Functional Anatomy of the Cervical Spine: Difference between revisions
No edit summary |
No edit summary |
||
| Line 4: | Line 4: | ||
== Introduction == | == Introduction == | ||
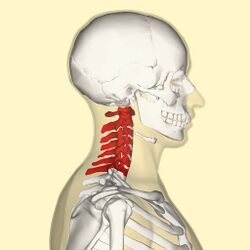
The cervical spine supports and promotes movement of the head and neck.<ref>Frost BA, Camarero-Espinosa S, Foster EJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6356370/ Materials for the spine: anatomy, problems, and solutions]. Materials. 2019 Jan;12(2):253</ref> <ref name=":0">Kaiser JT, Lugo-Pico JG. | The cervical spine supports and promotes movement of the head and neck.<ref>Frost BA, Camarero-Espinosa S, Foster EJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6356370/ Materials for the spine: anatomy, problems, and solutions]. Materials. 2019 Jan;12(2):253</ref> <ref name=":0">Kaiser JT, Reddy V, Lugo-Pico JG. Anatomy, Head and Neck: Cervical Vertebrae. [Updated 2022 Oct 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539734/</ref> Intervertebral discs maintain the spaces between the vertebrae. These discs act like shock absorbers throughout the spinal column to cushion the bones as the body moves. Ligaments hold the vertebrae in place, and tendons attach the muscles to the spinal column. The cervical spine is subjected to extrinsic factors such as repetitive movements, whole body vibrations and static load.<ref>Petersen JA, Brauer C, Thygesen LC, Flachs EM, Lund CB, Thomsen JF. [https://bmjopen.bmj.com/content/12/2/e053999 Prospective, population-based study of occupational movements and postures of the neck as risk factors for cervical disc herniation]. BMJ open. 2022 Feb 1;12(2):e053999.</ref>[[File:C-spine-picture.jpg|thumb|250x250px|Cervical spine]] | ||
== Key Terms == | == Key Terms == | ||
[[Cardinal Planes and Axes of Movement|Axes]]: lines around which an object rotates. The rotation axis is a line that passes through the centre of mass. There are three axes of rotation: ''sagittal'' passing from posterior to anterior, ''frontal'' passing from left to right, and ''vertical'' passing from inferior to superior. The rotation axes of the foot joints are perpendicular to the cardinal planes. Therefore, motion at these joints results in rotations within three planes. Example: supination involves inversion, internal rotation, and plantarflexion. | [[Cardinal Planes and Axes of Movement|Axes]]: lines around which an object rotates. The rotation axis is a line that passes through the centre of mass. There are three axes of rotation: ''sagittal'' passing from posterior to anterior, ''frontal'' passing from left to right, and ''vertical'' passing from inferior to superior. The rotation axes of the foot joints are perpendicular to the cardinal planes. Therefore, motion at these joints results in rotations within three planes. Example: supination involves inversion, internal rotation, and plantarflexion. | ||
| Line 12: | Line 12: | ||
[[Capsular and Non-Capsular Patterns|Capsule]]: one of the characteristics of the synovial joints. It is a fibrous connective tissue which forms a band that seals the joint space, provides passive and active stability and may even form articular surfaces for the joint. The capsular pattern is "the proportional motion restriction in range of motion during passive exercises due to tightness of the joint capsule." | [[Capsular and Non-Capsular Patterns|Capsule]]: one of the characteristics of the synovial joints. It is a fibrous connective tissue which forms a band that seals the joint space, provides passive and active stability and may even form articular surfaces for the joint. The capsular pattern is "the proportional motion restriction in range of motion during passive exercises due to tightness of the joint capsule." | ||
Closed pack position: the position with the most congruency of the joint surfaces. In this position, joint stability increases. For example, the closed pack position for the interphalangeal joints is | Closed pack position: the position with the most congruency of the joint surfaces. In this position, joint stability increases. For example, the closed pack position for the interphalangeal joints is full extension. | ||
Degrees of freedom: the direction of joint movement or rotation; there is a maximum of six degrees of freedom, including three translations and three rotations. | Degrees of freedom: the direction of joint movement or rotation; there is a maximum of six degrees of freedom, including three translations and three rotations. | ||
| Line 25: | Line 25: | ||
=== '''Cervical Vertebrae''' === | === '''Cervical Vertebrae''' === | ||
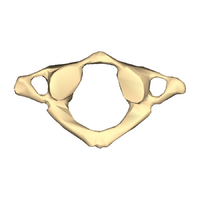
There are seven cervical vertebrae, which are known as C1-C7. There role is to support the head and neck and to promote head movement. The cervical spine is only subject to relatively small weight-bearing loads. Therefore, the cervical vertebral bodies do not need to be large and "an increased range of motion takes priority over vertebral size and rigidity".<ref name=":0" /> However, because of this increased range of motion at the cervical spine, there is heightened injury risk for the spinal cord and the associated neurovascular structures.<ref name=":0" />[[File:Cervical vertebra 1 close-up bottom (1).png|thumb|200x200px|Atlas - C1]]The seven vertebral bodies have unique characteristics:<ref name=":0" /><ref name=":1">Teach me anatomy The cervical Spine Available from:https://teachmeanatomy.info/neck/bones/cervical-spine/</ref> | |||
There are seven cervical vertebrae, which are known as C1-C7 | |||
[[Atlas]] (C1) | |||
[[Atlas]] | |||
* no vertebral body | * no vertebral body | ||
* no spinous process | * no spinous process | ||
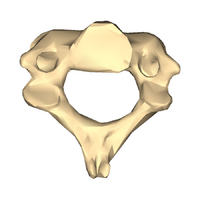
[[File:Cervical vertebra 2 close-up bottom.png|thumb|200x200px|Axis - C2]][[Axis]] (C2) | |||
* odontoid process (dens) extends superiorly from the anterior portion of the vertebra | |||
* odontoid process (dens) | |||
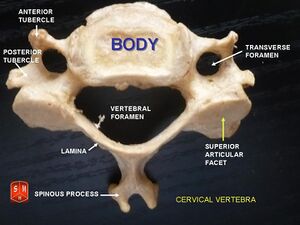
C3-C6 | C3-C6 | ||
* triangular vertebral foramen | * triangular vertebral foramen | ||
* bifed spinous process | * bifed spinous process | ||
* transverse foramina (space for nerves and vasculature)[[File:Cervical vertebrabifud.jpg|thumb|C3-C6 | * transverse foramina (space for nerves and vasculature)[[File:Cervical vertebrabifud.jpg|thumb|C3-C6]] | ||
C7 | C7 | ||
| Line 51: | Line 44: | ||
* larger spinous process | * larger spinous process | ||
< | <nowiki>**</nowiki>In supine, it may be difficult to palpate the spinous process of C3-C6 in individuals with normal cervical lordosis. | ||
< | == Intervertebral Discs (IVD) == | ||
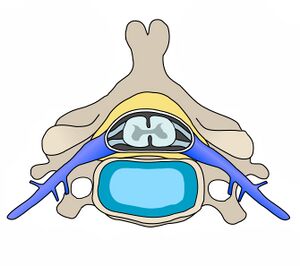
The intervertebral discs make up 25% of the height of the entire spine. However, in the cervical region, they make up 40% of the height. This increased height relative to vertebral body height provides a mobility advantage.<ref name=":2" /> | |||
The nucleus pulposus of the cervical discs is gelatinous in children and young people. However, it dries out by the age of 30 years and becomes a firm, fibrocartilaginous plate.<ref>Peng B, Bogduk N. [https://academic.oup.com/painmedicine/article/20/3/446/5232305?login=false Cervical discs as a source of neck pain. An analysis of the evidence.] Pain Medicine. 2019 Mar 1;20(3):446-55.</ref>[[File:Cervical Vertebra Unlabeled.jpg|thumb|Intervertebral disc]] | |||
The following are characteristics of the cervical spine intervertebral discs: | The following are characteristics of the cervical spine intervertebral discs: | ||
* thicker anteriorly than | * thicker anteriorly than posteriorly | ||
* concave superior surface | * concave superior surface | ||
* convex inferior surface | * convex inferior surface | ||
| Line 65: | Line 58: | ||
* anteroposterior translation does occur | * anteroposterior translation does occur | ||
<nowiki>**</nowiki> Due to location of uncinate process, posterolateral | <nowiki>**</nowiki> Due to location of uncinate process, posterolateral disc herniations are less frequent. | ||
=== Cervical Lordosis === | === Cervical Lordosis === | ||
Typically, the cervical spine has a lordotic curvature. A lordotic posture is able to resist large compressive loads. It also helps to decrease stress on vertebral end plates. Compressive loads are distributed differently in the cervical spine compared to the thoracic and lumbar spine: the anterior column absorbs 36% of the load and the posterior facet (zygapophyseal) joints absorb 64% of the load.<ref>Guo GM, Li J, Diao QX, Zhu TH, Song ZX, Guo YY, Gao YZ. [https://josr-online.biomedcentral.com/articles/10.1186/s13018-018-0854-6 Cervical lordosis in asymptomatic individuals: a meta-analysis. J]ournal of orthopaedic surgery and research. 2018 Dec;13(1):1-7.</ref> | |||
== Kinematics and Joints of the Cervical Spine == | == Kinematics and Joints of the Cervical Spine == | ||
=== Kinematics === | === Kinematics === | ||
[[File:Cervical spine exercises.png|thumb|Range of Motion in Cervical Spine]] | [[File:Cervical spine exercises.png|thumb|Range of Motion in Cervical Spine]] | ||
The most mobile part of the vertebral column is | The cervical spine is the most mobile part of the vertebral column. | ||
'''Flexion''' range of motion is usually around 40 degrees and extension is around 50 degrees. The largest contributors to flexion/extension are: | |||
* C4/C5 and C5/C6 in sitting | |||
* C6/C7 in supine | |||
C7/T1 contibutes the least to flexion/extension. | |||
Lateral flexion | '''Lateral flexion''' range of motion is normally close to 30 degrees. C3/C4 and C6/C7 allow for the most movement in this plane of motion. | ||
Cervical '''rotation''' range of motion is usually close to 70 degrees. Flexibility in this plane is mainly achieved through the C1/C2 segment.<ref>Lindenmann S, Tsagkaris C, Farshad M, Widmer J. [https://link.springer.com/article/10.1007/s10439-022-03088-8 Kinematics of the Cervical Spine Under Healthy and Degenerative Conditions: A Systematic Review]. Annals of Biomedical Engineering. 2022 Dec 10:1-29.</ref> | |||
{| class="wikitable" | {| class="wikitable" | ||
| Line 84: | Line 82: | ||
!'''<small>Joint</small>''' | !'''<small>Joint</small>''' | ||
!'''<small>Disc Joint</small>''' | !'''<small>Disc Joint</small>''' | ||
!'''<small>Facet | !'''<small>Facet (Zygapophyseal) Joints</small>''' | ||
!'''<small>Uncovertebral Joint</small>''' | !'''<small>Uncovertebral Joint</small>''' | ||
!'''<small>Atlanto-Axial Joint</small>''' | !'''<small>Atlanto-Axial Joint</small>''' | ||
!'''<small>Atlanto-Occipital Joint</small>''' | !'''<small>Atlanto-Occipital Joint</small>''' | ||
|- | |- | ||
!<small>Location/articulations</small> | |||
| | | | ||
* <small>between vertebral bodies</small> | * <small>between vertebral bodies</small> | ||
| Line 107: | Line 105: | ||
* <small>between superior facets of lateral masses of the atlas and the occipital condyles</small> | * <small>between superior facets of lateral masses of the atlas and the occipital condyles</small> | ||
|- | |- | ||
!<small>Functions</small> | |||
| | | | ||
# <small>bear weight</small> | # <small>bear weight</small> | ||
| Line 124: | Line 122: | ||
# <small>lateral flexion</small> | # <small>lateral flexion</small> | ||
|- | |- | ||
!<small>Orientation/Composition</small> | |||
| | | | ||
| | | | ||
Revision as of 12:52, 17 July 2023
Top Contributors - Robin Tacchetti, Jess Bell, Kim Jackson, Tarina van der Stockt, Vidya Acharya and Ewa Jaraczewska
Introduction[edit | edit source]
The cervical spine supports and promotes movement of the head and neck.[1] [2] Intervertebral discs maintain the spaces between the vertebrae. These discs act like shock absorbers throughout the spinal column to cushion the bones as the body moves. Ligaments hold the vertebrae in place, and tendons attach the muscles to the spinal column. The cervical spine is subjected to extrinsic factors such as repetitive movements, whole body vibrations and static load.[3]
Key Terms[edit | edit source]
Axes: lines around which an object rotates. The rotation axis is a line that passes through the centre of mass. There are three axes of rotation: sagittal passing from posterior to anterior, frontal passing from left to right, and vertical passing from inferior to superior. The rotation axes of the foot joints are perpendicular to the cardinal planes. Therefore, motion at these joints results in rotations within three planes. Example: supination involves inversion, internal rotation, and plantarflexion.
Bursae: reduce friction between the moving parts of the body joints. A bursa is a fluid-filled sac. There are four types of bursae: adventitious, subcutaneous, synovial, and sub-muscular.
Capsule: one of the characteristics of the synovial joints. It is a fibrous connective tissue which forms a band that seals the joint space, provides passive and active stability and may even form articular surfaces for the joint. The capsular pattern is "the proportional motion restriction in range of motion during passive exercises due to tightness of the joint capsule."
Closed pack position: the position with the most congruency of the joint surfaces. In this position, joint stability increases. For example, the closed pack position for the interphalangeal joints is full extension.
Degrees of freedom: the direction of joint movement or rotation; there is a maximum of six degrees of freedom, including three translations and three rotations.
Ligament: fibrous connective tissue that holds the bones together.
Open (loose) pack position: position with the least joint congruency where joint stability is reduced.
Planes of movement: describe how the body moves. Up and down movements (flexion/extension) occur in the sagittal plane. Sideway movements (abduction/adduction) occur in the frontal plane. The transverse plane movements are rotational (internal and external rotation).
Cervical Spine Structure[edit | edit source]
Cervical Vertebrae[edit | edit source]
There are seven cervical vertebrae, which are known as C1-C7. There role is to support the head and neck and to promote head movement. The cervical spine is only subject to relatively small weight-bearing loads. Therefore, the cervical vertebral bodies do not need to be large and "an increased range of motion takes priority over vertebral size and rigidity".[2] However, because of this increased range of motion at the cervical spine, there is heightened injury risk for the spinal cord and the associated neurovascular structures.[2]
The seven vertebral bodies have unique characteristics:[2][4]
Atlas (C1)
- no vertebral body
- no spinous process
Axis (C2)
- odontoid process (dens) extends superiorly from the anterior portion of the vertebra
C3-C6
- triangular vertebral foramen
- bifed spinous process
- transverse foramina (space for nerves and vasculature)
C7
- singular spinous process
- larger spinous process
**In supine, it may be difficult to palpate the spinous process of C3-C6 in individuals with normal cervical lordosis.
Intervertebral Discs (IVD)[edit | edit source]
The intervertebral discs make up 25% of the height of the entire spine. However, in the cervical region, they make up 40% of the height. This increased height relative to vertebral body height provides a mobility advantage.[5]
The nucleus pulposus of the cervical discs is gelatinous in children and young people. However, it dries out by the age of 30 years and becomes a firm, fibrocartilaginous plate.[6]
The following are characteristics of the cervical spine intervertebral discs:
- thicker anteriorly than posteriorly
- concave superior surface
- convex inferior surface
- movement limited by uncinate process
- anteroposterior translation does occur
** Due to location of uncinate process, posterolateral disc herniations are less frequent.
Cervical Lordosis[edit | edit source]
Typically, the cervical spine has a lordotic curvature. A lordotic posture is able to resist large compressive loads. It also helps to decrease stress on vertebral end plates. Compressive loads are distributed differently in the cervical spine compared to the thoracic and lumbar spine: the anterior column absorbs 36% of the load and the posterior facet (zygapophyseal) joints absorb 64% of the load.[7]
Kinematics and Joints of the Cervical Spine[edit | edit source]
Kinematics[edit | edit source]
The cervical spine is the most mobile part of the vertebral column.
Flexion range of motion is usually around 40 degrees and extension is around 50 degrees. The largest contributors to flexion/extension are:
- C4/C5 and C5/C6 in sitting
- C6/C7 in supine
C7/T1 contibutes the least to flexion/extension.
Lateral flexion range of motion is normally close to 30 degrees. C3/C4 and C6/C7 allow for the most movement in this plane of motion.
Cervical rotation range of motion is usually close to 70 degrees. Flexibility in this plane is mainly achieved through the C1/C2 segment.[8]
| Joint | Disc Joint | Facet (Zygapophyseal) Joints | Uncovertebral Joint | Atlanto-Axial Joint | Atlanto-Occipital Joint |
|---|---|---|---|---|---|
| Location/articulations |
|
|
|
|
|
| Functions |
|
|
|
|
|
| Orientation/Composition |
|
|
|
Spinal Ligaments[edit | edit source]
| Ligament | Origin | Insertion | Role/Function |
|---|---|---|---|
| Nuchal ligament | occiput | tips of the spinous process from C1-C7 | limit hyperflexion |
| Transverse ligament | connects lateral masses of atlas | anchors dens in place | |
| Apical ligament | dens of the axis | foramen magnum | stabilises skull on spiine |
| Lar Ligament | dens of the axis | occiput | limits atlanto-axial rotation |
| Cruciform or Cruciate Ligament
1. superior longitudinal band 2. inferior longitudinal band 3. transverse band |
|
|
hold dens in place |
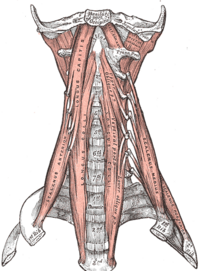
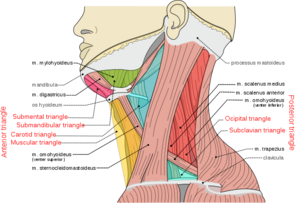
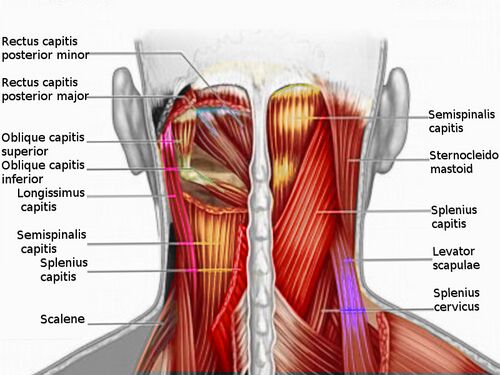
Muscles of the Cervical Spine[edit | edit source]
Muscles of the cervical spine can be divided by location or by the movement they create.
Anterior (Prevertebral) Vertebral Muscles[edit | edit source]
These are also termed Deep cervical flexor:
- Rectus Capitis Anterior
- Rectus Capitis Lateralis
- Longus capitis
- Longus colli/ Longus cervicis (3 portions: superior oblique, inferior oblique, vertical)
Lateral Vertebral Muscles[edit | edit source]
Scalenes - anterior, middle, posterior and minimus scalene muscles
Posterior Vertebral Muscles[edit | edit source]
These can be further divided into intrinsic and extrinsic muscles.
Extrinsic muscles[edit | edit source]
Trapezius and Levator scapulae
Intrinsic muscles[edit | edit source]
- Superficial muscles :
- Deep muscles:
- Suboccipital group -
- Transversospinalis muscles -
- semispinalis capitis
- semispinalis cervicis
- rotatores cervicis
- multifidus (these are also known as deep neck extensors)
- Interspinales and intertransversarii
Movement[edit | edit source]
| Motion | Flexion | Extension | Lateral Flexion | Rotation |
|---|---|---|---|---|
| Muscles |
|
|
Cervical Spine Flexors[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Rectus capitis anterior | Lateral mass and transverse process of atlas (C1) | Basilar part of occipital bone | Anterior rami of 1st and 2nd cervical spinal nerves (C1 - C2) | Flexion of head at atlanto-occipital joint |
| Longus colli | transverse processes of C3 to C5 and the vertebral bodies of C5 to T3 | anterior tubercle of C1, the vertebral bodies of C2 to 4, and the transverse processes of C5 and C6. | Anterior rami of 2nd to 6th cervical spinal nerves (C2 - C6) | Unilateral contractions - neck lateral flexion (ipsilateral), neck rotation (contralateral)
Bilateral contractions - neck flexion |
| Longus capitis | transverse processes of C3 to C6 | occipital bone | Anterior rami of 1st to 3rd cervical spinal nerves (C1 - C3) | Unilateral contractions - rotation of head (ipsilateral)
Bilateral contractions - flexion of head and neck |
| Anterior scalene | transverse processes of C3 to C6 | first rib | Anterior rami of 4th to 6th cervical spinal nerves (C4 - C6) | Unilateral contractions - neck lateral flexion (ipsilateral), neck rotation (contralateral), elevation of first rib
Bilateral contractions - neck flexion |
| Sternocleidomastoid | manubrium and the medial portion of the clavicle | mastoid process of the temporal bone | Accessory nerve (CN XI), branches of cervical plexus (C2 - C3) | Unilateral contractions - neck ipsilateral flexion, elevation of chin, head contralateral rotation
Bilateral contractions - extension of upper vertebral joints, extension of neck and head, elevation of head, elevation of sternum and clavicle, expansion of thoracic cavity |
| Rectus capitis lateralis | Transverse process of atlas (C1) | Jugular process of occipital bone | Anterior rami of 1st and 2nd cervical spinal nerves (C1 - C2) | Lateral flexion of head (ipsilateral), stabilization of atlanto-occipital joint |
Cervical Spine Extensors[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Obliques capitis superior | transverse process of the atlas | occipital bone | Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1)) | stabilises atlanto-occipital joint |
| Oblique capitis inferior | spinous process of the axis and inserts into the transverse process of the atlas, | tansverse process of atlas | Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1)) | stabilises atlanto-occipital joint |
| Rectus capitis posterior major | spinous process of C2 | occipital bone | Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1)) | Unilateral contractions - head rotation (ipsilateral)
Bilateral contractions - head extension |
| Rectus capitis posterior minor | posterior tubercle of the atlas | occipital bone | Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1)) | head extension |
| Iliocostal cervicis | ribs 3-6 | transverse process of C4-C6 | dorsal rami of the upper thoracic and lower cervical spinal nerves. | Laterally flexes and extends the lower cervical region |
| Trapezius | occipital bone, nuchal ligament and spinous process C7-T12 | lateral third of clavicle, the acromian and the spine of s scapula |
|
supporting the spinal column to remain erect |
| Spelnius cervicis | spinous process T3-T6 | transverse process of C1C3 | Dorsal rami of cervical spinal nerves (C5, 6, 7, and 8) | Bilaterally they extend the neck |
| Splenius capitus | spinous process C7-T3 and nuchal ligament | occipital bone | posterior rami of the 2nd and 3rd cervical spinal nerves. | Acting bilaterally: extension of the head and cervical spine |
** The transversospinal muscles (rotatores, multifidus, semispinalis) are the deep muscle layers in the spine. They attach between the transverse and spinous process of the vertebrae. They stabilise and extend the spine. The rotatores also provide rotation.
Cervical Spine Lateral Flexors[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Splenius cervicis | spinous process T3-T6 | transverse process C1-C3 | Dorsal rami of cervical spinal nerves (C5,6,7 and 8) | unilaterally they laterally flex and rotate the head and neck to the ipsilateral (same) side |
| Splenius capitis | spinous process C7-T3 and nuchal ligament | occipital bone | posterior rami of the 2nd and 3rd cervical spinal nerves | Acting unilaterally: lateral flexion of the head and neck and rotation the head to the same side |
| Sternocleidomastoid | manubrium and the medial portion of the clavicle | mastoid process of the temporal bone | Accessory nerve (CN XI), branches of cervical plexus (C2 - C3) | Unilateral contractions - neckpper vertebral joints, extension of neck and head, elevation of head, elevation of sternum and clavicle, expansion of thoracic cah cervical spinal nerves (C4 - C6) |
| Middle scalene | posterior tubercles of the transverse processes of C2-C7 | scalene tubercle of the first rib. | Anterior rami of C3-C8. | Elevation of the first rib. Ipsilateral contraction causes ipsilateral lateral flexion of the neck |
| Posterior scalene | posterior tubercles of the transverse processes of C5-C7 | 2nd rib | Anterior rami of C6-C8 | Elevation of the second rib, and ipsilateral lateral flexion of the neck |
| Trapezius | occipital bone, nuchal ligament and spinous process C7-T12 | lateral third of clavicle, the acromian and the spine of s scapula |
|
side bending |
| Rectus capitis lateralis | Superior surface of the transverse process of atlas | Inferior surface of the jugular process of the occipital bone | Anterior rami of C1-C2 spinal nerves | Stabilizes the atlanto-occipital joint; head lateral flexion (ipsilateral) |
Cervical Spine Rotators[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Rectus capitis posterior major | spinous process of C2 | occipital bone | Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1)) | Unilateral contractions - head rotation (ipsilateral)
Bilateral contractions - head extension |
| Rectus capitis posterior major | spinous process of C2 | occipital bone | Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1)) | Unilateral contractions - head rotation (ipsilateral)
Bilateral contractions - head extension |
| Sternocleidomastoid | manubrium and the medial portion of the clavicle | mastoid process of the temporal bone | Accessory nerve (CN XI), branches of cervical plexus (C2 - C3) | Unilateral contractions - neck ipsilateral flexion, elevation of chin, head contralateral rotation
Bilateral contractions - extension of upper vertebral joints, extension of neck and head, elevation of head, elevation of sternum and clavicle, expansion of thoracic cah cervical spinal nerves (C4 - C6) |
| Splenius capitis | spinous process C7-T3 and nuchal ligament | occipital bone | posterior rami of the 2nd and 3rd cervical spinal nerves | Acting unilaterally: lateral flexion of the head and neck and rotation the head to the same side |
| Splenius cervicis | spinous process T3-T6 | transverse process C1-C3 | Dorsal rami of cervical spinal nerves (C5,6,7 and 8) | unilaterally they laterally flex and rotate the head and neck to the ipsilateral (same) side |
Innervation of the Cervical Spine[edit | edit source]
Nerves originating from the cervical plexus innervate the muscles of the neck. Each nerve root in the cervical spine exits above its corresponding nerve root. There are eight pairs of cervical nerves despite the presence of seven cervical vertebrae. The C8 nerve root exits below the seventh cervical vertebrae. The accessory nerve which is cranial nerve X1 innervates the sternocleidomastoid as well as the trapezius. [2]
| Nerve | Motor | Sensory |
|---|---|---|
| C1 | head and neck extensor;
rectus capitus anterior and lateral longus capitus |
|
| C2 | head and neck extensor;
rectus capitus anterior and lateral, longus capitus, longus colli |
lateral occiput and submandibular area |
| C3 | head and neck extensors,
longus capitus, longus colli, levator scapulae, scaleni, and trapezius |
lateral occiput and lateral neck, overlapping C2 |
| C4 | head and neck extensors,
longus coli, levator scapulae, scaleni, trapezius, and diaphragm. |
lower lateral neck and medial shoulder area |
| C5 | deltoid, biceps, bicep tendon reflex | clavicle level and lateral arm |
| C6 | biceps, wrist extensors, brachioradialis tendon reflex | lateral forearm, thumb, index and half of 2nd finger |
| C7 | wrist flexors, triceps, triceps tendon reflex | second finger |
| C8 | finger flexors, interossei | medial forearm, ring and little finger |
| T1 | interossei | medial arm |
Vascular Supply of the Cervical Spine[edit | edit source]
Vertebral arteries, veins and nerves pass through the transverse foramina of the cervical vertebrae. C7 is the only exception in that the vertebral artery passes around the vertebra instead of through the transverse foramen.[4]The neural components sit posterior to the vertebral artery.[11]
The cervical spine vascular supply is primarily provided by the vertebral arteries one on each side. These arteries arise from the subclavian arteries that originate directly from the arch of the aorta on the right side, and via the brachiocephalic trunk on the left side.
** The common carotid arteries bifurcates into the internal and external carotid arteries at the C3 segmental level. Only the external carotid artery provides any blood supply to the neck.
Clinical Relevance[edit | edit source]
- Atlanto-axial instability (AAI) can cause serious neurological consequences:
- conditions with potential for AAI include:
- rheumatoid arthritis
- Down syndrome:
- Laxity in the transverse ligament is present in 14% to 22% of individuals with Down syndrome.
- conditions with potential for AAI include:
- Tight sternocleidomastoid muscle can cause torticollis.
- Disc herniation:
- disc herniations in the cervical spine are a lot less common than in the lumbar spine,
- typical locations:
- C5 to 6
- C6 to 7
- Prevertebral cervical muscles stabilise the neck.
- Dysfunction in these muscles can cause cervicogenic pain.
- Trigger point that develop in the suboccipital muscles can refer pain to the head causing cervicogenic headaches.[12]
Resources[edit | edit source]
References[edit | edit source]
- ↑ Frost BA, Camarero-Espinosa S, Foster EJ. Materials for the spine: anatomy, problems, and solutions. Materials. 2019 Jan;12(2):253
- ↑ 2.0 2.1 2.2 2.3 2.4 Kaiser JT, Reddy V, Lugo-Pico JG. Anatomy, Head and Neck: Cervical Vertebrae. [Updated 2022 Oct 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539734/
- ↑ Petersen JA, Brauer C, Thygesen LC, Flachs EM, Lund CB, Thomsen JF. Prospective, population-based study of occupational movements and postures of the neck as risk factors for cervical disc herniation. BMJ open. 2022 Feb 1;12(2):e053999.
- ↑ 4.0 4.1 Teach me anatomy The cervical Spine Available from:https://teachmeanatomy.info/neck/bones/cervical-spine/
- ↑ 5.0 5.1 Learn muscles . Cervical spine joints. Available from: https://learnmuscles.com/blog/2017/08/01/cervical-spinal-joints/ (last accessed 29.1.2020)
- ↑ Peng B, Bogduk N. Cervical discs as a source of neck pain. An analysis of the evidence. Pain Medicine. 2019 Mar 1;20(3):446-55.
- ↑ Guo GM, Li J, Diao QX, Zhu TH, Song ZX, Guo YY, Gao YZ. Cervical lordosis in asymptomatic individuals: a meta-analysis. Journal of orthopaedic surgery and research. 2018 Dec;13(1):1-7.
- ↑ Lindenmann S, Tsagkaris C, Farshad M, Widmer J. Kinematics of the Cervical Spine Under Healthy and Degenerative Conditions: A Systematic Review. Annals of Biomedical Engineering. 2022 Dec 10:1-29.
- ↑ RSNA Joints of Luschka Available from: https://pubs.rsna.org/doi/10.1148/66.2.181 (last accessed 28.1.2020)
- ↑ Palastanga, N., & Soames, R. (2012). Anatomy and human movement (6th ed.). Edinburgh: Churchill Livingstone.
- ↑ Joshi N, Klinger N, Halalmeh DR, Tubbs RS, Moisi MD. The Neural Sulcus of the Cervical Vertebrae: A Review of Its Anatomy and Surgical Perspectives. Cureus. 2020 Jan 18;12(1)
- ↑ Xuan, D. Exploring Clinical Anatomy. Plus. 2023