Functional Anatomy of the Foot: Difference between revisions
No edit summary |
No edit summary |
||
| Line 7: | Line 7: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
Human feet allow bipedal locomotion <ref>Farris DJ, Kelly LA, Cresswell AG, Lichtwark GA. [https://www.pnas.org/doi/epdf/10.1073/pnas.1812820116 The functional importance of human foot muscles for bipedal locomotion]. PNAS 2019; 116(5).</ref>, and they are an essential sensory structure for postural control.<ref>Viseux FJF. The sensory role of the sole of the foot: Review and update on clinical perspectives. Neurophysiol Clin. 2020 Feb;50(1):55-68.</ref> The foot structure is complex, with many bones, joints and | Human feet allow bipedal locomotion <ref>Farris DJ, Kelly LA, Cresswell AG, Lichtwark GA. [https://www.pnas.org/doi/epdf/10.1073/pnas.1812820116 The functional importance of human foot muscles for bipedal locomotion]. PNAS 2019; 116(5).</ref>, and they are an essential sensory structure for postural control.<ref>Viseux FJF. The sensory role of the sole of the foot: Review and update on clinical perspectives. Neurophysiol Clin. 2020 Feb;50(1):55-68.</ref> The foot structure is complex, with many bones, joints, ligaments and muscles that divide the foot into a rearfoot, midfoot, and forefoot. Clinicians’ ability to understand the anatomical structures of the foot is a crucial component of their examination and treatment intervention, especially when treating clients with musculoskeletal conditions. <ref>Lee SW, Le PU, Van Dien C, Hansen M, Tiu T. Evaluation of Resident Palpation Skills in Foot and Ankle Anatomic Structures Using Bedside Ultrasound. HCA Healthcare Journal of Medicine 2020; 1(3).</ref> <ref>Kitagawa T, Aoki Y, Sugimoto H, Ozaki N. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8786950/pdf/41598_2022_Article_5290.pdf Randomised controlled trial for evaluation of an ultrasound-guided palpation intervention for palpation skill training.] Sci Rep. 2022 Jan 24;12(1):1189.</ref> This article discusses the foot assessment's elements, including key anatomical structures. | ||
== Anatomy Basic Vocabulary == | == Anatomy Basic Vocabulary == | ||
| Line 318: | Line 318: | ||
Dorsal: Abduction of the lateral four digits & flexion at the metatarsophalangeal joints. | Dorsal: Abduction of the lateral four digits & flexion at the metatarsophalangeal joints. | ||
|} | |||
[[File:Tibial.jpg|thumb]] | |||
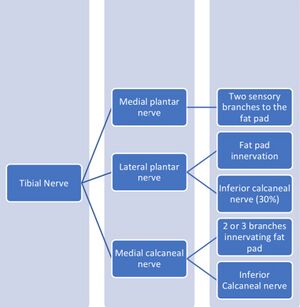
== Innervation of the Foot == | |||
=== Plantar Nerve === | |||
The plantar nerve originates from the [[Tibial Nerve|tibial nerve]] at the medial malleolus. The nerve divides into two branches: medial and lateral. It provides motor and sensory innervation to the foot muscles. | |||
* [[Medial Plantar Nerve|Medial plantar nerve]] | |||
** ''Motor fibres:'' abductor hallucis, flexor digitorum brevis, and flexor hallucis brevis muscles''.'' | |||
** ''Sensory fibres'': sole innervation, 1st, 2nd and 3rd toes, often 4th toe. | |||
* [[Lateral Plantar Nerve|Lateral plantar nerve]] | |||
** ''Motor fibres'': abductor and flexor digiti minimi, the adductor hallucis, and the interossei muscles. | |||
** ''Sensory fibres'': sole innervation, 5th toe, occasionally 4th toe. | |||
=== Sural Nerve === | |||
The [[Sural Nerve|sural nerve]] originates from the tibial nerve and cutaneous branches of the common fibular nerve. It is divided into the sural communication nerve and lateral sural cutaneous nerve. | |||
* ''Sensory fibres:'' posterior aspect of the distal leg and lateral aspect of the foot. | |||
== Vascular Supply of the Foot == | |||
Blood supply to the foot comes primary from the anterior and posterior tibial arteries, and the terminal branches of the popliteal artery.<ref>Attinger CE, Evans KK, Bulan E, Blume P, Cooper P. [https://www.inova.org/sites/default/files/education/podiatric_residency/Attinger_Angiosomes_of_the_foot_and_ankle_and_clinical_implications_for_limb_salvage_reconst.pdf Angiosomes of the foot and ankle and clinical implications for limb salvage: reconstruction, incisions, and revascularization.] Plast Reconstr Surg. 2006 Jun;117(7 Suppl):261S-293S.</ref> | |||
{| class="wikitable" | |||
|+ | |||
!Artery | |||
!Origin | |||
!Branches | |||
!Supply | |||
|- | |||
|Posterior tibial artery | |||
|Popliteal artery | |||
|Posterior compartment of the leg→inferior to the medial malleolus→tubercle of calcaneus→'''lateral and medial plantar arteries''' | |||
|Muscles of sole of foot | |||
|- | |||
|Anterior tibial artery | |||
|Terminal branch of the popliteal artery | |||
|Popliteal fossa→lower border of the popliteus muscle→posterior compartment of the leg→between heads of the posterior tibialis muscle→proximal part of the interosseous membrane→medial to the fibular neck→anterior compartment of the leg→anterior aspect of the interosseous membrane →anterior surface of the tibia→'''dorsalis pedis artery''' | |||
|Dorsal side of the foot | |||
|- | |||
|Medial plantar artery (MPA)& Lateral plantar artery (LPA) | |||
|Posterior tibial artery | |||
|Plantar arch extending from the 1st to the 5th metatarsal | |||
|MPA supplies abductor hallucis muscle and flexor digitorum brevis muscle | |||
LPA supplies plantar aponeurosis between flexor digitorum brevis and abductor digiti minimi muscles | |||
|- | |||
|Sural artery | |||
|Popliteal artery | |||
|Lateral and medial brunch | |||
|Supplies plantaris muscle | |||
|} | |} | ||
| Line 333: | Line 384: | ||
== Resources == | == Resources == | ||
* | *Golanó P, Vega J, de Leeuw PA, Malagelada F, Manzanares MC, Götzens V, van Dijk CN. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2855022/pdf/167_2010_Article_1100.pdf Anatomy of the ankle ligaments: a pictorial essay]. Knee Surg Sports Traumatol Arthrosc. 2010 May;18(5):557-69. | ||
== References == | == References == | ||
<references /> | <references /> | ||
Revision as of 02:22, 31 March 2023
Original Editor - User Name
Top Contributors - Ewa Jaraczewska and Jess Bell
Introduction[edit | edit source]
Human feet allow bipedal locomotion [1], and they are an essential sensory structure for postural control.[2] The foot structure is complex, with many bones, joints, ligaments and muscles that divide the foot into a rearfoot, midfoot, and forefoot. Clinicians’ ability to understand the anatomical structures of the foot is a crucial component of their examination and treatment intervention, especially when treating clients with musculoskeletal conditions. [3] [4] This article discusses the foot assessment's elements, including key anatomical structures.
Anatomy Basic Vocabulary[edit | edit source]
Axes: lines around which an object rotates. The rotation axis is a line that passes through the centre of mass. There are three axes of rotation: saggital passing from posterior to anterior, frontal passing from left to right, and vertical passing from inferior to superior. The rotation axes of foot joints are perpendicular to the cardinal planes therefore motions at these joints result in rotations within three planes. Example: supination involves inversion, internal rotation, and plantar flexion.
Bursae: reduces friction between the moving parts of the body joints. It is a fluid-filled sac. There are four types of bursae: adventitious, subcutaneous, synovial, and sub-muscular.
Capsule: one of the characteristics of the synovial joints. It is a fibrous connective tissue which forms a band that seals the joint space, provides passive and active stability and may even form articular surfaces for the joint.[5]
Closed pack position: most of the area of joint contact between the two sides of the joint. In this position, joint stability increases. The closed pack position for interphalangeal joints is at full extension.
Degrees of freedom: the direction of joint movement or rotation, with six being a maximum, including three translations and three rotations.
Ligament: fibrous connective tissue that holds the bones together.
Open (loose) pack position: least amount of joint contact area where joint stability is reduced.
Planes of movement: describe how the body moves. Up and down movements (flexion/extension) occur in a saggital plane. Sideway movements (abduction/adduction) are done in the frontal plane. Movements in the transverse plane are rotational (internal and external rotation).
Foot Structure[edit | edit source]
The anatomical structure of the foot consists of the hindfoot, midfoot and forefoot. Each part of the foot is composed of several bones.
Bones of the Foot[edit | edit source]
The talus and calcaneus form the foot's posterior aspect, called the hindfoot. The midfoot (located between the hindfoot and forefoot) is made up of five tarsal bones: the navicular, cuboid, and medial, intermediate, and lateral cuneiforms. The most anterior aspect of the foot, including the metatarsals, phalanges, and sesamoid bones, is called the forefoot. Each digit, except for the great toe, consists of a metatarsal and three phalanges. The great toe has only two phalanges.
Foot Articulations[edit | edit source]
The hindfoot has a talus and calcaneus articulation called the subtalar joint (ST, also known as the talocalcaneal joint [TC]). Three facets of the talus and the calcaneus are part of this joint. The main motions are inversion and eversion of the ankle and hindfoot.
The talonavicular and calcaneocuboid joints are known as Chopart's joint (MT, midtarsal or transverse tarsal joint), which is located between the hindfoot and midfoot. This joint allows forefoot rotation. The navicular articulates with all three cuneiform bones distally. In addition to the navicular and cuneiform bones, the cuboid bone has a distal articulation with the base of the fourth and fifth metatarsal bones.
The tarsometatarsal joint (TMT or Lisfranc's joint) connects the midfoot with the forefoot and originates from the lateral, intermediate and medial cuneiforms articulating with the bases of the three metatarsal bone (1st, 2nd, and 3rd). The small movement that occurs in the joint is described as dorsal and plantarflexion. The bases of the remaining metatarsal bones (4th and 5th) connect with the cuboid bone.
The five rays, metatarsal and corresponding phalanges create the forefoot medial and lateral columns where rays 1,2, and 3 belong to the middle column, and rays 4 and 5 to the lateral column. The metatarsophalangeal joints (MTP joints) are the main components of the forefoot. Each toe, except for the great toe, has proximal and distal interphalangeal joints (IP joints). The latter has only one IP joint.
Below is a summary of the foot articulations and kinematics:
| Joint | Type of Joint | Plane of Movement | Motion | Kinematics | Closed pack position | Open pack position |
|---|---|---|---|---|---|---|
| ST joint | Condyloid |
Mainly transverse |
Inversion & Eversion |
The average ROM:
30 degrees inversion / 18 degrees eversion[6] |
Full inversion | Inversion/plantarflexion |
| MT joint (Chopart's joint) |
TN joint - Ball and socket CC joint - Modified saddle |
Largely in transverse Some sagittal |
Inversion & Eversion Dorsiflexion & Plantarflexion [7] Abduction & Adduction[8] |
Inversion: approximately 8 to 10 degrees
Eversion: between 2 and 3 degrees. |
TN: Full supination
CC: Full supination |
Midway between extreme range of motion of a total range of motion |
| TMT joint (Lisfranc's joint) | Plane synovial | Saggital | Dorsiflexion & Plantarflexion | The mean ROM ranges from 22.4 to 33.5°.
MTP 5 through 2 show increasing values. [9] |
Full supination | Midway between supination and pronation |
| MTP joint | Condyloid |
Sagittal Some Transverse |
Dorsiflexion & Plantarflexion Abduction & Adduction |
Only the first and fifth metatarsal bones have a range of motion.
First MTP joint: maximum dorsiflexion from 17 to 62 degrees[10]. The adduction ranges from 6 to 11 degrees. |
1st MTP:
Hyperextension 2nd to 5th MTP: Maximum flexion |
Slight (10 degrees) extension |
| IP joint | Hinge | Sagittal | Flexion & Extension | First IP joint:
70 degrees of extension and 45 degrees of flexion |
Full extension | Slight flexion |
Arches of the Foot[edit | edit source]
The role of the foot arches are the following:
- Support and protect the foot
- Redistribute pressure during dynamic loading
- Alter the foot flexibility and rigidity
Lateral longitudinal arch: formed by the calcaneus, cuboid and the lateral two metatarsal bones
Medial longitudinal arch: formed by the calcaneus, talus, navicular, three cuneiforms and the medial three metatarsal bones
Transverse arch: runs across the tarsometatarsal joints
Foot Bursae[edit | edit source]
Bursae can be found in multiple locations at the foot: at the metatarsophalangeal joints, the base of the fifth metatarsal, and the back of the heel near the insertion of the Achilles tendon. Read more about the bursae pathology here and here.
Ligaments of the Foot[edit | edit source]
The main function of the short and long plantar ligaments and the calcaneonavicular ligament (spring ligament) is to assist in the passive maintenance of the arch.
| Ligament | Origin | Insertion | Characteristic | Action/Role |
|---|---|---|---|---|
| Plantar Fascia | Medial calcaneal tubercle | Five metatarsal bones | Extremely strong ligament | Primary passive plantar tissue that supports the medial longitudinal arch
Absorbs the impact of the ground reaction force in running or jumping Maintains and stores energy in the foot Disperses stress throughout the metatarsus |
| Plantar calcaneonavicular ligament
(SL, Spring ligament) Superomedial (SM) Lateral CN (LCN) Intermedial CN (ICN) |
Anterior sustentaculum tali | Navicular
(merges with a portion of superficial deltoid ligament) |
The strongest medial ligament | The passive stabiliser of the plantar arch in the talocalcaneal joint
Assists with preventing talus medial rotation and plantar flexion Limits navicular dorsiflexion, eversion, and abduction |
| Calcaneocuboid ligament (CC):
Medial CC (MCC) Dorsolateral CC (DLCC) Plantar CC (PCC)
|
DLCC:distal dorsolateral surface of the anterior process of the calcaneus
PCC: anterior tubercle of calcaneus |
DLCC: proximal lateral surface of the cuboid bone
PCC: the plantar surface of the cuboid posterior to the groove for the fibularis longus tendon |
Supports the medial and lateral longitudinal arches
Stabiliser of the calcaneocuboid joint and the midtarsal joint. | |
| Lisfranc ligament | Lateral side of the medial cuneiform bone | Medial side of the base of the second metatarsal bone | Maintains the stability of the medial column and axial column of the foot arch |
Muscles of the Foot[edit | edit source]
The dorsal muscles of the foot include: extensor digitorum brevis, extensor hallucis brevis
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Extensor Digitorum brevis | Calcaneus &
inferior extensor retinaculum |
Long extensor tendons of the medial four toes | Deep fibular nerve | Extension of the toes 2-5 |
| Extensor Hallucis brevis | Calcaneus &
inferior extensor retinaculum |
Base of the proximal phalanx of the great toe | Deep fibular nerve | Extension of the 1st toe |
The plantar muscles of the foot lie within the central compartment between the muscles of the big and little toe and they form the central surface of the foot sole:
- 1st layer: abductor hallucis, flexor digitorum brevis, abductor digiti minimi
- 2nd layer: quadratus plantae, lumbricals
- 3rd layer: flexor hallucis brevis, adductor hallucis, flexor digiti minimi brevis
- 4th layer: plantar and dorsal interossei
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Abductor hallucis | Medial tubercle of the calcaneus,
the flexor retinaculum & the plantar aponeurosis |
Medial base of the proximal phalanx of the 1st toe | Medial plantar nerve (S2,S3) | Abduction & flexion of the 1st toe |
| Flexor digitorum brevis | Medial tubercle of the calcaneus & the plantar aponeurosis | Middle phalanges of the digits 2-5 | Medial plantar nerve (S2,S3) | Flexion of the toes 2-5 at the proximal interphalangeal joints (PIP) |
| Abductor digiti minimi | Medial and lateral tubercles of the calcaneus & the plantar aponeurosis | Lateral base of the proximal phalanx of the 5th digit | Lateral plantar nerve (S1-S3) | Abduction & flexion of the 5th toe |
| Quadratus plantae | Calcaneus | Tendon of the flexor digitorum longus | Lateral plantar nerve (S1-S3) | Flexion of the toes 2-5, together with flexor digitorum longus |
| Lumbricals | Tendon of the flexor digitorum longus | Medial proximal phalanx &dorsal expansion of the extensor digitorum longus | Lumbrical 1: Medial plantar nerve (S2, S3);
Lumbricals 2-4: Lateral plantar nerve (S2-S3) |
Flexion at the metatarsophalangeal joints & extension at the interphalangeal joints |
| Flexor hallucis brevis | Lateral head – plantar surfaces of the cuboid &lateral cuneiforms
Medial head – posterior tibialis tendon. |
The base of the proximal phalanx of the 1st toe. | Medial plantar nerve (S2,S3) | Flexion of the 1st toe at the metatarsophalangeal joint |
| Adductor hallucis | Oblique head – the bases of the 2nd, 3rd, and 4th metatarsals.
Transverse head – the plantar ligaments of the metatarsophalangeal joints. |
lateral aspect of the base of the proximal phalanx of the 1st toe. | Deep branch of lateral plantar nerve | Adduction of the 1st toe
Supports the transverse arch of the foot |
| Flexor digiti minimi brevis | Base of the fifth metatarsal | Base of the proximal phalanx of the fifth digit. | Superficial branch of lateral plantar nerve | Flexion of the 5th toe at the metatarsophalangeal joint. |
| Plantar and dorsal interossei | Plantar: medial side of metatarsals 3-5
Dorsal:lateral aspect of the metatarsals |
Plantar:medial sides of the phalanges of digits 3-5
Dorsal: medial side of the proximal phalanx of the second digit &lateral sides of the proximal phalanxes of digits 2-4 |
Lateral plantar nerve | Plantar: Adduction of the lateral three digits & flexion at the metatarsophalangeal joints
Dorsal: Abduction of the lateral four digits & flexion at the metatarsophalangeal joints. |
Innervation of the Foot[edit | edit source]
Plantar Nerve[edit | edit source]
The plantar nerve originates from the tibial nerve at the medial malleolus. The nerve divides into two branches: medial and lateral. It provides motor and sensory innervation to the foot muscles.
- Medial plantar nerve
- Motor fibres: abductor hallucis, flexor digitorum brevis, and flexor hallucis brevis muscles.
- Sensory fibres: sole innervation, 1st, 2nd and 3rd toes, often 4th toe.
- Lateral plantar nerve
- Motor fibres: abductor and flexor digiti minimi, the adductor hallucis, and the interossei muscles.
- Sensory fibres: sole innervation, 5th toe, occasionally 4th toe.
Sural Nerve[edit | edit source]
The sural nerve originates from the tibial nerve and cutaneous branches of the common fibular nerve. It is divided into the sural communication nerve and lateral sural cutaneous nerve.
- Sensory fibres: posterior aspect of the distal leg and lateral aspect of the foot.
Vascular Supply of the Foot[edit | edit source]
Blood supply to the foot comes primary from the anterior and posterior tibial arteries, and the terminal branches of the popliteal artery.[11]
| Artery | Origin | Branches | Supply |
|---|---|---|---|
| Posterior tibial artery | Popliteal artery | Posterior compartment of the leg→inferior to the medial malleolus→tubercle of calcaneus→lateral and medial plantar arteries | Muscles of sole of foot |
| Anterior tibial artery | Terminal branch of the popliteal artery | Popliteal fossa→lower border of the popliteus muscle→posterior compartment of the leg→between heads of the posterior tibialis muscle→proximal part of the interosseous membrane→medial to the fibular neck→anterior compartment of the leg→anterior aspect of the interosseous membrane →anterior surface of the tibia→dorsalis pedis artery | Dorsal side of the foot |
| Medial plantar artery (MPA)& Lateral plantar artery (LPA) | Posterior tibial artery | Plantar arch extending from the 1st to the 5th metatarsal | MPA supplies abductor hallucis muscle and flexor digitorum brevis muscle
LPA supplies plantar aponeurosis between flexor digitorum brevis and abductor digiti minimi muscles |
| Sural artery | Popliteal artery | Lateral and medial brunch | Supplies plantaris muscle |
Clinical Relevance[edit | edit source]
- Knee varus leads to a greater peak hindfoot eversion[12], and increases foot rigidity. [13]
- Dysfunction of plantar fascia affects the height and shape of the medial longitudinal arch.[14]
- Pes planus may be produced by isolated spring ligament injuries.[15]
- Calcaneocuboid ligament can be damaged during inversion injury of the foot.[16]
- The transtarsal joint achieves its stability through the bony shape, ligament tightness and extrinsic muscles crossing the foot as there are no intrinsic muscles attaching to the talus or calcaneus and inserting to the cuboid or navicular bones. This may be the cause of this joint's frequent hypermobility.[17]
- The transtarsal joint achieves its stability through the bony shape, ligament tightness and extrinsic muscles crossing the foot as there are no intrinsic muscles attaching to the talus or calcaneus and inserting to the cuboid or navicular bones. This may be the cause of this joint's frequent hypermobility.[17]
- Hammer and claw toe deformities can be prevented with strong action of the interossei and lumbricals.
- Increased tissue stiffness in gastrocnemius and hamstrings muscles can lead to plantar fasciitis, and calf muscle stretching can be the solution for the problem.[18]
- Acute or chronic tears in the plantar fascia can be diagnosed by palpation of the painful lump on the sole of the foot.[19]
Resources[edit | edit source]
- Golanó P, Vega J, de Leeuw PA, Malagelada F, Manzanares MC, Götzens V, van Dijk CN. Anatomy of the ankle ligaments: a pictorial essay. Knee Surg Sports Traumatol Arthrosc. 2010 May;18(5):557-69.
References[edit | edit source]
- ↑ Farris DJ, Kelly LA, Cresswell AG, Lichtwark GA. The functional importance of human foot muscles for bipedal locomotion. PNAS 2019; 116(5).
- ↑ Viseux FJF. The sensory role of the sole of the foot: Review and update on clinical perspectives. Neurophysiol Clin. 2020 Feb;50(1):55-68.
- ↑ Lee SW, Le PU, Van Dien C, Hansen M, Tiu T. Evaluation of Resident Palpation Skills in Foot and Ankle Anatomic Structures Using Bedside Ultrasound. HCA Healthcare Journal of Medicine 2020; 1(3).
- ↑ Kitagawa T, Aoki Y, Sugimoto H, Ozaki N. Randomised controlled trial for evaluation of an ultrasound-guided palpation intervention for palpation skill training. Sci Rep. 2022 Jan 24;12(1):1189.
- ↑ Ralphs JR, Benjamin M. The joint capsule: structure, composition, ageing and disease. J Anat. 1994 Jun;184 ( Pt 3)(Pt 3):503-9.
- ↑ Ball P, Johnson GR. Technique for the measurement of hindfoot inversion and eversion and its use to study a normal population. Clin Biomech (Bristol, Avon). 1996 Apr;11(3):165-169.
- ↑ A Salih, Demirbüken I. Chapter 23 - Ankle and foot complex. Editor(s): Salih Angin, Ibrahim Engin Şimşek. Comparative Kinesiology of the Human Body, Academic Press 2020: pp 411-439.
- ↑ Walter WR, Hirschmann A, Tafur M, Rosenberg ZS. Imaging of Chopart (Midtarsal) Joint Complex: Normal Anatomy and Posttraumatic Findings. AJR Am J Roentgenol. 2018 Aug;211(2):416-425.
- ↑ Oosterwaal M, Carbes S, Telfer S, Woodburn J, Tørholm S, Al-Munajjed AA, van Rhijn L, Meijer K. The Glasgow-Maastricht foot model, evaluation of a 26 segment kinematic model of the foot. J Foot Ankle Res. 2016 Jul 8;9:19.
- ↑ Allan JJ, McClelland JA, Munteanu SE, Buldt AK, Landorf KB, Roddy E, Auhl M, Menz HB. First metatarsophalangeal joint range of motion is associated with lower limb kinematics in individuals with first metatarsophalangeal joint osteoarthritis. J Foot Ankle Res. 2020 Jun 8;13(1):33.
- ↑ Attinger CE, Evans KK, Bulan E, Blume P, Cooper P. Angiosomes of the foot and ankle and clinical implications for limb salvage: reconstruction, incisions, and revascularization. Plast Reconstr Surg. 2006 Jun;117(7 Suppl):261S-293S.
- ↑ Barrios JA, Davis IS, Higginson JS, Royer TD. Lower extremity walking mechanics of young individuals with asymptomatic varus knee alignment. J Orthop Res. 2009 Nov;27(11):1414-9.
- ↑ Arnold J, Mackintosh S, Jones S, Thewlis D. Altered dynamic foot kinematics in people with medial knee osteoarthritis during walking: a cross-sectional study. Knee. 2014 Dec;21(6):1101-6.
- ↑ Peng Y, Wai-Chi Wong D, Wang Y, Lin-Wei Chen T, Zhang G, Yan F, Zhang M.Computational models of flatfoot with three-dimensional fascia and bulk soft tissue interaction for orthosis design. Medicine in Novel Technology and Devices,2021;9.
- ↑ Casado-Hernández I, Becerro-de-Bengoa-Vallejo R, Losa-Iglesias ME, Santiago-Nuño F, Mazoteras-Pardo V, López-López D, Rodríguez-Sanz D, Calvo-Lobo C. Association between anterior talofibular ligament injury and ankle tendon, ligament, and joint conditions revealed by magnetic resonance imaging. Quant Imaging Med Surg. 2021 Jan;11(1):84-94.
- ↑ Edama M, Takabayashi T, Yokota H. et al. Morphological characteristics of the plantar calcaneocuboid ligaments. J Foot Ankle Res 2021; 14 (3).
- ↑ 17.0 17.1 Hastings MK. Movement system syndromes of the foot and ankle. In:Sahrmann S and Associates. Movement system impairment syndromes of the extremities, cervical and thoracic spine St.Louis, MO (USA): Elsevier Mosby; 2011:p.439-482
- ↑ Wilke J, Schleip R, Yucesoy CA, Banzer W. Not merely a protective packing organ? A review of fascia and its force transmission capacity. Journal of Applied Physiology. 2018 Jan 1;124(1):234-44.
- ↑ Bourne M, Talkad A, Varacallo M. Anatomy, Bony Pelvis and Lower Limb, Foot Fascia. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2022.