Fracture: Difference between revisions
No edit summary |
Abbey Wright (talk | contribs) (general edit) |
||
| Line 2: | Line 2: | ||
== Definition == | == Definition == | ||
A fracture is a discontinuity in a [[bone]] (or cartilage) resulting from mechanical forces that exceed the bone's ability to withstand them.<ref name=":0">Radiopedia [https://radiopaedia.org/articles/fracture-1 Fracture] Available from:https://radiopaedia.org/articles/fracture-1 (last accessed 2.4.2020)</ref> Fractures can occur in a variety of | A fracture is a discontinuity in a [[bone]] (or cartilage) resulting from mechanical forces that exceed the bone's ability to withstand them.<ref name=":0">Radiopedia [https://radiopaedia.org/articles/fracture-1 Fracture] Available from:https://radiopaedia.org/articles/fracture-1 (last accessed 2.4.2020)</ref> Fractures can occur in a variety of methods: | ||
* A normal bone subjected to acute overwhelming force, usually in the setting of trauma | * A normal bone subjected to acute overwhelming force, usually in the setting of trauma | ||
* Weakened bone from a focal lesion (e.g. metastasis, or bone cyst), known as pathological fractures. | * Weakened bone from a focal lesion (e.g. metastasis, or bone cyst), known as '''pathological fractures'''. | ||
* Weakened bone due to metabolic abnormalities (e.g. [[osteoporosis]]) or less frequently, genetic abnormalities (e.g. [[Osteogenesis Imperfecta|osteogenesis imperfecta]]). Resulting in [[Insufficiency Fracture|'''insufficiency fractures.''']] | |||
* Chronic application of abnormal stresses (e.g. running),resulting in '''microfractures''' and eventually, macroscopic failure (fatigue fractures). | |||
Together, insufficiency and fatigue fractures are often grouped together as '''stress fractures'''. | |||
== Location == | == Location == | ||
[[File:Bone_1.jpg|alt=|right|frameless]] | [[File:Bone_1.jpg|alt=|right|frameless]] | ||
'''Type of Bone Fractured''' | '''Type of Bone Fractured'''<ref name=":2">Bigham‐Sadegh A, Oryan A. [https://onlinelibrary.wiley.com/doi/full/10.1111/iwj.12231 Basic concepts regarding fracture healing and the current options and future directions in managing bone fractures.] International wound journal. 2015 Jun;12(3):238-47.</ref> | ||
* long bone (femur, tibia, fibula and humerus) | * long bone (femur, tibia, fibula and humerus) | ||
* short bone (carpal bones) | * short bone (carpal bones) | ||
* flat bone (scapulae, ribs) | * flat bone (scapulae, ribs) | ||
* Sesamoid bone | * [[Sesamoid|Sesamoid bone]] (patella) | ||
* Irregular bone (vertebrae and skull) | * Irregular bone (vertebrae and skull) | ||
<br>'''Part of Bone Fractured''' | <br>'''Part of Bone Fractured''' | ||
| Line 23: | Line 26: | ||
* Physis | * Physis | ||
* Metaphysis | * Metaphysis | ||
* Diaphysis | * Diaphysis | ||
* Specific Features within a bone (tubercle, epicondyle) | * Specific Features within a bone (tubercle, epicondyle) | ||
== Types of Bone Fracture == | == Types of Bone Fracture == | ||
[[File:Fractures.jpg|right|frameless|629x629px|Types of bone fracture.]]In general, there are many different classification systems used for fractures which fall within a set number of patterns | [[File:Fractures.jpg|right|frameless|629x629px|Types of bone fracture.]]In general, there are many different classification systems used for fractures which fall within a set number of patterns:<ref name=":2" /> | ||
*'''Complete:''' Extends all the way across the bone (most common) | *'''Complete:''' Extends all the way across the bone (most common) | ||
* '''Incomplete:''' does not cross the bone completely (usually encountered in children) | * '''Incomplete:''' does not cross the bone completely (usually encountered in children) | ||
| Line 46: | Line 49: | ||
* '''Greenstick Fracture:''' Fracture in a young, soft bone in which the bone bends and the cortex is broken, but only on one side<ref name=":0" /> | * '''Greenstick Fracture:''' Fracture in a young, soft bone in which the bone bends and the cortex is broken, but only on one side<ref name=":0" /> | ||
== Pathophysiology of Bone Healing == | == Pathophysiology of Bone Healing == | ||
The pathophysiological sequence of events that occur following a fracture for [[Bone Healing|bone healing]] can be divided into three main phases<ref>Bahney CS, Zondervan RL, Allison P, Theologis A, Ashley JW, Ahn J, Miclau T, Marcucio RS, Hankenson KD. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6542569/ Cellular biology of fracture healing]. Journal of Orthopaedic Research®. 2019 Jan;37(1):35-50.</ref><ref>Kostenuik P, Mirza FM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6120140/ Fracture healing physiology and the quest for therapies for delayed healing and nonunion]. Journal of Orthopaedic Research®. 2017 Feb;35(2):213-23.</ref> | The pathophysiological sequence of events that occur following a fracture for [[Bone Healing|bone healing]] can be divided into three main phases<ref name=":2" /><ref>Bahney CS, Zondervan RL, Allison P, Theologis A, Ashley JW, Ahn J, Miclau T, Marcucio RS, Hankenson KD. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6542569/ Cellular biology of fracture healing]. Journal of Orthopaedic Research®. 2019 Jan;37(1):35-50.</ref><ref>Kostenuik P, Mirza FM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6120140/ Fracture healing physiology and the quest for therapies for delayed healing and nonunion]. Journal of Orthopaedic Research®. 2017 Feb;35(2):213-23.</ref> | ||
# Inflammatory Phase | # Inflammatory Phase | ||
| Line 52: | Line 55: | ||
# Remodelling Phase | # Remodelling Phase | ||
=== Phase 1 - Inflammatory Phase (Hours - Days) === | === Phase 1 - Inflammatory Phase (Hours - Days) === | ||
Immediately at the time of fracture, the space between the ends of the fracture is filled with blood, forming a heamatoma. This prevents additional bleeding and provides structural and biochemical support for the influx of inflammatory cells. The inflammatory reaction results in the release of cytokines, growth factors and prostaglandins, all of which are important in healing. The fibroblasts, chondroblasts and the ingrowth of capillaries is then infiltrated by fibrovascular tissue. This forms a matrix for bone formation and primary callus. Phase 1 takes approximately a week, forming a primary callus which is non-mineralized. | Immediately at the time of fracture, the space between the ends of the fracture is filled with blood, forming a heamatoma. This prevents additional bleeding and provides structural and biochemical support for the influx of inflammatory cells. | ||
The inflammatory reaction results in the release of cytokines, growth factors and prostaglandins, all of which are important in healing. The fibroblasts, chondroblasts and the ingrowth of capillaries is then infiltrated by fibrovascular tissue. This forms a matrix for bone formation and primary callus. Phase 1 takes approximately a week, forming a primary callus which is non-mineralized.<ref name=":2" /> | |||
This is not readily visible on radiography. | This is not readily visible on radiography. | ||
=== Phase 2 - Reparative Phase (Days - Weeks) === | === Phase 2 - Reparative Phase (Days - Weeks) === | ||
Over the next few weeks, this primary callus is transformed into a bony callus by the activation of osteoprogenitor cells. These cells lay down woven bone which stabilises the fracture site. Soft callus is organised and remodelled into hard callus over several weeks. Soft callus is plastic and can easily deform or bend if the fracture is not adequately supported. Hard callus is weaker than normal bone but is better able to withstand external forces and equates to the stage of "clinical union", i.e. the fracture is not tender to palpate or with movement. | Over the next few weeks, this primary callus is transformed into a bony callus by the activation of osteoprogenitor cells. These cells lay down woven bone which stabilises the fracture site. <ref name=":2" /> | ||
Soft callus is organised and remodelled into hard callus over several weeks. Soft callus is plastic and can easily deform or bend if the fracture is not adequately supported. Hard callus is weaker than normal bone but is better able to withstand external forces and equates to the stage of "clinical union", i.e. the fracture is not tender to palpate or with movement. | |||
This can be seen on radiographs within 7-10 days after injury. | This can be seen on radiographs within 7-10 days after injury. | ||
=== Phase 3 - Remodelling Phase (Months to Years) === | === Phase 3 - Remodelling Phase (Months to Years) === | ||
The remodelling phase is longest phase and may last several years. This phase represents the gradual formation of compact cortical bone with greater biomechanical properties. This allows for the reduction of the width of the callus. During remodelling, the healed fracture and surrounding callus responds to activity, external forces, functional demands and growth. Bone (external callus) which is no longer needed is removed and the fracture site is smoothened and sculpted. Remodelling can result in almost perfect healing, however, where alignment of the fracture site is not perfect, a residual deformity may remain.<ref name=":0" /> | The remodelling phase is longest phase and may last several years. <ref name=":2" /> | ||
This phase represents the gradual formation of compact cortical bone with greater biomechanical properties. This allows for the reduction of the width of the callus. | |||
During remodelling, the healed fracture and surrounding callus responds to activity, external forces, functional demands and growth. Bone (external callus) which is no longer needed is removed and the fracture site is smoothened and sculpted. | |||
Remodelling can result in almost perfect healing, however, where alignment of the fracture site is not perfect, a residual deformity may remain.<ref name=":0" /> | |||
{{#ev:youtube|od8oU5OLMGU|300}}<ref>Whats Up Dude. How Does A Bone Break Heal - Bone Fracture Healing Process. Available from: http://www.youtube.com/watch?v=od8oU5OLMGU[last accessed 8/6/2020]</ref> | {{#ev:youtube|od8oU5OLMGU|300}}<ref>Whats Up Dude. How Does A Bone Break Heal - Bone Fracture Healing Process. Available from: http://www.youtube.com/watch?v=od8oU5OLMGU[last accessed 8/6/2020]</ref> | ||
== Complications == | == Complications == | ||
Many of the aforementioned fracture types can also go on to have additional complications (and many associated soft tissue injuries). See [[Fracture Complications]] | Many of the aforementioned fracture types can also go on to have additional complications (and many associated soft tissue injuries). See [[Fracture Complications]] | ||
* Acute [[Compartment Syndrome]] is common in | * Acute [[Compartment Syndrome]] is common in fractures of the forearm. | ||
* Fat embolism syndrome (a piece of fat that released into the blood vessels causing blockage of blood flow) <ref>Maitre S. [https://journalofethics.ama-assn.org/article/causes-clinical-manifestations-and-treatment-fat-embolism/2006-09 Causes, clinical manifestations, and treatment of fat embolism.] AMA Journal of Ethics. 2006 Sep 1;8(9):590-2.</ref> that is most commonly associated with long bone and pelvic fracture<ref>Hershey K. Fracture complications. Critical Care Nursing Clinics. 2013 Jun 1;25(2):321-31.</ref> | * Fat embolism syndrome (a piece of fat that released into the blood vessels causing blockage of blood flow) <ref>Maitre S. [https://journalofethics.ama-assn.org/article/causes-clinical-manifestations-and-treatment-fat-embolism/2006-09 Causes, clinical manifestations, and treatment of fat embolism.] AMA Journal of Ethics. 2006 Sep 1;8(9):590-2.</ref> that is most commonly associated with long bone and pelvic fracture<ref>Hershey K. Fracture complications. Critical Care Nursing Clinics. 2013 Jun 1;25(2):321-31.</ref> | ||
* [[Osteomyelitis]] of bone in response to infection. | * [[Osteomyelitis]] of bone in response to infection. | ||
| Line 73: | Line 86: | ||
* Fracture Blisters | * Fracture Blisters | ||
* Compound Fracture: extending through the skin | * Compound Fracture: extending through the skin | ||
* Joint Involvement: intracapsular, articular, dislocation<br> | * Joint Involvement: intracapsular, articular, dislocation. This can lead to [[osteoarthritis]] in the long term. <br> | ||
{{#ev:youtube|RKScXgsYXwk|300}}<ref>Jay Cheon. Complications of fractures. Available from: http://www.youtube.com/watch?v=RKScXgsYXwk[last accessed 8/6/2020]</ref> | {{#ev:youtube|RKScXgsYXwk|300}}<ref>Jay Cheon. Complications of fractures. Available from: http://www.youtube.com/watch?v=RKScXgsYXwk[last accessed 8/6/2020]</ref> | ||
== Clinical Features of Fracture == | == Clinical Features of Fracture == | ||
| Line 80: | Line 93: | ||
* [[Pain Mechanisms|Pain]] | * [[Pain Mechanisms|Pain]] | ||
* Deformity | * Deformity | ||
* Oedema | * [[Edema Assessment|Oedema]] | ||
* Loss of Function | * Loss of Function | ||
* Muscle Spasm | * Muscle Spasm | ||
Revision as of 16:00, 16 March 2022
Top Contributors - Esraa Mohamed Abdullzaher, Naomi O'Reilly, Kalyani Yajnanarayan, Lucinda hampton, Khloud Shreif, Kim Jackson, Claire Knott, Abbey Wright and Aminat Abolade
Definition[edit | edit source]
A fracture is a discontinuity in a bone (or cartilage) resulting from mechanical forces that exceed the bone's ability to withstand them.[1] Fractures can occur in a variety of methods:
- A normal bone subjected to acute overwhelming force, usually in the setting of trauma
- Weakened bone from a focal lesion (e.g. metastasis, or bone cyst), known as pathological fractures.
- Weakened bone due to metabolic abnormalities (e.g. osteoporosis) or less frequently, genetic abnormalities (e.g. osteogenesis imperfecta). Resulting in insufficiency fractures.
- Chronic application of abnormal stresses (e.g. running),resulting in microfractures and eventually, macroscopic failure (fatigue fractures).
Together, insufficiency and fatigue fractures are often grouped together as stress fractures.
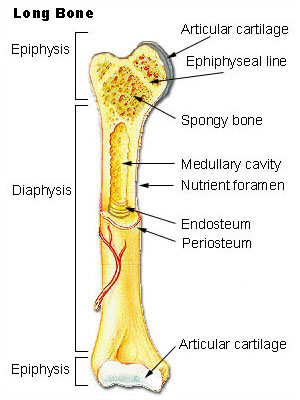
Location[edit | edit source]
Type of Bone Fractured[2]
- long bone (femur, tibia, fibula and humerus)
- short bone (carpal bones)
- flat bone (scapulae, ribs)
- Sesamoid bone (patella)
- Irregular bone (vertebrae and skull)
Part of Bone Fractured
- Epiphysis
- Physis
- Metaphysis
- Diaphysis
- Specific Features within a bone (tubercle, epicondyle)
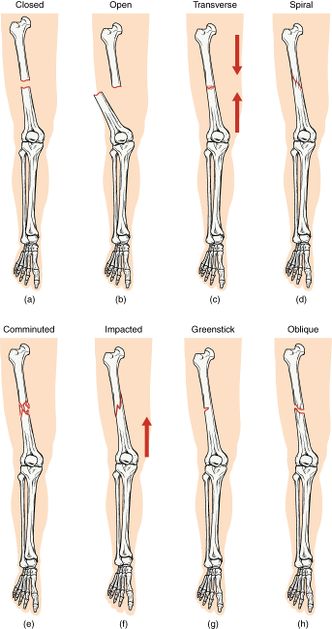
Types of Bone Fracture[edit | edit source]
In general, there are many different classification systems used for fractures which fall within a set number of patterns:[2]
- Complete: Extends all the way across the bone (most common)
- Incomplete: does not cross the bone completely (usually encountered in children)
- Non-Displaced / Stable: Fractured ends of the bone line up
- Displaced / Unstable: Fractured portions of bone are separated or misaligned.
- Closed / Simple: Bone has not pierced the skin
- Open / Compound: Skin has been pierced or punctured by the bone or by a blow that breaks the skin at the time of the fracture. The bone or may not be visible.
- Transverse: Fracture is in a straight line across or perpendicular to axis of bone
- Oblique: Fracture is orientated obliquely across the bone
- Spiral: Fracture spirals around the bone, or a helical fracture path usually in the diaphysis of long bones, common in twisting injuries.
- Stress: Small crack or severe bruising within a bone
- Comminuted: Fracture is in three or more pieces with fragments present at site
- Compression: Bone is crushed causing the fractured bone to be wider or flatter in appearance
- Segmental: Same bone is fractured in two places so there is ‘floating’ segment of bone
- Bowing: Incomplete fracture of long bone in infants/children due to forces in the axial load[3].
- Buckle Fracture: Due to direct axial load, the cortex is buckled, often in the distal radius
- Greenstick Fracture: Fracture in a young, soft bone in which the bone bends and the cortex is broken, but only on one side[1]
Pathophysiology of Bone Healing[edit | edit source]
The pathophysiological sequence of events that occur following a fracture for bone healing can be divided into three main phases[2][4][5]
- Inflammatory Phase
- Reparative Phase
- Remodelling Phase
Phase 1 - Inflammatory Phase (Hours - Days)[edit | edit source]
Immediately at the time of fracture, the space between the ends of the fracture is filled with blood, forming a heamatoma. This prevents additional bleeding and provides structural and biochemical support for the influx of inflammatory cells.
The inflammatory reaction results in the release of cytokines, growth factors and prostaglandins, all of which are important in healing. The fibroblasts, chondroblasts and the ingrowth of capillaries is then infiltrated by fibrovascular tissue. This forms a matrix for bone formation and primary callus. Phase 1 takes approximately a week, forming a primary callus which is non-mineralized.[2]
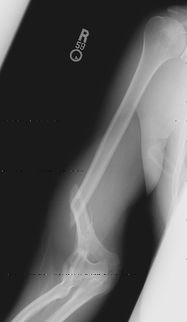
This is not readily visible on radiography.
Phase 2 - Reparative Phase (Days - Weeks)[edit | edit source]
Over the next few weeks, this primary callus is transformed into a bony callus by the activation of osteoprogenitor cells. These cells lay down woven bone which stabilises the fracture site. [2]
Soft callus is organised and remodelled into hard callus over several weeks. Soft callus is plastic and can easily deform or bend if the fracture is not adequately supported. Hard callus is weaker than normal bone but is better able to withstand external forces and equates to the stage of "clinical union", i.e. the fracture is not tender to palpate or with movement.
This can be seen on radiographs within 7-10 days after injury.
Phase 3 - Remodelling Phase (Months to Years)[edit | edit source]
The remodelling phase is longest phase and may last several years. [2]
This phase represents the gradual formation of compact cortical bone with greater biomechanical properties. This allows for the reduction of the width of the callus.
During remodelling, the healed fracture and surrounding callus responds to activity, external forces, functional demands and growth. Bone (external callus) which is no longer needed is removed and the fracture site is smoothened and sculpted.
Remodelling can result in almost perfect healing, however, where alignment of the fracture site is not perfect, a residual deformity may remain.[1]
Complications[edit | edit source]
Many of the aforementioned fracture types can also go on to have additional complications (and many associated soft tissue injuries). See Fracture Complications
- Acute Compartment Syndrome is common in fractures of the forearm.
- Fat embolism syndrome (a piece of fat that released into the blood vessels causing blockage of blood flow) [7] that is most commonly associated with long bone and pelvic fracture[8]
- Osteomyelitis of bone in response to infection.
- Healing complications: malunion, delayed union or non-union. [9]
- Avascular Necrosis
- Fracture Blisters
- Compound Fracture: extending through the skin
- Joint Involvement: intracapsular, articular, dislocation. This can lead to osteoarthritis in the long term.
Clinical Features of Fracture[edit | edit source]
Clinical features vary depending on the cause of injury, nature and the patients level of consciousness. These features are :
- Pain
- Deformity
- Oedema
- Loss of Function
- Muscle Spasm
- Muscle Atrophy
- Abnormal Movement
- Limitation in Joint Range of Motion
- Shock
When Is Fracture Healed[edit | edit source]
The average time for bone healing is about 6-8 weeks, but can varies depending upon many factors;
Local Factors
- The type of fracture, severity and extent of the misalignment of the fractured bone.
- Infections that can lead to delayed, poor, or non-union healing.
- The blood supply to the fractured bone.
- The type of fixation (cast, splint, ORIF procedure, etc).
Systemic Factors
- The age of the person (individuals with osteoporosis are predisposed to further healing complications).
- The nutritional status of the individual.
- Smoking (delayed healing)
- The treatment undergone.[11]
A fracture is considered to be clinically healed based upon the combination of physical findings and symptoms over time. The following suggest complete healing :
- Absence of pain on weight-bearing, lifting or movement
- No tenderness on palpation at the fracture site
- Blurring or disappearance of the fracture line on X-ray
- Full or near to full functional ability[12].
Treatment and Prognosis[edit | edit source]
The basics of fracture healing rely on alignment and immobilisation.
Alignment may or may not be necessary depending on the degree of displacement, the importance of correct alignment (e.g. index finger vs rib), and the patient (e.g. professional athlete vs debilitated elderly).
Immobilisation can be achieved in a variety of ways, depending on the location, morphology of the fracture, and device of fixation
- None (e.g. most rib fractures)
- Sling (e.g. many clavicular fractures)
- Cast (e.g. many forearm fractures)
- Internal fixation (e.g. most hip fractures)
- External fixation
Fixation Devices[edit | edit source]
Stress Sharing Devices[edit | edit source]
It allows micromotion between the two fractured sites and partial transmission of load. This promotes secondary bone healing with callus formation (a relatively rapid bone healing).
For example; intramedullary nail, casts, rods.
Stress Shielding Devices[edit | edit source]
The stress at the fracture site is transmitted through the shielding device therefore, there is no motion at the fracture site. This promotes primary bone healing without callus formation (slower than the healing with callus formation).
For example; compression plate[13][14].
Role of Physiotherapy[edit | edit source]
The physiotherapist’s role is to identify the root cause of the problem and select appropriate treatment techniques to help patient's return to their desired activities of daily living.
As with any physiotherapy session, conducting a patient assessment is crucial. The problem-oriented medical record (POMR) system is based on a data collection system that incorporates the acronym SOAP:
- Subjective – information given by the patient: allergies, past medical history, past surgical history, family history, social history (living arrangements, social conditions, employment, medication), review of systems .
- Objective – all information obtained through observation or testing, e.g. range of joint movement, muscle strength .
- Analysis – a listing of problems based on what you know from a review of subjective and objective data.
- Plan – this refers to the plan of treatment).
The treatment provided is largely dependent on the problems identified during your initial assessment. may include a mixture of the following:
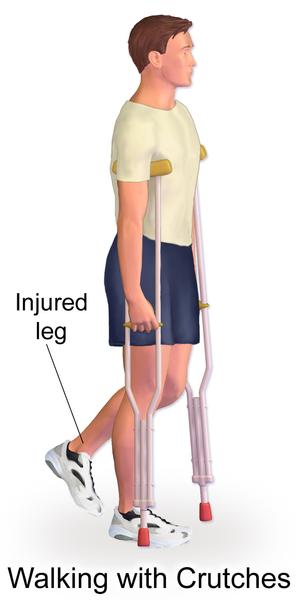
Examples of early treatment include;
- Education
- on ambulation with assistive devices during various tasks such as walking up and down stairs or to get in and out of a car. Consideration of the client's weightbearing restrictions are also crucial during these sessions, advising clients on ways to ambulate whilst adhering to the restrictions. Since safety is paramount, it's essential that client's are proficient and comfortable using these devices prior to discharge.
- on the application and removal of slings post upper extremity fractures.
- Soft tissue massage, particularly to manage oedema and swelling
- Scar management post surgery
- Ice therapy
- Stretching exercises to regain joint range of movement
- Joint manual therapy and mobilizations to assist in regaining joint mobility
- Structured and progressive strengthening regime
- Balance and control work and gait (walking) re-education where appropriate
- Taping to support the injured area/help with swelling management
- Return to sport preparatory work and advice where required[12]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Radiopedia Fracture Available from:https://radiopaedia.org/articles/fracture-1 (last accessed 2.4.2020)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Bigham‐Sadegh A, Oryan A. Basic concepts regarding fracture healing and the current options and future directions in managing bone fractures. International wound journal. 2015 Jun;12(3):238-47.
- ↑ https://radiologykey.com/types-of-fractures-in-children/
- ↑ Bahney CS, Zondervan RL, Allison P, Theologis A, Ashley JW, Ahn J, Miclau T, Marcucio RS, Hankenson KD. Cellular biology of fracture healing. Journal of Orthopaedic Research®. 2019 Jan;37(1):35-50.
- ↑ Kostenuik P, Mirza FM. Fracture healing physiology and the quest for therapies for delayed healing and nonunion. Journal of Orthopaedic Research®. 2017 Feb;35(2):213-23.
- ↑ Whats Up Dude. How Does A Bone Break Heal - Bone Fracture Healing Process. Available from: http://www.youtube.com/watch?v=od8oU5OLMGU[last accessed 8/6/2020]
- ↑ Maitre S. Causes, clinical manifestations, and treatment of fat embolism. AMA Journal of Ethics. 2006 Sep 1;8(9):590-2.
- ↑ Hershey K. Fracture complications. Critical Care Nursing Clinics. 2013 Jun 1;25(2):321-31.
- ↑ Jackson LC, Pacchiana PD. Common complications of fracture repair. Clinical techniques in small animal practice. 2004 Aug 1;19(3):168-79.
- ↑ Jay Cheon. Complications of fractures. Available from: http://www.youtube.com/watch?v=RKScXgsYXwk[last accessed 8/6/2020]
- ↑ Sheen JR, Garla VV. Fracture Healing Overview. InStatPearls [Internet] 2019 Nov 25. StatPearls Publishing.
- ↑ 12.0 12.1 Tidy's Physiotherapy Chapter 22 Churchill Livingstone Elsevier London 2013
- ↑ Burgoyne W. Treatment and rehabilitation of fractures. Edited by Stanley Hoppenfeld and Vasantha L. Murthy. Pp 574. Hagerstown, Maryland: Lippincott Williams & Wilkins, 2000. ISBN: 0-7817-2197-0. $69.95.
- ↑ http://chambalravine.blogspot.com/2013/07/biomechanical-principles-of-fracture.html