipidemia, hypertension, osteoporosis, and psychological disorders[20] Corticosteroid use, overuse of bronchodilators, and interactions with other medications can further complicate management of PA programs in these patients. Other concerns during both rest and exercise include pulmonary hypertension, gas-trapping, dynamic hyperinflation, poor gas exchange, and increased respiratory pressure associated with destruction of lung parenchyma and increased airway resistance.[21]
To facilitate engagement in exercise programs many approaches should be addressed, such as managing acute dyspnoea[22], Psychosocial and behavioral interventions through educational sessions focusing on specific problems such as stress management, instructions in relaxation exercises, panic control,and smoking cessation[23]. Nutritional interventions should be considered[24], as well as social support, the option to participate in group activities, and the availability of professional support are frequently reported as enablers of physical activity.[25]
EXERCISE PRESCRIPTION:[edit | edit source]
Individualized exercise training prescriptions should be based on patient characteristics, such as baseline pulmonary function, exercise capacity, habitual physical activity levels, inflammation and infection status to establish favorable exercise-training induced effects.[26]
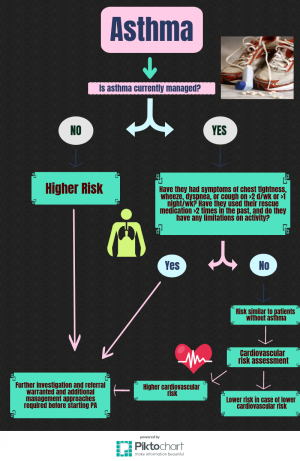
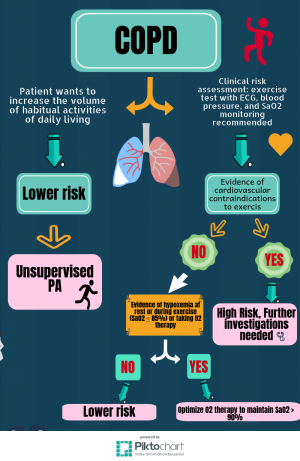
Burr, Davidson, Shephard and Eves Developed two clinical decision trees for assessing the risk of adverse events during PA in patients with COPD ad Asthma. These decision trees can be used to categorize a patient as higher or lower risk, informing the requirements of PA prescription and the monitoring of exercise programs. The info-graphs below illustrate the clinical decision trees:
INTERVAL TRAINING:[edit | edit source]
In patients with advanced COPD, interval exercise consisting of repeated bouts (30–60 s) of high- or even maximal-intensity work (80–100% peak) separated by periods (30–60 s) of lower intensity work intervals, has been shown to be associated with a small increase in arterial lactate concentration, lower ventilation and degrees of dynamic hyperinflation and lower symptoms of dyspnoea and leg discomfort, thus allowing the total amount of work performed to be significantly greater than that of constant-load exercise.[27]
Implementation of high-intensity interval training in patients with COPD has proven to be effective in terms of improvements in muscle fibre oxidative capacity, thus enhancing the utilization of oxygen by the exercising muscles. [28]
Aerobic Exercises:[edit | edit source]
Moderate aerobic exercises is defined as exercise, which noticeably accelerates heart rate and requires 3.0 to 6.0 metabolic equivalents (METs) (e.g. slow cycling, brisk walking or swimming), whereas vigorous aerobic exercise requires more than 6.0 METs and causes rapid breathing and a substantial increase in heart rate (e.g. running fast, swimming laps, singles tennis)[29]
A large body of evidence demonstrates important health benefits from aerobic exercise, including decreases in dynamic hyperinflation and exertional dyspnea; improved exercise tolerance; and enhanced quality of life, with fewer disease exacerbations and reported sick days.[30]
STRENGTH TRAINING:[edit | edit source]
To optimize the benefits gleaned from a strength training program, the exercise prescription variables of intensity, volume and frequency should be tailored to the needs of each patient.[31]
strength training exercises be performed at an intensity of approximately 60% of the muscle’s maximum force generating capacity to increase strength. To determine the amount of weight of the appropriate stimulus, the common approach is based on a 1 repetition maximum, (1-RM) or the ability to lift or perform a movement only once before fatigue prevents a subsequent contraction. If the weight employed is below 60% of the 1-RM, there may be only modest improvements of 5% to 10% in strength.
The volume of the strength training exercise is a function of the number of repetitions and sets of an exercise completed. For frail patients, the ACSM recommends that at least one set of each exercise be performed. As patients increase the intensity of their exercise prescription, the number of sets of an exercise may also increase. Once the patient can complete the pre-determined number of repetitions for all the prescribed sets, the resistance should be increased. Specific exercises should target strength improvements for the major muscle groups which include the chest, shoulders, arms, upper and lower back, abdomen, hips and legs. One or more exercises can be prescribed for each of these muscle groups depending upon the patient’s specific needs.
The final component of the exercise prescription that needs to be considered is frequency or the number of times the exercise should be performed per week. Outpatient recommendations stipulate that individuals exercise 2 to 3 times per week and to allow 48 hours of recovery between exercise bouts.[32]
PRECAUTIONS:[edit | edit source]
Exercises should be discouraged during periods of active infection in patients with Cystic Fibrosis.[26]
patients with substantial hypoxemia (SpO2 < 90%) at rest or during exertion, uncontrolled asthma, or the presence of pulmonary hypertension should be optimally medically managed before starting exercise[30]
Persons with COPD who wish to become more physically active should be evaluated using a graded exercise test including ECG monitoring and pulse oximetry. Remarkable test results and evidence of serious cardiovascular conditions (ie, angina, ischemia, complex ectopy, high-degree AV block, uncontrolled blood pressure) should be seen by the appropriate specialist before commencing PA[30]
Supervising exercise professionals should have specific training with and monitor for potential pulmonaryrelated complications as well as complications related to the common sequelae and comorbidities of COPD[30]
To reduce the risk of exercise-related adverse events, those with asthma should make sure that their disease is properly controlled before becoming more physically active. Those with poor or partial control of their asthma should see their physicians before becoming more active[30]
For individuals who develop EIB or asthmalike symptoms with exercise, a rapid-acting β2-agonist should be taken before exercise. Individuals with asthma should also incorporate a progressive warm-up and should try to avoid exercising in the excessive cold or environments with known asthma triggers[30]
Resources[edit | edit source]The Motivate2Move website, created by Wales Deanery, has a useful section on physical activity and respiratory disease. References[edit | edit source]
|