Introduction to Foot Neuropathy
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (6/08/2023)
Original Editor - User Name
Top Contributors - Stacy Schiurring, Jess Bell and Matt Huey
Introduction[edit | edit source]
diabetes is a global epidemic. It's been found to affect more than 537 million adults worldwide. 75% of those individuals have been found to come from low- to middle-income countries or low- to middle-income regions of more affluent countries. It is believed that 50% of individuals with diabetes are undiagnosed, and those that are diagnosed have been found to have diabetes for many years prior to their diagnosis. 6,7 million deaths have been attributed to diabetes, although the article did not mention the timeframe that involved that number. Diabetes accounts for 9% of total health care costs for adults, and the complications of foot and lower extremity issues related to diabetes affects 40 to 60 million people worldwide. The prevalence of neuropathy in one study was found to be anywhere from 10 to 85 percent, and the discrepancies found in the various studies were attributed to different definitions of when a diagnosis of neuropathy is made, which caused that huge variable in the prevalence study.
Another startling finding is that less than 33% of physicians surveyed will recognise the signs of a neuropathy when they're evaluating their patient. The lifetime risk of an individual developing a diabetic foot ulcer after they have diabetes is anywhere from 19 to 34 percent. Or put another way, one in four people with diabetes will develop a diabetic foot ulcer at some point in time. A person with diabetes who develops a diabetic foot ulcer is at 2,5 times greater risk of mortality than a person with diabetes who doesn't develop a diabetic foot ulcer. To put that more seriously, a person with a diabetic foot ulcer has a 5% mortality rate within one year. Their mortality rate increases to 42% within 5 years of developing a diabetic foot ulcer. After 5 years of a minor amputation, the mortality rate is 46%. And with a major amputation, after 5 years, the mortality rate increases to 57%. After 1 year, 20% of diabetic foot ulcers remain unhealed. And the recurrence rate after they do heal is 40% within one year and 65% within five years, which is a huge problem for diabetic patients. Once they have a foot ulcer, their risk of developing another one is significantly high.
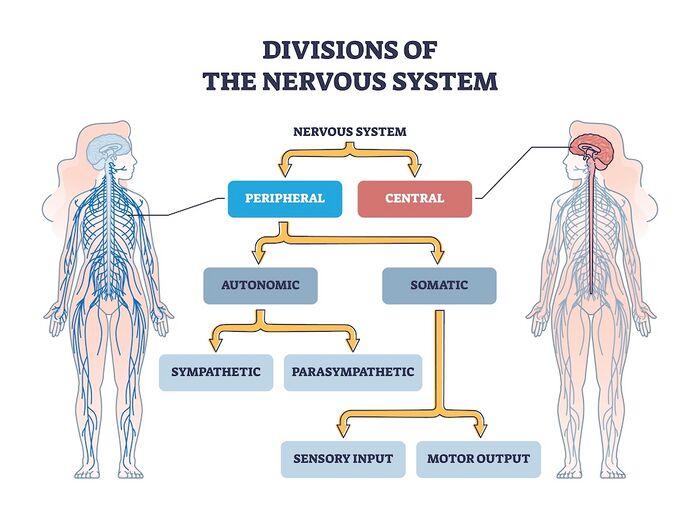
Neuroanatomy Review[edit | edit source]
- Central Nervous System: includes the brain and spinal cord. The central nervous system (CNS) is the body's processing centre. In general terms, the three functions of the CNS are to (1) take in sensory information, (2) process that information, and (3) send out motor signals. Through these mechanisms, the CNS controls most of the body's functions, to include: movement, sensation through our five senses, and higher level functions such as cognition, awareness, and speech. The spinal cord is an extension of the brain and serves as a neural pathway for information exchange with the rest of the body.
- Peripheral Nervous System: a complex network of nerves which convey sensory information in from the body to the CNS via the spinal cord, and transmit information out from the CNS via the spinal cord to the body. Examples of outgoing signals transmitted along the peripheral nervous system (PNS) include (1) motor information for muscle activity and(2) autonomic functioning (heart rate, blood pressure, respiration, digestion, sexual arousal)[1].
- Motor Nerves: relay information to skeletal muscles and somatic tissue, which creates voluntary movement
- Sensory Nerves: conveys sensory information about the environment in from sensory receptors in the body to the CNS
- Autonomic Nervous System: relay motor information to the visceral organs to innervate smooth muscle, cardiac muscle, and glands and functions to maintain the body's homeostasis. The autonomic nervous system has two parts: the sympathetic and parasympathetic divisions which innervate visceral organs. The sympathetic stimulates ("fight or flight") while the parasympathetic inhibits ("rest and digest") their functions.
Peripheral Neuropathy[edit | edit source]
Peripheral neuropathy (PN) describes the many conditions which involve damage to the peripheral nervous system. Initially, that presents as nerve malfunction due to cellular and chemical changes. Eventually, that malfunction becomes true nerve or structural damage, resulting in atrophy and demyelination[2]. There are more than 100 known types of peripheral neuropathy, each with unique symptoms and prognosis. PN symptoms are dependent on the category of nerves involved, motor, sensory, or autonomic[1].
The exact pathophysiology of PN is contingent upon the underlying disease processes, however the mechanisms of peripheral nerve injury exhibit similar patterns. These reactions include (1) segmental demyelination, (2) Wallerian degeneration, and (3) axonal degeneration[3].
Classification methods of PN include:
- Categorisation as mono-neuropathies, multifocal neuropathies, poly-neuropathies and radiculopathies[4][3].
- Further sub-classification by separating PN as axonal, demyelinating, or mixed[3].
Common symptoms of PN include:
To learn more about neuropathy, please read this optional article.
Aetiology of Peripheral Neuropathies[edit | edit source]
The National Institute of Health (NIH) states that PN aetiology can involve many courses, to include metabolic, systemic, and toxic causes[3]:
- Diabetes mellitus[2][3]
- Chronic alcoholism[2][3]
- Nutritional deficiencies (e.g., B1, B6, B12, and vitamin E)[2][3]
- Inflammatory conditions (e.g., vasculitis)[3]
- Hypothyroidism[2][3]
- Autoimmune disorders (e.g., Sjogren's syndrome[2], lupus, rheumatoid arthritis)[3]
- Infections (e.g., Lyme disease[2], Epstein-Barr virus, hepatitis C, shingles, leprosy, HIV)[3]
- Guillain-Barre syndrome[3]
- Toxins (heavy metals, chemicals such as mercury, lead, and arsenic)[3]
- Chemotherapy agents[2][3]
- Medications (antibiotics, cardiovascular medications)[3]
- Tumors (secondary to compression or associated paraneoplastic syndromes)[3]
- Inherited conditions (e.g., Charcot-Marie-Tooth disease, amyloidosis)[3]
- Trauma/injury (e.g., carpel tunnel syndrome)[3]
- Multiple myeloma and its treatments[3]
- Monoclonal gammopathy of undetermined significance (MGUS)[3][5]
- Idiopathic, when no direction cause can be identified[2]
General Categories of Peripheral Neuropathies[edit | edit source]
Sensory Neuropathy[edit | edit source]
One of them is damage to the sensory nerves, and that presents as loss of protective sensation or LOPS. There is also gait imbalance and ataxia. And when you combine the sensory neuropathy with a motor neuropathy that I'll discuss in a moment, that gait and ataxia issue become even more severe.
The injuries that you will see as a result of the loss of protective sensation are pretty much in three general categories. One is due to constant, prolonged pressure. Something like wearing shoes that are too tight. The pressure of the shoe against the skin over a bony prominence causes loss of blood flow to that area of skin, and that skin will eventually necrose. One of the theories for patients who wear shoes that are too tight is that they buy those shoes because that's what they feel when they put them on their foot. Because they don't have normal sensation, they don't feel the shoe that fits correctly, so they buy one that's too small because now they know that they have a shoe on because of the way they feel it. So that is one of the issues that needs a lot of education for patients with diabetes.
The second mechanism of injury that you might see related to loss of protective sensation is due to repetitive moderate to high pressure, which sets up a cycle of tissue damage, inflammation in response to that tissue damage, which causes more tissue damage, which causes more inflammation. And it's this cyclical process that goes on unchecked until it is identified and can be dealt with. The most common example of this is a callus that develops on the bottom of the foot. I'm not sure exactly what starts the callus. It could be some kind of irritation in the shoe. It could be a bony prominence that's adding pressure in a specific area. But once that callus starts, it results in a pressure from the bulk of the callus plus the sheer force as the person is walking and pushing off around that callus, which eventually leads to tissue breakdown and ultimately a wound. Having a callus on the bottom of the foot is like walking on a rock. And because they don't feel it, they continue to walk on it. That constant shearing and pressure causes that cycle of inflammation and eventually tissue breakdown, which can lead to a wound.
Calluses can become very large before a person realises that they have it on the bottom of their foot. It can also be caused by walking with something in the shoe like a rock without knowing it and causing a callus or an irritation and eventually a wound from that as well. And bony prominences will do the same thing just because of that high pressure and the shearing force of the skin over that bony prominence causing that cycle of inflammation and tissue damage. All of those are kind of related and can cause that callus to continue to grow until it is identified and can be responded to.
The third injury that you'll see related to loss of protective sensation is that brief high pressure injury like stepping on a sharp object. There's an immediate penetration and oftentimes the patient doesn't recognise that they've stepped on something because they don't have sensation in their foot and so then it becomes embedded in their foot and remains in their foot. And many times the patient will come in saying, "I noticed blood on my sock or some kind of drainage on my sock." Didn't realise they had a wound until it had started to become infected and started draining and bleeding.
Sometimes we've found needles in patients' foot wounds. In this example, they stepped on a piece of glass. They actually knew that they had been around glass. So when they had this discoloured area on their foot, they reported that there might be glass and they were taken to surgery and that piece of glass was found in their wound. But all of these can be related to damage directly because of loss of protective sensation.
Motor Neuropathy[edit | edit source]
The second type of neuropathy is the motor neuropathy or damage to the motor nerves. This affects the intrinsic muscles first as they become weaker due to the damage to the motor nerves and eventually the extrinsic muscles can be affected as well. Because of the imbalance of one muscle group to their opposing muscle group, multiple deformities can develop including hammer toe, claw toe, pes equinus. It can also result in tendon shortening, specifically the Achilles and the flexor hallucis tendons because of that weakness and the change in the gait pattern that develops. There's other causes of that tendon tightening as well.
Another sign of motor neuropathy is loss of reflexes, which can be an early sign that a motor neuropathy has developed, but unless you know what their baseline reflexes were, that's difficult to use in guiding the diagnosis of a motor neuropathy. The injuries that you will see that are directly related to the motor neuropathy are primarily changes in the foot structure because of that muscle imbalance, changes in the arch where you have a really high arch or maybe a flat foot, hyperextension or contraction of the metatarsophalangeal joints or the interphalangeal joints of the toes which can become malpositioned and cause toe deformities.
There are other injuries that are related to the combination of the motor and the sensory neuropathies. Because of the changes in the foot structure and the lack of sensation to recognise that things have changed, you get abnormal foot loading during gait and many gait imbalances, which can lead to all kinds of injuries from tripping, bumping into things, all kinds of issues related to just gait abnormalities. You also get abnormal pressures on the weight-bearing surface of the foot from the changes in the foot structure from the bony deformities and the inflexible foot. Our foot normally is used to accommodating to changes in the surface that we're walking on or changes in the shoe that we're wearing and it kind of can accommodate to the different pressures. And when you have a person who has deformities that put abnormal pressures in areas that aren't used to sustaining those pressures, and you can't feel them and you don't have the flexibility to accommodate to some of those changes, the constant repetition of walking causes that repetitive trauma and pressure to areas that can't sustain that pressure for long and eventually a wound will develop. In addition, the hyperkeratosis that causes increased thickening of the skin and callus causes additional pressure and eventually can lead to wounds.
Autonomic Neuropathy[edit | edit source]
The third neuropathy that can develop related to diabetes is the autonomic neuropathy. It's often not talked about as much, but it has some significant ramifications to the skin and physiology of the foot as well. An autonomic neuropathy causes dry skin or anhidrosis and hair loss. It also is the main cause of the medial arterial stenosis that develops in the arteries of the foot. The medial lining of the foot becomes calcified, directly related to the effect of diabetes on the circulation, and that stiffens those arteries so they can't respond to environmental changes as they should.
There's also systemic changes related to the autonomic neuropathy that can affect the gastrointestinal system, the cardiac system, the urogenital system. One of the most common ways that that's recognised is when someone has a silent heart attack. Because they don't have sensation, they don't recognise that their heart muscle is being damaged from an ischaemic event. They don't recognise their heart attack, and it can go untreated. In many cases, that's fatal because they don't get the treatment that they need. Injuries that you might see due to the autonomic neuropathy are things like, because of a sweating dysfunction, you can get really wet skin, which can create problems or more often really dry skin because of lack of sweating, and that can cause the skin to start to crack and fissure and lead to dermal openings where that wound can then develop an infection.
Another autonomic neuropathy effect is the increased glycation of keratin, which causes that really thickened, taut, inflexible skin on the foot. Because the skin is so taut and not flexible, there is an additional pressure against the bony prominences, which can cause an ischaemic ulcer to develop over those areas. There's also the decreased vasodilatory response, as I talked about, due to that medial calcinosis of the arteries in the foot.
Sub Heading 3[edit | edit source]
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 National Institute of Health. Peripheral Neuropathy. Available from: https://www.ninds.nih.gov/health-information/disorders/peripheral-neuropathy#toc-what-is-peripheral-neuropathy- (accessed 3/August/2023).
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Merwarth, D. Understanding the Foot Programme. Introduction to Foot Neuropathy. Physioplus. 2023.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 Hammi C, Yeung B. Neuropathy. 2022 Available from;https://www.ncbi.nlm.nih.gov/books/NBK542220/(last accessed 5/August/2023)
- ↑ Martyn CN, Hughes R. Epidemiology of peripheral neuropathy. Journal of neurology, neurosurgery, and psychiatry. 1997 Apr;62(4):310.
- ↑ Rögnvaldsson S, Steingrímsson V, Turesson I, Björkholm M, Landgren O, Kristinsson SY. Peripheral neuropathy and monoclonal gammopathy of undetermined significance: a population-based study including 15,351 cases and 58,619 matched controls. haematologica. 2020 Nov 11;105(11):2679.