Facial Palsy
Original Editor - Wendy Walker.
Top Contributors - Wendy Walker, Jess Bell, Kim Jackson, Redisha Jakibanjar, Muhammad Umar, Vidya Acharya, Lucinda hampton, Admin, Evan Thomas, WikiSysop, Rishika Babburu, Naomi O'Reilly, Tarina van der Stockt, Darine Mohieldeen, Ahmed Essam and 127.0.0.1
One Page Owner - Wendy Walker as part of the One Page Project
Introduction[edit | edit source]
Facial palsy is caused by damage in the facial nerve that supplies the muscles of the face. It can be categorised into two types based on the location of casual pathology:
- Central facial palsy
- Due to damage above the facial nucleus
- Peripheral facial palsy
- Due to damage at or below the facial nucleus[1]
Clinically Relevant Anatomy[edit | edit source]
For more detail on the anatomy of the facial nerve, please see the Facial Nerve page.
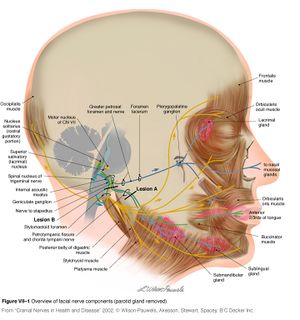
Cranial Nerve VII has its nucleus in the pons. It takes a rather winding route before exiting the skull through the stylomastoid foramen. It then passes through the parotid gland, splitting into 5 branches:
- Temporal
- Zygomatic
- Buccal
- Mandibular
- Cervical
Please click through to see videos on the Facial Muscles
Causes of Peripheral Facial Palsy[1][edit | edit source]
- Idiopathic or Bell's Palsy
- Tumour
- A tumour compressing the facial nerve can cause facial paralysis, but more commonly the facial nerve is damaged during surgical removal of a tumour
- The most common tumour to cause facial palsy during surgical removal is the acoustic neuroma (also known as vestibular schwannoma)
- Less common tumours to cause facial palsy (or the surgery to remove them) include cholesteatoma, hemangioma, facial schwannoma or parotid gland tumours
- Infection
- Ramsay Hunt syndrome - caused by Herpes Zoster infection
- A syndromic occurrence of facial paralysis, herpetiform vesicular eruptions, and vestibulocochlear dysfunction
- Patients presenting with Ramsay Hunt syndrome are generally at increased risk of hearing loss than patients with Bell's palsy, and the course of disease is more painful
- There is also a lower recovery rate from the facial palsy is observed in Ramsay Hunt syndrome patients[5][6]
- Lyme disease - caused by infection with Borrelia burgdorferi via tick bites
- 10 percent of patients affected with Lyme disease develop facial paralysis - 25 percent of these patients present with bilateral facial palsy[7]
- Ramsay Hunt syndrome - caused by Herpes Zoster infection
- Iatrogenic facial nerve damage
- Occurs most commonly in temporomandibular joint replacement, mastoidectomy, and parotidectomy[8]
- Congenital
- Rare causes, including:
- Neurosarcoidosis
- Otitis media
- Multiple sclerosis
- Moebius syndrome
- Melkersson-Rosenthal syndrome
- Guillain-Barre syndrome
- Millard-Gubler syndrome (AKA Ventral Pontine Syndrome) - an ipsilateral facial palsy with contralateral hemiplegia that involves the corticospinal tract and paralysis of lateral rectus on the ipsilateral side due to the involvement of the abducent nerve
- Foville Syndrome (AKA Inferior Medial Pontine Syndrome) - an ipsilateral facial palsy, contralateral hemiplegia with ipsilateral conjugate gaze effects
- Eight-and-a-half syndrome - facial palsy with internuclear ophthalmoplegia and horizontal gaze palsy
- Trauma - especially temporal and mastoid bone fractures
Risk factors[edit | edit source]
- Diabetes[9]
- Pregnancy - potentially due to hypercoagulability, increased blood pressure and fluid load, viral infections and suppressed immunity[10]
- Infection of ear
- Upper respiratory tract infection
- Obesity[1] [11][12]
Clinical Presentation[edit | edit source]
Paralysis of the muscles supplied by the facial nerve presents on the affected side of the face as follows:
Appearance and Range of Movement[edit | edit source]
- Inability to close the eye
- Inability to move the lips (e.g. into a smile, pucker)
- At rest, the affected side of the face may "droop"
- If, however, the person is in synkinesis, the affected side of the mouth may sit higher than the other side
- The lower eyelid may droop and turn outward, which is known as "ectropion"
Functional Effects[edit | edit source]
- Difficulty eating and drinking as the lack of lip seal makes it difficult to keep fluids and food in the oral cavity
- Reduced clarity of speech as the "labial consonents" (ie. b, p, m, v, f) all require lip seal
- Dryness of the affected eye - more information on this is available on the Dry Eye page
Somatic Effects[edit | edit source]
The facial nerve supplies the lachrymal glands of the eye, the saliva glands, and to the muscle of the stirrup bone in the middle ear (the stapes). It also transmits taste from the anterior two thirds of the tongue.
Facial palsy often involves:
- Lack of tear production in the affected eye, causing a dry eye, and the risk of corneal ulceration
- There are two factors which contribute to dry eye in facial nerve palsy:
- The greater petrosal nerve, derived from the facial nerve, supplies the parasympathetic autonomic component of the lacrimal gland - controlling the production of moisture / tearing in eyes
- The zygomatic branch of the facial nerve supplies orbicularis oculi, and the resulting paralysis causes inability (or reduced ability) to close the eye or blink, so the tears (or artificial lubrication in the form of drops, gel or ointment) are not spread across the cornea properly
- There are two factors which contribute to dry eye in facial nerve palsy:
- Hyperacusis - i.e. sensitivity to sudden loud noises
- Altered taste sensation
Bell's Phenomenon[edit | edit source]
Differential Diagnosis[edit | edit source]
Upper Motor Neuron versus Lower Motor Neuron[edit | edit source]
If the forehead is not affected (i.e. the patient is able to raise fully the eyebrow on the affected side) then the facial palsy is likely to be an upper motor neuron (UMN) lesion.[3] Paralysis which includes the forehead, such that the patient is unable to raise the affected eyebrow, is a lower motor neuron (LMN) lesion.
However, caution is advised in using preservation of forehead function to diagnose a central lesion. Patients may have sparing of forehead function with lesions in the pontine facial nerve nucleus, with selective lesions in the temporal bone, or with an injury to the nerve in its distribution in the face. It is worth remembering that a cortical lesion that produces a lower facial palsy / paresis is usually associated with a motor deficit of the tongue and weakness of the thumb, fingers, or hand on the ipsilateral side.[13]
Bell's Palsy versus Ramsey Hunt Syndrome[edit | edit source]
Diagnostic Procedures[edit | edit source]
- Laboratory investigations include an audiogram, nerve conduction studies (ENoG), computed tomography (CT) or magnetic resonance imaging (MRI), electromyography (EMG)[15][16]
- According to a clinical guideline, published in 2013, clinicians "should not obtain routine laboratory and imaging testing in patients with new-onset Bell’s palsy"[12]
Outcome Measures[17][edit | edit source]
- Sunnybrook Facial Grading System[18]
- Often preferred by physiotherapists because of its sensitivity and synkinesis section
- The regions of the face are evaluated separately, with the use of five standard expressions:
- Eyebrow raise
- Eye closure
- Open mouth smile
- Lip pucker
- Snarl / show teeth
- House-Brackmann facial nerve grading scale
- Synkinesis Assessment Questionnaire
- Linear Measurement Index
- Facial Disability Index
- Lip-length (LL) and Snout (S) Indices
- Five-Point Scale
Management / Interventions[edit | edit source]
Medical and surgical management depends on the cause of facial palsy.
Medical Management[edit | edit source]
The medical management of these conditions are discussed more in the linked pages, but Bell's palsy and Ramsay Hunt syndrome are treated with corticosteroids (prednisone), given within 72 hours of onset.[19][3] This can be accompanied by antiviral medication.[20][21][22]
Surgical Management[edit | edit source]
As discussed in the linked pages, tumours such as acoustic neuromas and facial schwannomas are frequently resected surgically. Patients at high risk of a corneal ulcer may be offered oculoplastic surgery to protect the eye.
For patients with dense facial palsy and no nerve function, a number of surgical interventions may be used. These fall into the following categories:
- Facial reanimation surgeries which involve nerve graft or anastomosis
- Facial reanimation surgeries which involve muscle transposition
- Static surgeries (i.e. plastic surgery) is used to improve symmetry at rest but does not improve movement
Physiotherapy[edit | edit source]
In the early stages of facial palsy, the most important thing to do is to check that the patient is caring for the affected eye in an appropriate way. As the facial nerve is responsible for production of lubrication to the cornea, the patient is highly likely to suffer from a dry eye in the early weeks and months of facial palsy. This puts them at risk of developing a corneal ulcer, which can cause vision damage in the affected eye.
The therapist should educate the patient about dry eye management if this has not been done by other medical personnel. If the eye is looking red or the patient reports frequent episodes of redness, an urgent referral to opthalmology is required. Alternatively they should be advised to attend an Eye Hospital Emergency Department. For more information on dry eye including presentation, risk of corneal ulcer and management such as taping / use of artificial lubrication, please click here.
Other physiotherapy treatments include:
- Neuromuscular retraining (NMR) [23][24]
- For more information on this concept please see the Neuromuscular Reeducation in Facial Palsy page
- Electromyography (EMG) and mirror biofeedback[1][25]
- Trophic electrical stimulation (TES)[26]
- Proprioceptive neuro muscular facilitation (PNF) techniques[11]
- Kabath technique[27]
- Mime therapy[28]
Evidence for Physiotherapy Treatments[edit | edit source]
- According to clinical practice guidelines, physiotherapy is recommended ("weak recommendation") in Bell's palsy,[12][29] and neuromuscular retraining techniques are effective in increasing facial range of movement and symmetry, as well as reducing / minimising synkinesis[23][30][31][32]
- Mime therapy can improve functionality for patients with facial palsy
- The effect of electrical stimulation is controversial[1][33][34]
- One study found that PNF technique is more effective than conventional exercises[11]
- One study found PNF / Kabat technique is more effective than no exercise[27]
Complications and Sequelae[edit | edit source]
Synkinesis (AKA aberrant regeneration) occurs after injury to the facial nerve. Synkinesis develops in cases of axonotmesis damage to the facial nerve and is, therefore, a normal sequelae to facial nerve damage.
Physiotherapy is extremely helpful in management of synkinesis - neuromuscular retraining techniques and mirror feedback exercises in particular are effective in reducing the problems associated with synkinesis.
Effects on Quality of Life[edit | edit source]
A large retrospective study of 920 patients from 2018 looked into the correlation between facial palsy severity and quality of life.[35] It concluded that: "A correlation between facial palsy severity and quality of life was found in a large cohort of patients comprising various etiologies. Additionally, novel factors that predict the quality of life in facial palsy were revealed".[35]
Resources[edit | edit source]
Charity for Facial Palsy from any cause
Bell's Palsy Association, Charity
Information web-site on Bell's Palsy
Here's a link to the Facebook group for Facialpalsy.org
This link is to an introductory video about the effects of facial palsy
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Zhao Y, Feng G, Gao Z. Advances in diagnosis and non-surgical treatment of Bell's palsy. Journal of otology. 2015;10(1):7-12.
- ↑ Peiterson,E. Bell's Palsy; the spontaneous course of 2,500 peripheral facial nerve palsies of different etiologies. Acta Oto-Laryngologica. Supplementum 2002;549:4-30.
- ↑ 3.0 3.1 3.2 Somasundara D, Sullivan F. Management of Bell's palsy. Australian prescriber.2017;40(3):94-7.
- ↑ Holland NJ, Weiner GM. Recent developments in Bell's Palsy. BMJ. 2004;329(7465):553-7.
- ↑ Hah YM, Kim SH, Jung J, Kim SS, Byun JY, Park MS et al. Prognostic value of the blink reflex test in Bell's palsy and Ramsay-Hunt syndrome. Auris Nasus Larynx. 2018;45(5):966-70.
- ↑ Cai Z1, Li H, Wang X, Niu X, Ni P, Zhang W et al. Prognostic factors of Bell's palsy and Ramsay Hunt syndrome. Medicine (Baltimore). 2017;96(2):e5898.
- ↑ Clark JR, Carlson RD, Sasaki CT, Pachner AR, Steere AC. Facial paralysis in Lyme disease. Laryngoscope. 1985;95(11):1341-5.
- ↑ Hohman MH, Bhama PK, Hadlock TA. Epidemiology of iatrogenic facial nerve injury: a decade of experience. Laryngoscope. 2014;124(1):260-5.
- ↑ Adour KK, Wingerd J, Doty HE. Prevalence of concurrent diabetes mellitus and idiopathic facial paralysis (Bell’s palsy). Diabetes. 1975;24:449-51.
- ↑ Cohen Y, Lavie O, Granovsky-Grisaru S, Aboulafia Y, Diamant YZ. Bell palsy complicating pregnancy: a review. Obstet Gynecol Surv. 2000;55(3):184-8.
- ↑ 11.0 11.1 11.2 Tharani G, Rajalaxmi V, Yuvarani G, Kamatchi K. Comparison of PNF versus conventional exercises for facial symmetry and facial function in Bell's palsy. International Journal of Current Advanced Research. 2018;7(1):9347-50. . 10.24327/ijcar.2018.9350.1542. available from:
- ↑ 12.0 12.1 12.2 Baugh RF, Basura GJ, Ishii LE, Schwartz SR, Drumheller CM, Burkholder R et al. Clinical practice guideline: Bell’s palsy. Otolaryngology–Head and Neck Surgery. 2013;149(3_suppl):S1-27.
- ↑ Jenny AB, Saper CB. Organization of the facial nucleus and corticofacial projection in the monkey: a reconsideration of the upper motor neuron facial palsy. Neurology. 1987;37(6):930-9.
- ↑ MedEdPRO Facial Palsy Upper and Lower Motor Neuron Lesions - Dr MDM Available from https://www.youtube.com/watch?v=5T4G27xkckE
- ↑ Kumar A, Mafee MF, Mason T. Value of imaging in disorders of the facial nerve. Top Magn Reson Imaging. 2000;11(1):38-51.
- ↑ Zimmermann J, Jesse S, Kassubek J et al. Differential diagnosis of peripheral facial nerve palsy: a retrospective clinical, MRI and CSF-based study. J Neurol. 2019;266:2488–94.
- ↑ 17.0 17.1 Pereira LM, Obara K, Dias JM, Menacho MO, Lavado EL et al. Facial exercise therapy for facial palsy: systematic review and meta-analysis. Clinical rehabilitation. 2011;25(7):649-58.
- ↑ Jirawatnotai S, Jomkoh P, Voravitvet TY, Tirakotai W, Somboonsap N. Computerized Sunnybrook facial grading scale (SBface) application for facial paralysis evaluation. Arch Plast Surg. 2021;48(3):269-277.
- ↑ Gronseth GS, Paduga R. Evidence-based guideline update: Steroids and antivirals for Bell palsy: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2012;79 (22):2209-13.
- ↑ Butler DP, Grobbelaar AO. Facial palsy: what can the multidisciplinary team do? J Multidiscip Healthc. 2017; 10: 377-81.
- ↑ De Almeida JR, Al Khabori M, Guyatt GH, Witterick IJ, Lin VY, Nedzelski JM, Chen JM. Combined corticosteroid and antiviral treatment for Bell palsy: a systematic review and meta-analysis. Jama. 2009;302(9):985-93.
- ↑ Salinas RA, Alvarez G, Daly F, Ferreira J. Corticosteroids for Bell's palsy (idiopathic facial paralysis). Cochrane Database of Systematic Reviews. 2010(3).
- ↑ 23.0 23.1 Manikandan N. Effect of facial neuromuscular re-education on facial symmetry in patients with Bell's palsy: a randomized controlled trial. Clin Rehabil. 2007;21(4):338-43.
- ↑ Van Swearingen JM, Brach JS. Changes in facial movement and synkinesis with facial neuromuscular reeducation. Plast Reconstr Surg 2003;111:2370–2375.
- ↑ Bossi D, Buonocore M et al. Usefulness of BFB/EMG in facial palsy rehabilitation. Disabil Rehabil. 2005;27(14):809-15.
- ↑ Targan R S, Alon G, Kay SL. Effect of long-term electrical stimulation on motor recovery and improvement of clinical residuals in patients with unresolved facial nerve palsy. Otolaryngol Head Neck Surgery. 2000;122(2):246-52.
- ↑ 27.0 27.1 Monini S, Iacolucci CM, Di Traglia M, Lazzarino AI, Barbara M. Role of Kabat rehabilitation in facial nerve palsy: a randomised study on severe cases of Bell's palsy. Acta Otorhinolaryngologica Italica. 2016;36(4):282.
- ↑ 28.0 28.1 Beurskens CH, Heymans PG. Mime therapy improves facial symmetry in people with long-term facial nerve paresis: a randomised controlled trial. Australian Journal of Physiotherapy. 2006;52(3):177-83.
- ↑ de Almeida JR, Guyatt GH, Sud S, Dorion J, Hill MD, Kolber MR et al. Management of Bell palsy: clinical practice guideline. Cmaj. 2014;186(12):917-22.
- ↑ Brach JS, Van Swearingen JM. Physical therapy for facial paralysis: a tailored treatment approach. Phys Ther. 1999;79:397-404.
- ↑ van Landingham SW, Diels J, Lucarelli MJ. Physical therapy for facial nerve palsy. Current Opinion in Ophthalmology. 2018;29(5):469-75.
- ↑ Karp E, Waselchuk E, Landis C, Fahnhorst J, Lindgren B, Lyford-Pike S. Facial rehabilitation as noninvasive treatment for chronic facial nerve paralysis. Otology & Neurotology. 2019;40(2):241-5.
- ↑ Puls WC, Jarvis JC, Ruck A, Lehmann T, Guntinas-Lichius O, Volk GF. Surface electrical stimulation for facial paralysis is not harmful. Muscle Nerve. 2020;61(3):347-53.
- ↑ Teixeira LJ, Valbuza JS, Prado GF. Physical therapy for Bell's palsy (idiopathic facial paralysis). Cochrane database of systematic reviews. 2011(12).
- ↑ 35.0 35.1 Tavares-Brito J, van Veen MM, Dusseldorp JR, Bahmad F Jr, Hadlock TA. Facial palsy-specific quality of life in 920 patients: correlation with clinician-graded severity and predicting factors. Laryngoscope. 2018.