Carers Guide to Dementia
Original Editor - Aileen Lambe, Aisling Kavanagh, Carla Ellis, Claire Hagan as part of the Queen Margaret University's Current and Emerging Roles in Physiotherapy Practice Project
Top Contributors - Carla Ellis, Aisling Kavanagh, Scott Buxton, Claire Hagan, Aileen Lambe, Kim Jackson, Lucinda hampton, Shaimaa Eldib, Admin, Gillian Condy, Eugenie Lamprecht, 127.0.0.1, Tony Lowe, Vidya Acharya and Lauren Lopez
Introduction[edit | edit source]
Currently, Dementia neurodegenerative disease has no known cure and is not part of the normal ageing process. It is characterised by changes in reasoning, memory, comprehension, problem-solving, and/or attention[1].
Some statistics;
- 750,000 people are living with dementia in the UK at present.
- This number is expected to double over the next 30 years.
- As of 2010, 35.6 million people worldwide have dementia [2].
- 25% of hospital beds are occupied by people over the age of 65 with dementia [3].
Types of Dementia[edit | edit source]
There are many types of dementia. Below is a list of the most common forms of dementia, with their prevalence. In some cases, the cause may be another disease (eg. Huntington's disease) or from a head injury.
- Dementia with Alzheimer's disease = 62%: This is the most common form of dementia. Loss of nerve tissue along with changes in the chemistry and structure of the brain leads to the death of brain cells.
- Vascular Dementia = 17%: This is more common following a stroke or a series of small strokes. The blood - and oxygen supply to the brain are affected, causing brain cells to die. The person may start to forget or have trouble planning ahead. Balance problems can also occur.
- Dementia with Lewy Bodies = 4%: This is caused by the breakdown of brain tissue following the formation of abnormal structures in nerve cells. The individual will generally have slower movement patterns and increased risk of falling[4].
- Fronto-Temporal Dementia = 2%: This is due to damage to the anterior part of the brain, leading to personality - and behaviour changes. Memory is less likely to be affected in the early stages.
- Mixed Dementia = 10%: this form of Dementia has the characteristics of both Alzheimer's Disease and vascular dementia.
Less common causes of dementia:[edit | edit source]
- Motor Neurone Disease.
- Multiple Sclerosis (MS).
- Huntington's Disease.
- Parkinson's (2%).
- HIV related cognitive impairment.
- Creutzfeldt-Jakobs Disease (CJD) :it is a degenerative brain disorder that leads to dementia and it belongs to the group of transmissible spongiform encephalopathies (TSE) or prion diseases.[5]
- Korsakoff's Syndrome: caused by heavy drinking over a long period that leads to brain cell death and short-term memory loss. Although not strictly classified as dementia, it is included here as symptoms are similar.
For more information on the different types of dementia visit this site.
Alzheimer's Disease[edit | edit source]
As explained above Alzheimer's Disease is the most common form of dementia with approximately 62% of dementia cases involving Alzheimer's Disease equating to more than 520,000 people in the UK[6]. During the course of the disease proteins called 'plaques' and 'tangles' build up within the nerve cells of the brain leading to nerve cells dying off and loss of brain tissue. There is also a shortage of neurotransmitters causing ineffective nerve conduction. As these 'plaques' and 'tangles' increase in numbers so does the severity of symptoms with different areas of the brain being involved.
Symptoms[edit | edit source]
Symptoms of Alzheimer's can be said to progress through 7 stages[7]
- Stage 1 - No impairment - The person does not experience memory, movement or cognitive difficulties.
- Stage 2 - Very Mild Cognitive Decline
- Stage 3 - Mild Cognitive Decline - Family and friends begin noticing cognitive difficulties at this stage, there are common difficulties including; difficulties finding names, difficulties retaining new information, social and work interactions are challenging, losing and misplacing valuable items and difficulty planning or organising.
- Stage 4 - Moderate Cognitive Decline - At this stage clear symptoms are evident in several areas; forgetful of recent events, difficulty with challenging mental arithmetic, complex planning tasks are nearly impossible, forgetful of the persons own history, mood swings, withdrawn and frustration set in.
- Stage 5 - Moderately Severe Cognitive Decline - Day-to-day activities become a challenge, recalling addresses, phone number, orientation to place, choosing to clothe and remembering significant details about themselves all decline into almost impossible tasks however eating and toileting are still independent.
- Stage 6 - Severe Cognitive Decline - Memory and personality changes worsen and individuals need help with daily activities. Individuals may; lose awareness of recent experiences, difficulty remembering their own name, unable to remember familiar faces, need help dressing, making mistakes with buttons, major changes in sleep patterns, need help with toileting including Urinary Incontinence, major personality changes and wandering becomes commonplace with a subsequent increase in falls. Hallucinations and delusions may also become troubling for the person with dementia.
- Stage 7 - Very Severe Cognitive Decline - In this final stage of the disease process individuals lose the ability to respond to their environments, all daily activities need to be assisted, muscles grow rigid and swallowing becomes impaired.
Most people who develop Alzheimer's Disease are over the age of 65 but younger people can develop the disease. Currently it is estimated the 40,000 under the age of 65 in the UK have early-onset Alzheimer's[6].
Vascular Dementia[edit | edit source]
This is the second most common type of dementia affecting approximately 150,000 people in the UK[6]. In vascular dementia, the individual suffers similar symptoms to other types of dementia, such as Alzheimer's Disease, but the cause of the cognitive decline is different. These symptoms occur when the brain is damaged because of problems with blood supply to the brain. Nerve cells need perfusion, just like any other cell in the body, and they die when blood does not reach them. The death of the nerve cells then causes the brain to decrease in abilities and performance leading to dementia. There are different types of vascular dementia.
- Stroke-related Dementia , A stroke occurs when there is a sudden cut off in the blood supply to the brain causing death to a large are of the brain, depending on the location the symptoms can vary greatly.
- Post-stroke Dementia , Not everyone who has a stoke will develop dementia but around 20% do[6] and it will develop within 6 months of the cerebrovascular event.
- Single-infarct and Multi-infarct Dementia , This occurs when a single stroke is large enough to cause cognitive impairment or when several strokes cause cognitive impairment.
- Subcortical Dementia - This is the most common form of vascular dementia, the blood vessels which lie deep within the brain tissue become sclerotic causing impaired circulation to smaller nerves. These nerves which are damaged are known as the white matter and lie deeper within the brain so the symptoms of this type of dementia are different.
Symptoms[edit | edit source]
The symptoms caused by vascular dementia varies greatly between individuals, which relies upon which type and the severity of the vascular damage done to the individual. The symptoms may be similar to other dementia types and also to Alzheimer's Disease.
The most common symptoms include:
- Problems with planning, organising, decision making and solving problems.
- Slower thought processing.
- Poor concentration.
- Memory difficulties when recalling events.
- Speech may become less fluent.
- Problems perceiving and solving problems involving visuospatial skills.
- Apathy and mood changes.
- Stroke related movement and sensory impairments.
- Early loss of bladder control.
Risk Factors[edit | edit source]
- Age is the strongest risk factor with risk doubling every 5 years over the age of 65.
- Men are at slightly increased risk.
- Stroke or diabetes patients suffer are at double the risk.
- Sleep Apnoea.
- Depression.
- Cardiovascular disease.
- Genetic factors.
- Ethnicity.
Dementia with Lewy Bodies[edit | edit source]
Dementia with Lewy Bodies(DLB) shares symptoms of Alzheimer's Disease and Parkinson's accounting for approximately 10% of all dementia cases. Lewy bodies are tiny deposits of protein in nerve cells and have been linked to a reduction in acetylcholine and dopamine. Over time the nerve cells and brain tissue progressively dies off. Depending on where the Lewy bodies are located the symptoms can vary, if they are deep in the brain then movement symptoms are likely and if they are in the outer layers of the brain then cognitive problems arise. Movement and cognitive problems can occur together, with around 33% of Parkinson's individuals developing dementia later on in the disease process. Around 66% of DLB sufferers having movement disorder symptoms at some stage.
Symptoms[edit | edit source]
The initial symptoms of DLB include difficulties with attention and alertness and fluctuate greatly throughout the day. There may be difficulties perceiving objects in three dimensions and judging distances along with planning and organising. The symptoms are very individual, in keeping with the pathological process, and can vary day-to-day. Visual hallucinations and delusions occur greatly in DLB patients and can be very distressing, they can be very detailed in nature and need to be handled sensitively. Up to two-thirds of DLB patients have movement disorders in keeping with Parkinsonism such as; rigidity, tremor, reduced blink rate, lack of facial expression and stooped postures. These movement symptoms are why persons with DLB are prone to falls. At night symptoms persist with restless legs and impaired REM sleep leading to fatigue during the day. As DLB is progressive symptoms worsen and cognitive decline sets in with similar cognitive difficulties as mid-late stage Alzheimer's dementia. On average someone might live for 8 years after DLB symptoms onset.
Normal Ageing Vs Early Signs of Dementia [edit | edit source]
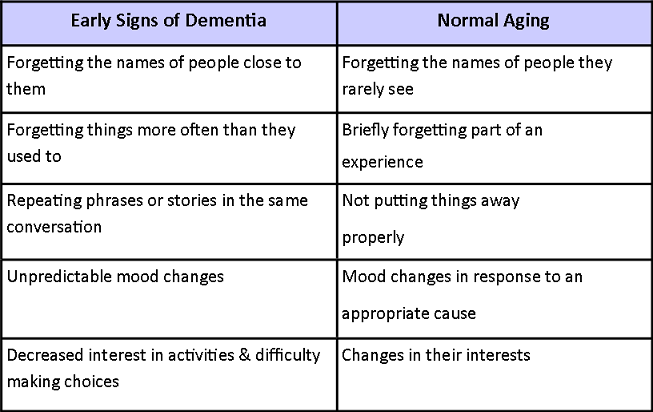
It is sometimes difficult to tell the difference between what is normal ageing and what is the early onset of dementia. You may be concerned that an elderly relative or friend is developing dementia. So, how will you know? In normal ageing, the term Mild Cognitive Impairment describes problems with mental abilities such as thinking, knowing and remembering. People with mild cognitive impairment often have difficulties with day-to-day memory, however these signs do not mean that the person is suffering from dementia [8]. You can use this table to compare the signs of early-onset dementia and normal ageing.
The 3 Stages of Dementia[edit | edit source]
This table shows the 3 generalised 'main stages' of the different types of dementia. It is important to consider each type specifically as they each have their own characteristic symptoms. It is available here as a document if you wish to print it off or save it for future reference. To open this document click on this link and then the file name File:The Three Main Stages of Dementia Download 2.pdf
Some symptoms may appear earlier or later than indicated on this table and the stages may overlap. Progression through the stages varies from person to person and depends on many factors including:
1. The type of dementia
2. Age of onset
3. The presence of other illnesses
4. The level of support and care available
What else to expect?[edit | edit source]
People with dementia may suffer from depression and/or behavioural problems. They may often become easily irritated/ frustrated or act aggressively towards a family member or friend. Behaviour management is one strategy that is used to decrease depression in individuals with dementia and can be carried out by carers. Reducing the repetition of words, managing aggression and the eating behaviours in people with dementia has a positive effect on their behaviour and overall well-being [12].
Mood is also commonly affected in individuals with dementia. Individuals can often become flustered and distressed and in some cases can become aggressive and depressed. Regular movement will balance their mood, help to reduce depression and keep them calm. Physical activities can help improve sleep pattern which can often be disturbed by dementia. Regular routines can include household activities, exercise classes, resistance training and stretching [13].
What Can Physiotherapy Offer?[edit | edit source]
Physiotherapists use movement of the body to help bring about physical, psychological and social well-being. Physiotherapy has an important role in promoting and maintaining mobility in people with dementia as well as improving their quality of life and reducing the burden of care.
More information on dementia and physiotherapy can be found by following this link
Fall prevention[edit | edit source]
Poor balance is known to increase the risk of falls. Physiotherapy can lower an individual's risk of falling by providing exercises specifically for improving balance. Fall prevention programmes can also address their fear of falling to ensure they maintain independence and safety with ADLs.
Some Facts and Figures:[edit | edit source]
In those over the age of 65,
- 1 in 3 women will fall
- 1 in 5 men will fall
- The risk of falling will increase even higher if the individual also suffers from dementia[14].
It is important that the fear of falling does not cause the person with dementia to stop being active, as inactivity can lead to many health complications. To help avoid inactivity you can focus on:
- Improving the person's mobility and,
- Maintaining their independence and confidence.
The ultimate aim is to reduce the fear of falling and maintain function.
More information about falls can be found here.
Benefits of Exercise [edit | edit source]
Exercise prevents and reduces the risk of developing heart conditions.
Examples of heart conditions are:
- Angina
- Hardening of the arteries- often due to cholesterol
- High Blood Pressure
- Palpitations
Exercise is also recommended in people with Type 2 Diabetes [15].
Exercise has also been linked with improving bone density and preventing osteoporosis [16]. This is especially important in women. Exercise should be weight-bearing, this means any exercise where the hands and feet support your weight [17]. Examples are walking, dancing and lifting weights. Although cycling and swimming are good forms of exercise they are not weight-bearing and so will not help improve bone density. Taking part in physical exercise also enhances mood and improve mental function [18]. This, in turn, may decrease the need for management with drugs & medications [16].
Physiotherapy & Exercise[edit | edit source]
Physiotherapy can provide;
- Strengthening exercises: to increase bone strength and decrease the risk of osteoporosis.
- Balance: to prevent falls and increase confidence in everyday tasks.
- Flexibility & stretching: to prevent muscle tightening and make movement easier.
- Maintenance of independence: to stay as involved as possible for as long as possible in everyday life.
- Postural management: Regular change in body position is essential for comfort and prevention of poor posture which may lead to muscle tightness and spasms, decreased movement of joints and pressure sores [19].
- Help and advice on aids for the house: Equipment and adaptations at home will help make life easier for your loved one with dementia and keep them independent for as long as possible
It is also assessed everyday activities such as walking, going up and downstairs, getting out of a chair and getting in and out of bed. If someone is struggling to do any of these activities appropriate exercises should be incorporated into the treatment plan.
Physiotherapy and Pain[edit | edit source]
Physiotherapy can help manage pain. Pain affects mental function, motivation and will affect how the person with dementia responds to any rehabilitation programme. People living with dementia who have difficulty speaking will not be able to easily report pain. These people are at risk of receiving inadequate medication and treatment of pain. It is important that pain is addressed before and during therapy to allow for better rehabilitation [12].
Education[edit | edit source]
By teaching carers about the disease, they will know what to expect and be better able to handle the challenges associated with dementia. Some suggestions are:
- Create a daily routine with small rituals - Predictability can be calming. This may help to relax the person.
- Allow the individual do as much as they can independently
- Give the individual a role/task; doing the washing up, peeling the vegetables, pairing socks.
- Do less for them while encouraging them to do more for themselves.
- If motivation is an issue, make the tasks functional: walk to the kitchen to get a drink instead of carrying it to them.
- If the person is wandering around or restless, then think about why this might be happening. Some people walk because they are bored, have excess energy or it may be a reaction to an hallucination.
- By doing as much as possible by themselves, they will be more likely to retain their self esteem.
- Plan activities that you can both enjoy
- If it is realistic to do so, encourage them to take the person for a walk each day. It will burn off energy and the fresh air will do them both good.
- Encourage other activities such as gardening, baking, listening to music, singing, dancing or playing cards. What is important is that the person is participating in an activity that makes him/her feel useful.
- Assess the home - The home can be full of potential hazards contributing to falls. Make sure there is nothing around the house that the person could trip on. For example carpets, rugs, doorway thresholds.
Improve Communication[edit | edit source]
- Keep commands simple- one request at a time.
- Allow extra time for a response to your question before repeating it.
- If the individual doesn't appear to understand your request, try rephrasing it.
- Don't chat whilst the person is trying to perform a task, this will likely be a distraction.
- Make sure communication problems are not due to problems with the individual's sight or hearing. Check that glasses and hearing aids are in good working order.
- Use names and explain phrases where possible, such as "Your son, John."
Other forms of communication that may be useful [edit | edit source]
Touch :can be used to help movement during walking by placing a hand on their shoulder or by taking their hand.
Sounds :can provide extra stimulation to encourage normal movement or to trigger a response to an instruction. Walking can improve by providing rhythm, for example counting aloud or by playing music with a rhythm the person can walk to.
Visual communication: can be used to show tasks or give instructions. When performing exercises it is betting o show the exercise than to say the instructions [12].
Resources[edit | edit source]
www.mentalhealth.org.uk - A charity that works across all age ranges and all aspects of mental health. Type “Dementia” in to the search box for helpful information and publications relating to dementia.
http://www.alz.co.uk/ADI-publications - An international website dedicated to Alzheimer’s Disease. Contains information and support networks for those suffering from the disease and those who are care for loved ones
For NHS information about dementia follow this link
For NHS information about support for carers, care homes and financial support follow this link
For information about Alzheimer' Disease follow this link
For information about the Lewy Body Dementia Association follow this link
For information about the Parkinson's Foundation and research into the disease follow this link
For information about Parkinson's and support available follow this link
For information about Huntingtons's disease and support in England & Wales follow this link
Carers Support Networks [edit | edit source]
Carers UK is a charity set up to help carers. This website provides information and advice about caring, alongside practical and emotional support for carers. There is an online community network where you can chat online with other carers and share your experiences.
http://www.carersuk.org
This is an international carers support network that provides support and friendship between carers online.
http://www.carersconnectint.com/Home.aspx?pid=10
Alzheimer's and Dementia Support Services (ADSS) is a charity that provides support for carers including a 24 hour help line (0800 500 3014). Calls are free from a landline within the UK but a charge may be incurred from moblies.
www.alzheimers-dementia.org.uk
References[edit | edit source]
- ↑ NHS Choices 2012. www.nhs.uk/conditions/dementia/pages/introduction/apsx (accessed 21/10/2012)
- ↑ Alzheimers UK (2012) The Global Voice on Dementia. Available online at: www.alz.co.uk/research/statistics Accessed on 12/11/2012
- ↑ Chartered Society of Physiotherapy 2012 http://www.csp.org.uk/publications/physiotherapy-works-dementia-care (accessed 21/10/2012)
- ↑ Gaig C, Valldeoriola F, Gelpi E, Ezquerra M, Llufriu S, Buongiorno M, Rey MJ, Martí MJ, Graus F, Tolosa E. Rapidly progressive diffuse Lewy body disease. Movement disorders. 2011 Jun;26(7):1316-23.
- ↑ Gubbels S, Bacci S, Laursen H, Høgenhaven H, Cowan S, Mølbak K, Christiansen M. Description and analysis of 12 years of surveillance for Creutzfeldt–Jakob disease in Denmark, 1997 to 2008. Eurosurveillance. 2012 Apr 12;17(15):20142.
- ↑ 6.0 6.1 6.2 6.3 ALzhimer's Society. What is Alzheimer's Disease? [ONLINE] available from http://www.alzheimers.org.uk/site/scripts/documents_info.php?documentID=100 [Accessed] 19/04/2015
- ↑ ALZ.org. Disease stages. [ONLINE] Accessed from http://www.alz.org/alzheimers_disease_stages_of_alzheimers.asp 19/04/2015
- ↑ Alzheimers UK (2012) Available online at: http://www.alzheimers.org.uk/site/scripts/documents_info.php?documentID=120 Accessed on 12/11/2012
- ↑ http://www.onmemory.ca/en/signs_symptoms/aging_vs_alzheimers/ (accessed on 21/10/2012)
- ↑ http://www.psychiatry24x7.com/bgdisplay.jhtml?itemname=dementia_memoryloss
- ↑ Psychiatry 24 7 (2012) Available online at:http://www.psychiatry24x7.com/bgdisplay.jhtml?itemname=dementia_symptoms#stages Accessed 12/11/2012)
- ↑ 12.0 12.1 12.2 Marshall, M. 2005. Perspectives on Rehabilitation and Dementia. [Online book] London: Jessica Kingsley. Available at: http://books.google.co.uk/books/about/Perspectives_On_Rehabilitation_And_Demen.html?id=KqhaW28SZ8oC [Accessed November 05 2012]
- ↑ Dementia Physiotherapist (2012) Available online at: http://www.healthcentre.org.uk/physiotherapists/physiotherapist-dementia.html Accessed 12/11/2012)
- ↑ O'Loughlin, JL; Robitaille, Y; Boivin, JF & Suissia, S. 1993. Incidence of and risk factors for falls and injurious falls amoung the community dwelling elderly. American Journal of Epidemiology. Vol 137 (3) 342-354
- ↑ Diabetes and Exercise (2012) Available online at: http://www.diabetes.org.uk/Documents/Position%20statements/ABCD%20position%20statement%20on%20exercise%5b1%5d.pdf Accessed on 12/11/2012
- ↑ 16.0 16.1 Heyn, P., Abreu, B.C. and Ottenbacher, K.J. 2004. The Effects of Exercise Training on Elderly Persons With Cognitive Impairment and Dementia: A Meta-Analysis. Archive of Physical Medicine and Rehabilitation. Vol 85, pp. 1694-1704
- ↑ NHS (2012) Osteoporosis prevention Available online at http://www.nhs.uk/Conditions/Osteoporosis/Pages/Prevention.aspx Accessed 12/11/2012
- ↑ Toulette, C., Fabre, C., Dangremont, B., Lensel, G. and Thevenon, A. 2003. Effects of physical training on the physical capacity of frail, demented patients with a history of falling: A randomised controlled trial. Age and Ageing. Vol 32, pp. 67-73
- ↑ NHS Postural Management Survey 2012