Autonomic Dysreflexia: Difference between revisions
No edit summary |
No edit summary |
||
| (45 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Surinder Singh|Surinder Singh]] '''Top Contributors''' - {{Special:Contributors/{{ | <div class="editorbox"> '''Original Editor '''- [[User:Surinder Singh|Surinder Singh]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
== Introduction == | == Introduction == | ||
Autonomic dysreflexia is a life-threatening condition | [[Autonomic Dysreflexia]] (AD), also called autonomic hyperreflexia, is the product of dysregulation of the autonomic system, leading to an uncoordinated response to a noxious stimulus below the level of a spinal cord injury.<ref name=":4">Cowan H, Lakra C, Desai M. Autonomic dysreflexia in spinal cord injury. BMJ. 2020;371:m3596. </ref> It is a common pathological life-threatening condition after a [[Spinal Cord Injury]] (SCI), usually occurring if the SCI is at or above the T6 level. Clinically, AD is defined as an acute episode of systolic blood pressure elevated by 25 mm Hg or above the patient’s normal measurements.<ref>Allen KJ, Leslie SW. Autonomic dysreflexia. StatPearls 2020.https://www.ncbi.nlm.nih.gov/books/NBK482434/</ref> | ||
{{#ev:youtube|eocOmytfg8s}}<ref> Dr Matt & Dr Mike. Autonomic Dysreflexia. Available from: http://www.youtube.com/watch?v=eocOmytfg8s last accessed 6/6/2009]</ref> | |||
== Signs & Symptoms == | |||
Acute autonomic dysreflexia reaction is characterized by | |||
# Severe Paroxysmal [[Hypertension]] associated with throbbing [[Headaches and Dizziness|headaches]]. | |||
# Profuse sweating, nasal congestion and piloerection above the level of injury. | |||
# Flushing of the skin above the level of the lesion (vasodilatation). | |||
#[[Bradycardia|Bradycardia.]] | |||
# Cool, pale skin below the level of injury (vasoconstriction). | |||
# Visual disturbances, dizziness, anxiety or a feeling of doom, which is sometimes accompanied by [[Cognitive Impairments|cognitive impairment]]<ref name=":2">Khastgir J, Drake MJ, Abrams P. [https://pubmed.ncbi.nlm.nih.gov/17472540/ Recognition and effective management of autonomic dysreflexia in spinal cord injuries. Expert opinion on pharmacotherapy.] 2007 May 1;8(7):945-56.</ref><ref name=":0">Allen KJ, Leslie SW. [https://pubmed.ncbi.nlm.nih.gov/29494041/ Autonomic dysreflexia]. InStatPearls [Internet] 2022 Feb 14. StatPearls Publishing.</ref><ref name=":1" />. | |||
# Increased spasticity. | |||
# Constricted pupils. | |||
== Pathophysiology == | == Pathophysiology == | ||
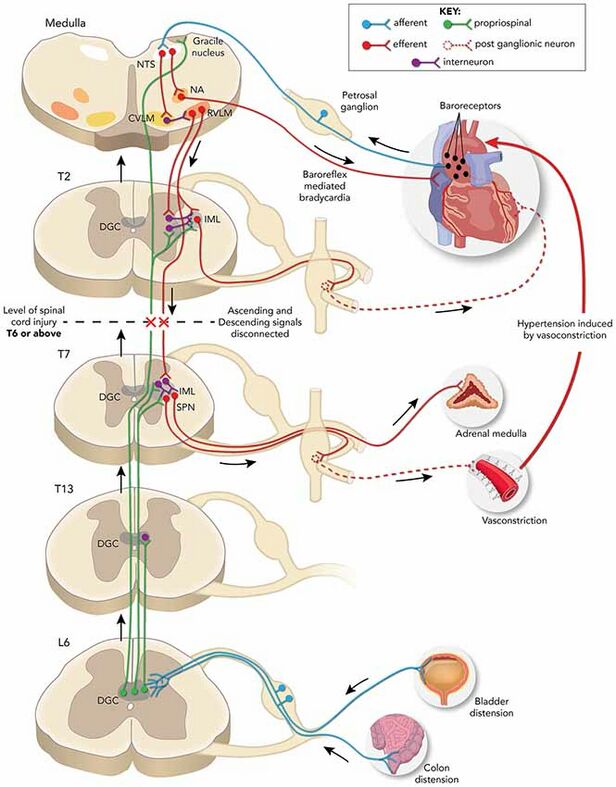
* Cutaneous or visceral triggers below the level of the injury send afferent signals to the intermediolateral grey columns of the [[Spinal cord anatomy|spinal cord]] that start abnormal reflex sympathetic nervous system activity from T6 to L2. | |||
* The sympathetic response is increased due to a lack of compensatory descending [[Parasympathetic System|parasympathetic]] stimulation and intrinsic post-traumatic hypersensitivity. | |||
* Lead to diffuse vasoconstriction, typically to the lower 2/3 of the body, and a severe rise in BP despite maximum parasympathetic vasodilatory efforts above the level of injury (in an intact autonomic system, this increased blood pressure activates the carotid sinus and aortic arch [[baroreceptors]] leading to a parasympathetic response that slows the heart rate via vagal nerve activity and causes diffuse vasodilation to correct the original increased sympathetic toe)e<ref name=":3" />. | |||
* In a person with [[Spinal cord anatomy|spinal cord]] injury, the normal parasympathetic response from the medullary vasomotor center cannot travel below the level of the spinal injury, and generalized vasoconstriction affects the splanchnic, muscular, vascular, and cutaneous arterial circulatory networks. | |||
* This leads to systemic hypertension which is often severe and potentially life-threatening. | |||
* The compensatory vagal and parasympathetic stimulation leads to [[bradycardia]] and vasodilation, but only above the level of the spinal cord injury<ref name=":1" />.[[File:AutoDys2019.jpeg|center|thumb|788x788px|Autonomic Dysreflexia]] | |||
== Etiology == | == Etiology == | ||
The cause of this condition is a spinal cord injury, commonly at or above the T6 level. In the examination, AD episode | The cause of this condition is a spinal cord injury, commonly at or above the T6 level. In the examination, an AD episode has been described as an increase in systolic blood pressure of at least 20–40 mmHg or more above baseline<ref name=":1">[https://pubmed.ncbi.nlm.nih.gov/34353860/ Lakra] C, Swayne O, Christofi G, Desai M. [https://pubmed.ncbi.nlm.nih.gov/34353860/ Autonomic dysreflexia in spinal cord injury. Practical neurology.] 2021 Dec 1;21(6):532-8.</ref>. A severe episode would usually have a systolic blood pressure of at least 150 mmHg or more than 40 mmHg of the patient's baseline. The higher the injury level, the greater the severity of the cardiovascular dysfunction. The severity and frequency of autonomic dysreflexia episodes are also associated with the severity of the spinal cord injury as well as the level. | ||
Autonomic dysreflexia does not develop until after the period of spinal shock when reflexes have recovered<ref name=":1" />. The earliest reported case appeared | Autonomic dysreflexia does not develop until after the period of spinal shock, when reflexes have recovered<ref name=":1" />. The earliest reported case appeared oi the fourth-year post-injury. Most of the patients (92%) who will ultimately develop autonomic dysreflexia will do so within the first year after their injury. | ||
The six "B"s that are the common triggers | The six "B"s that are the common triggers to consider for autonomic dysreflexia<ref name=":0" /> and are reminders of possible triggers to consider in an emergency scenario are<ref name=":5">Flack CK, Mellon MJ. Current management strategies for autonomic dysreflexia. Current Bladder Dysfunction Reports 2018; 13(4): 224-229</ref>: | ||
# Bladder (catheter blockage, distension, stones, infection, spasms) | # Bladder (catheter blockage, distension, stones, infection, spasms) | ||
# Bowel (constipation, impaction) | # Bowel (constipation, impaction) | ||
# Back passage (hemorrhoids, rectal issues, anal abscess, fissure) | # Back passage (hemorrhoids, rectal issues, anal abscess, fissure) | ||
# Boils (skin lesions, infected ulcers | # Boils (skin lesions, infected ulcers) | ||
# Bones (fractures, dislocations) | # [[Bone|Bones]] ([[Fracture|fractures]], dislocations) | ||
# Babies (pregnancy) | # Babies (pregnancy, sexual intercourse, breastfeeding) | ||
The most common cause is over-distension of the bladder, accounting for 75%-85% of all cases <ref>Shergill IS, Arya M, Hamid R, Khastgir J, Patel HR, Shah PJ. The importance of autonomic dysreflexia to the urologist. BJU Int 2004;93:923-6</ref>and being by far the most common trigger, followed by fecal impaction<ref>Shergill IS, Arya M, Hamid R, Khastgir J, Patel HR, Shah PJ. The importance of autonomic dysreflexia to the urologist. BJU international. 2004 May;93(7):923-6.</ref>. | |||
== Diagnosis == | |||
The initial | The most common initial complaint is a severe, throbbing [[headache]]. If the patient with a spinal cord injury (spinal cord injury at or above the T6 level) complains of a severe [[headache]], the practitioner should immediately have their blood pressure checked. If BP is elevated, a provisional diagnosis of autonomic dysreflexia can be made. The patient may also have flushing and sweating of the skin above the level of their spinal cord lesion, along with blurred vision and nasal congestion.<ref name=":4" /> | ||
[[ | The diagnosis can also be made by obtaining a history of previous autonomic dysreflexia episodes with the triggering event if known, monitoring [[Vital Signs|vital signs]], and watching for any developing signs and symptoms. Many patients with spinal cord injuries will have [[hypotension]]. [[Orthostatic Hypotension|Orthostatic hypotension]] is found in over 50% of patients with autonomic dysreflexia<ref>Gibbons CH, Freeman R. [https://pubmed.ncbi.nlm.nih.gov/16832073/ Delayed orthostatic hypotension: a frequent cause of orthostatic intolerance. Neurology.] 2006 Jul 11;67(1):28-32.</ref>. | ||
Fortunately, most episodes are relatively mild and can be managed at home by the patient and their usual caregivers without acute medical intervention<ref name=":2" />. | |||
Fortunately, most episodes are relatively mild and can be managed at home by the patient and their usual caregivers without acute medical intervention | |||
== Epidemiology == | == Epidemiology == | ||
Autonomic dysreflexia | Autonomic dysreflexia affects 48% to 70% of patients with a spinal cord injury above the T6 level and is not very common to affect if the injury is below T10 in patients with spinal cord injury<ref name=":3">Karlsson AK. [https://pubmed.ncbi.nlm.nih.gov/10432257/ Autonomic dysreflexia. Spinal cord]. 1999 Jun;37(6):383-91.</ref>. [[Guillain-Barre Syndrome|Guillain–Barré Syndrome]] may also cause autonomic dysreflexia<ref>Autonomic Dysreflexia https://medlineplus.gov/ency/article/001431.htm</ref>. Patients with a complete spinal cord injury are more than three times more likely to develop autonomic dysreflexia than those with incomplete injuries (91% to 27%).<ref>Del Fabro AS, Mejia M, Nemunaitis G. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5810793/ An investigation of the relationship between autonomic dysreflexia and intrathecal baclofen in patients with spinal cord injury.] The journal of spinal cord medicine. 2018 Jan 2;41(1):102-5. </ref> | ||
== Physiotherapy Management == | |||
In the event of an episode, the physiotherapist should perform the following steps: | |||
# Sit the patient upright with their legs dangling (lying the patient down is contraindicated). | |||
# Notify nearby nurse or doctor for assistance. | |||
# Check catheter for kink, block, fullness (notify nurse to empty if needed) | |||
# Remove any tight clothing or constrictive devices, which will help lower their blood pressure by inducing the pooling of blood in the abdominal and lower extremity vessels as well as eliminating possible triggering stimuli. | |||
# Look for another potentially noxious stimulus below NLI. | |||
# Vital signs should be closely monitored, and identification of the triggering stimulus should be immediately attempted. | |||
# Blood pressure should be checked at least every 5 minutes, and an arterial line should be considered. The noxious stimuli should be corrected as soon as possible<ref>Trop CS, Bennett CJ. [https://pubmed.ncbi.nlm.nih.gov/1942319/ Autonomic dysreflexia and its urological implications: a review. The Journal of urology.] 1991 Dec 1;146(6):1461-9.</ref><ref name=":0" />. | |||
# Document. | |||
'''Note: If the clinician cannot find the triggering stimulus and the above-mentioned steps do not manage the systolic blood pressure below 150 mmHg or less than 40 mmHg above the patient's usual baseline, the clinician should immediately inform the medical staff (doctor or nurse).''' | |||
''' | |||
== Complications == | |||
Common complications of Autonomic dysreflexia are: | |||
# [[Pulmonary Oedema|Pulmonary Edema]] | |||
# Left Ventricular Dysfunction | |||
# Retinal Detachment | |||
# Intracranial Hemorrhage | |||
# Seizures, or Death. | |||
# Cardiac arrest | |||
# Encephalopathy<ref name=":5" /> | |||
# If the patient has coronary artery disease, an episode of autonomic dysreflexia may cause a [[Myocardial Infarction]]<ref name=":1" />. | |||
# Vasomotor instability may contribute to other rare complications acute neurogenic pulmonary edema, aphasia<ref>Wan D, Krassioukov AV. Life-threatening outcomes associated with autonomic dysreflexia: a clinical review. J Spinal Cord Med. 2014;37(1):2–10.</ref>, and cortical blindness.<ref>Edvardsson B, Persson S. Reversible cerebral vasoconstriction syndrome associated with autonomic dysreflexia. J Headache Pain. 2010;11(3):277–80</ref> | |||
== Prognosis == | == Prognosis == | ||
The prognosis of autonomic dysreflexia is | The prognosis of autonomic dysreflexia is good if the condition is identified early, and sufficient education is provided to the patient with spinal cord injury and caregivers. | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
* Acute glomerulonephritis | * Acute glomerulonephritis | ||
* Anxiety | * Anxiety | ||
* [[Cushing's Syndrome|Cushing's syndrome]] | |||
* Cushing's syndrome | |||
* Drug use or overdose (e.g., stimulants, especially alcohol, cocaine, or levothyroxine) | * Drug use or overdose (e.g., stimulants, especially alcohol, cocaine, or levothyroxine) | ||
* Hyperaldosteronism | * Hyperaldosteronism | ||
* [[Hyperthyroidism]] | |||
* Hyperthyroidism | |||
* Intracranial hemorrhage | * Intracranial hemorrhage | ||
* Ischemic [[stroke]] | * Ischemic [[stroke]] | ||
* Nephritic and nephrotic syndrome | * Nephritic and nephrotic syndrome | ||
* Polycystic [[kidney]] disease | |||
* Polycystic kidney disease | |||
== Resources == | == Resources == | ||
An excellent free informational website devoted to patient and professional education about spinal cord injuries can be found at the International Spinal Cord Society ([https://www.iscos.org.uk/ ISCoS]) website. It provides educational modules designed for all stages and levels of spinal cord injury for both laypersons and healthcare personnel<ref name=":1" />. | An excellent free informational website devoted to patient and professional education about [[Spinal Cord Injury|spinal cord injuries]] can be found at the International Spinal Cord Society ([https://www.iscos.org.uk/ ISCoS]) website [http://www.elearnsci.org/ e-learning modules]. It provides educational modules designed for all stages and levels of spinal cord injury for both laypersons and healthcare personnel<ref name=":1" />. | ||
{{#ev:youtube|AMjKn7w4C1o}}<ref>PT Exam Prep. Study Topics: Autonomic Dysreflexia Made Easy. Available from: http://www.youtube.com/watch?v=AMjKn7w4C1o[last accessed 25/4/2022]</ref> | |||
== References == | == References == | ||
Latest revision as of 23:08, 19 June 2023
Introduction[edit | edit source]
Autonomic Dysreflexia (AD), also called autonomic hyperreflexia, is the product of dysregulation of the autonomic system, leading to an uncoordinated response to a noxious stimulus below the level of a spinal cord injury.[1] It is a common pathological life-threatening condition after a Spinal Cord Injury (SCI), usually occurring if the SCI is at or above the T6 level. Clinically, AD is defined as an acute episode of systolic blood pressure elevated by 25 mm Hg or above the patient’s normal measurements.[2]
Signs & Symptoms[edit | edit source]
Acute autonomic dysreflexia reaction is characterized by
- Severe Paroxysmal Hypertension associated with throbbing headaches.
- Profuse sweating, nasal congestion and piloerection above the level of injury.
- Flushing of the skin above the level of the lesion (vasodilatation).
- Bradycardia.
- Cool, pale skin below the level of injury (vasoconstriction).
- Visual disturbances, dizziness, anxiety or a feeling of doom, which is sometimes accompanied by cognitive impairment[4][5][6].
- Increased spasticity.
- Constricted pupils.
Pathophysiology[edit | edit source]
- Cutaneous or visceral triggers below the level of the injury send afferent signals to the intermediolateral grey columns of the spinal cord that start abnormal reflex sympathetic nervous system activity from T6 to L2.
- The sympathetic response is increased due to a lack of compensatory descending parasympathetic stimulation and intrinsic post-traumatic hypersensitivity.
- Lead to diffuse vasoconstriction, typically to the lower 2/3 of the body, and a severe rise in BP despite maximum parasympathetic vasodilatory efforts above the level of injury (in an intact autonomic system, this increased blood pressure activates the carotid sinus and aortic arch baroreceptors leading to a parasympathetic response that slows the heart rate via vagal nerve activity and causes diffuse vasodilation to correct the original increased sympathetic toe)e[7].
- In a person with spinal cord injury, the normal parasympathetic response from the medullary vasomotor center cannot travel below the level of the spinal injury, and generalized vasoconstriction affects the splanchnic, muscular, vascular, and cutaneous arterial circulatory networks.
- This leads to systemic hypertension which is often severe and potentially life-threatening.
- The compensatory vagal and parasympathetic stimulation leads to bradycardia and vasodilation, but only above the level of the spinal cord injury[6].
Etiology[edit | edit source]
The cause of this condition is a spinal cord injury, commonly at or above the T6 level. In the examination, an AD episode has been described as an increase in systolic blood pressure of at least 20–40 mmHg or more above baseline[6]. A severe episode would usually have a systolic blood pressure of at least 150 mmHg or more than 40 mmHg of the patient's baseline. The higher the injury level, the greater the severity of the cardiovascular dysfunction. The severity and frequency of autonomic dysreflexia episodes are also associated with the severity of the spinal cord injury as well as the level.
Autonomic dysreflexia does not develop until after the period of spinal shock, when reflexes have recovered[6]. The earliest reported case appeared oi the fourth-year post-injury. Most of the patients (92%) who will ultimately develop autonomic dysreflexia will do so within the first year after their injury.
The six "B"s that are the common triggers to consider for autonomic dysreflexia[5] and are reminders of possible triggers to consider in an emergency scenario are[8]:
- Bladder (catheter blockage, distension, stones, infection, spasms)
- Bowel (constipation, impaction)
- Back passage (hemorrhoids, rectal issues, anal abscess, fissure)
- Boils (skin lesions, infected ulcers)
- Bones (fractures, dislocations)
- Babies (pregnancy, sexual intercourse, breastfeeding)
The most common cause is over-distension of the bladder, accounting for 75%-85% of all cases [9]and being by far the most common trigger, followed by fecal impaction[10].
Diagnosis[edit | edit source]
The most common initial complaint is a severe, throbbing headache. If the patient with a spinal cord injury (spinal cord injury at or above the T6 level) complains of a severe headache, the practitioner should immediately have their blood pressure checked. If BP is elevated, a provisional diagnosis of autonomic dysreflexia can be made. The patient may also have flushing and sweating of the skin above the level of their spinal cord lesion, along with blurred vision and nasal congestion.[1]
The diagnosis can also be made by obtaining a history of previous autonomic dysreflexia episodes with the triggering event if known, monitoring vital signs, and watching for any developing signs and symptoms. Many patients with spinal cord injuries will have hypotension. Orthostatic hypotension is found in over 50% of patients with autonomic dysreflexia[11].
Fortunately, most episodes are relatively mild and can be managed at home by the patient and their usual caregivers without acute medical intervention[4].
Epidemiology[edit | edit source]
Autonomic dysreflexia affects 48% to 70% of patients with a spinal cord injury above the T6 level and is not very common to affect if the injury is below T10 in patients with spinal cord injury[7]. Guillain–Barré Syndrome may also cause autonomic dysreflexia[12]. Patients with a complete spinal cord injury are more than three times more likely to develop autonomic dysreflexia than those with incomplete injuries (91% to 27%).[13]
Physiotherapy Management[edit | edit source]
In the event of an episode, the physiotherapist should perform the following steps:
- Sit the patient upright with their legs dangling (lying the patient down is contraindicated).
- Notify nearby nurse or doctor for assistance.
- Check catheter for kink, block, fullness (notify nurse to empty if needed)
- Remove any tight clothing or constrictive devices, which will help lower their blood pressure by inducing the pooling of blood in the abdominal and lower extremity vessels as well as eliminating possible triggering stimuli.
- Look for another potentially noxious stimulus below NLI.
- Vital signs should be closely monitored, and identification of the triggering stimulus should be immediately attempted.
- Blood pressure should be checked at least every 5 minutes, and an arterial line should be considered. The noxious stimuli should be corrected as soon as possible[14][5].
- Document.
Note: If the clinician cannot find the triggering stimulus and the above-mentioned steps do not manage the systolic blood pressure below 150 mmHg or less than 40 mmHg above the patient's usual baseline, the clinician should immediately inform the medical staff (doctor or nurse).
Complications[edit | edit source]
Common complications of Autonomic dysreflexia are:
- Pulmonary Edema
- Left Ventricular Dysfunction
- Retinal Detachment
- Intracranial Hemorrhage
- Seizures, or Death.
- Cardiac arrest
- Encephalopathy[8]
- If the patient has coronary artery disease, an episode of autonomic dysreflexia may cause a Myocardial Infarction[6].
- Vasomotor instability may contribute to other rare complications acute neurogenic pulmonary edema, aphasia[15], and cortical blindness.[16]
Prognosis[edit | edit source]
The prognosis of autonomic dysreflexia is good if the condition is identified early, and sufficient education is provided to the patient with spinal cord injury and caregivers.
Differential Diagnosis[edit | edit source]
- Acute glomerulonephritis
- Anxiety
- Cushing's syndrome
- Drug use or overdose (e.g., stimulants, especially alcohol, cocaine, or levothyroxine)
- Hyperaldosteronism
- Hyperthyroidism
- Intracranial hemorrhage
- Ischemic stroke
- Nephritic and nephrotic syndrome
- Polycystic kidney disease
Resources[edit | edit source]
An excellent free informational website devoted to patient and professional education about spinal cord injuries can be found at the International Spinal Cord Society (ISCoS) website e-learning modules. It provides educational modules designed for all stages and levels of spinal cord injury for both laypersons and healthcare personnel[6].
References[edit | edit source]
- ↑ 1.0 1.1 Cowan H, Lakra C, Desai M. Autonomic dysreflexia in spinal cord injury. BMJ. 2020;371:m3596.
- ↑ Allen KJ, Leslie SW. Autonomic dysreflexia. StatPearls 2020.https://www.ncbi.nlm.nih.gov/books/NBK482434/
- ↑ Dr Matt & Dr Mike. Autonomic Dysreflexia. Available from: http://www.youtube.com/watch?v=eocOmytfg8s last accessed 6/6/2009]
- ↑ 4.0 4.1 Khastgir J, Drake MJ, Abrams P. Recognition and effective management of autonomic dysreflexia in spinal cord injuries. Expert opinion on pharmacotherapy. 2007 May 1;8(7):945-56.
- ↑ 5.0 5.1 5.2 Allen KJ, Leslie SW. Autonomic dysreflexia. InStatPearls [Internet] 2022 Feb 14. StatPearls Publishing.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Lakra C, Swayne O, Christofi G, Desai M. Autonomic dysreflexia in spinal cord injury. Practical neurology. 2021 Dec 1;21(6):532-8.
- ↑ 7.0 7.1 Karlsson AK. Autonomic dysreflexia. Spinal cord. 1999 Jun;37(6):383-91.
- ↑ 8.0 8.1 Flack CK, Mellon MJ. Current management strategies for autonomic dysreflexia. Current Bladder Dysfunction Reports 2018; 13(4): 224-229
- ↑ Shergill IS, Arya M, Hamid R, Khastgir J, Patel HR, Shah PJ. The importance of autonomic dysreflexia to the urologist. BJU Int 2004;93:923-6
- ↑ Shergill IS, Arya M, Hamid R, Khastgir J, Patel HR, Shah PJ. The importance of autonomic dysreflexia to the urologist. BJU international. 2004 May;93(7):923-6.
- ↑ Gibbons CH, Freeman R. Delayed orthostatic hypotension: a frequent cause of orthostatic intolerance. Neurology. 2006 Jul 11;67(1):28-32.
- ↑ Autonomic Dysreflexia https://medlineplus.gov/ency/article/001431.htm
- ↑ Del Fabro AS, Mejia M, Nemunaitis G. An investigation of the relationship between autonomic dysreflexia and intrathecal baclofen in patients with spinal cord injury. The journal of spinal cord medicine. 2018 Jan 2;41(1):102-5.
- ↑ Trop CS, Bennett CJ. Autonomic dysreflexia and its urological implications: a review. The Journal of urology. 1991 Dec 1;146(6):1461-9.
- ↑ Wan D, Krassioukov AV. Life-threatening outcomes associated with autonomic dysreflexia: a clinical review. J Spinal Cord Med. 2014;37(1):2–10.
- ↑ Edvardsson B, Persson S. Reversible cerebral vasoconstriction syndrome associated with autonomic dysreflexia. J Headache Pain. 2010;11(3):277–80
- ↑ PT Exam Prep. Study Topics: Autonomic Dysreflexia Made Easy. Available from: http://www.youtube.com/watch?v=AMjKn7w4C1o[last accessed 25/4/2022]