Neuroblastoma: Difference between revisions
No edit summary |
No edit summary |
||
| (146 intermediate revisions by 11 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors '''- Colleen Mathews [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | |||
'''Original Editors '''- Colleen Mathews [[Pathophysiology of Complex Patient Problems|from Bellarmine University's | |||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
[[File:Neuroblastoma.jpeg|right|frameless]] | |||
Neuroblastoma is the most common solid tumour of childhood. | |||
'''Image 1: Giant neuroblastoma in an Ethiopian shepherd child''' | |||
It is almost exclusively a childhood [[Oncology|cancer]] occurring most commonly between the ages of 0-5 years. Neuroblastomas are cancers that start in early [[Neurone|nerve cells]] (called neuroblasts) of the [[Sympathetic Nervous System|sympathetic nervous system]]. This means that tumours can be found anywhere along this system; most commonly (about 50%) start in the [[Adrenal Glands|adrenal glands]] (above the [[kidney]]), or near the spine, chest, neck or [[pelvis]]. | |||
= | Rarely, a neuroblastoma has spread so widely by the time it is found, doctors can’t tell exactly where it started.<ref name=":1">Neuroblastoma Australia [https://www.neuroblastoma.org.au/pages/faqs/category/what-is-neuroblastoma What is neuroblastoma?] Available:https://www.neuroblastoma.org.au/pages/faqs/category/what-is-neuroblastoma (accessed 14.10.2021)</ref> | ||
Due to the high variability in its presentation, clinical signs and symptoms at presentation can range from benign palpable mass with distension to major illness from substantial tumor spread.<ref name=":2">Mahapatra S, Challagundla KB. [https://www.ncbi.nlm.nih.gov/books/NBK448111/ Cancer, neuroblastoma]. Cancer. 1918 Apr 13;10:49. 2021 Available: https://www.ncbi.nlm.nih.gov/books/NBK448111/ (accessed 14.10.2021)</ref> | |||
== | This video (3 minutes) is of the common symptoms of neuroblastoma | ||
''<nowiki/>''{{#ev:youtube|L9r_y4BnIzw|300}}<ref name=":4" /> | |||
== Epidemiolgy == | |||
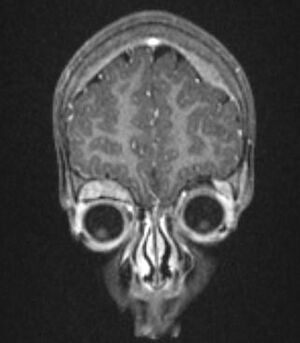
[[File:Neuroblastoma infant.jpeg|right|frameless|295x295px]] | |||
The tumours typically occur in infants and very young children (mean age of presentation being ~22 months) with 95% of cases diagnosed before the age of 10 years. Occasionally, they may be identified antenatally or immediately at birth.<ref name=":3">Radiopedia [https://radiopaedia.org/articles/neuroblastoma Neuroblastoma] Available:https://radiopaedia.org/articles/neuroblastoma (accessed 14.10.2021)</ref> | |||
'''Image 2''': STAGE IV-S NEUROBLASTOMA This infant has massive hepatomegaly due to metastatic neuroblastoma. Intra-abdominal pressure is partially relieved by a silastic pouch. | |||
== | == Etiology == | ||
There are no known reasons as to why this cancer occurs and there are no clear environmental links. Risk factors for the acquisition of mutations in key genes leading to neuroblastoma have yet to be identified, although exposures during conception and pregnancy are a topic of investigation. Neuroblastoma can develop either sporadically or be transmitted in the germline<ref name=":2" />. | |||
There are rare cases where neuroblastoma runs in families due to a [[Genetic Disorders|genetic mutation]], but in most cases there is no known genetic cause.<ref name=":1" /> | |||
== Characteristics/Clinical Presentation == | |||
[[File:Raccooneyes.jpg|thumb|Raccoon eyes]]Neuroblastoma presents in a variety of forms based upon the location of its manifestation and the size of the tumor.<ref name="Ped-Onc">Thiele CJ. [https://www.nature.com/articles/nrdp201678#Sec20 Neuroblastoma]. InHuman cell culture 2002 (pp. 21-53). Springer, Dordrecht.</ref>. Presentation is typically with [[Pain Behaviours|pain]] or a palpable mass and abdominal distension. The neuroblastoma presentation changes if cancer has spread (metastasis), and if the tumor secretes [[hormones]]. At the time of the patient's diagnosis, neuroblastoma cells have already spread to other parts of the body 73% of the time due to local mass effect.[[File:Neuroblastoma mets.jpg|thumb|Orbital and skull vault neuroplastoma]]Other accompanying syndromes include: | |||
== | |||
Neuroblastoma | |||
< | |||
The | |||
= | * Hutchinson syndrome: skeletal metastases may present with skeletal pain or limping and irritability or proptosis with periorbital and cranial bumps. | ||
* Pepper syndrome: hepatomegaly due to extensive liver metastasis | |||
* Blueberry muffin syndrome: multiple cutaneous lesions | |||
* Opsomyoclonus: rapid, involuntary conjugate fast eye movements | |||
* Proptosis and periorbital ecchymoses ("raccoon eyes"): orbital metastases<ref name=":3" /> | |||
This video (3 minutes) is of the common symptoms of neuroblastoma | |||
''<nowiki/>''{{#ev:youtube|L9r_y4BnIzw|300}}<ref name=":4"> | |||
Health Apta. SYMPTOMS OF NEUROBLASTOMA. Available from: http://www.youtube.com/watch?v=L9r_y4BnIzw[last accessed on 29/ 6/2021]</ref> | |||
== Location == | |||
Neuroblastomas arise from the sympathetic nervous system. Intra-abdominal disease (two-thirds of cases) is more prevalent than intrathoracic disease. Specific sites include: | |||
* Adrenal glands: most common site of origin, 35% | |||
* Retroperitoneum: 30-35% | |||
* Coeliac axis | |||
* Paravertebral sympathetic chain | |||
* Posterior mediastinum: 20% | |||
* Neck: 1-5% | |||
* Pelvis: 2-3% | |||
== Treatment and Prognosis == | |||
Treatment depends on the patient's stage. Localised tumours considered to be 'low-risk' are surgically excised, and patients tend to do very well (see below). In 'high-risk' tumours, a combination of [[Surgery and General Anaesthetic|surgery]], [[Chemotherapy Side Effects and Syndromes|chemotherapy]] +/- [[Bone Marrow|bone marrow]] transplantation is employed, unfortunately with poor overall results. In some cases, where tumours are very large, pre-surgical chemotherapy to attempt to downstage the tumour may be administered. | |||
== | Patients with stage 1, 2, or 4S have a better prognosis. Unfortunately 40-60% of patients present with stage 3 or 4 diseases 4. For advanced disease, the age of the child is most important.<ref name=":3" /> | ||
== Stages of Neuroblastoma == | |||
The International Neuroblastoma Staging System (INSS) based on surgical resection is used to stage neuroblastomas in the United States. | |||
''' | <u>'''Stage 1:'''</u> The percentage of children diagnosed at this stage is 21%. | ||
<u>Stage | <u>'''Stage 2:'''</u> The percentage of children diagnosed at this stage is 15% | ||
The | <u>'''Stage 3:'''</u> The percentage of children diagnosed at this stage is 17%. | ||
<u>Stage | <u>'''Stage 4:'''</u> The percentage of children diagnosed at this stage is 41%. | ||
<u>'''Stage 4S:'''</u> The percentage of children diagnosed at this stage is 6%.<ref name="cncf staging">Children's Neuroblastoma Cancer Foundation: neuroblastoma staging. http://www.cncfhope.org/Staging_Neuroblastoma (accessed on 7 March 2011).</ref> | |||
'''Poor prognostic factors:''' later age of onset: >18 months; higher stage: particularly in the presence of metastasis; N-Myc mutation; chromosome 1p deletion; unfavourable Shimada histology index | |||
< | '''Better prognostic factors:''' TRK-A expression<ref name=":3" /> | ||
== Diagnosis == | |||
Neuroblastoma may be difficult to diagnose as symptoms often do not become apparent until the tumour has reached a certain size. Even then symptoms may be subtle and similar to other more common non-serious childhood diseases. As a result it often takes some time before the final diagnosis of neuroblastoma is made<ref name=":1" />. | |||
The | The clinical presentation along with initial [[Laboratory Tests|laboratory testing]], such as complete [[Blood Physiology|blood]] count, serum [[electrolytes]], [[Liver Function Tests|liver function tests]], [[Chest X-Rays|chest radiograph]], [[urine]] or serum catecholamines may show abnormalities. Imaging such as [[CT Scans|CT]] scan (neck, chest, abdomen), [[Ultrasound Scans|ultrasound]], [[MRI Scans|MRI]], iodine-metaiodobenzylguanidine (MIBG) scan, and fluorodeoxyglucose positive emission tomography (FDG-PET) can be utilized for the detection of primary or secondary tumors. The confirmation of neuroblastoma can only be done by biopsy from a specimen obtained from a tumor or bone marrow.<ref name=":0">Pain assist Best Exercises/Activities For Neuroblastoma Patients Available:https://www.epainassist.com/fitness-and-exercise/best-exercises-activities-for-neuroblastoma-patients (accessed 14.10.2021)</ref> | ||
< | == Summary == | ||
Neuroblastoma is a rare abdominal tumor in young children. However, if the diagnosis is missed, the tumor is fatal. Hence, the diagnosis and treatment of neuroblastoma are best managed by an interprofessional team that includes a pediatrician, a pediatric surgeon, oncologist, radiation therapist, social workers, pharmacist, dietitian, and specialty care nurses. A team dedicated to childhood cancers is vital as these patients have special needs. All cancer treatments can stunt growth, and hence, a dietitian should be involved early in the care.<ref name=":2" /> | |||
== Physical Therapy Management == | |||
[[Image:Wiihab.jpg|alt=|right|frameless]]Advances in treatment have led to an increase in the number of cancer survivors. However, childhood cancers are associated with a lot of late effects, such as impaired growth and development, cognition, neurological function, musculoskeletal, cardiopulmonary function, and secondary tumors. Children also experience impaired physical fitness owing to [[Chemotherapy Side Effects and Syndromes|chemotherapy]], [[Radiation Side Effects and Syndromes|radiation therapy]], and surgical intervention. It includes decreased muscle strength and cardiopulmonary function, fatigue, and altered physical function. Incorporating exercises soon after treatment can improve cardiopulmonary and musculoskeletal function and increase the opportunities for participating in recreational activities<ref name=":0" />. | |||
'''Image 5''': Wiihab | |||
[[Quality of Life|Quality of life]] is an important theme when it comes to treating children with neuroblastoma and any form of childhood cancer. Side effects of the cancer treatment/medication (chemotherapy, radiation, etc.) and symptoms of cancer itself can lead to a risk of musculoskeletal and neurological issues and psychosocial changes <ref name="CSM">Miale, S presenter. Improving the Quality of Life of Children with Cancer: The Role of Rehabilitation. Presented at Combined Sections Meeting of the American Physical Therapy Association; 2011 February 9-12; New Orleans, Louisiana.</ref> eg Neurological changes including (peripheral neuropathy and radiculopathy); Musculoskeletal changes (disuse atrophy and joint contractures due to radiation fibrosis); Psychosocial (developmental delay, depression and anxiety, social Isolation, behavioral Issues)<ref name="CSM" /> | |||
== Case Reports/ Case Studies == | == Case Reports/ Case Studies == | ||
*[https://pubmed.ncbi.nlm.nih.gov/8776703/ Case-control study of neuroblastoma in West-Germany after the Chernobyl accident: case-control study.] | |||
*[https://pubmed.ncbi.nlm.nih.gov/7429428/ Placental infiltration in congenital neuroblastoma: a case study with ultrastructure.] | |||
*[https://www.nature.com/articles/6605504 Paternal occupation and neuroblastoma]: a case-control study based on cancer registry data for Great Britain 1962–1999.<br> | |||
* | |||
== References == | |||
<references /> | <references /> | ||
[[Category:Oncology]] | |||
[[Category:Medical]] | |||
[[Category:Paediatrics]] | |||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]] | ||
[[Category:Paediatrics - Conditions]] | |||
Latest revision as of 04:41, 14 October 2021
Original Editors - Colleen Mathews from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Colleen Mathews, Lucinda hampton, Khloud Shreif, Elaine Lonnemann, Admin, Fasuba Ayobami, Kim Jackson, Tony Lowe, Evan Thomas, WikiSysop and Wendy Walker
Introduction[edit | edit source]
Neuroblastoma is the most common solid tumour of childhood.
Image 1: Giant neuroblastoma in an Ethiopian shepherd child
It is almost exclusively a childhood cancer occurring most commonly between the ages of 0-5 years. Neuroblastomas are cancers that start in early nerve cells (called neuroblasts) of the sympathetic nervous system. This means that tumours can be found anywhere along this system; most commonly (about 50%) start in the adrenal glands (above the kidney), or near the spine, chest, neck or pelvis.
Rarely, a neuroblastoma has spread so widely by the time it is found, doctors can’t tell exactly where it started.[1]
Due to the high variability in its presentation, clinical signs and symptoms at presentation can range from benign palpable mass with distension to major illness from substantial tumor spread.[2]
This video (3 minutes) is of the common symptoms of neuroblastoma
Epidemiolgy[edit | edit source]
The tumours typically occur in infants and very young children (mean age of presentation being ~22 months) with 95% of cases diagnosed before the age of 10 years. Occasionally, they may be identified antenatally or immediately at birth.[4]
Image 2: STAGE IV-S NEUROBLASTOMA This infant has massive hepatomegaly due to metastatic neuroblastoma. Intra-abdominal pressure is partially relieved by a silastic pouch.
Etiology[edit | edit source]
There are no known reasons as to why this cancer occurs and there are no clear environmental links. Risk factors for the acquisition of mutations in key genes leading to neuroblastoma have yet to be identified, although exposures during conception and pregnancy are a topic of investigation. Neuroblastoma can develop either sporadically or be transmitted in the germline[2].
There are rare cases where neuroblastoma runs in families due to a genetic mutation, but in most cases there is no known genetic cause.[1]
Characteristics/Clinical Presentation[edit | edit source]
Neuroblastoma presents in a variety of forms based upon the location of its manifestation and the size of the tumor.[5]. Presentation is typically with pain or a palpable mass and abdominal distension. The neuroblastoma presentation changes if cancer has spread (metastasis), and if the tumor secretes hormones. At the time of the patient's diagnosis, neuroblastoma cells have already spread to other parts of the body 73% of the time due to local mass effect.
Other accompanying syndromes include:
- Hutchinson syndrome: skeletal metastases may present with skeletal pain or limping and irritability or proptosis with periorbital and cranial bumps.
- Pepper syndrome: hepatomegaly due to extensive liver metastasis
- Blueberry muffin syndrome: multiple cutaneous lesions
- Opsomyoclonus: rapid, involuntary conjugate fast eye movements
- Proptosis and periorbital ecchymoses ("raccoon eyes"): orbital metastases[4]
This video (3 minutes) is of the common symptoms of neuroblastoma
Location[edit | edit source]
Neuroblastomas arise from the sympathetic nervous system. Intra-abdominal disease (two-thirds of cases) is more prevalent than intrathoracic disease. Specific sites include:
- Adrenal glands: most common site of origin, 35%
- Retroperitoneum: 30-35%
- Coeliac axis
- Paravertebral sympathetic chain
- Posterior mediastinum: 20%
- Neck: 1-5%
- Pelvis: 2-3%
Treatment and Prognosis[edit | edit source]
Treatment depends on the patient's stage. Localised tumours considered to be 'low-risk' are surgically excised, and patients tend to do very well (see below). In 'high-risk' tumours, a combination of surgery, chemotherapy +/- bone marrow transplantation is employed, unfortunately with poor overall results. In some cases, where tumours are very large, pre-surgical chemotherapy to attempt to downstage the tumour may be administered.
Patients with stage 1, 2, or 4S have a better prognosis. Unfortunately 40-60% of patients present with stage 3 or 4 diseases 4. For advanced disease, the age of the child is most important.[4]
Stages of Neuroblastoma[edit | edit source]
The International Neuroblastoma Staging System (INSS) based on surgical resection is used to stage neuroblastomas in the United States.
Stage 1: The percentage of children diagnosed at this stage is 21%.
Stage 2: The percentage of children diagnosed at this stage is 15%
Stage 3: The percentage of children diagnosed at this stage is 17%.
Stage 4: The percentage of children diagnosed at this stage is 41%.
Stage 4S: The percentage of children diagnosed at this stage is 6%.[6]
Poor prognostic factors: later age of onset: >18 months; higher stage: particularly in the presence of metastasis; N-Myc mutation; chromosome 1p deletion; unfavourable Shimada histology index
Better prognostic factors: TRK-A expression[4]
Diagnosis[edit | edit source]
Neuroblastoma may be difficult to diagnose as symptoms often do not become apparent until the tumour has reached a certain size. Even then symptoms may be subtle and similar to other more common non-serious childhood diseases. As a result it often takes some time before the final diagnosis of neuroblastoma is made[1].
The clinical presentation along with initial laboratory testing, such as complete blood count, serum electrolytes, liver function tests, chest radiograph, urine or serum catecholamines may show abnormalities. Imaging such as CT scan (neck, chest, abdomen), ultrasound, MRI, iodine-metaiodobenzylguanidine (MIBG) scan, and fluorodeoxyglucose positive emission tomography (FDG-PET) can be utilized for the detection of primary or secondary tumors. The confirmation of neuroblastoma can only be done by biopsy from a specimen obtained from a tumor or bone marrow.[7]
Summary[edit | edit source]
Neuroblastoma is a rare abdominal tumor in young children. However, if the diagnosis is missed, the tumor is fatal. Hence, the diagnosis and treatment of neuroblastoma are best managed by an interprofessional team that includes a pediatrician, a pediatric surgeon, oncologist, radiation therapist, social workers, pharmacist, dietitian, and specialty care nurses. A team dedicated to childhood cancers is vital as these patients have special needs. All cancer treatments can stunt growth, and hence, a dietitian should be involved early in the care.[2]
Physical Therapy Management[edit | edit source]
Advances in treatment have led to an increase in the number of cancer survivors. However, childhood cancers are associated with a lot of late effects, such as impaired growth and development, cognition, neurological function, musculoskeletal, cardiopulmonary function, and secondary tumors. Children also experience impaired physical fitness owing to chemotherapy, radiation therapy, and surgical intervention. It includes decreased muscle strength and cardiopulmonary function, fatigue, and altered physical function. Incorporating exercises soon after treatment can improve cardiopulmonary and musculoskeletal function and increase the opportunities for participating in recreational activities[7].
Image 5: Wiihab
Quality of life is an important theme when it comes to treating children with neuroblastoma and any form of childhood cancer. Side effects of the cancer treatment/medication (chemotherapy, radiation, etc.) and symptoms of cancer itself can lead to a risk of musculoskeletal and neurological issues and psychosocial changes [8] eg Neurological changes including (peripheral neuropathy and radiculopathy); Musculoskeletal changes (disuse atrophy and joint contractures due to radiation fibrosis); Psychosocial (developmental delay, depression and anxiety, social Isolation, behavioral Issues)[8]
Case Reports/ Case Studies[edit | edit source]
- Case-control study of neuroblastoma in West-Germany after the Chernobyl accident: case-control study.
- Placental infiltration in congenital neuroblastoma: a case study with ultrastructure.
- Paternal occupation and neuroblastoma: a case-control study based on cancer registry data for Great Britain 1962–1999.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Neuroblastoma Australia What is neuroblastoma? Available:https://www.neuroblastoma.org.au/pages/faqs/category/what-is-neuroblastoma (accessed 14.10.2021)
- ↑ 2.0 2.1 2.2 Mahapatra S, Challagundla KB. Cancer, neuroblastoma. Cancer. 1918 Apr 13;10:49. 2021 Available: https://www.ncbi.nlm.nih.gov/books/NBK448111/ (accessed 14.10.2021)
- ↑ 3.0 3.1 Health Apta. SYMPTOMS OF NEUROBLASTOMA. Available from: http://www.youtube.com/watch?v=L9r_y4BnIzw[last accessed on 29/ 6/2021]
- ↑ 4.0 4.1 4.2 4.3 Radiopedia Neuroblastoma Available:https://radiopaedia.org/articles/neuroblastoma (accessed 14.10.2021)
- ↑ Thiele CJ. Neuroblastoma. InHuman cell culture 2002 (pp. 21-53). Springer, Dordrecht.
- ↑ Children's Neuroblastoma Cancer Foundation: neuroblastoma staging. http://www.cncfhope.org/Staging_Neuroblastoma (accessed on 7 March 2011).
- ↑ 7.0 7.1 Pain assist Best Exercises/Activities For Neuroblastoma Patients Available:https://www.epainassist.com/fitness-and-exercise/best-exercises-activities-for-neuroblastoma-patients (accessed 14.10.2021)
- ↑ 8.0 8.1 Miale, S presenter. Improving the Quality of Life of Children with Cancer: The Role of Rehabilitation. Presented at Combined Sections Meeting of the American Physical Therapy Association; 2011 February 9-12; New Orleans, Louisiana.