Groin Strain: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (285 intermediate revisions by 16 users not shown) | |||
| Line 1: | Line 1: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | <div class="editorbox"> | ||
</div> | '''Original Editor '''- [[User:Els Van Haver|Els Van Haver]]as part of the [[Vrije Universiteit Brussel Evidence-based Practice Project|Vrije Universiteit Brussel's Evidence-based Practice project]] | ||
== | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | |||
== Definition/Description == | |||
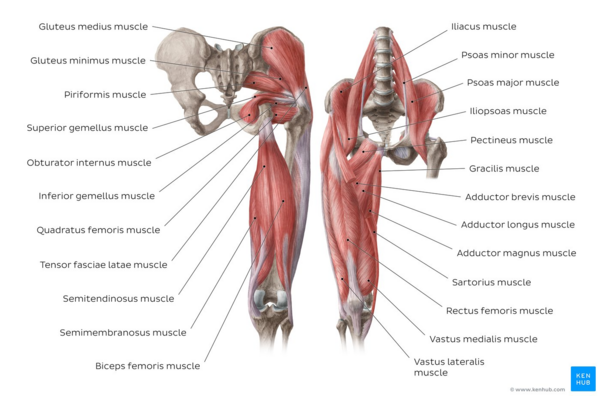
[[File:Muscles of the hip and thigh - Kenhub.png|alt=Overview of the muscles of the hip and thigh - anterior and posterior views|right|frameless|600x600px|Overview of the muscles of the hip and thigh - anterior and posterior views]] | |||
Groin [[Muscle Strain|strain]] is an injury to the muscle-tendon unit that produces pain on palpation of the adductor tendons or its insertion on the pubic bone and pain in the adductor region on resistance testing of the adductors.<ref name=":2">Weir A, Brukner P, Delahunt E, Ekstrand J, Griffin D, Khan KM, Lovell G, Meyers WC, Muschaweck U, Orchard J, Paajanen H. [https://bjsm.bmj.com/content/49/12/768.short Doha agreement meeting on terminology and definitions in groin pain in athletes. British journal of sports medicine]. 2015 Jun 1;49(12):768-74.</ref> Groin muscle strains are encountered more frequently in ice hockey and soccer.<ref name=":3">Orchard JW. [https://bjsm.bmj.com/content/49/12/798.short Men at higher risk of groin injuries in elite team sports: a systematic review]. British journal of sports medicine. 2015 Jun 1;49(12):798-802.</ref> | |||
'' | These sports require a strong eccentric contraction of the adductor musculature during competition and practice.<ref name="'Tyler'">Tyler TF, Fukunaga T, Gellert J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4223288/ Rehabilitation of soft tissue injuries of the hip and pelvis.] International journal of sports physical therapy 2014;9(6):785.</ref> The underlying injury is most often a muscle or tendon strain at the insertion of the tendon of the adductor muscle to the bone.<ref name="'Gino'">Kerkhoffs GM, Servien E, editors. [https://link.springer.com/book/10.1007%2F978-3-319-03722-6 Acute muscle injuries.] Springer International Publishing; 2014.</ref> The [[Adductor Longus|adductor longus]] is most commonly injured.<ref name=":4">Kiel J, Kaiser K. [https://europepmc.org/article/NBK/NBK493166 Adductor Strain.] StatPearls Publishing, Treasure Island; 2018.</ref> | ||
The difference between groin tendinopathy and strain are: | |||
*First of all, strains are acute and tendinosis is chronic. Tendinosis is a repetitive strain. | |||
*The second difference is that acute injuries are more often localized in the myotendon junctions and chronic injuries are localized at the tendinous insertions on the [[Pubis|pubic bone]]. | |||
See page for [[Adductor Tendinitis|adductor tendinitis]]. | |||
Image: Overview of the muscles of the hip and thigh - anterior and posterior views.<ref > Overview of the muscles of the hip and thigh - anterior and posterior views image - © Kenhub https://www.kenhub.com/en/library/anatomy/hip-and-thigh-muscles</ref> | |||
== Clinically Relevant Anatomy == | |||
In human anatomy, the groin is the junctional area between the abdomen and the thigh on either side of the pubic bone. This is also known as the medial compartment of the thigh. | |||
{{#ev:youtube|watch?v=MjPAPTJdxa8|200}}<ref>AnatomyZone Muscles of the Thigh Part 2 - Medial Compartment - Anatomy Tutorial | |||
Available from https://www.youtube.com/watch?time_continue=10&v=MjPAPTJdxa8</ref> | |||
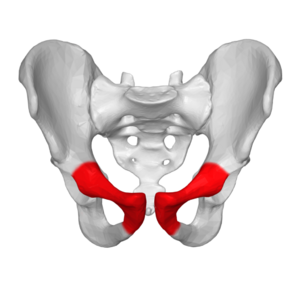
[[File:Pubic anterior view.png|right|frameless]] | |||
The groin muscles consist of three large groups of muscles that can be injured: the [[Abdominal Muscles|abdominal]], [[iliopsoas]] and the [[Hip Adductors|adductor muscle group.]] | |||
Image: Anterior view pelvis, pubic bone in red | |||
* The adductor muscle group: The adductors of the hip joint include 6 muscles: the [[Adductor Longus|adductor longus]], [[Adductor Magnus|magnus]] and [[Adductor Brevis|brevis]], [[gracilis]], [[Obturator Externus|obturator externus]], and [[Pectinus Muscle|pectineus]]. All these are innervated by the [[Obturator Nerve|obturator nerve]] except that of [[Pectinus Muscle|pectineus]], which receives innervation from the [[Femoral Nerve|femoral nerve]]. The adductors all originate on the [[Pubis|pubic]] ramus as almost all insert on the linea aspera of the posterior femur. The posterior head of the [[Adductor Magnus|adductor magnus]] has a proximal attachment on the [[Ischium|ischial]] tuberosity anteroinferiorly and attaches distally on the medial distal femur at the adductor tubercle. The gracilis insertion is on the medial border of the tuberosity of the tibia. The primary function of this muscle group is adduction of the thigh in open-chain motions and stabilization of the lower extremity and pelvis in closed chain motion. | |||
In football, the majority of groin injuries are adductor related. <ref>Hölmich P, Thorborg K, Dehlendorff C, Krogsgaard K, Gluud C. [https://bjsm.bmj.com/content/48/16/1245.short Incidence and clinical presentation of groin injuries in sub-elite male soccer.] British journal of sports medicine. 2014 Aug 1;48(16):1245-50.</ref> The proximal attachment of the [[Adductor Longus|adductor longus]] contributes to an anatomical pathway across the anterior pubic symphysis that is likely required to withstand the transmission of large forces during multidirectional athletic activities. Its lack of mechanical advantage may make it more susceptible to strain.<ref name="'Norton-old'">Norton‐old KJ, Schache AG, Barker PJ, Clark RA, Harrison SM, Briggs CA. [https://d1wqtxts1xzle7.cloudfront.net/49700088/ca.2211620161018-8888-1l38i3h.pdf?1476835149=&response-content-disposition=inline%3B+filename%3DAnatomical_and_mechanical_relationship_b.pdf&Expires=1595263708&Signature=fAsRGkdBhCibLIz1y4BG8~wxqpBlOwVCviQxiz Anatomical and mechanical relationship between the proximal attachment of adductor longus and the distal rectus sheath.] Clinical Anatomy 2013;26(4):522-30.</ref> | |||
*The abdominal group: The abdominal musculature comprise the [[Rectus Abdominis|rectus abdominis]], the [[Internal Abdominal Oblique|obliques internus]] and [[External Abdominal Oblique|externus abdominis]]. (See page for [[Abdominal Muscles|abdominal muscles]]). | |||
*The iliopsoas group: The iliopsoas, comprised of [[iliacus]] and [[Psoas Major|psoas major]] muscles, is the only muscle directly connecting the spine and the lower limb. (See page for [[Hip Anatomy|hip anatomy]]).<ref name="'Tyler'" /> | |||
== Epidemiology /Etiology == | |||
< | Groin strains are common amongst athletes who compete in sports that involve repetitive twisting, turning, sprinting and kicking such as football, ice hockey, Australian and Gaelic football.<ref name=":3" /> Groin injuries are reported more in males compared to female football athletes. Injuries in men accounted for 4–19% of all injuries and 2–14% in women.<ref>Waldén M, Hägglund M, Ekstrand J. [https://bjsm.bmj.com/content/49/12/792.short The epidemiology of groin injury in senior football: a systematic review of prospective studies.] British journal of sports medicine. 2015 Jun 1;49(12):792-7.</ref> | ||
= | The exact incidence of groin muscle strains in most sports is unknown because athletes often play through minor groin pain and the injury goes unreported. In addition, overlapping diagnoses can skew the incidence.<ref name="'Tyler, T.'" /> Cumulative or single injury seem to be important etiological factors. Chronic tendinitis of the adductor muscles/tendons, especially that of the [[Adductor Longus|adductor longus]], is the most frequently diagnosed.<ref name=":4" /> | ||
The injury mechanism can be divided into 3 groups: | |||
# Direct blunt trauma: An acute injury, typically a direct injury to the soft tissues resulting in muscle hematoma. | |||
# Forceful contraction: The most common groin injury in athletes is muscle and tendon strain of the adductor muscle group. Change of direction and kicking has been described as the main actions resulting in [[Adductor Longus|adductor longus]] injury. Videos analysis of acute [[Adductor Longus|adductor longus]] <ref>Serner A, Mosler AB, Tol JL, Bahr R, Weir A. [https://bjsm.bmj.com/content/53/3/158.abstract Mechanisms of acute adductor longus injuries in male football players: a systematic visual video analysis]. British journal of sports medicine. 2019 Feb 1;53(3):158-64.</ref> injuries in 17 professional male football players showed most injuries occurred in non-contact situations, following a quick reaction to a change in play. Injury actions were: change of direction, kicking, reaching/stretching and jumping. The injury may also occur during a forceful concentric contraction of the muscle.<ref name="'Mc'" /> Lower-extremity athletes such as ice hockey and soccer players are naturally more prone to this pathology due to the repetitive twisting, turning, sprinting and kicking.<ref name=":3" /> | |||
# Microtrauma by repetitive injury: musculotendinous injuries to the groin are mainly a consequence of cumulative microtraumas (overuse trauma, repeated minor injuries) leading to chronic groin pain. | |||
== Characteristics/Clinical Presentation == | |||
The main sign of groin strain is intense pain in the groin area. [[Muscle Strain|Muscle strain]] injuries often arise from excessive stretching or stretching when the muscle is being activated. When there is a strain in the muscle, the damage is often localized near the muscle-tendon junction. Acute adductor longus injuries may also involve tendinous rupture/ avulsion, primarily at the proximal insertions. <ref>Serner A, Weir A, Tol JL, Thorborg K, Roemer F, Guermazi A, Yamashiro E, Hölmich P. [https://onlinelibrary.wiley.com/doi/abs/10.1111/sms.12936 Characteristics of acute groin injuries in the adductor muscles: a detailed MRI study in athletes]. Scandinavian journal of medicine & science in sports. 2018 Feb;28(2):667-76.</ref> | |||
Clinically for an adductor strain, the patient presents with pain in the inner thigh and tenderness along the muscle belly, tendon or insertion. The pain is exacerbated by adduction.<ref name=":11">Thorborg K, Reiman MP, Weir A, Kemp JL, Serner A, Mosler AB, Hölmich P. [https://www.jospt.org/doi/full/10.2519/jospt.2018.7850 Clinical examination, diagnostic imaging, and testing of athletes with groin pain: an evidence-based approach to effective management]. journal of orthopaedic & sports physical therapy. 2018 Apr;48(4):239-49.</ref> Tears frequently occur at the myotendinous junction, which is the weakest part of the muscle-tendon unit but is also commonly seen in the muscle belly. The same mechanism of injury that results in a muscle tear in an adult may cause an apophyseal avulsion in an adolescent. There is a well-established clinical grading system for muscle tears, which has 3 components:<ref>Davies AG, Clarke AW, Gilmore J, Wotherspoon M, Connell DA. [https://link.springer.com/article/10.1007/s00256-009-0768-9 imaging of groin pain in the athlete. Skeletal radiology]. 2010 Jul;39(7):629-44.</ref> | |||
* Grade 1: no loss of function or strength. Muscle tears can show normal appearances or a small area of focal disruption (<5% of the muscle volume), with hematoma and perifascial fluid relatively common on imaging with US and MRI. | |||
* Grade 2: severe, with some weakness. Injury corresponds to a partial tear, with muscle fibre disruption seen (>5% of the muscle volume) but not affecting the whole muscle belly. In '''acute''' grade 1 or 2 strains of the adductor muscle, there is intense pain in the groin area, like a sudden stab with a knife, if the athlete attempts to continue the activity. Locally a haemorrhage and swelling can be seen a few days after the injury. A typical trauma history, localized tenderness and difficulties to contract the hip abductors. | |||
* Grade 3: complete muscle tear and complete functional loss. Injuries are complete muscle tears with frayed margins and bunching and/or retraction of the torn muscle fibres.<span class="reference" id="cite_ref-.27Mc.27_11-1"></span> Complete muscle tears or grade 3 strains are most often found in the distal musculotendinous junction located toward the insertion on the femur. | |||
== Differential Diagnosis == | |||
Traditionally, groin pain has been thought to be complex with various definitions and terminologies without any diagnostic criteria.<ref>Hölmich P. [https://pubmed.ncbi.nlm.nih.gov/17261557/ Long-standing groin pain in sportspeople falls into three primary patterns, a “clinical entity” approach: a prospective study of 207 patients]. British journal of sports medicine. 2007 Apr 1;41(4):247-52.</ref> In a systematic review on the treatment of groin pain in athletes, more than 30 different diagnostic terminologies were used to describe groin pain which adds up to the complexity of groin injuries in athletes.<ref>Serner A, van Eijck CH, Beumer BR, Hölmich P, Weir A, de Vos RJ. [https://pubmed.ncbi.nlm.nih.gov/25633830/ Study quality on groin injury management remains low: a systematic review on treatment of groin pain in athletes. British journal of sports medicine]. 2015 Jun 1;49(12):813-.</ref> | |||
In the attempt to address the different terminologies and definitions used, a consensus meeting was held in Doha, Qatar during the first World Conference of Grain Pain in Athletes , in November 2014. A group of 24 experts from 14 different countries was invited to agree on a standard terminology, along with accompanying definitions. <ref name=":2" /> | |||
A classification system of groin pain was described in three main subheading during the Doha agreement meeting; | |||
{| class="wikitable" | |||
|+The Doha agreement diagnostic classification <ref name=":2" /> | |||
!'''Defined Entities.''' | |||
!'''Other musculoskeletal causes.''' | |||
!'''Not to be missed.''' | |||
|- | |||
| | |||
* Adductor-related groin pain | |||
* Iliopsoas-related groin pain | |||
* Inguinal-related groin pain | |||
* Pubic-related groin pain | |||
* Hip-related groin pain | |||
| | |||
# Inguinal or femoral hernia | |||
# Posthernioplasty pain | |||
# Nerve entrapment | |||
#* Obturator | |||
#* Ilioinguinal | |||
#* Genitofemoral | |||
#* Iliohypogastric | |||
# referred pain | |||
#* Lumbar spine | |||
#* Sacroiliac joint | |||
# Apophysitis or avulsion fracture | |||
#* Anterior superior iliac spine | |||
#* Anterior inferior iliac spine | |||
#* Pubic bone | |||
# Referred pain | |||
| | |||
Stress fracture | |||
* Neck of femur | |||
* Pubic ramus | |||
* Acetabulum | |||
[[Hip Anatomy|Hip joint]] | |||
* Slipped capital femoral epiphysis (adolescents) | |||
* Perthes’ disease (children and adolescents) | |||
* Avascular necrosis/transient osteoporosis of the head of the femur | |||
* Arthritis of the hip joint (reactive or infectious) | |||
Inguinal lymphadenopathy Intra-abdominal abnormality | |||
* Prostatitis | |||
* Urinary tract infections | |||
* Kidney stone | |||
* Appendicitis | |||
* Diverticulitis | |||
Gynaecological conditions Spondyloarthropathies | |||
* Ankylosing spondylitis Tumours | |||
* Testicular tumours | |||
* Bone tumours | |||
* Prostate cancer | |||
* Urinary tract cancer ▸ Digestive tract cancer ▸ Soft tissue tumours | |||
|} | |||
== Diagnostic Procedures == | |||
< | First of all, there needs to be a patient history and an identification of the pain by the examination of the physiotherapist. On evaluation, there is tenderness to palpation with focal swelling of the adductors and decreased adductor strength and pain with resisted adduction. The diagnosis can be made with focal findings on examination using the guidelines from the Doha agreement classification system without the need for imaging. <ref name=":2" /><ref>Branci S, Thorborg K, Nielsen MB, Hölmich P. [https://bjsm.bmj.com/content/47/10/611.short Radiological findings in symphyseal and adductor-related groin pain in athletes: a critical review of the literature.] British journal of sports medicine. 2013 Jul 1;47(10):611-9.</ref> However, imaging can be useful to rule out or in differential diagnosis after a comprehensive clinical examination. Abnormal radiological findings around the pubic symphysis such as pubic bone marrow oedema are common in athletes with adductor and pubic-related pain. These radiological findings are also common in asymptomatic athletes. Radiological findings alone should not be used in making diagnostic decisions as morphology does not necessarily mean pathology. <ref>Branci S, Thorborg K, Bech BH, Boesen M, Nielsen MB, Hölmich P. [https://bjsm.bmj.com/content/49/10/681.short MRI findings in soccer players with long-standing adductor-related groin pain and asymptomatic controls]. British journal of sports medicine. 2015 May</ref> | ||
== Outcome Measures == | == Outcome Measures == | ||
The [[Copenhagen Hip and Groin Outcome Score (HAGOS)|Copenhagen hip and groin outcome score]] (HAGOS)<ref>Thorborg K, Hölmich P, Christensen R, Petersen J, Roos EM. T[https://bjsm.bmj.com/content/45/6/478.short he Copenhagen Hip and Groin Outcome Score (HAGOS): development and validation according to the COSMIN checklist]. British journal of sports medicine. 2011 May 1;45(6):478-91.</ref> | |||
The | |||
== Examination == | == Examination == | ||
Bilateral evaluation of adductor muscle and strength: palpation at the adductor insertion at the pubic bone, adduction against resistance ([[Adductor Squeeze Test|squeeze tests]] in 0° and 45°), and passive stretching of the adductor muscles.<ref name=":11" /> | |||
{{#ev:youtube|https://www.youtube.com/watch?v=mg_f_sIu05U|200}} | |||
< | A complete clinical examination should be performed for every patient with groin pain. The injured athlete should first be examined by inspection in a standing position to evaluate the alignment of extremities. The patient should then be asked to lie in a supine position to be able to check the motion of the [[Hip Anatomy|hip joint]] and the flexibility of the groin and hip muscles. The diagnosis classification system provided by the Doha agreement should be used as a guideline to all groin injuries. <ref name=":2" /> | ||
=== Squeeze Test === | |||
{{#ev:youtube|https://www.youtube.com/watch?v=GwxrgZ_XgOU|200}}<ref>Wichita, groin squeeze test. Access from https://www.youtube.com/watch?v=GwxrgZ_XgOU</ref> | |||
# If adductor longus muscle is injured pain will be elucidated to the injured area by resisting leg adduction and in passive stretching at full abduction of the hip. Tenderness on palpation is localized to the injury site at the origin of the adductor longus tendon or at the musculotendinous junction.<ref name=":2" /> | |||
# Evaluation of iliopsoas muscle-related pain, strength and flexibility: palpation above the inguinal ligament, isometric strength test in hip flexion and a modified Thomas test.<ref name=":5">Hölmich P. [http://old.ortopaedi.dk/fileadmin/phd/Per_Holmich_56974.pdf Groin injuries in athletes—development of clinical entities, treatment, and prevention.] Dan Med J. 2015 Dec 1;62(12):B5184.</ref> ''[[Thomas Test]]'' | |||
# Abdominal muscle-related pain and strength: palpation of the abdominal muscle insertion at the pubic bone and a functional sit-up test and symphysis joint tenderness at palpation.<ref name=":5" /> | |||
# The location of the injury was based on a minimum of 1 positive finding on palpation, stretching, or muscle resistance testing.<ref name=":8">Serner A, Tol JL, Jomaah N, Weir A, Whiteley R, Thorborg K, Robinson M, Hölmich P. [https://journals.sagepub.com/doi/abs/10.1177/0363546515585123 Diagnosis of acute groin injuries: a prospective study of 110 athletes]. The American journal of sports medicine. 2015 Aug;43(8):1857-64.</ref> | |||
< | == Medical Management == | ||
Management is non-operative with rest, ice, compression, analgesia and physical therapy. Analgesia includes non-steroidal anti-inflammatory agents which help in reducing pain. <ref>Elattar O, Choi HR, Dills VD, Busconi B. [https://journals.sagepub.com/doi/abs/10.1177/1941738116653711 Groin injuries (athletic pubalgia) and return to play.] Sports health. 2016 Jul;8(4):313-23.</ref>Injection at the [[Adductor Longus|adductor longus]] enthesis is helpful for refractory patients to conservative management. <ref name=":6">Kiel J, Kaiser K. [https://www.ncbi.nlm.nih.gov/books/NBK493166/ Adductor Strain]. 2018</ref> | |||
<br> | Non-operative therapy should be tried for several months and is successful in most instances. However, if symptoms and significant restriction of performance persist after an appropriate conservative management regimen, surgical intervention should be considered. Adductor tenotomy has been suggested as a technique to improve symptoms. <ref>Queiroz RD, Carvalho RT, Queiroz Szeles PR, Janovsky C, Cohen M. [https://www.scielo.br/j/rbort/a/CMqTg3cpszfK3JjtShsgQVG/abstract/?lang=en Return to sport after surgical treatment for pubalgia among professional soccer players]. Revista brasileira de ortopedia. 2014 May;49:233-9.</ref> | ||
< | In a recent systematic review that compared surgical intervention to conservative intervention, there was a quicker return to return to play(RTP) time in athletes who had surgical intervention. However, the varied nature of surgical interventions and lack of quality randomised control trial (RCT) in the meta-analysis makes it impractical to recommend the surgical intervention. <ref>Bastia P, Ghirarduzzi P, Schiavi P, Donelli D, Pedrazzini A, Leigheb M, Ceccarelli F, Pogliacomi F. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7233710/#ref26 Surgical or conservative treatment in ARGP syndrome? A systematic review]. Acta Bio Medica: Atenei Parmensis. 2019;90(Suppl 12):14.</ref> | ||
< | == Prevention == | ||
Subsequent [[Groin Strain|groin strains]] may occur, resulting in a recurrent problem. Hence primary and secondary prevention is equally important. To identify the athlete at risk and possibly correct the predisposing factor(s), the intrinsic and extrinsic risk factors for the injury type must be known.<ref>Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. [https://pubmed.ncbi.nlm.nih.gov/20699426/ Intrinsic risk factors for groin injuries among male soccer players: a prospective cohort study. The American journal of sports medicine]. 2010 Oct;38(10):2051-7.</ref> | |||
< | Previous groin injuries, reduced hip adduction strength, higher level of play and lower levels of sports-specific training are associated with increased risk of new groin injuries.<ref name=":9">Whittaker JL, Small C, Maffey L, Emery CA. [https://bjsm.bmj.com/content/49/12/803.short Risk factors for groin injury in sport: an updated systematic review]. British journal of sports medicine. 2015 Jun 1;49(12):803-9.</ref> Hölmich et al demonstrated that an 8 to 12-week active strengthening program, consisting of progressive resistive adduction and abduction exercises, balance training, abdominal strengthening and skating movements on a slide board, was effective in treating chronic groin strains. Also, coordination exercises (focused on the muscles related to the pelvis), core stability and eccentric exercises are a part of the prevention program.<ref>Hölmich P, Larsen K, Krogsgaard K, Gluud C. [https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1600-0838.2009.00998.x Exercise program for prevention of groin pain in football players: a cluster‐randomized trial]. Scandinavian journal of medicine & science in sports. 2010 Dec;20(6):814-21.</ref> | ||
< | '''Adductor strain injury prevention program'''<ref name="'Tyler, T.'">Tyler TF, Silvers HJ, Gerhardt MB, Nicholas SJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3445110/ Groin injuries in sports medicine.] Sports health 2010;2(3):231-6.</ref> | ||
{| class="wikitable" | |||
| colspan="1" rowspan="1" |Warm-up | |||
| colspan="1" rowspan="1" |Bike | |||
|- | |||
| colspan="1" rowspan="1" | | |||
| colspan="1" rowspan="1" |Adductor stretching | |||
|- | |||
| colspan="1" rowspan="1" | | |||
| colspan="1" rowspan="1" |Sumo squats | |||
|- | |||
| colspan="1" rowspan="1" | | |||
| colspan="1" rowspan="1" |Side lunges | |||
|- | |||
| colspan="1" rowspan="1" | | |||
| colspan="1" rowspan="1" |Kneeling pelvic tilts | |||
|- | |||
| colspan="1" rowspan="1" |Strengthening program | |||
| colspan="1" rowspan="1" |Ball squeezes (legs bent to legs straight) | |||
|- | |||
| colspan="1" rowspan="1" | | |||
| colspan="1" rowspan="1" |Different ball sizes | |||
|- | |||
| colspan="1" rowspan="1" | | |||
| colspan="1" rowspan="1" |Concentric adduction with weight against gravity | |||
|- | |||
| colspan="1" rowspan="1" | | |||
| colspan="1" rowspan="1" |Adduction in standing on a cable column or elastic resistance | |||
|- | |||
| colspan="1" rowspan="1" | | |||
| colspan="1" rowspan="1" |Seated adduction machine | |||
|- | |||
| colspan="1" rowspan="1" | | |||
| colspan="1" rowspan="1" |Standing with involved foot on sliding board moving in the sagittal plane | |||
|- | |||
| colspan="1" rowspan="1" | | |||
| colspan="1" rowspan="1" |Bilateral adduction on sliding board moving in the frontal plane (ie, simultaneous bilateral adduction) | |||
|- | |||
| colspan="1" rowspan="1" | | |||
| colspan="1" rowspan="1" |Unilateral lunges with reciprocal arm movements | |||
|- | |||
| colspan="1" rowspan="1" |Sports-specific training | |||
| colspan="1" rowspan="1" |On ice kneeling adductor pull together | |||
|- | |||
| colspan="1" rowspan="1" | | |||
| colspan="1" rowspan="1" |Standing resisted stride lengths on cable column to simulate skating | |||
|- | |||
| colspan="1" rowspan="1" | | |||
| colspan="1" rowspan="1" |Slide skating | |||
|- | |||
| colspan="1" rowspan="1" | | |||
| colspan="1" rowspan="1" |Cable column crossover pulls | |||
|- | |||
| colspan="1" rowspan="1" |Clinical goal | |||
| colspan="1" rowspan="1" |Adduction strength at least 80% of the abduction strength | |||
|} | |||
'''Copenhagen Adductor Exercise''' | |||
< | In a cluster-randomised controlled trial involving 35 semiprofessional Norwegian football teams, using a simple adductor strengthening exercise ''(Copenhagen Adductor Exercise )'' with three progression levels, three times per week during the preseason (6-8 weeks), and once per week during the competitive season (28 weeks). There was a significant reduction in the risk of groin problems compared to the controlled group who trained as normal during the season. The intervention group was made up of 18 teams, 339 players and the controlled group 17 teams, 313 players. The prevalence of groin problems was measured weekly in both groups during the competitive season using the Oslo Sports Trauma Research Center Overuse Injury Questionnaire. <ref name=":7" /><gallery mode="nolines" widths="500" showfilename="yes"> | ||
File:Copenhagen exx.jpeg | |||
</gallery> | |||
== Physiotherapy Management == | |||
< | The treatment of musculotendinous groin strains are generally conservative. Surgical treatment in acute groin injuries is rarely indicated.<ref name=":6" /> | ||
< | In the treatment of muscle-tendon injuries, immobilization should be limited to as short a period as possible to avoid the harmful effects of immobilization including muscle atrophy and loss of function. Immediate rest after the injury should be used until a diagnosis is secured. | ||
*The primary goal of the treatment program is to minimize the effects of immobilization, regain full range of motion, and restore full muscle strength, endurance and coordination. Therefore, crutches, local cold application, and anti-inflammatory medication are recommended in the initial phase. Muscle exercises can usually be started early, but training should be performed within the limits of pain with careful isometric contractions against resistance. | |||
*After the initial phase, heat is usually valuable, especially when muscle training is started. In general, exercises are performed in a pain-free range of motion and increased pain should not occur after activity. | |||
*As rehabilitation progresses, mild pain can be allowed during exercise, but it should subside immediately after the cessation of training. | |||
*When full range of motion is accomplished, the injured muscle and tendon tolerates higher loads and the goal of rehabilitation should shift towards specific strength training exercises aiming for muscular recovery, increased endurance and a full range of motion. | |||
*The final step is the gradual return to sports activity, which may in some cases take as long as 3 to 6 months.<ref name="'Mc'">McSweeney SE, Naraghi A, Salonen D, Theodoropoulos J, White LM. [https://journals.sagepub.com/doi/abs/10.1016/j.carj.2010.11.001 Hip and groin pain in the professional athlete.] Canadian Association of Radiologists Journal 2012;63(2):87-99.</ref> | |||
< | ===='''Adductor-related groin strain injury program'''==== | ||
Enda et al. (2018) examined the effectiveness of rehabilitation that targeted intersegmental control in patients with groin pain. There was significant improvement in the functional performance and return to play time among athletes with groin pain across the various diagnostic entities.<ref name=":1" /> | |||
< | The intervention consists of three(3) levels, addressing intersegmental control and strength, linear running mechanics and increasing linear running load tolerance and multidirectional mechanics and the transition back to high intensity sprinting.<ref name=":1">King E, Franklyn-Miller A, Richter C, O’Reilly E, Doolan M, Moran K, Strike S, Falvey É. [https://bjsm.bmj.com/content/52/16/1054.abstract Clinical and biomechanical outcomes of rehabilitation targeting intersegmental control in athletic groin pain: prospective cohort of 205 patients]. British journal of sports medicine. 2018 Aug 1;52(16):1054-62.</ref> | ||
< | '''Level 1:''' Intersegmental control and strength | ||
{| class="wikitable" | |||
!'''<small>Streams</small>''' | |||
! | |||
!'''<small>Progressions</small>''' | |||
! | |||
|- | |||
|'''<small>Hip Flexor</small>''' | |||
|<small>Supine</small> | |||
|<small>Standing Supported</small> | |||
|<small>Free Standing.</small> | |||
|- | |||
|'''<small>Lateral Hip Control</small>''' | |||
|<small>Supported Hip Hitched</small> | |||
|<small>Free Standing Hip Hitch</small> | |||
|<small>Step Up</small> | |||
|- | |||
|'''<small>Abdominal</small>''' | |||
|<small>Crook Lying Leg Lift</small> | |||
|<small>Crook lying Alternate Leg Drop</small> | |||
|<small>Pallof Kneeling Split Lunge</small> | |||
|- | |||
|'''<small>Double leg Squat</small>''' | |||
|<small>High Goblet Squat</small> | |||
|<small>Low Goblet Squat</small> | |||
|<small>Front Squat</small> | |||
|- | |||
|'''<small>Lateral Hip Strength</small>''' | |||
|<small>Abduction/External rotation in mini squat</small> | |||
|<small>Abduction/External rotation in a mini squat at wall</small> | |||
|<small>Banded Squat</small> | |||
|- | |||
|'''<small>Deadlift</small>''' | |||
|<small>Hip Hinge</small> | |||
|<small>1/2 Rack Deadlift</small> | |||
|<small>Floor Deadlift</small> | |||
|- | |||
|'''<small>Lunge</small>''' | |||
|Split Lunge | |||
|Overhead Split Lunge | |||
|Weighted Split Lunge | |||
|- | |||
|'''<small>Plyometric</small>''' | |||
|On Spot Hopping | |||
|Line Hopping | |||
|Cone Hopping | |||
|} | |||
'''Level 2:''' Linear running mechanics | |||
{| class="wikitable" | |||
!'''<small>Linear</small>''' | |||
!'''<small>Instructions</small>''' | |||
|- | |||
|'''<small>Marching and skipping</small>''' | |||
|<small>March skip on the spot with arms overhead, maintaining lumbopelvic and neutral and with aggressive ground contact</small> | |||
|- | |||
|'''<small>Barbell/Overhead Running</small>''' | |||
|<small>Run with dowel overhead or barbell across shoulders focusing on tall running posture and keeping stick still</small> | |||
|- | |||
|'''<small>Leg change drill</small>''' | |||
|<small>In single leg stand, focus on rapid leg change to drive alternating leg extension and swing leg recovery.</small> | |||
|- | |||
| | |||
|<small>Complete 5-6reps of 3-4sets. Focus entirely on the quality of execution</small> | |||
|} | |||
< | '''level 3:''' Multidirectional mechanics and transitions | ||
{| class="wikitable" | |||
!'''<small>Linear</small>''' | |||
!'''<small>Instructions</small>''' | |||
|- | |||
|'''<small>Lateral shuffle</small>''' | |||
|<small>Side shuffle between 2 cones 8 meters apart arms locked overhead focusing on getting away from cones as quickly as possible. Progress to race to instruction or shadow opponent while shuffling</small> | |||
|- | |||
|'''<small>Zig-Zag cutting</small>''' | |||
|<small>5 cones in zig zag formation, 5 meters apart from each other. Run and cut as quickly as possible around the cones. Add holding a med ball for increased resistance and higher centre of mass. (CoM)</small> | |||
|- | |||
|'''<small>180-degree cone cutting.</small>''' | |||
|<small>5 cones in a semi-circle, start in the middle and run at any cone and cut back straight to the starting point. Add holding a med ball for increased resistance and CoM.</small> | |||
|- | |||
| | |||
|<small>Complete 3-4sets of 5-6reps. Focus entirely on the quality of execution</small> | |||
|} | |||
The patient progresses to level 2 once they have a negative crossover sign and from level 2 to level 3 when they have a symmetrical internal hip rotation at 90 degrees, pain-free groin squeeze test at 45 degrees and no symptoms during the Linear running programme. Progression from level 3 when they complete the multidirectional drills at maximum intensity pain-free. <ref name=":1" /> | |||
< | ===='''Modified Hölmich Protocol'''==== | ||
The recently published study suggests that '''modified Hölmich protocol'''<ref name=":10" /> may be safer and ''<u>'''more effective'''</u> than'' the Hölmich protocol in athletes with longstanding adductor groin pain in promoting their return to sports activity. Hölmich et al. (1999)<ref>Hölmich P, Uhrskou P, Ulnits L, Kanstrup IL, Nielsen MB, Bjerg AM, Krogsgaard K. [https://pubmed.ncbi.nlm.nih.gov/9989713/ Effectiveness of active physical training as treatment for long-standing adductor-related groin pain in athletes: randomised trial]. The Lancet. 1999 Feb 6;353(9151):439-43.</ref> showed that therapeutic exercise (concentrated on hip and abdominal muscle strengthening) compared with physiotherapy including passive agents (stretching, TENS, transverse friction massage, and laser therapy) leads to better results in terms of reducing pain and returning to sports activity. The modified Hölmich ''ten-week protocol'' that benefits from strengthening the muscles affecting the ''pelvis, core stabilization, hip adductor stretching and high-intensity eccentric exercise of the hip adductors'' may have a considerable effect on primary measured outcomes including pain, hip adductor and abductor muscle strength, hip ROM, functional ability, and returning to the sport.<ref name=":10">Yousefzadeh A, Shadmehr A, Olyaei GR, Naseri N, Khazaeipour Z. [https://www.hindawi.com/journals/rerp/2018/8146819/ The Effect of Therapeutic Exercise on Long-Standing Adductor-Related Groin Pain in Athletes: Modified Hölmich Protocol.] Rehabilitation research and practice 2018;1-10.</ref> | |||
=== Stretching Exercises === | |||
< | {{#ev:youtube|f2e_oi2FbPM|300}}<ref>The Prehab Guys. 3 Exercises to Prehab your Adductor Strain / Groin Pain. Available from https://www.youtube.com/watch?v=f2e_oi2FbPM </ref> | ||
== | === Strengthening Exercises === | ||
- | ==== Hip Adductors ==== | ||
* Side-lying hip-adduction and ball-squeeze exercises display the highest overall activation of [[Adductor Longus|adductor longus]] muscle.<ref name="'Delmore'">Delmore RJ, Laudner KG, Torry MR. [https://elementssystem.com/wp-content/uploads/2020/01/Delmore-adductor-longus-2014.pdf Adductor longus activation during common hip exercises.] Journal of sport rehabilitation 2014;23(2):79-87.</ref> | |||
< | {| width="100%" cellspacing="1" cellpadding="1" | ||
|- | |||
|{{#ev:youtube|watch?v=bmjGd7z7fHc|300}}<ref>Natalie Wetzel.Adductor isometric exercise. Available from https://www.youtube.com/watch?time_continue=6&v=bmjGd7z7fHc | |||
</ref> | |||
|{{#ev:youtube|watch?v=bP9W4-vgSgA|300}}<ref>Jason Craig Hip Adductor Strengthening in Side Lying. Available from https://www.youtube.com/watch?v=bP9W4-vgSgA | |||
</ref> | |||
|} | |||
= | * Resisted training: | ||
Resisted work with weights or elastic bands.{{#ev:youtube|watch?v=jn22rqsaeV8|300}}<ref>Upright Health An exercise to safely strengthen your adductors.Available from https://www.youtube.com/watch?time_continue=4&v=jn22rqsaeV8 </ref> | |||
* Eccentric exercises:<ref name="'Jensen'2">Jensen J, Hölmich P, Bandholm T, Zebis MK, Andersen LL, Thorborg K. [https://www.researchgate.net/profile/Thomas_Bandholm/publication/228324060_Eccentric_strengthening_effect_of_hip-adductor_training_with_elastic_bands_in_Soccer_players_A_randomised_controlled_trial/links/543cdf520cf24ef33b764869/Eccentric-strengthening-ef Eccentric strengthening effect of hip-adductor training with elastic bands in soccer players: a randomised controlled trial.] British Journal of Sports Medicine 2014;48(4):332-8.</ref> | |||
A simple adduction strengthening programme based on Copenhagen Adduction Exercise reduced the risk of a groin problem in footballer players according to the study published in the British Journal of Sports Medicine.<ref name=":7">Harøy J, Clarsen B, Wiger EG, Øyen MG, Serner A, Thorborg K, Hölmich P, Andersen TE, Bahr R. [https://bjsm.bmj.com/content/53/3/150.abstract The adductor strengthening programme prevents groin problems among male football players: a cluster-randomised controlled trial.] British journal of sports medicine 2019;53(3):150-7.</ref> | |||
* Squats: | |||
== | Squats can help in strengthening hip and knee muscles including the adductors. Greater stance width in the squat and deadlift, and squeezing a medicine ball between the legs in the leg press may increase adductor longus muscle activity. The research shows that squats performed at 30° of hip external rotation and at least 90° of knee flexion significantly increased the activity of hip adductors.<ref>Pereira GR, Leporace G, das Virgens Chagas D, Furtado LF, Praxedes J, Batista LA. [https://escolatef.eadplataforma.com/upload/files/1806202015925089432010-pereiraetal.-influenceofhipexternalrotationonhipadductorandrectusfemorismyoelectricactivityduringadynamicparallelsquat.pdf Influence of hip external rotation on hip adductor and rectus femoris myoelectric activity during a dynamic parallel squat.] The Journal of Strength & Conditioning Research 2010;24(10):2749-54.</ref> | ||
{{#ev:youtube|watch?v=MSC4X5k1QC4|300}}<ref>2Fitathome.com Sumo Squats: Works your inner thighs, quads and glutes! Multiple Fitness Level Tutorial. Available from https://www.youtube.com/watch?v=MSC4X5k1QC4</ref> | |||
==== Hip Abductors ==== | |||
Strengthening the hip abductors along with hip adductors is important as decreased strength in the hip abductors ([[Gluteus Medius|gluteus medius]]) has been found in athletes who sustained a groin injury due to reduced activity.<ref name=":7" /> Ensuring that hip abductor strength training is included in the rehabilitation programme is another key factor in groin injury prevention.<ref name=":0">Krommes K, Bandholm T, Jakobsen MD, Andersen LL, Serner A, Hölmich P, Thorborg K. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5455186/ Dynamic hip adduction, abduction and abdominal exercises from the Holmich groin-injury prevention program are intense enough to be considered strengthening exercises–a cross-sectional study.] International journal of sports physical therapy 2017;12(3):371.</ref><ref>Kloskowska P, Morrissey D, Small C, Malliaras P, Barton C. [https://link.springer.com/article/10.1007/s40279-016-0523-z Movement patterns and muscular function before and after onset of sports-related groin pain: a systematic review with meta-analysis.] Sports Medicine 2016;46(12):1847-67.</ref> The most evidence-based treatment for both acute and chronic adductor-related issues is progressive strength training combined individualised sport<ref>Thorborg K. [https://meridian.allenpress.com/jat/article/58/7-8/589/483877/Current-Clinical-Concepts-Exercise-and-Load Current Clinical Concepts: Exercise and Load Management of Adductor Strains, Adductor Ruptures, and Long-Standing Adductor-Related Groin Pain]. ''J Athl Train.'' 2023; 58 (7-8): 589–601. </ref> specific loading. | |||
= | {{#ev:youtube|watch?v=HE-8qeIZo3o|300}}<ref>eHowFitness How to Do Thigh Abduction & Adduction Exercises With Bands : Stretching & Exercise. Available from https://www.youtube.com/watch?time_continue=6&v=HE-8qeIZo3o</ref> | ||
== Conclusion == | |||
Groin strains are common in sports, especially adductor muscle [[Muscle Strain|strain]]. Diagnosis should use the clinical diagnostic entities provided by the Doha agreement meeting. There is support for an association of precious injury and greater abductor to adductor strength ratios as well as sport specificity of training and pre-season sport-specific training as individual risk factors for groin strain injury in athletes.<ref name=":9" /> Most athletes will return to sports with no pain and normal function with appropriate rehabilitation and rarely will there be a need for surgery. Active training rehabilitation was found to be very effective in managing groin strains. <ref name=":8" /> | |||
== Resources == | |||
This 17 minute video is a good overview of the muscles of the hip and thigh.<ref > Muscles of the hip and thigh video - © Kenhub https://www.kenhub.com/en/library/anatomy/hip-and-thigh-muscles</ref>{{#ev:youtube|g5QshZM-XOA}} | |||
== References == | |||
[[Category:Vrije_Universiteit_Brussel_Project | <references /> | ||
[[Category:Vrije_Universiteit_Brussel_Project]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Sports Injuries]] | |||
[[Category:Primary Contact]] | |||
[[Category:Muscle strain]] | |||
[[Category:Sports (Lower Limb)]] | |||
Latest revision as of 12:08, 19 March 2024
Original Editor - Els Van Haveras part of the Vrije Universiteit Brussel's Evidence-based Practice project Top Contributors - Vidya Acharya, Astrid Lahousse, Geubels Kaat, Nele Kiekens, Mats Vandervelde, Prince Wilson, Kim Jackson, Admin, Laure Lievens, Wanda van Niekerk, Lucinda hampton, Joao Costa, Kai A. Sigel, 127.0.0.1, Leana Louw, George Prudden, Uchechukwu Chukwuemeka, Claire Knott, Rachael Lowe, Els Van Haver and Naomi O'Reilly
Definition/Description[edit | edit source]
Groin strain is an injury to the muscle-tendon unit that produces pain on palpation of the adductor tendons or its insertion on the pubic bone and pain in the adductor region on resistance testing of the adductors.[1] Groin muscle strains are encountered more frequently in ice hockey and soccer.[2]
These sports require a strong eccentric contraction of the adductor musculature during competition and practice.[3] The underlying injury is most often a muscle or tendon strain at the insertion of the tendon of the adductor muscle to the bone.[4] The adductor longus is most commonly injured.[5]
The difference between groin tendinopathy and strain are:
- First of all, strains are acute and tendinosis is chronic. Tendinosis is a repetitive strain.
- The second difference is that acute injuries are more often localized in the myotendon junctions and chronic injuries are localized at the tendinous insertions on the pubic bone.
See page for adductor tendinitis.
Image: Overview of the muscles of the hip and thigh - anterior and posterior views.[6]
Clinically Relevant Anatomy[edit | edit source]
In human anatomy, the groin is the junctional area between the abdomen and the thigh on either side of the pubic bone. This is also known as the medial compartment of the thigh.
The groin muscles consist of three large groups of muscles that can be injured: the abdominal, iliopsoas and the adductor muscle group.
Image: Anterior view pelvis, pubic bone in red
- The adductor muscle group: The adductors of the hip joint include 6 muscles: the adductor longus, magnus and brevis, gracilis, obturator externus, and pectineus. All these are innervated by the obturator nerve except that of pectineus, which receives innervation from the femoral nerve. The adductors all originate on the pubic ramus as almost all insert on the linea aspera of the posterior femur. The posterior head of the adductor magnus has a proximal attachment on the ischial tuberosity anteroinferiorly and attaches distally on the medial distal femur at the adductor tubercle. The gracilis insertion is on the medial border of the tuberosity of the tibia. The primary function of this muscle group is adduction of the thigh in open-chain motions and stabilization of the lower extremity and pelvis in closed chain motion.
In football, the majority of groin injuries are adductor related. [8] The proximal attachment of the adductor longus contributes to an anatomical pathway across the anterior pubic symphysis that is likely required to withstand the transmission of large forces during multidirectional athletic activities. Its lack of mechanical advantage may make it more susceptible to strain.[9]
- The abdominal group: The abdominal musculature comprise the rectus abdominis, the obliques internus and externus abdominis. (See page for abdominal muscles).
- The iliopsoas group: The iliopsoas, comprised of iliacus and psoas major muscles, is the only muscle directly connecting the spine and the lower limb. (See page for hip anatomy).[3]
Epidemiology /Etiology[edit | edit source]
Groin strains are common amongst athletes who compete in sports that involve repetitive twisting, turning, sprinting and kicking such as football, ice hockey, Australian and Gaelic football.[2] Groin injuries are reported more in males compared to female football athletes. Injuries in men accounted for 4–19% of all injuries and 2–14% in women.[10]
The exact incidence of groin muscle strains in most sports is unknown because athletes often play through minor groin pain and the injury goes unreported. In addition, overlapping diagnoses can skew the incidence.[11] Cumulative or single injury seem to be important etiological factors. Chronic tendinitis of the adductor muscles/tendons, especially that of the adductor longus, is the most frequently diagnosed.[5]
The injury mechanism can be divided into 3 groups:
- Direct blunt trauma: An acute injury, typically a direct injury to the soft tissues resulting in muscle hematoma.
- Forceful contraction: The most common groin injury in athletes is muscle and tendon strain of the adductor muscle group. Change of direction and kicking has been described as the main actions resulting in adductor longus injury. Videos analysis of acute adductor longus [12] injuries in 17 professional male football players showed most injuries occurred in non-contact situations, following a quick reaction to a change in play. Injury actions were: change of direction, kicking, reaching/stretching and jumping. The injury may also occur during a forceful concentric contraction of the muscle.[13] Lower-extremity athletes such as ice hockey and soccer players are naturally more prone to this pathology due to the repetitive twisting, turning, sprinting and kicking.[2]
- Microtrauma by repetitive injury: musculotendinous injuries to the groin are mainly a consequence of cumulative microtraumas (overuse trauma, repeated minor injuries) leading to chronic groin pain.
Characteristics/Clinical Presentation[edit | edit source]
The main sign of groin strain is intense pain in the groin area. Muscle strain injuries often arise from excessive stretching or stretching when the muscle is being activated. When there is a strain in the muscle, the damage is often localized near the muscle-tendon junction. Acute adductor longus injuries may also involve tendinous rupture/ avulsion, primarily at the proximal insertions. [14]
Clinically for an adductor strain, the patient presents with pain in the inner thigh and tenderness along the muscle belly, tendon or insertion. The pain is exacerbated by adduction.[15] Tears frequently occur at the myotendinous junction, which is the weakest part of the muscle-tendon unit but is also commonly seen in the muscle belly. The same mechanism of injury that results in a muscle tear in an adult may cause an apophyseal avulsion in an adolescent. There is a well-established clinical grading system for muscle tears, which has 3 components:[16]
- Grade 1: no loss of function or strength. Muscle tears can show normal appearances or a small area of focal disruption (<5% of the muscle volume), with hematoma and perifascial fluid relatively common on imaging with US and MRI.
- Grade 2: severe, with some weakness. Injury corresponds to a partial tear, with muscle fibre disruption seen (>5% of the muscle volume) but not affecting the whole muscle belly. In acute grade 1 or 2 strains of the adductor muscle, there is intense pain in the groin area, like a sudden stab with a knife, if the athlete attempts to continue the activity. Locally a haemorrhage and swelling can be seen a few days after the injury. A typical trauma history, localized tenderness and difficulties to contract the hip abductors.
- Grade 3: complete muscle tear and complete functional loss. Injuries are complete muscle tears with frayed margins and bunching and/or retraction of the torn muscle fibres. Complete muscle tears or grade 3 strains are most often found in the distal musculotendinous junction located toward the insertion on the femur.
Differential Diagnosis[edit | edit source]
Traditionally, groin pain has been thought to be complex with various definitions and terminologies without any diagnostic criteria.[17] In a systematic review on the treatment of groin pain in athletes, more than 30 different diagnostic terminologies were used to describe groin pain which adds up to the complexity of groin injuries in athletes.[18]
In the attempt to address the different terminologies and definitions used, a consensus meeting was held in Doha, Qatar during the first World Conference of Grain Pain in Athletes , in November 2014. A group of 24 experts from 14 different countries was invited to agree on a standard terminology, along with accompanying definitions. [1]
A classification system of groin pain was described in three main subheading during the Doha agreement meeting;
| Defined Entities. | Other musculoskeletal causes. | Not to be missed. |
|---|---|---|
|
|
Stress fracture
Inguinal lymphadenopathy Intra-abdominal abnormality
Gynaecological conditions Spondyloarthropathies
|
Diagnostic Procedures[edit | edit source]
First of all, there needs to be a patient history and an identification of the pain by the examination of the physiotherapist. On evaluation, there is tenderness to palpation with focal swelling of the adductors and decreased adductor strength and pain with resisted adduction. The diagnosis can be made with focal findings on examination using the guidelines from the Doha agreement classification system without the need for imaging. [1][19] However, imaging can be useful to rule out or in differential diagnosis after a comprehensive clinical examination. Abnormal radiological findings around the pubic symphysis such as pubic bone marrow oedema are common in athletes with adductor and pubic-related pain. These radiological findings are also common in asymptomatic athletes. Radiological findings alone should not be used in making diagnostic decisions as morphology does not necessarily mean pathology. [20]
Outcome Measures[edit | edit source]
The Copenhagen hip and groin outcome score (HAGOS)[21]
Examination[edit | edit source]
Bilateral evaluation of adductor muscle and strength: palpation at the adductor insertion at the pubic bone, adduction against resistance (squeeze tests in 0° and 45°), and passive stretching of the adductor muscles.[15]
A complete clinical examination should be performed for every patient with groin pain. The injured athlete should first be examined by inspection in a standing position to evaluate the alignment of extremities. The patient should then be asked to lie in a supine position to be able to check the motion of the hip joint and the flexibility of the groin and hip muscles. The diagnosis classification system provided by the Doha agreement should be used as a guideline to all groin injuries. [1]
Squeeze Test[edit | edit source]
- If adductor longus muscle is injured pain will be elucidated to the injured area by resisting leg adduction and in passive stretching at full abduction of the hip. Tenderness on palpation is localized to the injury site at the origin of the adductor longus tendon or at the musculotendinous junction.[1]
- Evaluation of iliopsoas muscle-related pain, strength and flexibility: palpation above the inguinal ligament, isometric strength test in hip flexion and a modified Thomas test.[23] Thomas Test
- Abdominal muscle-related pain and strength: palpation of the abdominal muscle insertion at the pubic bone and a functional sit-up test and symphysis joint tenderness at palpation.[23]
- The location of the injury was based on a minimum of 1 positive finding on palpation, stretching, or muscle resistance testing.[24]
Medical Management[edit | edit source]
Management is non-operative with rest, ice, compression, analgesia and physical therapy. Analgesia includes non-steroidal anti-inflammatory agents which help in reducing pain. [25]Injection at the adductor longus enthesis is helpful for refractory patients to conservative management. [26]
Non-operative therapy should be tried for several months and is successful in most instances. However, if symptoms and significant restriction of performance persist after an appropriate conservative management regimen, surgical intervention should be considered. Adductor tenotomy has been suggested as a technique to improve symptoms. [27]
In a recent systematic review that compared surgical intervention to conservative intervention, there was a quicker return to return to play(RTP) time in athletes who had surgical intervention. However, the varied nature of surgical interventions and lack of quality randomised control trial (RCT) in the meta-analysis makes it impractical to recommend the surgical intervention. [28]
Prevention[edit | edit source]
Subsequent groin strains may occur, resulting in a recurrent problem. Hence primary and secondary prevention is equally important. To identify the athlete at risk and possibly correct the predisposing factor(s), the intrinsic and extrinsic risk factors for the injury type must be known.[29]
Previous groin injuries, reduced hip adduction strength, higher level of play and lower levels of sports-specific training are associated with increased risk of new groin injuries.[30] Hölmich et al demonstrated that an 8 to 12-week active strengthening program, consisting of progressive resistive adduction and abduction exercises, balance training, abdominal strengthening and skating movements on a slide board, was effective in treating chronic groin strains. Also, coordination exercises (focused on the muscles related to the pelvis), core stability and eccentric exercises are a part of the prevention program.[31]
Adductor strain injury prevention program[11]
| Warm-up | Bike |
| Adductor stretching | |
| Sumo squats | |
| Side lunges | |
| Kneeling pelvic tilts | |
| Strengthening program | Ball squeezes (legs bent to legs straight) |
| Different ball sizes | |
| Concentric adduction with weight against gravity | |
| Adduction in standing on a cable column or elastic resistance | |
| Seated adduction machine | |
| Standing with involved foot on sliding board moving in the sagittal plane | |
| Bilateral adduction on sliding board moving in the frontal plane (ie, simultaneous bilateral adduction) | |
| Unilateral lunges with reciprocal arm movements | |
| Sports-specific training | On ice kneeling adductor pull together |
| Standing resisted stride lengths on cable column to simulate skating | |
| Slide skating | |
| Cable column crossover pulls | |
| Clinical goal | Adduction strength at least 80% of the abduction strength |
Copenhagen Adductor Exercise
In a cluster-randomised controlled trial involving 35 semiprofessional Norwegian football teams, using a simple adductor strengthening exercise (Copenhagen Adductor Exercise ) with three progression levels, three times per week during the preseason (6-8 weeks), and once per week during the competitive season (28 weeks). There was a significant reduction in the risk of groin problems compared to the controlled group who trained as normal during the season. The intervention group was made up of 18 teams, 339 players and the controlled group 17 teams, 313 players. The prevalence of groin problems was measured weekly in both groups during the competitive season using the Oslo Sports Trauma Research Center Overuse Injury Questionnaire. [32]
Physiotherapy Management[edit | edit source]
The treatment of musculotendinous groin strains are generally conservative. Surgical treatment in acute groin injuries is rarely indicated.[26]
In the treatment of muscle-tendon injuries, immobilization should be limited to as short a period as possible to avoid the harmful effects of immobilization including muscle atrophy and loss of function. Immediate rest after the injury should be used until a diagnosis is secured.
- The primary goal of the treatment program is to minimize the effects of immobilization, regain full range of motion, and restore full muscle strength, endurance and coordination. Therefore, crutches, local cold application, and anti-inflammatory medication are recommended in the initial phase. Muscle exercises can usually be started early, but training should be performed within the limits of pain with careful isometric contractions against resistance.
- After the initial phase, heat is usually valuable, especially when muscle training is started. In general, exercises are performed in a pain-free range of motion and increased pain should not occur after activity.
- As rehabilitation progresses, mild pain can be allowed during exercise, but it should subside immediately after the cessation of training.
- When full range of motion is accomplished, the injured muscle and tendon tolerates higher loads and the goal of rehabilitation should shift towards specific strength training exercises aiming for muscular recovery, increased endurance and a full range of motion.
- The final step is the gradual return to sports activity, which may in some cases take as long as 3 to 6 months.[13]
[edit | edit source]
Enda et al. (2018) examined the effectiveness of rehabilitation that targeted intersegmental control in patients with groin pain. There was significant improvement in the functional performance and return to play time among athletes with groin pain across the various diagnostic entities.[33]
The intervention consists of three(3) levels, addressing intersegmental control and strength, linear running mechanics and increasing linear running load tolerance and multidirectional mechanics and the transition back to high intensity sprinting.[33]
Level 1: Intersegmental control and strength
| Streams | Progressions | ||
|---|---|---|---|
| Hip Flexor | Supine | Standing Supported | Free Standing. |
| Lateral Hip Control | Supported Hip Hitched | Free Standing Hip Hitch | Step Up |
| Abdominal | Crook Lying Leg Lift | Crook lying Alternate Leg Drop | Pallof Kneeling Split Lunge |
| Double leg Squat | High Goblet Squat | Low Goblet Squat | Front Squat |
| Lateral Hip Strength | Abduction/External rotation in mini squat | Abduction/External rotation in a mini squat at wall | Banded Squat |
| Deadlift | Hip Hinge | 1/2 Rack Deadlift | Floor Deadlift |
| Lunge | Split Lunge | Overhead Split Lunge | Weighted Split Lunge |
| Plyometric | On Spot Hopping | Line Hopping | Cone Hopping |
Level 2: Linear running mechanics
| Linear | Instructions |
|---|---|
| Marching and skipping | March skip on the spot with arms overhead, maintaining lumbopelvic and neutral and with aggressive ground contact |
| Barbell/Overhead Running | Run with dowel overhead or barbell across shoulders focusing on tall running posture and keeping stick still |
| Leg change drill | In single leg stand, focus on rapid leg change to drive alternating leg extension and swing leg recovery. |
| Complete 5-6reps of 3-4sets. Focus entirely on the quality of execution |
level 3: Multidirectional mechanics and transitions
| Linear | Instructions |
|---|---|
| Lateral shuffle | Side shuffle between 2 cones 8 meters apart arms locked overhead focusing on getting away from cones as quickly as possible. Progress to race to instruction or shadow opponent while shuffling |
| Zig-Zag cutting | 5 cones in zig zag formation, 5 meters apart from each other. Run and cut as quickly as possible around the cones. Add holding a med ball for increased resistance and higher centre of mass. (CoM) |
| 180-degree cone cutting. | 5 cones in a semi-circle, start in the middle and run at any cone and cut back straight to the starting point. Add holding a med ball for increased resistance and CoM. |
| Complete 3-4sets of 5-6reps. Focus entirely on the quality of execution |
The patient progresses to level 2 once they have a negative crossover sign and from level 2 to level 3 when they have a symmetrical internal hip rotation at 90 degrees, pain-free groin squeeze test at 45 degrees and no symptoms during the Linear running programme. Progression from level 3 when they complete the multidirectional drills at maximum intensity pain-free. [33]
Modified Hölmich Protocol[edit | edit source]
The recently published study suggests that modified Hölmich protocol[34] may be safer and more effective than the Hölmich protocol in athletes with longstanding adductor groin pain in promoting their return to sports activity. Hölmich et al. (1999)[35] showed that therapeutic exercise (concentrated on hip and abdominal muscle strengthening) compared with physiotherapy including passive agents (stretching, TENS, transverse friction massage, and laser therapy) leads to better results in terms of reducing pain and returning to sports activity. The modified Hölmich ten-week protocol that benefits from strengthening the muscles affecting the pelvis, core stabilization, hip adductor stretching and high-intensity eccentric exercise of the hip adductors may have a considerable effect on primary measured outcomes including pain, hip adductor and abductor muscle strength, hip ROM, functional ability, and returning to the sport.[34]
Stretching Exercises[edit | edit source]
Strengthening Exercises[edit | edit source]
Hip Adductors[edit | edit source]
- Side-lying hip-adduction and ball-squeeze exercises display the highest overall activation of adductor longus muscle.[37]
| [38] | [39] |
- Resisted training:
Resisted work with weights or elastic bands.
- Eccentric exercises:[41]
A simple adduction strengthening programme based on Copenhagen Adduction Exercise reduced the risk of a groin problem in footballer players according to the study published in the British Journal of Sports Medicine.[32]
- Squats:
Squats can help in strengthening hip and knee muscles including the adductors. Greater stance width in the squat and deadlift, and squeezing a medicine ball between the legs in the leg press may increase adductor longus muscle activity. The research shows that squats performed at 30° of hip external rotation and at least 90° of knee flexion significantly increased the activity of hip adductors.[42]
Hip Abductors[edit | edit source]
Strengthening the hip abductors along with hip adductors is important as decreased strength in the hip abductors (gluteus medius) has been found in athletes who sustained a groin injury due to reduced activity.[32] Ensuring that hip abductor strength training is included in the rehabilitation programme is another key factor in groin injury prevention.[44][45] The most evidence-based treatment for both acute and chronic adductor-related issues is progressive strength training combined individualised sport[46] specific loading.
Conclusion[edit | edit source]
Groin strains are common in sports, especially adductor muscle strain. Diagnosis should use the clinical diagnostic entities provided by the Doha agreement meeting. There is support for an association of precious injury and greater abductor to adductor strength ratios as well as sport specificity of training and pre-season sport-specific training as individual risk factors for groin strain injury in athletes.[30] Most athletes will return to sports with no pain and normal function with appropriate rehabilitation and rarely will there be a need for surgery. Active training rehabilitation was found to be very effective in managing groin strains. [24]
Resources[edit | edit source]
This 17 minute video is a good overview of the muscles of the hip and thigh.[48]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Weir A, Brukner P, Delahunt E, Ekstrand J, Griffin D, Khan KM, Lovell G, Meyers WC, Muschaweck U, Orchard J, Paajanen H. Doha agreement meeting on terminology and definitions in groin pain in athletes. British journal of sports medicine. 2015 Jun 1;49(12):768-74.
- ↑ 2.0 2.1 2.2 Orchard JW. Men at higher risk of groin injuries in elite team sports: a systematic review. British journal of sports medicine. 2015 Jun 1;49(12):798-802.
- ↑ 3.0 3.1 Tyler TF, Fukunaga T, Gellert J. Rehabilitation of soft tissue injuries of the hip and pelvis. International journal of sports physical therapy 2014;9(6):785.
- ↑ Kerkhoffs GM, Servien E, editors. Acute muscle injuries. Springer International Publishing; 2014.
- ↑ 5.0 5.1 Kiel J, Kaiser K. Adductor Strain. StatPearls Publishing, Treasure Island; 2018.
- ↑ Overview of the muscles of the hip and thigh - anterior and posterior views image - © Kenhub https://www.kenhub.com/en/library/anatomy/hip-and-thigh-muscles
- ↑ AnatomyZone Muscles of the Thigh Part 2 - Medial Compartment - Anatomy Tutorial Available from https://www.youtube.com/watch?time_continue=10&v=MjPAPTJdxa8
- ↑ Hölmich P, Thorborg K, Dehlendorff C, Krogsgaard K, Gluud C. Incidence and clinical presentation of groin injuries in sub-elite male soccer. British journal of sports medicine. 2014 Aug 1;48(16):1245-50.
- ↑ Norton‐old KJ, Schache AG, Barker PJ, Clark RA, Harrison SM, Briggs CA. Anatomical and mechanical relationship between the proximal attachment of adductor longus and the distal rectus sheath. Clinical Anatomy 2013;26(4):522-30.
- ↑ Waldén M, Hägglund M, Ekstrand J. The epidemiology of groin injury in senior football: a systematic review of prospective studies. British journal of sports medicine. 2015 Jun 1;49(12):792-7.
- ↑ 11.0 11.1 Tyler TF, Silvers HJ, Gerhardt MB, Nicholas SJ. Groin injuries in sports medicine. Sports health 2010;2(3):231-6.
- ↑ Serner A, Mosler AB, Tol JL, Bahr R, Weir A. Mechanisms of acute adductor longus injuries in male football players: a systematic visual video analysis. British journal of sports medicine. 2019 Feb 1;53(3):158-64.
- ↑ 13.0 13.1 McSweeney SE, Naraghi A, Salonen D, Theodoropoulos J, White LM. Hip and groin pain in the professional athlete. Canadian Association of Radiologists Journal 2012;63(2):87-99.
- ↑ Serner A, Weir A, Tol JL, Thorborg K, Roemer F, Guermazi A, Yamashiro E, Hölmich P. Characteristics of acute groin injuries in the adductor muscles: a detailed MRI study in athletes. Scandinavian journal of medicine & science in sports. 2018 Feb;28(2):667-76.
- ↑ 15.0 15.1 Thorborg K, Reiman MP, Weir A, Kemp JL, Serner A, Mosler AB, Hölmich P. Clinical examination, diagnostic imaging, and testing of athletes with groin pain: an evidence-based approach to effective management. journal of orthopaedic & sports physical therapy. 2018 Apr;48(4):239-49.
- ↑ Davies AG, Clarke AW, Gilmore J, Wotherspoon M, Connell DA. imaging of groin pain in the athlete. Skeletal radiology. 2010 Jul;39(7):629-44.
- ↑ Hölmich P. Long-standing groin pain in sportspeople falls into three primary patterns, a “clinical entity” approach: a prospective study of 207 patients. British journal of sports medicine. 2007 Apr 1;41(4):247-52.
- ↑ Serner A, van Eijck CH, Beumer BR, Hölmich P, Weir A, de Vos RJ. Study quality on groin injury management remains low: a systematic review on treatment of groin pain in athletes. British journal of sports medicine. 2015 Jun 1;49(12):813-.
- ↑ Branci S, Thorborg K, Nielsen MB, Hölmich P. Radiological findings in symphyseal and adductor-related groin pain in athletes: a critical review of the literature. British journal of sports medicine. 2013 Jul 1;47(10):611-9.
- ↑ Branci S, Thorborg K, Bech BH, Boesen M, Nielsen MB, Hölmich P. MRI findings in soccer players with long-standing adductor-related groin pain and asymptomatic controls. British journal of sports medicine. 2015 May
- ↑ Thorborg K, Hölmich P, Christensen R, Petersen J, Roos EM. The Copenhagen Hip and Groin Outcome Score (HAGOS): development and validation according to the COSMIN checklist. British journal of sports medicine. 2011 May 1;45(6):478-91.
- ↑ Wichita, groin squeeze test. Access from https://www.youtube.com/watch?v=GwxrgZ_XgOU
- ↑ 23.0 23.1 Hölmich P. Groin injuries in athletes—development of clinical entities, treatment, and prevention. Dan Med J. 2015 Dec 1;62(12):B5184.
- ↑ 24.0 24.1 Serner A, Tol JL, Jomaah N, Weir A, Whiteley R, Thorborg K, Robinson M, Hölmich P. Diagnosis of acute groin injuries: a prospective study of 110 athletes. The American journal of sports medicine. 2015 Aug;43(8):1857-64.
- ↑ Elattar O, Choi HR, Dills VD, Busconi B. Groin injuries (athletic pubalgia) and return to play. Sports health. 2016 Jul;8(4):313-23.
- ↑ 26.0 26.1 Kiel J, Kaiser K. Adductor Strain. 2018
- ↑ Queiroz RD, Carvalho RT, Queiroz Szeles PR, Janovsky C, Cohen M. Return to sport after surgical treatment for pubalgia among professional soccer players. Revista brasileira de ortopedia. 2014 May;49:233-9.
- ↑ Bastia P, Ghirarduzzi P, Schiavi P, Donelli D, Pedrazzini A, Leigheb M, Ceccarelli F, Pogliacomi F. Surgical or conservative treatment in ARGP syndrome? A systematic review. Acta Bio Medica: Atenei Parmensis. 2019;90(Suppl 12):14.
- ↑ Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Intrinsic risk factors for groin injuries among male soccer players: a prospective cohort study. The American journal of sports medicine. 2010 Oct;38(10):2051-7.
- ↑ 30.0 30.1 Whittaker JL, Small C, Maffey L, Emery CA. Risk factors for groin injury in sport: an updated systematic review. British journal of sports medicine. 2015 Jun 1;49(12):803-9.
- ↑ Hölmich P, Larsen K, Krogsgaard K, Gluud C. Exercise program for prevention of groin pain in football players: a cluster‐randomized trial. Scandinavian journal of medicine & science in sports. 2010 Dec;20(6):814-21.
- ↑ 32.0 32.1 32.2 Harøy J, Clarsen B, Wiger EG, Øyen MG, Serner A, Thorborg K, Hölmich P, Andersen TE, Bahr R. The adductor strengthening programme prevents groin problems among male football players: a cluster-randomised controlled trial. British journal of sports medicine 2019;53(3):150-7.
- ↑ 33.0 33.1 33.2 King E, Franklyn-Miller A, Richter C, O’Reilly E, Doolan M, Moran K, Strike S, Falvey É. Clinical and biomechanical outcomes of rehabilitation targeting intersegmental control in athletic groin pain: prospective cohort of 205 patients. British journal of sports medicine. 2018 Aug 1;52(16):1054-62.
- ↑ 34.0 34.1 Yousefzadeh A, Shadmehr A, Olyaei GR, Naseri N, Khazaeipour Z. The Effect of Therapeutic Exercise on Long-Standing Adductor-Related Groin Pain in Athletes: Modified Hölmich Protocol. Rehabilitation research and practice 2018;1-10.
- ↑ Hölmich P, Uhrskou P, Ulnits L, Kanstrup IL, Nielsen MB, Bjerg AM, Krogsgaard K. Effectiveness of active physical training as treatment for long-standing adductor-related groin pain in athletes: randomised trial. The Lancet. 1999 Feb 6;353(9151):439-43.
- ↑ The Prehab Guys. 3 Exercises to Prehab your Adductor Strain / Groin Pain. Available from https://www.youtube.com/watch?v=f2e_oi2FbPM
- ↑ Delmore RJ, Laudner KG, Torry MR. Adductor longus activation during common hip exercises. Journal of sport rehabilitation 2014;23(2):79-87.
- ↑ Natalie Wetzel.Adductor isometric exercise. Available from https://www.youtube.com/watch?time_continue=6&v=bmjGd7z7fHc
- ↑ Jason Craig Hip Adductor Strengthening in Side Lying. Available from https://www.youtube.com/watch?v=bP9W4-vgSgA
- ↑ Upright Health An exercise to safely strengthen your adductors.Available from https://www.youtube.com/watch?time_continue=4&v=jn22rqsaeV8
- ↑ Jensen J, Hölmich P, Bandholm T, Zebis MK, Andersen LL, Thorborg K. Eccentric strengthening effect of hip-adductor training with elastic bands in soccer players: a randomised controlled trial. British Journal of Sports Medicine 2014;48(4):332-8.
- ↑ Pereira GR, Leporace G, das Virgens Chagas D, Furtado LF, Praxedes J, Batista LA. Influence of hip external rotation on hip adductor and rectus femoris myoelectric activity during a dynamic parallel squat. The Journal of Strength & Conditioning Research 2010;24(10):2749-54.
- ↑ 2Fitathome.com Sumo Squats: Works your inner thighs, quads and glutes! Multiple Fitness Level Tutorial. Available from https://www.youtube.com/watch?v=MSC4X5k1QC4
- ↑ Krommes K, Bandholm T, Jakobsen MD, Andersen LL, Serner A, Hölmich P, Thorborg K. Dynamic hip adduction, abduction and abdominal exercises from the Holmich groin-injury prevention program are intense enough to be considered strengthening exercises–a cross-sectional study. International journal of sports physical therapy 2017;12(3):371.
- ↑ Kloskowska P, Morrissey D, Small C, Malliaras P, Barton C. Movement patterns and muscular function before and after onset of sports-related groin pain: a systematic review with meta-analysis. Sports Medicine 2016;46(12):1847-67.
- ↑ Thorborg K. Current Clinical Concepts: Exercise and Load Management of Adductor Strains, Adductor Ruptures, and Long-Standing Adductor-Related Groin Pain. J Athl Train. 2023; 58 (7-8): 589–601.
- ↑ eHowFitness How to Do Thigh Abduction & Adduction Exercises With Bands : Stretching & Exercise. Available from https://www.youtube.com/watch?time_continue=6&v=HE-8qeIZo3o
- ↑ Muscles of the hip and thigh video - © Kenhub https://www.kenhub.com/en/library/anatomy/hip-and-thigh-muscles