Post-traumatic Stress Disorder: Difference between revisions
Wendy Walker (talk | contribs) No edit summary |
No edit summary |
||
| (37 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:User Name|Samantha Sowder]] [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
'''Original | == Introduction == | ||
[[Image:PTSD image 1.jpg|right]] | |||
< | Post-traumatic Stress Disorder (PTSD) is an anxiety disorder characterised by psychological symptoms that continue to be experienced long after a traumatic event.<ref name="Comer">Comer RJ. Abnormal Psychology. 6th ed. New York, NY: Worth Publishers; 2007.</ref><ref name=":0">Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behaviour research and therapy. 2000 Apr 1;38(4):319-45.</ref> Any physical or psychological trauma can trigger PTSD, but there is most often an involvement of actual or threatened serious injury to the person or someone close to them.<ref name="Hockenbury">Hockenbury DH, Hockenbury SE. Psychology. 3rd ed. New York, NY: Worth Publishers; 2003.</ref> The most common traumatic events leading to PTSD are combat, natural disasters, forced displacement, abuse and victimisation, including sexual assault and terrorism.<ref name="NIMH">National Institute of Mental Health. Health Topics: Post-Traumatic Stress Disorder (PTSD). Available at http://www.nimh.nih.gov/health/publications/post-traumatic-stress-disorder-ptsd/complete-index.shtml. Updated August 31, 2010. Accessed March 6, 2011.</ref> The psychological pattern, characterised by persistent and chronic symptoms, that arise in certain individuals in response to such events define this disorder. The three primary symptoms of PTSD are<ref name=":0" />: | ||
* Recollections of the event | |||
* Avoidance of stimuli | |||
* Increased anxiety and irritability | |||
< | == Etiology == | ||
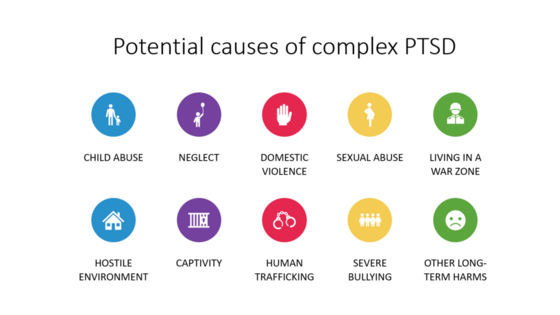
[[File:PTS.png|right|frameless|560x560px|alt=]] | |||
Anyone can develop PTSD following a traumatic event, but people are at greater risk if the event involved deliberate harm such as physical or sexual assault or they have had repeated traumatic experiences. eg childhood sexual abuse, living in a war zone, a near-death experience, combat-related trauma, interpersonal conflicts, sexual abuse or after a medical illness<ref name=":2">Beyond Blue [https://www.beyondblue.org.au/the-facts/anxiety/types-of-anxiety/ptsd PTSD] Available:https://www.beyondblue.org.au/the-facts/anxiety/types-of-anxiety/ptsd (accessed 4.9.2021)</ref>. | |||
< | * Chronic PTSD occurs in patients who are unable to recover from the trauma due to maladaptive responses.<ref name=":1">Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. [https://www.statpearls.com/articlelibrary/viewarticle/27568/ Posttraumatic stress disorder in the National Comorbidity Survey]. Archives of general psychiatry. 1995 Dec 1;52(12):1048-60.Available:https://www.statpearls.com/articlelibrary/viewarticle/27568/ (accessed 4.9.2021)</ref> | ||
* The most commonly reported PTEs in the pediatric population include physical injuries, domestic violence, and natural disasters.<ref name=":3">Fariba K, Gupta V. [https://www.statpearls.com/articlelibrary/viewarticle/19404/ Posttraumatic Stress Disorder In Children]. StatPearls [Internet]. 2021 Feb 6. Available:https://www.statpearls.com/articlelibrary/viewarticle/19404/ (accessed 4.9.2021)</ref> | |||
* Risk Factors - Apart from the event itself, risk factors for developing PTSD include: a past history of trauma or previous mental health problems; ongoing stressful life events after the trauma; an absence of social supports; gender (more prevalent in women); childhood adversities; low socioeconomic status; less education; the nature and the severity of the trauma.<ref name=":1" /> | |||
* A 2021 cross-sectional study found a PTSD prevalence of 30.2% after acute COVID-19 infection<ref>Janiri D, Carfì A, Kotzalidis GD, Bernabei R, Landi F, Sani G, COVID GA, Post-Acute Care Study Group. Posttraumatic stress disorder in patients after severe COVID-19 infection. JAMA psychiatry. 2021 May 1;78(5):567-9.Available:https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2776722 (ACCESSED 4.9.2021)</ref> | |||
* The 2021 Taliban takeover is triggering post-traumatic stress disorder symptoms for former military personnel<ref>Sky News Afghanistan: Taliban takeover triggering post-traumatic stress disorder symptoms for ex-soldiers Available:https://news.sky.com/story/afghanistan-taliban-takeover-triggering-post-traumatic-stress-disorder-symptoms-for-ex-soldiers-12390975 (accessed 4.9.2021)</ref> | |||
* Political violence is known to cause psychological distress. There is a large body of empirical studies drawing correlations between war trauma, [[Rehabilitation for Survivors of Torture|torture]], and post-traumatic stress disorder (PTSD). <ref>Ibrahim H, Hassan CQ. [https://pubmed.ncbi.nlm.nih.gov/28265252/ Post-traumatic stress disorder symptoms resulting from torture and other traumatic events among Syrian Kurdish refugees in Kurdistan Region, Iraq]. Frontiers in psychology. 2017 Feb 20;8:241. Available:https://pubmed.ncbi.nlm.nih.gov/28265252/ Accessed 4.9.2021</ref> | |||
== Epidemiology == | |||
The prevalence of traumatic events in the lives of individuals ranges from 61% to 80%. After the trauma, PTSD occurs in approximately 5% to 10% of the population and is higher in women than in men. Studies have shown that the rates vary depending upon the specific population being considered<ref name=":1" />. | |||
< | * Current estimates suggest 10% of children less than 18 years of age are diagnosed with PTSD, with girls four times more likely than boys to develop it<ref name=":3" /> | ||
* Around 12 per cent of Australians will experience PTSD in their lifetime. Serious accidents are one of the leading causes of PTSD in Australia<ref name=":2" /> | |||
* Rape is the type of trauma most commonly associated with PTSD. Conservative estimates of the number of women raped during the Bosnian war are between 20,000 and 50,000. Estimates of sexual assault rates range from 3% to 6% in Bosnian [[Mental Health and Forced Displacement|refugee]] women, and posttraumatic stress symptoms were found in up to 75% of Bosnian refugees. In Darfur, rates of rape are difficult to establish; however, some estimate that 10,000 girls and women have been raped each year since 2003.<ref>Hamblen J, Barnett E. PTSD: [https://www.ptsd.va.gov/professional/treat/specific/warzone_rape.asp National center for ptsd]. Behavioral Medicine. 2018 Nov:366-7.Available: https://www.ptsd.va.gov/professional/treat/specific/warzone_rape.asp (accessed 4.9.2021)</ref> | |||
== Characteristics == | |||
[[Image:PTSD image 2.jpg|right|230x230px]] | |||
People with PTSD often experience feelings of panic or extreme fear, similar to the fear they felt during the traumatic event. A person with PTSD experiences four main types of difficulties. | |||
* Re-living the traumatic event – The person relives the event through unwanted and recurring memories, often in the form of vivid images and nightmares. There may be intense emotional or physical reactions, such as sweating, heart palpitations or panic when reminded of the event. | |||
* Being overly alert or wound up – The person experiences [[Sleep Deprivation and Sleep Disorders|sleeping difficulties]], irritability and lack of concentration, becoming easily startled and constantly on the lookout for signs of danger. | |||
* Avoiding reminders of the event – The person deliberately avoids activities, places, people, thoughts or feelings associated with the event because they bring back painful memories. | |||
* Feeling emotionally numb – The person loses interest in day-to-day activities, feels cut off and detached from friends and family, or feels emotionally flat and numb.<ref name=":2" /> | |||
< | The phenomenology of PTSD in younger demographics is often often more complex and can mimic variant internalizing and externalizing disorders. It is likely that adults will relegate manifestations of PTSD as disagreeable youthful behavior. Internalizing and externalizing symptomatology that can manifest in the setting of PTSD include separation anxiety, shame, guilt, low frustration tolerance, hyperarousal, impulsivity, temper outbursts, hostility, defiance, aggression, irritability, and mood changes.<ref name=":3" /> | ||
== Complications == | |||
[[File:Drug addict.jpeg|right|frameless]] | |||
Posttraumatic stress disorder has a devastating impact on those suffering and their families. Psychiatric and medical comorbidities are common with PTSD such as: | |||
* Mood disorders | |||
* [[Neurological Disorders|Neurological disorders]] including [[dementia]] | |||
* [[Substance Use Disorder|Substance abuse disorder]] | |||
Studies have shown that 51.9% of men with PTSD concomitantly abuse [[Alcoholism|alcohol]] and have reported early age of onset of alcohol dependence, increased cravings, and legal problems owing to alcohol abuse. There is an overall increased risk of suicide ideation and attempts. Dementia may also occur due to [[Traumatic Brain Injury|traumatic injury]] or alterations in the functioning of the brain<ref name=":1" />. | |||
< | Research shows that people with PTSD are at an increased risk of developing diseases of the nervous system, circulatory systems, digestive system, musculoskeletal system, and ill-defined conditions.<sup><ref name="Andersen">Andersen J, et al. Association Between Posttraumatic Stress Disorder and Primary Care Provider-Diagnosed Disease Among Iraq and Afghanistan Veterans. Psychosomatic Medicine 72:000-000. 2010. doi:10.1097/PSY.0b013e3181d969a1. Available at: http://judithandersen.squarespace.com/storage/Andersen%20et%20al%202010%20PTSD%20and%20Phys%20Health%20MS%20Psychosomatic%20Medicine.pdf. Accessed April 5, 2011.</ref></sup> Furthermore, veterans with PTSD have a higher prevalence of physical illnesses in these areas when compared to veterans without PTSD.<sup><ref name="Schnurr">Schnurr et al. Physician-Diagnosed Medical Disorders in Relation to PTSD Symptoms in Older Male Military Veterans. Health Psychology. 2000;19(1):91-97. doi: 10.1037//0278-6133.19.1.91. Available at: http://www.bu.edu/lab/Publications/Schnurr_Spiro_Paris_2000.pdf. Accessed April 5, 2011.</ref><ref name="Boscarino">Boscarino JA. Posttraumatic Stress Disorder and Physical Illness: Results from Clinical and Epidemiologic Studies. Ann. N.Y. Acad. Sci. 2004; 1032:141-153. doi: 10.1196/annals.1314.011. Available at:http://www.cfids-cab.org/cfs-inform/Ptsd/boscarino04.pdf. Accessed April 5, 2011.</ref></sup> | ||
=== Treatment === | |||
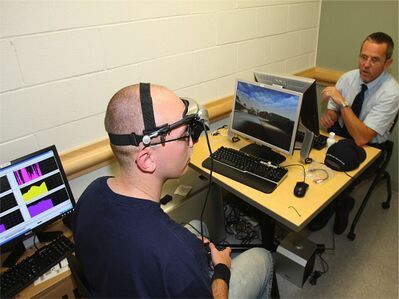
[[File:Biofeedback training program for post-traumatic stress symptoms.jpeg|right|frameless|399x399px]] | |||
We have come a long way in improving treatments for PTSD and now have a large body of research evidence to guide our decisions. | |||
Image R: Biofeedback training program for post-traumatic stress symptoms | |||
< | * The most effective treatment is trauma-focused psychological therapy. There are a few different forms, including cognitive behavioural therapies ([[Cognitive Behavioural Therapy|CBT]]), as well as something called eye movement desensitisation and reprocessing (EMDR). The thing they share in common is providing the survivor with an opportunity to confront the painful memories, and to “work through” the experience in a safe and controlled environment. This therapy is not easy for either the patient or the therapist, but it is very effective in most cases.<ref>The Conversation [https://theconversation.com/explainer-what-is-post-traumatic-stress-disorder-11135 Explainer: what is post-traumatic stress disorder?] Available: https://theconversation.com/explainer-what-is-post-traumatic-stress-disorder-11135 (accessed 4.9.2021)</ref> | ||
* Selective serotonin reuptake inhibitors (SSRI) and serotonin-norepinephrine reuptake inhibitors (SNRI) are the first-line drug of choice for the treatment of PTSD. However, their efficacy in children and adolescents is still to be proven. Insomnia is common in patients with PTSD, which may be treated by educating the patient regarding following adequate [[Sleep: Regulation and Assessment|sleep hygiene]].<ref name=":1" /> | |||
== Patient Education and Deterrence == | |||
The risk and recovery of the patient with posttraumatic stress disorder are highly dependent upon the social phenomenon. Studies have shown that individuals who have been exposed to human-generated traumatic events such as combat veterans are at increased risk of developing PTSD than the individuals who are exposed to other kinds of trauma. During childhood, the child's proximity with its caretaker modulates the coping skills and determines the sense of safety following the trauma. It is challenging for the patients to open up about their trauma, mostly during the first visit. PTSD also affects the development and the course of many physical illnesses. Awareness about the signs and symptoms of PTSD is essential for patients and health-care providers to start early treatment and limit the burden of the illness on the patient and the families of the survivors<ref name=":1" />. | |||
[[Image | === Physiotherapy Management === | ||
[[File:Physiotherapy Exercise and Physical Activity Image.png|right|frameless]] | |||
A physiotherapist is not involved in the primary treatment of PTSD. However, patients with PTSD may have experienced an injury during their traumatic event, i.e. military personnel, emergency personnel, first responders, etc, who need physiotherapy interventions. Acknowledging that the development of PTSD can occur quickly, or with a delayed onset, understanding the associated risk factors, and [[Rehabilitation for Survivors of Torture|recognizing signs and symptoms]] allows for physiotherapists to better address the needs of their patients. A patient exhibiting warning signs of PTSD may indicate the need for onward referral to a mental health professional. Also, collaboration with mental health professionals may be necessary to ensure the highest quality of care for these patients. | |||
[[ | Treating a patient who presents with a co-morbidity of PTSD, or who is exhibiting signs and symptoms of the disorder, may pose challenges throughout the course of therapy. Challenges may include patient’s response to treatment, patient's relationship with the physiotherapist, compliance, fear of symptoms, etc. | ||
[[File:Yoga Music Festival.jpg|right|frameless]] | |||
[[Therapeutic Exercise|Exercise]] is a potent technique for helping those with PTSD | |||
Exercise is a powerful tool in the fight of anxiety and depression. It promotes many changes in the [[Limbic System|brain]], including neural growth, reduced [[Inflammation Acute and Chronic|inflammation]], and new activity patterns that provide feelings of calm and well-being. It also boosts physical and mental energy, relieves tension and [[Stress and Health|stress]], and enhances well-being through the release of endorphins. Exercise can also serve as a much needed distraction, allowing you to find some time to break out of the cycle of negative thoughts that feed [[depression]]. In addition it also: | |||
* Helps you sleep better so you rest fully at night and feel more energised during the day. | |||
* Gives you a sense of accomplishment as your fitness improves and you start achieving your goals. | |||
* Exercise is usually a shared activity with others so you get the added benefits of social connection. | |||
< | Before starting any exercise program (eg [[yoga]], [[Aerobic Exercise|aerobics]]) client should first consult your doctor/physiotherapist to ensure that you do it safely. The doctor may also be able to help identify the best exercises given clients goals, age, weight, or other possible physical health problems<ref>Code9 [https://www.code9ptsd.org.au/ptsd-coping-techniques/physical-activity-and-ptsd PTSD coping techniques] Available:https://www.code9ptsd.org.au/ptsd-coping-techniques/physical-activity-and-ptsd (accessed 4.9.20210</ref>. | ||
== Diagnosis == | |||
{| width="700" border="1" cellspacing="1" cellpadding="1" | |||
|- | |||
| | |||
The DSM-V criteria for diagnosis of PTSD: <br>Diagnostic criteria for PTSD include a history of exposure to a traumatic event that meets specific stipulations and symptoms from each of four symptom clusters: intrusion, avoidance, negative alterations in cognitions and mood, and alterations in arousal and reactivity. The sixth criterion concerns duration of symptoms; the seventh assesses functioning; and, the eighth criterion clarifies symptoms as not attributable to a substance or co-occurring medical condition<sup><ref name="Comer" /><ref name="Fleener">Fleener, PE. Post Traumatic Stress Disorder Today: Post Traumatic Stress Disorder DSM-TR-IVTM Diagnosis & Criteria. Available at http://www.mental-health-today.com/ptsd/dsm.htm. Accessed March 13, 2011.</ref></sup>.<br> | |||
'''Criterion A: Stressor ''' | |||
*The person was exposed to: death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence via direct exposure, witnessing, indirectly, or repeated exposure. | |||
'''Criterion B: Intrusion Symptoms''' | |||
*The traumatic event is persistently re-experienced in one of the following ways: recurrent memories, traumatic nightmares, dissociative reactions (flashbacks), prolonged distress, or marked physiologic reactivity. | |||
'''Criterion C: Avoidance ''' | |||
*Persistent effortful avoidance of distressing trauma related stimuli after the event via thoughts/feelings or external reminders. | |||
'''Criterion D: Negative Alterations in Cognition and Mood''' | |||
*Negative alterations in cognitions and mood that began or worsened after the traumatic event in two of the following ways: dissociative amnesia, persistent negative beliefs, persistent distorted blame, persistent negative trauma related emotions, markedly diminished interest in significant activities, feeling alienated from others, or constrictive affect. | |||
'''Criterion E: Alterations in Arousal and Reactivity''' | |||
*Trauma related alterations in arousal and reactivity that began or worsened after the traumatic event in two of the following ways: irritable or aggressive behavior, self-destructive or reckless behavior, hypervigilance, exaggerated startle response, problems in concentration, or sleep disturbances. | |||
'''Criterion F: Duration''' | |||
*Persistence of symptoms (in Criteria B, C, D, and E) for more than one month. | |||
'''Criterion G: Functional Significance ''' | |||
* Significant symptom related distress or functional impairment (e.g. social, occupational). | |||
'''Criterion H: Exclusion''' | |||
* Disturbance is not due to medication, substance use, or other illness. | |||
|} | |} | ||
{{#ev:youtube|MUVKmhV8MX8}} | |||
== Case Reports == | |||
* [http://www.ncbi.nlm.nih.gov/pubmed/17326730 PTSD and Early Childhood Trauma <sup><ref name="Kaplow">Kaplow JB, Saxe JN, Putnam FW, Pynoos RN, Lieberman AP. The Long-Term Consequences of Early Childhood Trauma: A Case Study and Discussion. Psychiatry. 2006;69(4):362-75. Available at http://www.ncbi.nlm.nih.gov/pubmed/17326730. Accessed April 3, 2011.</ref></sup>][[Post-traumatic Stress Disorder#cite%20note-Kaplow-18|<span class="mw-reflink-text">[18]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-18|<span class="mw-reflink-text">[18]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-18|<span class="mw-reflink-text">[18]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-18|<span class="mw-reflink-text">[18]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-17|<span class="mw-reflink-text">[17]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-15|<span class="mw-reflink-text">[15]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-14|<span class="mw-reflink-text">[14]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-14|<span class="mw-reflink-text">[14]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-14|<span class="mw-reflink-text">[14]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-14|<span class="mw-reflink-text">[14]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-14|<span class="mw-reflink-text">[14]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-14|<span class="mw-reflink-text">[14]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-14|<span class="mw-reflink-text">[14]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-17|<span class="mw-reflink-text">[17]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-17|<span class="mw-reflink-text">[17]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-18|<span class="mw-reflink-text">[18]</span>]][[Post-traumatic Stress Disorder#cite%20note-Kaplow-16|<span class="mw-reflink-text">[16]</span>]][[Post-traumatic Stress Disorder|<span class="mw-reflink-text">[16]</span>]][[Post-traumatic Stress Disorder|<span class="mw-reflink-text">[16]</span>]][[Post-traumatic Stress Disorder|<span class="mw-reflink-text">[15]</span>]][[Post-traumatic Stress Disorder|<span class="mw-reflink-text">[15]</span>]][[Post-traumatic Stress Disorder|<span class="mw-reflink-text">[15]</span>]][[Post-traumatic Stress Disorder|<span class="mw-reflink-text">[14]</span>]][[Post-traumatic Stress Disorder|<span class="mw-reflink-text">[14]</span>]]<span class="mw-reflink-text">[15]</span><span class="mw-reflink-text">[15]</span> | |||
* [http://www.ingentaconnect.com/content/springer/jcogp/2007/00000021/00000001/art00009 PTSD treatment in Battered Women] <sup><ref name="Stapleton">Stapleton J, Taylor S, Asmundson G. Efficacy of Various Treatments for PTSD in Battered Women: Case Studies. Journal of Cognitive Psychotherapy [serial online]. Spring2007 2007;21(1):91-102. Available from: Academic Search Premier, Ipswich, MA. Available at http://www.ingentaconnect.com/content/springer/jcogp/2007/00000021/00000001/art00009. Accessed April 4, 2011.</ref></sup> | |||
* <sup></sup>[http://www.ncbi.nlm.nih.gov/pubmed/10378165 Virtual Reality Exposure Therapy for Vietnam Veterans] <sup><ref name="Roth">Rothbaum B, Hodges L, Alarcon R, Ready D, Shahar F, Baltzell D, et al. Virtual Reality Exposure Therapy for PTSD Vietnam Veterans: A Case Study. Journal of Traumatic Stress [serial on the Internet]. 1999; 12(2):263-271. Available from: Academic Search Premier. Available at http://www.ncbi.nlm.nih.gov/pubmed/10378165. Accessed April 4, 2011.</ref></sup> | |||
* [http://info.onlinelibrary.wiley.com/userfiles/ccoch/file/CD003388.pdf PTSD Treatment Cochrane Review <sup><ref name="Cochrane review">Bisson J, Andrew M. Psychological treatment of post-traumatic stress disorder (PTSD) (Review). The Cochrane Library 2009, Issue 1. Available at http://info.onlinelibrary.wiley.com/userfiles/ccoch/file/CD003388.pdf. Accessed March 16, 2011.</ref></sup>][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-21|<span class="mw-reflink-text">[21]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-21|<span class="mw-reflink-text">[21]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-21|<span class="mw-reflink-text">[21]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-21|<span class="mw-reflink-text">[21]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-20|<span class="mw-reflink-text">[20]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-18|<span class="mw-reflink-text">[18]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-17|<span class="mw-reflink-text">[17]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-17|<span class="mw-reflink-text">[17]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-17|<span class="mw-reflink-text">[17]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-17|<span class="mw-reflink-text">[17]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-17|<span class="mw-reflink-text">[17]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-17|<span class="mw-reflink-text">[17]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-17|<span class="mw-reflink-text">[17]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-20|<span class="mw-reflink-text">[20]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-20|<span class="mw-reflink-text">[20]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-15|<span class="mw-reflink-text">[15]</span>]][[Post-traumatic Stress Disorder#cite%20note-Cochrane%20review-13|<span class="mw-reflink-text">[13]</span>]][[Post-traumatic Stress Disorder|<span class="mw-reflink-text">[14]</span>]][[Post-traumatic Stress Disorder|<span class="mw-reflink-text">[14]</span>]][[Post-traumatic Stress Disorder|<span class="mw-reflink-text">[18]</span>]][[Post-traumatic Stress Disorder|<span class="mw-reflink-text">[18]</span>]][[Post-traumatic Stress Disorder|<span class="mw-reflink-text">[18]</span>]][[Post-traumatic Stress Disorder|<span class="mw-reflink-text">[17]</span>]][[Post-traumatic Stress Disorder|<span class="mw-reflink-text">[17]</span>]]<span class="mw-reflink-text">[18]</span><span class="mw-reflink-text">[18]</span> | |||
<span | |||
<span | |||
< | |||
</span> | |||
<span | |||
<span | |||
< | |||
< | |||
- | |||
<span | |||
<span | |||
- | |||
- | |||
[[ | |||
[[ | |||
[[ | |||
<span | |||
- | |||
<span | |||
<span | |||
<references /> | == References == | ||
<references /><span style="font: 11.0px 'Lucida Grande'; letter-spacing: 0.0px" /><br> | |||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]] | ||
[[Category:Mental Health]] | |||
[[Category:Conditions]] | |||
[[Category:Mental Health - Conditions]] | |||
Latest revision as of 19:43, 27 January 2023
Introduction[edit | edit source]
Post-traumatic Stress Disorder (PTSD) is an anxiety disorder characterised by psychological symptoms that continue to be experienced long after a traumatic event.[1][2] Any physical or psychological trauma can trigger PTSD, but there is most often an involvement of actual or threatened serious injury to the person or someone close to them.[3] The most common traumatic events leading to PTSD are combat, natural disasters, forced displacement, abuse and victimisation, including sexual assault and terrorism.[4] The psychological pattern, characterised by persistent and chronic symptoms, that arise in certain individuals in response to such events define this disorder. The three primary symptoms of PTSD are[2]:
- Recollections of the event
- Avoidance of stimuli
- Increased anxiety and irritability
Etiology[edit | edit source]
Anyone can develop PTSD following a traumatic event, but people are at greater risk if the event involved deliberate harm such as physical or sexual assault or they have had repeated traumatic experiences. eg childhood sexual abuse, living in a war zone, a near-death experience, combat-related trauma, interpersonal conflicts, sexual abuse or after a medical illness[5].
- Chronic PTSD occurs in patients who are unable to recover from the trauma due to maladaptive responses.[6]
- The most commonly reported PTEs in the pediatric population include physical injuries, domestic violence, and natural disasters.[7]
- Risk Factors - Apart from the event itself, risk factors for developing PTSD include: a past history of trauma or previous mental health problems; ongoing stressful life events after the trauma; an absence of social supports; gender (more prevalent in women); childhood adversities; low socioeconomic status; less education; the nature and the severity of the trauma.[6]
- A 2021 cross-sectional study found a PTSD prevalence of 30.2% after acute COVID-19 infection[8]
- The 2021 Taliban takeover is triggering post-traumatic stress disorder symptoms for former military personnel[9]
- Political violence is known to cause psychological distress. There is a large body of empirical studies drawing correlations between war trauma, torture, and post-traumatic stress disorder (PTSD). [10]
Epidemiology[edit | edit source]
The prevalence of traumatic events in the lives of individuals ranges from 61% to 80%. After the trauma, PTSD occurs in approximately 5% to 10% of the population and is higher in women than in men. Studies have shown that the rates vary depending upon the specific population being considered[6].
- Current estimates suggest 10% of children less than 18 years of age are diagnosed with PTSD, with girls four times more likely than boys to develop it[7]
- Around 12 per cent of Australians will experience PTSD in their lifetime. Serious accidents are one of the leading causes of PTSD in Australia[5]
- Rape is the type of trauma most commonly associated with PTSD. Conservative estimates of the number of women raped during the Bosnian war are between 20,000 and 50,000. Estimates of sexual assault rates range from 3% to 6% in Bosnian refugee women, and posttraumatic stress symptoms were found in up to 75% of Bosnian refugees. In Darfur, rates of rape are difficult to establish; however, some estimate that 10,000 girls and women have been raped each year since 2003.[11]
Characteristics[edit | edit source]
People with PTSD often experience feelings of panic or extreme fear, similar to the fear they felt during the traumatic event. A person with PTSD experiences four main types of difficulties.
- Re-living the traumatic event – The person relives the event through unwanted and recurring memories, often in the form of vivid images and nightmares. There may be intense emotional or physical reactions, such as sweating, heart palpitations or panic when reminded of the event.
- Being overly alert or wound up – The person experiences sleeping difficulties, irritability and lack of concentration, becoming easily startled and constantly on the lookout for signs of danger.
- Avoiding reminders of the event – The person deliberately avoids activities, places, people, thoughts or feelings associated with the event because they bring back painful memories.
- Feeling emotionally numb – The person loses interest in day-to-day activities, feels cut off and detached from friends and family, or feels emotionally flat and numb.[5]
The phenomenology of PTSD in younger demographics is often often more complex and can mimic variant internalizing and externalizing disorders. It is likely that adults will relegate manifestations of PTSD as disagreeable youthful behavior. Internalizing and externalizing symptomatology that can manifest in the setting of PTSD include separation anxiety, shame, guilt, low frustration tolerance, hyperarousal, impulsivity, temper outbursts, hostility, defiance, aggression, irritability, and mood changes.[7]
Complications[edit | edit source]
Posttraumatic stress disorder has a devastating impact on those suffering and their families. Psychiatric and medical comorbidities are common with PTSD such as:
- Mood disorders
- Neurological disorders including dementia
- Substance abuse disorder
Studies have shown that 51.9% of men with PTSD concomitantly abuse alcohol and have reported early age of onset of alcohol dependence, increased cravings, and legal problems owing to alcohol abuse. There is an overall increased risk of suicide ideation and attempts. Dementia may also occur due to traumatic injury or alterations in the functioning of the brain[6].
Research shows that people with PTSD are at an increased risk of developing diseases of the nervous system, circulatory systems, digestive system, musculoskeletal system, and ill-defined conditions.[12] Furthermore, veterans with PTSD have a higher prevalence of physical illnesses in these areas when compared to veterans without PTSD.[13][14]
Treatment[edit | edit source]
We have come a long way in improving treatments for PTSD and now have a large body of research evidence to guide our decisions.
Image R: Biofeedback training program for post-traumatic stress symptoms
- The most effective treatment is trauma-focused psychological therapy. There are a few different forms, including cognitive behavioural therapies (CBT), as well as something called eye movement desensitisation and reprocessing (EMDR). The thing they share in common is providing the survivor with an opportunity to confront the painful memories, and to “work through” the experience in a safe and controlled environment. This therapy is not easy for either the patient or the therapist, but it is very effective in most cases.[15]
- Selective serotonin reuptake inhibitors (SSRI) and serotonin-norepinephrine reuptake inhibitors (SNRI) are the first-line drug of choice for the treatment of PTSD. However, their efficacy in children and adolescents is still to be proven. Insomnia is common in patients with PTSD, which may be treated by educating the patient regarding following adequate sleep hygiene.[6]
Patient Education and Deterrence[edit | edit source]
The risk and recovery of the patient with posttraumatic stress disorder are highly dependent upon the social phenomenon. Studies have shown that individuals who have been exposed to human-generated traumatic events such as combat veterans are at increased risk of developing PTSD than the individuals who are exposed to other kinds of trauma. During childhood, the child's proximity with its caretaker modulates the coping skills and determines the sense of safety following the trauma. It is challenging for the patients to open up about their trauma, mostly during the first visit. PTSD also affects the development and the course of many physical illnesses. Awareness about the signs and symptoms of PTSD is essential for patients and health-care providers to start early treatment and limit the burden of the illness on the patient and the families of the survivors[6].
Physiotherapy Management [edit | edit source]
A physiotherapist is not involved in the primary treatment of PTSD. However, patients with PTSD may have experienced an injury during their traumatic event, i.e. military personnel, emergency personnel, first responders, etc, who need physiotherapy interventions. Acknowledging that the development of PTSD can occur quickly, or with a delayed onset, understanding the associated risk factors, and recognizing signs and symptoms allows for physiotherapists to better address the needs of their patients. A patient exhibiting warning signs of PTSD may indicate the need for onward referral to a mental health professional. Also, collaboration with mental health professionals may be necessary to ensure the highest quality of care for these patients.
Treating a patient who presents with a co-morbidity of PTSD, or who is exhibiting signs and symptoms of the disorder, may pose challenges throughout the course of therapy. Challenges may include patient’s response to treatment, patient's relationship with the physiotherapist, compliance, fear of symptoms, etc.
Exercise is a potent technique for helping those with PTSD
Exercise is a powerful tool in the fight of anxiety and depression. It promotes many changes in the brain, including neural growth, reduced inflammation, and new activity patterns that provide feelings of calm and well-being. It also boosts physical and mental energy, relieves tension and stress, and enhances well-being through the release of endorphins. Exercise can also serve as a much needed distraction, allowing you to find some time to break out of the cycle of negative thoughts that feed depression. In addition it also:
- Helps you sleep better so you rest fully at night and feel more energised during the day.
- Gives you a sense of accomplishment as your fitness improves and you start achieving your goals.
- Exercise is usually a shared activity with others so you get the added benefits of social connection.
Before starting any exercise program (eg yoga, aerobics) client should first consult your doctor/physiotherapist to ensure that you do it safely. The doctor may also be able to help identify the best exercises given clients goals, age, weight, or other possible physical health problems[16].
Diagnosis[edit | edit source]
|
The DSM-V criteria for diagnosis of PTSD: Criterion A: Stressor
Criterion B: Intrusion Symptoms
Criterion C: Avoidance
Criterion D: Negative Alterations in Cognition and Mood
Criterion E: Alterations in Arousal and Reactivity
Criterion F: Duration
Criterion G: Functional Significance
Criterion H: Exclusion
|
Case Reports[edit | edit source]
- PTSD and Early Childhood Trauma [18][18][18][18][18][17][15][14][14][14][14][14][14][14][17][17][18][16][16][16][15][15][15][14][14][15][15]
- PTSD treatment in Battered Women [19]
- Virtual Reality Exposure Therapy for Vietnam Veterans [20]
- PTSD Treatment Cochrane Review [21][21][21][21][21][20][18][17][17][17][17][17][17][17][20][20][15][13][14][14][18][18][18][17][17][18][18]
References[edit | edit source]
- ↑ 1.0 1.1 Comer RJ. Abnormal Psychology. 6th ed. New York, NY: Worth Publishers; 2007.
- ↑ 2.0 2.1 Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behaviour research and therapy. 2000 Apr 1;38(4):319-45.
- ↑ Hockenbury DH, Hockenbury SE. Psychology. 3rd ed. New York, NY: Worth Publishers; 2003.
- ↑ National Institute of Mental Health. Health Topics: Post-Traumatic Stress Disorder (PTSD). Available at http://www.nimh.nih.gov/health/publications/post-traumatic-stress-disorder-ptsd/complete-index.shtml. Updated August 31, 2010. Accessed March 6, 2011.
- ↑ 5.0 5.1 5.2 Beyond Blue PTSD Available:https://www.beyondblue.org.au/the-facts/anxiety/types-of-anxiety/ptsd (accessed 4.9.2021)
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of general psychiatry. 1995 Dec 1;52(12):1048-60.Available:https://www.statpearls.com/articlelibrary/viewarticle/27568/ (accessed 4.9.2021)
- ↑ 7.0 7.1 7.2 Fariba K, Gupta V. Posttraumatic Stress Disorder In Children. StatPearls [Internet]. 2021 Feb 6. Available:https://www.statpearls.com/articlelibrary/viewarticle/19404/ (accessed 4.9.2021)
- ↑ Janiri D, Carfì A, Kotzalidis GD, Bernabei R, Landi F, Sani G, COVID GA, Post-Acute Care Study Group. Posttraumatic stress disorder in patients after severe COVID-19 infection. JAMA psychiatry. 2021 May 1;78(5):567-9.Available:https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2776722 (ACCESSED 4.9.2021)
- ↑ Sky News Afghanistan: Taliban takeover triggering post-traumatic stress disorder symptoms for ex-soldiers Available:https://news.sky.com/story/afghanistan-taliban-takeover-triggering-post-traumatic-stress-disorder-symptoms-for-ex-soldiers-12390975 (accessed 4.9.2021)
- ↑ Ibrahim H, Hassan CQ. Post-traumatic stress disorder symptoms resulting from torture and other traumatic events among Syrian Kurdish refugees in Kurdistan Region, Iraq. Frontiers in psychology. 2017 Feb 20;8:241. Available:https://pubmed.ncbi.nlm.nih.gov/28265252/ Accessed 4.9.2021
- ↑ Hamblen J, Barnett E. PTSD: National center for ptsd. Behavioral Medicine. 2018 Nov:366-7.Available: https://www.ptsd.va.gov/professional/treat/specific/warzone_rape.asp (accessed 4.9.2021)
- ↑ Andersen J, et al. Association Between Posttraumatic Stress Disorder and Primary Care Provider-Diagnosed Disease Among Iraq and Afghanistan Veterans. Psychosomatic Medicine 72:000-000. 2010. doi:10.1097/PSY.0b013e3181d969a1. Available at: http://judithandersen.squarespace.com/storage/Andersen%20et%20al%202010%20PTSD%20and%20Phys%20Health%20MS%20Psychosomatic%20Medicine.pdf. Accessed April 5, 2011.
- ↑ Schnurr et al. Physician-Diagnosed Medical Disorders in Relation to PTSD Symptoms in Older Male Military Veterans. Health Psychology. 2000;19(1):91-97. doi: 10.1037//0278-6133.19.1.91. Available at: http://www.bu.edu/lab/Publications/Schnurr_Spiro_Paris_2000.pdf. Accessed April 5, 2011.
- ↑ Boscarino JA. Posttraumatic Stress Disorder and Physical Illness: Results from Clinical and Epidemiologic Studies. Ann. N.Y. Acad. Sci. 2004; 1032:141-153. doi: 10.1196/annals.1314.011. Available at:http://www.cfids-cab.org/cfs-inform/Ptsd/boscarino04.pdf. Accessed April 5, 2011.
- ↑ The Conversation Explainer: what is post-traumatic stress disorder? Available: https://theconversation.com/explainer-what-is-post-traumatic-stress-disorder-11135 (accessed 4.9.2021)
- ↑ Code9 PTSD coping techniques Available:https://www.code9ptsd.org.au/ptsd-coping-techniques/physical-activity-and-ptsd (accessed 4.9.20210
- ↑ Fleener, PE. Post Traumatic Stress Disorder Today: Post Traumatic Stress Disorder DSM-TR-IVTM Diagnosis & Criteria. Available at http://www.mental-health-today.com/ptsd/dsm.htm. Accessed March 13, 2011.
- ↑ Kaplow JB, Saxe JN, Putnam FW, Pynoos RN, Lieberman AP. The Long-Term Consequences of Early Childhood Trauma: A Case Study and Discussion. Psychiatry. 2006;69(4):362-75. Available at http://www.ncbi.nlm.nih.gov/pubmed/17326730. Accessed April 3, 2011.
- ↑ Stapleton J, Taylor S, Asmundson G. Efficacy of Various Treatments for PTSD in Battered Women: Case Studies. Journal of Cognitive Psychotherapy [serial online]. Spring2007 2007;21(1):91-102. Available from: Academic Search Premier, Ipswich, MA. Available at http://www.ingentaconnect.com/content/springer/jcogp/2007/00000021/00000001/art00009. Accessed April 4, 2011.
- ↑ Rothbaum B, Hodges L, Alarcon R, Ready D, Shahar F, Baltzell D, et al. Virtual Reality Exposure Therapy for PTSD Vietnam Veterans: A Case Study. Journal of Traumatic Stress [serial on the Internet]. 1999; 12(2):263-271. Available from: Academic Search Premier. Available at http://www.ncbi.nlm.nih.gov/pubmed/10378165. Accessed April 4, 2011.
- ↑ Bisson J, Andrew M. Psychological treatment of post-traumatic stress disorder (PTSD) (Review). The Cochrane Library 2009, Issue 1. Available at http://info.onlinelibrary.wiley.com/userfiles/ccoch/file/CD003388.pdf. Accessed March 16, 2011.
<span style="font: 11.0px 'Lucida Grande'; letter-spacing: 0.0px" />