Lumbar Fusion Rehabilitation: Difference between revisions
No edit summary |
Candace Goh (talk | contribs) mNo edit summary |
||
| (52 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox">Original Editor - [[User:Mariam Hashem|Mariam Hashem]] | |||
Top Contributors - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | |||
[[ | ==Introduction== | ||
[[Lumbar]] Spine Fusion is an effective treatment option to stabilise the painful motion segment, and may provide indirect decompression of the neural elements, restore lordosis and correct deformity<ref name=":1">Mobbs, R. J., Phan, K., Malham, G., Seex, K., & Rao, P. J. (2015). [https://scholar.google.com/scholar_url?url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5039869/&hl=en&sa=T&oi=gsb-ggp&ct=res&cd=0&d=13017676127347181189&ei=GZ2uY_yfMYa8yATUzZGgCg&scisig=AAGBfm03lVzUHVhRGS8YC8pG4Qkj11Oclg Lumbar interbody fusion] : techniques , indications and comparison of interbody fusion options including PLIF , TLIF , MI-TLIF , OLIF / ATP , LLIF and ALIF, ''3''(1), 2–18. <nowiki>https://doi.org/10.3978/j.issn.2414-469X.2015.10.05</nowiki></ref>. | |||
== | The [[Surgery and General Anaesthetic|surgery]] involves placement of an implant (cage, spacer or structural graft) within the intervertebral space after discectomy<ref name=":1" /> and successful union of two or more [[Lumbar Vertebrae|vertebra]]<ref name=":0" />. | ||
==== | ==Indications== | ||
* Discogenic/facetogenic low back pain<ref name=":1" />. | |||
* Post traumatic cases of segmental instability or potential neurologic injury<ref name=":1" />. | |||
- | * Degenerative spinal pathology with failure of conservative treatment<ref name=":0">Maxey, L. and Magnusson, J. (n.d.). [https://scholar.google.com/scholar_url?url=https://books.google.com/books%3Fhl%3Den%26lr%3D%26id%3DnxO7kIdEsPMC%26oi%3Dfnd%26pg%3DPP1%26dq%3DMaxey,%2BL.%2Band%2BMagnusson,%2BJ.%2B(n.d.).%25C2%25A0Rehabilitation%2Bfor%2Bthe%2Bpostsurgical%2Borthopedic%2Bpatient.%26ots%3DSR6thhGWWS%26sig%3Dklqy-qyNuMYlSy0rQ8DGa_bGFtg&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=735113821912823632&ei=Rp2uY4zkK86vywS1g6foAw&scisig=AAGBfm1tw_Lpmaw0JpgOf8sR51piVaVw_A Rehabilitation for the postsurgical orthopedic patient.]</ref>. | ||
* Neurogenic claudication<ref name=":1" />. | |||
* [[Radiculopathy]] due to foraminal stenosis<ref name=":1" />. | |||
* Lumbar degenerative spinal deformity including symptomatic [[spondylolisthesis]] and degenerative [[scoliosis]]<ref name=":1" />. | |||
==Degenerative cascade== | |||
[[Degenerative Disc Disease]] | |||
* | ==Diagnosis== | ||
[[File:Narrow disc space.jpg|thumb]] | |||
* | * Confirmatory diagnostic testing often includes [[MRI Scans|MRI]] scanning and discography for equivocal cases.<ref name=":0" /> | ||
* Spinal radiographs showing: | |||
** [[Osteophyte|Osteophytes]] and segmental disc space narrowing in patients with degenerative spondylosis. | |||
** A defect in the pars interarticularis. | |||
** Anterolisthesis, or a forward slippage of one vertebra on the next, is the hallmark radiographic finding in spondylolisthesis. | |||
** Flexion and extension films can help to detect hypermobility or excessive motion in degenerative lumbar conditions. | |||
[[File:Degenerative disc diseaseMRI.jpg|thumb]] | |||
==Lumbar Fusion Approaches== | |||
- | Today, most spine surgeons use pedicle screw constructs to immobilise the vertebrae rigidly while preserving the normal lumbar lordosis.<ref>Burkus K, et al: [https://pubmed.ncbi.nlm.nih.gov/19411467/ Six-year outcomes of anterior lumbar interbody arthrodesis with use of interbody fusion cages and recombinant human bone morphogenic protein-2.] J Bone Joint Surg 91:1181-1189, 2009. | ||
</ref> | |||
=== | === Posterolateral Lumbar Fusion === | ||
A midline posterior incision, with a [[laminectomy]] if necessary. | |||
Transverse process, pars interarticularis, and if needed, the sacral alae are decorticated (posterior fusion). then a bone graft is placed on the decorticated surfaces. | |||
Pedicle screws and rods or plates may be placed to immobilise the motion segments rigidly and augment the formation of a solid union. | |||
===== | In routine cases of posterolateral fusions the disc is not radically resected. Biomechanical studies have shown that people bear load through the middle and posterior thirds of the disc. Several reports describe a persistently painful disc under a solid posterior fusion.<ref>Ibrahim T, et al: [https://scholar.google.com/scholar_url?url=https://link.springer.com/article/10.1007/s00264-006-0269-6&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=403217471083671544&ei=9p2uY_yAG8iBywTQ4KTQBg&scisig=AAGBfm1wcM6MmVGO41v5s4Dk4dWF4SKhAg Surgical versus non-surgical treatment of chronic low back pain]: A meta-analysis of randomized trials. Int Orthop 32(7):107-113, 2006. | ||
</ref> | |||
===== D-Lateral Interbody Fusion | === Interbody Fusion === | ||
[[File:Posterior lumbar interbody fusion.jpg|thumb]] | |||
* A-posterior lumbar fusion (PLIF): associated with a higher incidence of postsurgical nerve injuries. | |||
* B- Transformational Lumbar Interbody Fusion | |||
* C-Anterior Lumbar Interbody Fusion | |||
* D-Lateral Interbody Fusion: nerve stretch injury reported, with L4 nerve root injury most common.<ref>Knight RQ, et al: [https://scholar.google.com/scholar_url?url=https://journals.lww.com/jspinaldisorders/fulltext/2009/02000/Direct_Lateral_Lumbar_Interbody_Fusion_for.6.aspx&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=12035724177052866777&ei=G56uY8LKOs6TywSl1LXoCA&scisig=AAGBfm2TE8ro7OlZOPlqajVOaxFcK8GCAg Direct lateral lumbar interbody fusion for degenerative conditions]: Early complication profile. J Spinal Disord Tech 22(1):34-37, 2009. | |||
</ref> | |||
* E-Interbody Cages: hollow cylinders made of titanium, carbon ,or bone filled with autogenous bone graft or a bone graft substitute and inserted between the vertebral bodies.<ref name=":0" /> | |||
{{#ev:youtube|N-2Gy3iIeu8}} | |||
== | ==Rehabilitation== | ||
=== | ===Preoperative phase:=== | ||
This is the proper timing for assessing functional outcomes and psychological support. | This is the proper timing for assessing functional outcomes and psychological support. This is possible through patient education, which includes: | ||
* | * [[CPR for Lumbar Stabilisation|Stabilisation-based exercises]] | ||
* Postoperative precautions | * Postoperative precautions | ||
* Bed mobility and transfers | * Bed mobility and transfers | ||
* Initial postoperative exercises | * Initial postoperative exercises | ||
* Gait training with any necessary assistive devices | * [[Gait training]] with any necessary [[Assistive Devices|assistive devices]] | ||
* Donning and doffing any required braces | * Donning and doffing any required braces | ||
* Wound care | * [[Wound Care Basics: Objective Assessment|Wound care]] | ||
* General overview and prognosis of the postoperative rehabilitation process | * General overview and prognosis of the postoperative rehabilitation process | ||
A tour of the facility and operating room along with meeting with individuals who have already undergone such a procedure may also help to decrease patient anxiety surrounding the surgery and hospital experience.<ref>Kisner C, Colby LA: [https://scholar.google.com/scholar_url?url=https://books.google.com/books%3Fhl%3Den%26lr%3D%26id%3DyZc6DwAAQBAJ%26oi%3Dfnd%26pg%3DPR1%26dq%3DKisner%2BC,%2BColby%2BLA%2B%2BTherapeutic%2Bexercise%2B%2BFoundations%2Band%2Btechniques,%2Bed%2B5,%2BPhiladelphia,%2B2007,%2BFA%2BDavis.%26ots%3DNfw0F2hDUe%26sig%3D10CnqTfr7cQUruuwAq0Z_ABIgUw&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=16766534394545827191&ei=RZ6uY_z3K86TywSl1LXoCA&scisig=AAGBfm3-Xke7HiSACVwH3GheEawiwvbxgg Therapeutic exercise: Foundations and techniques], ed 5, Philadelphia, 2007, FA Davis. | |||
</ref> | |||
- | |||
Therapist must have a complete picture about the procedure, surgical approach and fused levels. | |||
' | Note: During a posterior fusion, the multifidi are retracted from the spine. This partially tears the dorsal divisions of the spinal nerves, resulting in partial denervation of the multifidi. If an anterior fusion also has been performed, then a midline skin incision will be apparent and the abdominal muscular incision is lateral. The incision passes through the obliques, also partially denervating them. For this reason the therapist should teach the patient the proper way to recruit the transverse abdominis (TA), multifidi, and pelvic floor muscles and watch for any substitution patterns to promote proper spinal stabilisation.<ref name=":0" /> | ||
* [[Range of Motion|ROM]] | |||
* [[Posture]] | |||
* [[Balance]] | |||
* Gait | |||
* Strength | |||
* Body mechanics | |||
* Specific functional tasks | |||
* Specific [[Neurological Assessment|Neurological examination]] | |||
* The evaluation shouldn't include Lumbar ROM or hip flexor mobility especially at first stages of rehabilitation.<ref name=":0" /> | |||
===Phase I:=== | |||
* 1 to 5 days after surgery (inpatient) and up to 6 Weeks | |||
* Most patients are referred for physiotherapy anywhere between 4 to 7 weeks after their discharge from the hospital. | |||
* Physical therapy management during this phase consists of teaching patients the proper way to get in and out of bed, dress and perform other self-care activities, and walk (perhaps with a walker for the first 1 or 2 days). | |||
* Light TA and pelvic floor contractions to begin to practice them in different positions. | |||
* The therapist also can teach basic and simple neural mobilisation for the nerves involving the lumbosacral plexus. | |||
* Patients and their family should leave the hospital with an understanding of the home care required until they begin their outpatient physical therapy.<ref name=":0" /> | |||
Patients should be | ===Phase II:=== | ||
* 6 to 10 weeks after surgery | |||
* Patients should begin to approximate normal activities while the therapist controls | |||
* Patients should be slowly working up to 30 minutes of exercise and physical activity at least 5 days a week. | |||
* They can begin a light weight-training program, avoiding exercises that inappropriately load the lumbar spine but making sure to include some exercise for the lumbar paraspinals and other muscles that attach to the thoracodorsal fascia.<ref name=":0" /> | |||
* '''Common restrictions are no lifting greater than 10lb.''' '''and no overhead lifting.'''<ref>Thompson WR, editor: [https://scholar.google.com/scholar_url?url=https://books.google.com/books%3Fhl%3Den%26lr%3D%26id%3DhhosAwAAQBAJ%26oi%3Dfnd%26pg%3DPP1%26dq%3DThompson%2BWR,%2Beditor%2B%2BACSM%25E2%2580%2599s%2Bguidelines%2Bfor%2Bexercise%2Btesting%2Band%2Bprescription,%2Bed%2B8,%2BAmerican%2BCollege%2Bof%2BSports%2BMedicine,%2BBaltimore,%2B2004,%2BLippincott%2BWilliams%2B%2526%2BWilkins.%26ots%3DlkH41J-YPC%26sig%3D6faYgZ80ZWts_MwOxMeW7XF2-90&hl=en&sa=T&oi=gsb&ct=res&cd=0&d=15677296915985333758&ei=hZ6uY5HJIoa8yATUzZGgCg&scisig=AAGBfm1n3SOrwWUIlSL1Sd4nt23Y4M1vZQ ACSM’s guidelines for exercise testing and prescription], ed 8, American College of Sports Medicine, Baltimore, 2004, Lippincott Williams & Wilkins. | |||
</ref> | |||
==== '''Goals''' ==== | |||
* Achieve good body mechanics during ADL | |||
* Protect the surgical site from infection and mechanical stress | |||
* Nerve root mobility at the involved levels | |||
* Control pain and inflammation | |||
* Begin a stabilisation and reconditioning program | |||
* Improve scar and surrounding soft tissue mobility | |||
* Treat restrictions of thoracic, UEs, and LEs that can lead to more strain on the lumbar spine<ref name=":0" /> | |||
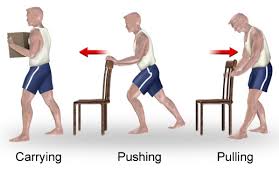
==== Body mechanics education ==== | |||
* Ved mobility | |||
* Pushing and pulling | |||
* [[Lifting]] and carrying | |||
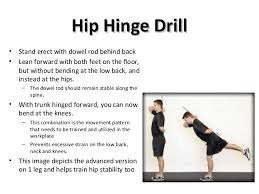
* [[Hip Hinge|Hip hinge technique]] | |||
See [[Injury Prevention and Body Mechanics]][[File:Push and pull.jpg|thumb|none]] | |||
[[File:Lifting mechanics.jpg|thumb|none]][[File:Hip hinge.jpg|thumb|none]] | |||
==== Nerve root gliding techniques ==== | |||
[[File:Nerve root gliding.png|thumb]] | |||
Patients should extend the knee while lying supine with the spine in a neutral position and the hip flexed to a 90° angle. When tension is encountered, the therapist helps the patient work the knee or ankle gently back and forth, gradually increasing the ROM. This stretch may cause increased symptoms during the stretch, which should resolve immediately on relaxing. | |||
' | ==== Pain management ==== | ||
* Prescribed medications and ice. | |||
* Ultrasound shouldn't be applied over a healing bony fusion. | |||
* Patients with severe pain problems can try using a home [https://www.physio-pedia.com/Transcutaneous_Electrical_Nerve_Stimulation_(TENS) transcutaneous electrical nerve stimulation] (TENS) unit or [https://www.physio-pedia.com/Interferential_Therapy interferential unit]. | |||
* Incisional pain can be expected to decrease gradually over 6 to 8 weeks. | |||
==== Strength and Reconditioning ==== | |||
* Co-contraction of the TA, multifidus, and pelvic floor muscles with and without using pressure biofeedback (BFB). See [[Spinal Stabilization|lumbar stabilisation]] | |||
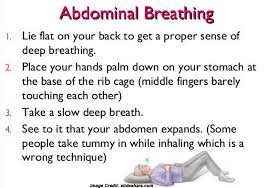
* Abdominal breathing | |||
[[File:Abdominal breathing.jpg|thumb|none]] | |||
* Abdominal bracing and supine marching are good exercises to begin strengthening the trunk. Before bracing is initiated, it is best to make sure the patient can isometrically contract the TA, multifidi, and pelvic floor muscles. | |||
* [[File:Abdominal bracing.jpg|thumb|none]] | |||
* Exercises are recommended to be practiced in sitting, standing, and quadruped. | |||
* General strength and conditioning exercises should also be initiated during this phase of rehabilitation after it is cleared by the physician and the patient demonstrates appropriate stabilisation. Examples of exercises would include: | |||
** Wall squats and sit to stand | |||
** Half lunges | |||
** Step ups and step downs | |||
** Walking | |||
* Cardiovascular reconditioning (using stair climber, brisk walking, and pool exercises once the incision is closed) | |||
* Care should be taken when starting more vigorous strengthening activities, because it is recommended that the patient be able to use the appropriate stabilisation muscles during components of the exercise before doing the full exercise. | |||
* Hip flexors stretching should only start after the permission of the surgeon. stretching should be very gentle and only pushed to the point the patient can brace to prevent lumbar motion. | |||
* ''one of the most stressful motions in the lumbar spine is rotation,'' ''which causes a shearing effect across the disc. Since the'' ''thoracic spine is designed to allow more rotation, limited'' ''motion here may increase strain on the lumbar spine during'' ''twisting motions.'' The PT can use manual mobilization techniques to increase thoracic spine mobility | |||
* Examples of other exercises (performed while bracing) initiated in the later stages of phase II include the following: | |||
** Bridging | |||
** Heel lifts | |||
** Superman (avoiding lumbar extension) | |||
** Lateral pulls (light resistance with approval of surgeon) | |||
** Seated upright rowing machine | |||
** Scapular depression (avoid resisting more than 40% of body weight) | |||
** Push-ups standing and leaning into the wall | |||
** Stair climber | |||
** Upper body ergometer (UBE) | |||
* What the therapist is attempting to develop at this stage is not so much muscle power as kinesthetic sense for the muscles and their role in protecting the spine. Therefore the proper form of each exercise should be emphasised. | |||
==== Scar and soft tissue mobility ==== | |||
Through soft tissue mobilisation techniques.<ref name=":0" /> | |||
===Phase III=== | |||
* 11 to 19 weeks after surgery | |||
==== Goals ==== | |||
* Return to work | |||
* continue to advance/progress exercise program, | |||
* practice specific skills program, | |||
* initiate resistance training program | |||
* They often return to work with modified duties or on a part-time schedule. | |||
* patient should be independent with self-care duties and also with a moderately challenging home exercise program. | |||
* More strenuous stabilisation activities, such as half and full front and side planks could be added. | |||
* The previous trunk stabilisation activities should be progressed within the patient tolerance with modifications according to the patient's condition. | |||
* It is not advised to do complex weight lifting tasks, but to focus on light free weight activity and machine based exercises that allow the patient to perform them with proper posture, technique, and bracing. | |||
* '''Patients should be extremely careful with overhead lifting because of the axial load and compressive forces placed on the spine.''' | |||
* Endurance and cardiovascular exercises should also be progressed at this stage and start to progress gradually. | |||
* For some individuals it may be advised to do more cardiovascular or resisted exercises in an aquatic rehabilitation environment. | |||
* At this stage the expectation is that pain continues to decrease and be at a minimal level. However, if pain persists and the surgeon reported absence of physical explanation, then the therapist should reinforce the functional improvements and minimise the importance of pain as a marker of improvement.<ref name=":0" /> | |||
===Phase IV=== | |||
* 20 weeks to 1 year after surgery | |||
==== Goals ==== | |||
* Restore pre-injury status | |||
* Continue home program of conditioning and stabilisation | |||
* Patients should be progressing to full restoration of their pre-injury level of function and be independent with conducting their previous home and gym program. | |||
* They should have a good grasp of not only the exercises and physical activity required to reach their goals but also ways to modify those activities. | |||
* Patients with fusions frequently develop problems at the level above or below the fusion. For these reasons, the patient should learn that spinal care is now a lifetime habit and must be maintained with regular exercise and good mechanics during all daily activities. | |||
* Later in this phase (and with clearance from the surgeon) they may begin agility and sport-specific drills, such as running, cutting, and jumping. If a more comprehensive weight training program is called for it should be again geared to the specific activity faced by the patient<ref name=":0" /> | |||
==Useful links:== | |||
[[Core Stability|Core stability]] | |||
[[Exercises for Lumbar Instability|Exercises for Lumbar Instability]] | |||
==References:== | |||
Latest revision as of 11:56, 24 April 2024
Top Contributors - Mariam Hashem, Kim Jackson, Admin, Rachael Lowe, Lucinda hampton, Chelsea Mclene and Candace Goh
Introduction[edit | edit source]
Lumbar Spine Fusion is an effective treatment option to stabilise the painful motion segment, and may provide indirect decompression of the neural elements, restore lordosis and correct deformity[1].
The surgery involves placement of an implant (cage, spacer or structural graft) within the intervertebral space after discectomy[1] and successful union of two or more vertebra[2].
Indications[edit | edit source]
- Discogenic/facetogenic low back pain[1].
- Post traumatic cases of segmental instability or potential neurologic injury[1].
- Degenerative spinal pathology with failure of conservative treatment[2].
- Neurogenic claudication[1].
- Radiculopathy due to foraminal stenosis[1].
- Lumbar degenerative spinal deformity including symptomatic spondylolisthesis and degenerative scoliosis[1].
Degenerative cascade[edit | edit source]
Diagnosis[edit | edit source]
- Confirmatory diagnostic testing often includes MRI scanning and discography for equivocal cases.[2]
- Spinal radiographs showing:
- Osteophytes and segmental disc space narrowing in patients with degenerative spondylosis.
- A defect in the pars interarticularis.
- Anterolisthesis, or a forward slippage of one vertebra on the next, is the hallmark radiographic finding in spondylolisthesis.
- Flexion and extension films can help to detect hypermobility or excessive motion in degenerative lumbar conditions.
Lumbar Fusion Approaches[edit | edit source]
Today, most spine surgeons use pedicle screw constructs to immobilise the vertebrae rigidly while preserving the normal lumbar lordosis.[3]
Posterolateral Lumbar Fusion[edit | edit source]
A midline posterior incision, with a laminectomy if necessary.
Transverse process, pars interarticularis, and if needed, the sacral alae are decorticated (posterior fusion). then a bone graft is placed on the decorticated surfaces.
Pedicle screws and rods or plates may be placed to immobilise the motion segments rigidly and augment the formation of a solid union.
In routine cases of posterolateral fusions the disc is not radically resected. Biomechanical studies have shown that people bear load through the middle and posterior thirds of the disc. Several reports describe a persistently painful disc under a solid posterior fusion.[4]
Interbody Fusion[edit | edit source]
- A-posterior lumbar fusion (PLIF): associated with a higher incidence of postsurgical nerve injuries.
- B- Transformational Lumbar Interbody Fusion
- C-Anterior Lumbar Interbody Fusion
- D-Lateral Interbody Fusion: nerve stretch injury reported, with L4 nerve root injury most common.[5]
- E-Interbody Cages: hollow cylinders made of titanium, carbon ,or bone filled with autogenous bone graft or a bone graft substitute and inserted between the vertebral bodies.[2]
Rehabilitation[edit | edit source]
Preoperative phase:[edit | edit source]
This is the proper timing for assessing functional outcomes and psychological support. This is possible through patient education, which includes:
- Stabilisation-based exercises
- Postoperative precautions
- Bed mobility and transfers
- Initial postoperative exercises
- Gait training with any necessary assistive devices
- Donning and doffing any required braces
- Wound care
- General overview and prognosis of the postoperative rehabilitation process
A tour of the facility and operating room along with meeting with individuals who have already undergone such a procedure may also help to decrease patient anxiety surrounding the surgery and hospital experience.[6]
Therapist must have a complete picture about the procedure, surgical approach and fused levels.
Note: During a posterior fusion, the multifidi are retracted from the spine. This partially tears the dorsal divisions of the spinal nerves, resulting in partial denervation of the multifidi. If an anterior fusion also has been performed, then a midline skin incision will be apparent and the abdominal muscular incision is lateral. The incision passes through the obliques, also partially denervating them. For this reason the therapist should teach the patient the proper way to recruit the transverse abdominis (TA), multifidi, and pelvic floor muscles and watch for any substitution patterns to promote proper spinal stabilisation.[2]
- ROM
- Posture
- Balance
- Gait
- Strength
- Body mechanics
- Specific functional tasks
- Specific Neurological examination
- The evaluation shouldn't include Lumbar ROM or hip flexor mobility especially at first stages of rehabilitation.[2]
Phase I:[edit | edit source]
- 1 to 5 days after surgery (inpatient) and up to 6 Weeks
- Most patients are referred for physiotherapy anywhere between 4 to 7 weeks after their discharge from the hospital.
- Physical therapy management during this phase consists of teaching patients the proper way to get in and out of bed, dress and perform other self-care activities, and walk (perhaps with a walker for the first 1 or 2 days).
- Light TA and pelvic floor contractions to begin to practice them in different positions.
- The therapist also can teach basic and simple neural mobilisation for the nerves involving the lumbosacral plexus.
- Patients and their family should leave the hospital with an understanding of the home care required until they begin their outpatient physical therapy.[2]
Phase II:[edit | edit source]
- 6 to 10 weeks after surgery
- Patients should begin to approximate normal activities while the therapist controls
- Patients should be slowly working up to 30 minutes of exercise and physical activity at least 5 days a week.
- They can begin a light weight-training program, avoiding exercises that inappropriately load the lumbar spine but making sure to include some exercise for the lumbar paraspinals and other muscles that attach to the thoracodorsal fascia.[2]
- Common restrictions are no lifting greater than 10lb. and no overhead lifting.[7]
Goals[edit | edit source]
- Achieve good body mechanics during ADL
- Protect the surgical site from infection and mechanical stress
- Nerve root mobility at the involved levels
- Control pain and inflammation
- Begin a stabilisation and reconditioning program
- Improve scar and surrounding soft tissue mobility
- Treat restrictions of thoracic, UEs, and LEs that can lead to more strain on the lumbar spine[2]
Body mechanics education[edit | edit source]
- Ved mobility
- Pushing and pulling
- Lifting and carrying
- Hip hinge technique
See Injury Prevention and Body Mechanics
Nerve root gliding techniques[edit | edit source]
Patients should extend the knee while lying supine with the spine in a neutral position and the hip flexed to a 90° angle. When tension is encountered, the therapist helps the patient work the knee or ankle gently back and forth, gradually increasing the ROM. This stretch may cause increased symptoms during the stretch, which should resolve immediately on relaxing.
Pain management[edit | edit source]
- Prescribed medications and ice.
- Ultrasound shouldn't be applied over a healing bony fusion.
- Patients with severe pain problems can try using a home transcutaneous electrical nerve stimulation (TENS) unit or interferential unit.
- Incisional pain can be expected to decrease gradually over 6 to 8 weeks.
Strength and Reconditioning[edit | edit source]
- Co-contraction of the TA, multifidus, and pelvic floor muscles with and without using pressure biofeedback (BFB). See lumbar stabilisation
- Abdominal breathing
- Abdominal bracing and supine marching are good exercises to begin strengthening the trunk. Before bracing is initiated, it is best to make sure the patient can isometrically contract the TA, multifidi, and pelvic floor muscles.
- Exercises are recommended to be practiced in sitting, standing, and quadruped.
- General strength and conditioning exercises should also be initiated during this phase of rehabilitation after it is cleared by the physician and the patient demonstrates appropriate stabilisation. Examples of exercises would include:
- Wall squats and sit to stand
- Half lunges
- Step ups and step downs
- Walking
- Cardiovascular reconditioning (using stair climber, brisk walking, and pool exercises once the incision is closed)
- Care should be taken when starting more vigorous strengthening activities, because it is recommended that the patient be able to use the appropriate stabilisation muscles during components of the exercise before doing the full exercise.
- Hip flexors stretching should only start after the permission of the surgeon. stretching should be very gentle and only pushed to the point the patient can brace to prevent lumbar motion.
- one of the most stressful motions in the lumbar spine is rotation, which causes a shearing effect across the disc. Since the thoracic spine is designed to allow more rotation, limited motion here may increase strain on the lumbar spine during twisting motions. The PT can use manual mobilization techniques to increase thoracic spine mobility
- Examples of other exercises (performed while bracing) initiated in the later stages of phase II include the following:
- Bridging
- Heel lifts
- Superman (avoiding lumbar extension)
- Lateral pulls (light resistance with approval of surgeon)
- Seated upright rowing machine
- Scapular depression (avoid resisting more than 40% of body weight)
- Push-ups standing and leaning into the wall
- Stair climber
- Upper body ergometer (UBE)
- What the therapist is attempting to develop at this stage is not so much muscle power as kinesthetic sense for the muscles and their role in protecting the spine. Therefore the proper form of each exercise should be emphasised.
Scar and soft tissue mobility[edit | edit source]
Through soft tissue mobilisation techniques.[2]
Phase III[edit | edit source]
- 11 to 19 weeks after surgery
Goals[edit | edit source]
- Return to work
- continue to advance/progress exercise program,
- practice specific skills program,
- initiate resistance training program
- They often return to work with modified duties or on a part-time schedule.
- patient should be independent with self-care duties and also with a moderately challenging home exercise program.
- More strenuous stabilisation activities, such as half and full front and side planks could be added.
- The previous trunk stabilisation activities should be progressed within the patient tolerance with modifications according to the patient's condition.
- It is not advised to do complex weight lifting tasks, but to focus on light free weight activity and machine based exercises that allow the patient to perform them with proper posture, technique, and bracing.
- Patients should be extremely careful with overhead lifting because of the axial load and compressive forces placed on the spine.
- Endurance and cardiovascular exercises should also be progressed at this stage and start to progress gradually.
- For some individuals it may be advised to do more cardiovascular or resisted exercises in an aquatic rehabilitation environment.
- At this stage the expectation is that pain continues to decrease and be at a minimal level. However, if pain persists and the surgeon reported absence of physical explanation, then the therapist should reinforce the functional improvements and minimise the importance of pain as a marker of improvement.[2]
Phase IV[edit | edit source]
- 20 weeks to 1 year after surgery
Goals[edit | edit source]
- Restore pre-injury status
- Continue home program of conditioning and stabilisation
- Patients should be progressing to full restoration of their pre-injury level of function and be independent with conducting their previous home and gym program.
- They should have a good grasp of not only the exercises and physical activity required to reach their goals but also ways to modify those activities.
- Patients with fusions frequently develop problems at the level above or below the fusion. For these reasons, the patient should learn that spinal care is now a lifetime habit and must be maintained with regular exercise and good mechanics during all daily activities.
- Later in this phase (and with clearance from the surgeon) they may begin agility and sport-specific drills, such as running, cutting, and jumping. If a more comprehensive weight training program is called for it should be again geared to the specific activity faced by the patient[2]
Useful links:[edit | edit source]
Exercises for Lumbar Instability
References:[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Mobbs, R. J., Phan, K., Malham, G., Seex, K., & Rao, P. J. (2015). Lumbar interbody fusion : techniques , indications and comparison of interbody fusion options including PLIF , TLIF , MI-TLIF , OLIF / ATP , LLIF and ALIF, 3(1), 2–18. https://doi.org/10.3978/j.issn.2414-469X.2015.10.05
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 Maxey, L. and Magnusson, J. (n.d.). Rehabilitation for the postsurgical orthopedic patient.
- ↑ Burkus K, et al: Six-year outcomes of anterior lumbar interbody arthrodesis with use of interbody fusion cages and recombinant human bone morphogenic protein-2. J Bone Joint Surg 91:1181-1189, 2009.
- ↑ Ibrahim T, et al: Surgical versus non-surgical treatment of chronic low back pain: A meta-analysis of randomized trials. Int Orthop 32(7):107-113, 2006.
- ↑ Knight RQ, et al: Direct lateral lumbar interbody fusion for degenerative conditions: Early complication profile. J Spinal Disord Tech 22(1):34-37, 2009.
- ↑ Kisner C, Colby LA: Therapeutic exercise: Foundations and techniques, ed 5, Philadelphia, 2007, FA Davis.
- ↑ Thompson WR, editor: ACSM’s guidelines for exercise testing and prescription, ed 8, American College of Sports Medicine, Baltimore, 2004, Lippincott Williams & Wilkins.