Craniotomy: Difference between revisions
Chloe Waller (talk | contribs) (Added links) |
Aya Alhindi (talk | contribs) m (corrected referencing style and added YT video showing the procedure) |
||
| (7 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
'''Original Editor '''- [[Chloe Waller]] | <div class="editorbox>'''Original Editor '''- [[User:Chloe Waller|Chloe Waller]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | |||
== Description == | == Description == | ||
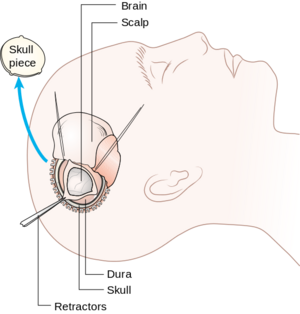
[[File:Diagram showing a craniotomy.png|thumb|alt=|Diagram showing a craniotomy]]A craniotomy is an operation where a part of the [[skull]] is removed in order to perform surgery on the [[Brain Anatomy|brain]]<ref>Brain & Spine Foundation. [https://www.brainandspine.org.uk/our-publications/our-fact-sheets/craniotomy/ Craniotomy Factsheet.] </ref>. If the removed part of [[bone]] is not put back, the operation is instead called a craniectomy, and the following surgery where the skull is reconstructed is called a cranioplasty<ref name=":0">Fernández-de Thomas RJ, De Jesus O. Craniotomy. Treasure Island (FL): StatPearls Publishing, 2022</ref>. | |||
A craniotomy | ==Indication== | ||
A craniotomy may be used in the treatment and/ or diagnosis of a number of conditions including<ref>Johns Hopkins Medicine. [https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/craniotomy Craniotomy]. </ref><ref name=":0" />: | |||
*Brain [[Brain Tumors|tumors]]. | |||
*Brain haematoma. | |||
*Aneurysms. | |||
* Brain [[Brain Tumors|tumors]]. | * | ||
* Brain haematoma. | [[Stroke|Blood clots]]. | ||
* Aneurysms. | *Increased intracranial pressure (ICP), common after [[Overview of Traumatic Brain Injury|traumatic brain injury.]] | ||
* [[Stroke|Blood clots]]. | *Arteriovenous malformations (AVMs). | ||
* Increased intracranial pressure (ICP), common after [[Overview of Traumatic Brain Injury|traumatic brain injury.]] | *Arteriovenous fistulas (AVFs). | ||
* Arteriovenous malformations (AVMs). | *Brain abscesses. | ||
* Arteriovenous fistulas (AVFs). | *Dura mater tear. | ||
* Brain abscesses. | *Skull [[Fracture|fractures]]. | ||
* Dura mater tear. | *[[Epilepsy]]. | ||
* Skull [[Fracture|fractures]]. | |||
* [[Epilepsy]]. | |||
* To implant [[Deep Brain Stimulation|stimulator devices]] for movement disorders. | * To implant [[Deep Brain Stimulation|stimulator devices]] for movement disorders. | ||
== Types of craniotomy == | ==Types of craniotomy== | ||
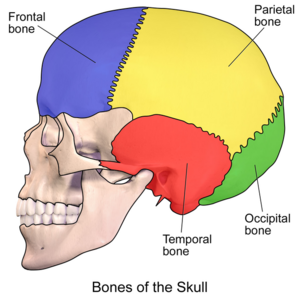
Craniotomies can be classified by the location, size or surgical technique<ref name=":1">Neurosurgeons of New Jersey. [https://www.neurosurgeonsofnewjersey.com/blog/types-of-craniotomy/ Understanding the Types and Purpose of Craniotomy.] </ref> | |||
[[File:Skull Bones.png|thumb]] | |||
The location classifications are<ref>Rao, D., Le, R. T., Fiester, P., Patel, J., Rahmathulla, G. An Illustrative Review of Common Modern Craniotomies. Journal of clinical imaging science. 2020: 10; 81.</ref>: | The location classifications are<ref>Rao, D., Le, R. T., Fiester, P., Patel, J., Rahmathulla, G. An Illustrative Review of Common Modern Craniotomies. Journal of clinical imaging science. 2020: 10; 81.</ref>: | ||
* [[Frontal Lobe|Frontal]] | *[[Frontal Lobe|Frontal]] | ||
* [[Temporal Lobe|Temporal]] | *[[Temporal Lobe|Temporal]] | ||
* [[Parietal Lobe|Parietal]] | *[[Parietal Lobe|Parietal]] | ||
* [[Occipital Bone|Occipital]] | *[[Occipital Bone|Occipital]] | ||
* Pterional (Frontotemporal) | *Pterional (Frontotemporal) | ||
* Suboccipital | *Suboccipital | ||
* Retrosigmoid | *Retrosigmoid | ||
* Orbitozygomatic | *Orbitozygomatic | ||
The size can range from the smallest, a Burr Hole craniotomy or a keyhole craniotomy, to operations with bone flaps that are multiple centimeters in diameter<ref name=":1" /><ref>Nahed B.V., Oglivy C.S., Anterior Circulation Aneurysms. In: Mohr J.P., Wolf P.A., Grotta J.C., Moskowitz M.A., Mayberg M.R., Kummer R.V. (editors). Stroke (Fifth Edition). W.B. Saunders, 2011. p.1301-1321.</ref>. | The size can range from the smallest, a Burr Hole craniotomy or a keyhole craniotomy, to operations with bone flaps that are multiple centimeters in diameter<ref name=":1" /><ref>Nahed B.V., Oglivy C.S., Anterior Circulation Aneurysms. In: Mohr J.P., Wolf P.A., Grotta J.C., Moskowitz M.A., Mayberg M.R., Kummer R.V. (editors). Stroke (Fifth Edition). W.B. Saunders, 2011. p.1301-1321.</ref>. | ||
Another type of craniotomy is an awake craniotomy, where the patient is woken up during the procedure<ref>Medindia. | Another type of craniotomy is an awake craniotomy, where the patient is woken up during the procedure<ref>Medindia. [https://www.neurosurgeonsofnewjersey.com/blog/types-of-craniotomy/ Craniotomy.]</ref>. | ||
== Post-Op Physiotherapy == | the following video shows 3D animation of craniotomy procedure: | ||
{{#ev:youtube|1RkseDeYS9g}} <ref>Amerra Medical. [https://www.youtube.com/watch?v=N7-wNsANn8g Craniectomy brain surgery - 3D animation] . Youtube; 2020. | |||
</ref> | |||
==Post-Op Physiotherapy == | |||
The level of physiotherapy intervention and rehabilitation post craniotomy varies widely, and is influenced by a number of factors including the actual surgery, the condition which is being treated, the patients' pre-morbid condition and also the general effects of being in hospital<ref>Taylor B.S., Kellner C.P., Connolly, Jr. E. | The level of physiotherapy intervention and rehabilitation post craniotomy varies widely, and is influenced by a number of factors including the actual surgery, the condition which is being treated, the patients' pre-morbid condition and also the general effects of being in hospital<ref>Taylor B.S., Kellner C.P., Connolly, Jr. E. [https://neurology.mhmedical.com/content.aspx?bookid=2155§ionid=16396534 Postcraniotomy Complication Management. In: Lee K.(editor) The NeuroICU Book (Seconds Edition)]. 2017.</ref>. | ||
Generally, the goals of physiotherapy post craniotomy are to maintain and/ or increase [[Range of Motion|range of motion]] and [[Muscle Strength Testing|muscle strength]], reduce and prevent [[spasticity]] and [[Contracture Management for Traumatic Brain Injury|contractures]], functional [[Transfer Aids|transfer]] or [[gait]] training, and to improve [[balance]] and [[Coordination Exercises|coordination]]<ref>Physio.co.uk. Neurosurgery. Available from: https://www.physio.co.uk/what-we-treat/neurological/neurosurgery/ (Accessed 14/06/2022)</ref>. | Generally, the goals of physiotherapy post craniotomy are to maintain and/ or increase [[Range of Motion|range of motion]] and [[Muscle Strength Testing|muscle strength]], reduce and prevent [[spasticity]] and [[Contracture Management for Traumatic Brain Injury|contractures]], functional [[Transfer Aids|transfer]] or [[gait]] training, and to improve [[balance]] and [[Coordination Exercises|coordination]]<ref>Physio.co.uk. Neurosurgery. Available from: https://www.physio.co.uk/what-we-treat/neurological/neurosurgery/ (Accessed 14/06/2022)</ref>. | ||
[[File:Gait rehabilitation.png|thumb]] | |||
Within Neurological Intensive Care Units, physiotherapy intervention is both safe and beneficial<ref name=":2">Sottile PD, Nordon-Craft A, Malone D, Luby DM, Schenkman M, Moss M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4498141/ Physical Therapist Treatment of Patients in the Neurological Intensive Care Unit: Description of Practice]. Phys Ther. 2015; 95:1 006-1014. </ref>. The benefits include decreased length of hospital stay, decreased time on [[Ventilation and Weaning|ventilation]], improved muscle strength and increased independence in activities of daily living<ref>Li Z, Peng X, Zhu B, Zhang Y, Xi X. [https://pubmed.ncbi.nlm.nih.gov/23127305/ Active mobilization for mechanically ventilated patients: a systematic review]. Arch Phys Med Rehabil. 2013; 94: 551–561.</ref><ref>Garzon-Serrano J, Ryan C, Waak K, Hirschberg R, Tully S. Bittner E. et al. [https://pubmed.ncbi.nlm.nih.gov/21497316/ Early mobilization in critically ill patients: patients' mobilization level depends on health care provider's profession]. PM&R. 2011; 3: 307–313. | Within [[Physiotherapists Role in ICU|Neurological Intensive Care Units]], physiotherapy intervention is both safe and beneficial<ref name=":2">Sottile PD, Nordon-Craft A, Malone D, Luby DM, Schenkman M, Moss M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4498141/ Physical Therapist Treatment of Patients in the Neurological Intensive Care Unit: Description of Practice]. Phys Ther. 2015; 95:1 006-1014. </ref>. The benefits include decreased length of hospital stay, decreased time on [[Ventilation and Weaning|ventilation]], improved muscle strength and increased independence in [[Activities of Daily Living|activities of daily living]]<ref>Li Z, Peng X, Zhu B, Zhang Y, Xi X. [https://pubmed.ncbi.nlm.nih.gov/23127305/ Active mobilization for mechanically ventilated patients: a systematic review]. Arch Phys Med Rehabil. 2013; 94: 551–561.</ref><ref>Garzon-Serrano J, Ryan C, Waak K, Hirschberg R, Tully S. Bittner E. et al. [https://pubmed.ncbi.nlm.nih.gov/21497316/ Early mobilization in critically ill patients: patients' mobilization level depends on health care provider's profession]. PM&R. 2011; 3: 307–313. | ||
</ref>. It has been found patients undergoing intracranial pressure monitoring received less frequent and intensive physiotherapy<ref name=":2" />, despite the evidence standard physiotherapy practice is safe for these patients<ref>Brimioulle S, Moraine JJ, Norrenberg D, Kahn RJ. [https://pubmed.ncbi.nlm.nih.gov/9413447/ Effects of positioning and exercise on intracranial pressure in a neurosurgical intensive care unit.] Phys Ther. 1997. Dec; 77: 1682-9</ref><ref>Anneli Thelandersson. [https://gupea.ub.gu.se/bitstream/handle/2077/41549/gupea_2077_41549_3.pdf;jsessionid=A657A807EEDF4EB3C490AE8D22007785?sequence=3 Early Physiotherapy in the Neurointensive Care Unit Passive Physiotherapy Interventions] [Dissertation] Gothenburg: University of Gotherburg. 2016</ref>. At present there are no set protocols for physiotherapy post craniotomy<ref>Srivastava A., Sharma N., Srivastav A K., Gehlot A. Functional rehabilitation in intensive care units for post craniotomy patients: study protocol. J. Physiother. Res. 2021: 11: 569-582</ref>, and instead care is directed by the physiotherapists' assessment findings. | </ref>. It has been found patients undergoing intracranial pressure monitoring received less frequent and intensive physiotherapy<ref name=":2" />, despite the evidence standard physiotherapy practice is safe for these patients<ref>Brimioulle S, Moraine JJ, Norrenberg D, Kahn RJ. [https://pubmed.ncbi.nlm.nih.gov/9413447/ Effects of positioning and exercise on intracranial pressure in a neurosurgical intensive care unit.] Phys Ther. 1997. Dec; 77: 1682-9</ref><ref>Anneli Thelandersson. [https://gupea.ub.gu.se/bitstream/handle/2077/41549/gupea_2077_41549_3.pdf;jsessionid=A657A807EEDF4EB3C490AE8D22007785?sequence=3 Early Physiotherapy in the Neurointensive Care Unit Passive Physiotherapy Interventions] [Dissertation] Gothenburg: University of Gotherburg. 2016</ref>. At present there are no set protocols for physiotherapy post craniotomy<ref>Srivastava A., Sharma N., Srivastav A K., Gehlot A. Functional rehabilitation in intensive care units for post craniotomy patients: study protocol. J. Physiother. Res. 2021: 11: 569-582</ref>, and instead care is directed by the physiotherapists' assessment findings. | ||
There can be long term impairments to a | There can be long term impairments to a patient's function and [[Quality of Life|quality of life]]<ref>Pfefferkorn T, Eppinger U, Linn J, Birnbaum T, Herzog J, Straube A. et al. [https://www.ahajournals.org/doi/10.1161/strokeaha.109.550871 Long-Term Outcome After Suboccipital Decompressive Craniectomy for Malignant Cerebellar Infarction]. Stroke. 2009; 40: 3045-3050</ref><ref>Mandona L, Bradaïa N, GuettardaI E, Bonana I, Vahedib K, Bousserb MG, et al. Do patients have any special medical or rehabilitation difficulties after a craniectomy for malignant cerebral infarction during their hospitalization in a physical medicine and rehabilitation department? Annals of Physical and Rehabilitation Medicine. 2010; 53: 86-95</ref>, for which they might require ongoing [[Neurology Treatment Techniques|physiotherapy intervention]]. Rehabilitation programs should be tailored to the individual patient abilities, prognosis and [[Goal Setting in Rehabilitation|goals]]<ref>Parreiras de Menezes KK. [https://www.iomcworld.org/open-access/physical-therapy-rehabilitation-after-traumatic-brain-injury-2155-9562-1000311.pdf Physical Therapy Rehabilitation after Traumatic Brain Injury.] J Neurol Neurophysiol. 2016; 6: 311</ref>. | ||
== Resources | ==Resources== | ||
Brain & Spine Foundation [https://www.brainandspine.org.uk/our-publications/our-fact-sheets/craniotomy/ Craniotomy Factsheet] | Brain & Spine Foundation [https://www.brainandspine.org.uk/our-publications/our-fact-sheets/craniotomy/ Craniotomy Factsheet] | ||
== References | ==References== | ||
<references /> | <references /> | ||
[[Category:Acquired Brain Injuries]] | |||
[[Category:Brain]] | |||
[[Category:Head]] | |||
[[Category:Neurology]] | |||
[[Category:Oncology]] | |||
[[Category:Neurological - Interventions]] | |||
Latest revision as of 16:03, 28 October 2023
Top Contributors - Chloe Waller, Kim Jackson, Lucinda hampton, Kirenga Bamurange Liliane, Aminat Abolade and Aya Alhindi
Description[edit | edit source]
A craniotomy is an operation where a part of the skull is removed in order to perform surgery on the brain[1]. If the removed part of bone is not put back, the operation is instead called a craniectomy, and the following surgery where the skull is reconstructed is called a cranioplasty[2].
Indication[edit | edit source]
A craniotomy may be used in the treatment and/ or diagnosis of a number of conditions including[3][2]:
- Brain tumors.
- Brain haematoma.
- Aneurysms.
- Increased intracranial pressure (ICP), common after traumatic brain injury.
- Arteriovenous malformations (AVMs).
- Arteriovenous fistulas (AVFs).
- Brain abscesses.
- Dura mater tear.
- Skull fractures.
- Epilepsy.
- To implant stimulator devices for movement disorders.
Types of craniotomy[edit | edit source]
Craniotomies can be classified by the location, size or surgical technique[4]
The location classifications are[5]:
- Orbitozygomatic
The size can range from the smallest, a Burr Hole craniotomy or a keyhole craniotomy, to operations with bone flaps that are multiple centimeters in diameter[4][6].
Another type of craniotomy is an awake craniotomy, where the patient is woken up during the procedure[7].
the following video shows 3D animation of craniotomy procedure:
Post-Op Physiotherapy[edit | edit source]
The level of physiotherapy intervention and rehabilitation post craniotomy varies widely, and is influenced by a number of factors including the actual surgery, the condition which is being treated, the patients' pre-morbid condition and also the general effects of being in hospital[9].
Generally, the goals of physiotherapy post craniotomy are to maintain and/ or increase range of motion and muscle strength, reduce and prevent spasticity and contractures, functional transfer or gait training, and to improve balance and coordination[10].
Within Neurological Intensive Care Units, physiotherapy intervention is both safe and beneficial[11]. The benefits include decreased length of hospital stay, decreased time on ventilation, improved muscle strength and increased independence in activities of daily living[12][13]. It has been found patients undergoing intracranial pressure monitoring received less frequent and intensive physiotherapy[11], despite the evidence standard physiotherapy practice is safe for these patients[14][15]. At present there are no set protocols for physiotherapy post craniotomy[16], and instead care is directed by the physiotherapists' assessment findings.
There can be long term impairments to a patient's function and quality of life[17][18], for which they might require ongoing physiotherapy intervention. Rehabilitation programs should be tailored to the individual patient abilities, prognosis and goals[19].
Resources[edit | edit source]
Brain & Spine Foundation Craniotomy Factsheet
References[edit | edit source]
- ↑ Brain & Spine Foundation. Craniotomy Factsheet.
- ↑ 2.0 2.1 Fernández-de Thomas RJ, De Jesus O. Craniotomy. Treasure Island (FL): StatPearls Publishing, 2022
- ↑ Johns Hopkins Medicine. Craniotomy.
- ↑ 4.0 4.1 Neurosurgeons of New Jersey. Understanding the Types and Purpose of Craniotomy.
- ↑ Rao, D., Le, R. T., Fiester, P., Patel, J., Rahmathulla, G. An Illustrative Review of Common Modern Craniotomies. Journal of clinical imaging science. 2020: 10; 81.
- ↑ Nahed B.V., Oglivy C.S., Anterior Circulation Aneurysms. In: Mohr J.P., Wolf P.A., Grotta J.C., Moskowitz M.A., Mayberg M.R., Kummer R.V. (editors). Stroke (Fifth Edition). W.B. Saunders, 2011. p.1301-1321.
- ↑ Medindia. Craniotomy.
- ↑ Amerra Medical. Craniectomy brain surgery - 3D animation . Youtube; 2020.
- ↑ Taylor B.S., Kellner C.P., Connolly, Jr. E. Postcraniotomy Complication Management. In: Lee K.(editor) The NeuroICU Book (Seconds Edition). 2017.
- ↑ Physio.co.uk. Neurosurgery. Available from: https://www.physio.co.uk/what-we-treat/neurological/neurosurgery/ (Accessed 14/06/2022)
- ↑ 11.0 11.1 Sottile PD, Nordon-Craft A, Malone D, Luby DM, Schenkman M, Moss M. Physical Therapist Treatment of Patients in the Neurological Intensive Care Unit: Description of Practice. Phys Ther. 2015; 95:1 006-1014.
- ↑ Li Z, Peng X, Zhu B, Zhang Y, Xi X. Active mobilization for mechanically ventilated patients: a systematic review. Arch Phys Med Rehabil. 2013; 94: 551–561.
- ↑ Garzon-Serrano J, Ryan C, Waak K, Hirschberg R, Tully S. Bittner E. et al. Early mobilization in critically ill patients: patients' mobilization level depends on health care provider's profession. PM&R. 2011; 3: 307–313.
- ↑ Brimioulle S, Moraine JJ, Norrenberg D, Kahn RJ. Effects of positioning and exercise on intracranial pressure in a neurosurgical intensive care unit. Phys Ther. 1997. Dec; 77: 1682-9
- ↑ Anneli Thelandersson. Early Physiotherapy in the Neurointensive Care Unit Passive Physiotherapy Interventions [Dissertation] Gothenburg: University of Gotherburg. 2016
- ↑ Srivastava A., Sharma N., Srivastav A K., Gehlot A. Functional rehabilitation in intensive care units for post craniotomy patients: study protocol. J. Physiother. Res. 2021: 11: 569-582
- ↑ Pfefferkorn T, Eppinger U, Linn J, Birnbaum T, Herzog J, Straube A. et al. Long-Term Outcome After Suboccipital Decompressive Craniectomy for Malignant Cerebellar Infarction. Stroke. 2009; 40: 3045-3050
- ↑ Mandona L, Bradaïa N, GuettardaI E, Bonana I, Vahedib K, Bousserb MG, et al. Do patients have any special medical or rehabilitation difficulties after a craniectomy for malignant cerebral infarction during their hospitalization in a physical medicine and rehabilitation department? Annals of Physical and Rehabilitation Medicine. 2010; 53: 86-95
- ↑ Parreiras de Menezes KK. Physical Therapy Rehabilitation after Traumatic Brain Injury. J Neurol Neurophysiol. 2016; 6: 311