Sleep: Regulation and Assessment
Original Editor - Wanda van Niekerk
Top Contributors - Wanda van Niekerk, Kim Jackson, Lucinda hampton and Admin
Introduction[edit | edit source]
How we sleep is regulated by two internal biological mechanisms. These two systems work together to regulate when we are awake and when we sleep. Sleep studies and specific objective and subjective measurements of sleep can provide important information on sleep in individuals with sleep-related issues or deprivation.
Regulation of Sleep[edit | edit source]
Sleep is regulated by two independent, yet interrelated processes.[1] These two processes are:
- Homeostatic Sleep Drive
- Circadian Rhythm
These processes play a role in sleep regulation with regards to[2]:
- sleep timing
- sleep intensity
- sleep duration
Homeostatic Sleep Drive[edit | edit source]
- Also known as process S[1]
- Represents sleep debt
- Sleep drive or the need for sleep increases during wakefulness and decreases during sleep
- Regulated by the duration of which we have been prior awake
- The result of the accumulation of sleep-inducing substances in the brain – increasing levels of the hormone Adenosine[4]
- Adenosine starts to build up from the moment of wakefulness and only relieved to the point of which one falls asleep
- Adenosine augments sleep propensity (the natural tendency to want to fall asleep)
- Caffeine is a stimulant that binds to the Adenosine receptor and blocks the impact of the desire for sleep propensity, but the pressure to sleep will still build up nonetheless.[5]
- In a sleep-deprived state, the homeostatic drive for sleep will increase and sleep will most likely occur at inappropriate times or unusual times[6]
- A typical phenomenon in a sleep-deprived individual is “micro-sleep” (when a person will disengage from their physical surroundings due to a momentary lapse in visual processing). Sleep debt can be paid back, but the long-term effects of sleep deprivation can be detrimental to physical, mental and emotional health. Read more about Sleep Deprivation.
- Slow-wave sleep (SWS) is the principal marker of homeostatic sleep drive or process S[1]
- Slow-wave sleep – greatest during initial sleep periods when the desire for sleep is very high, this decreases as sleep is initiated. For example, taking a nap during the day may decrease the level of deep sleep.
- Therefore slow-wave sleep activity and the measurement thereof represents an important marker of the homeostatic process
Circadian Rhythm[edit | edit source]
Also known as process C or the sleep/wake cycle[1] - Cycles between sleepiness and alertness at regular intervals
- Most predominant of biological functions involved in the normal sleep and wakefulness cycle
- Dependent on the system which oscillates within a period of approximately 24 hours, with daily alterations between lightness and darkness
- Human circadian rhythm is actually more than 24 hours – but light assists with regulating it into a 24-hour model[7]
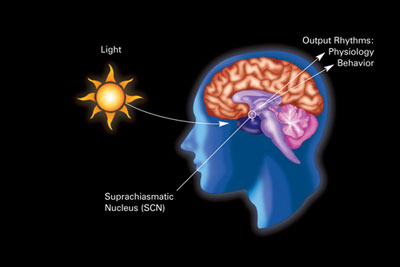
Superchiasmic nucleus (SCN) is the circadian pacemaker or biological clock in humans[8]
- SCN is situated in the hypothalamus
- SCN is synchronised by exogenous environmental cues known as "zeitgebers" (time-givers)[9]
- Most powerful zeitgeber is light – this activates photoreceptors in the retina and this inhibits the secretion of melatonin by the pineal gland
Sleep propensity of humans corresponds to body temperature and specifically nadir[10]
- Nadir is the point where the lowest core temperature is recorded
- Body temperature cycles are also controlled by the hypothalamus
- Body temperature increases during the day and decreases during the night
These temperature peaks and troughs are hypothesised to mirror sleep rhythm
- Maximum alertness will occur near the peak body temperature [11][12]
- Drowsiness will increase as temperature decreases
Circadian nadir will be when sleepiness become overpowering (typically around 2-3 am in the morning – people doing shift work find it difficult to stay awake around this time)[6]
Two-Process Model of Sleep[edit | edit source]
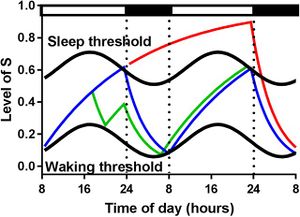
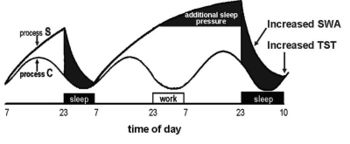
This model proposed by Borbely[1] posits that the ability to initiate sleep is determined by both the homeostatic sleep drive and the Circadian process. The homeostatic process, which is derived from the time course of slow-wave activity, is represented by a linear increase during wakefulness, and a linear decline during sleep. In ideal, non-sleep deprived scenarios the interaction between the homeostatic sleep drive and the circadian process is relatively synchronous.
Daan et al[14] (1984) investigated the timing of sleep (onset and duration) and determined and developed upper and lower thresholds to predict sleep timing. Taking a nap during the day will affect the consistency in sleep patterns and causes a transitory depression of the upper threshold of the homeostatic process. The evening maintenance wake zone refers to the increased level of self-alertness before falling asleep.[15] This indicates the circadian impact on sleep propensity. In the early evening before bedtime, the circadian drive for sleep is very low, shortly before the onset of melatonin secretion. Although this may seem counterintuitive, as it implies a high circadian drive for alertness in the evening, it was shown that the circadian arousal signal in the early evening causes higher subjective and objective alertness and it actually opposes the accumulated homeostatic sleep drive.[15] This dynamic interaction between these two processes in sleep/wake regulation allows for a wake period of around 16 hours during the daytime and a consolidated sleep period of approximately 8 hours at night, in humans.[16]
External Conditions Affecting the Threshold Levels[edit | edit source]
- Sleep deprivation conditions create a suspension in the upper thresholds, therefore allowing process S or homeostatic sleep drive to increase further
- Other factors such as bed rest, warmth, darkness or the absence of social stimulation lower the upper threshold so that sleep is precipitated.[14]
The circadian rhythm modulates these two thresholds and it determines the onset and termination of sleep episodes.[14]
Secondary Sleep Drive[edit | edit source]
Johns[18] developed a further process stating that sleep and wakefulness at a particular time are dependent on the relative strength of both processes but not on the absolute strength of them. It is theorised that the secondary wake drive is influenced by things such as[6]:
- Posture
- Behaviour
- Physical activity
- Feelings
- Mental activity
This then supports psychological approaches which have been shown to be effective in treating sleep-related disorders like insomnia.
The magnitude of the secondary sleep drive may be the most important determinant of sleep propensity as changes in this can be controlled by individuals themselves. This then emphasis that people need to look after their mental and physical health, and why sleep plays such a key role in the management of chronic pain.[6]
Factors implicated in sleep propensity[edit | edit source]
- Time of day
- Previous sleep deprivation
- Medication and their effect on the CNS
- Age
- Physical state of an individual
- Cognitive state of an individual
- Irregular work hours, shift work
- Presence of a sleep disorder[6]
Sleep Deprivation and Appetite[edit | edit source]
During stages of sleep deprivation, an increase in appetite is noticeable during the increased levels of sleepiness. This is due to changes in two of the main hormones which govern the level of hunger. These hormones are[19]:
- Leptin – hunger decreasing hormone
- Ghrelin – hunger increasing hormone
Studies have shown that individuals who work against their natural circadian rhythm are at an increased risk of obesity, cardiovascular disease, etc.[20]
Sleep Patterns[edit | edit source]
Initially, sleep was regarded as monophasic in nature, but anthropologically it is viewed as a polyphasic system with at least two phases of position for the occurrence of sleep in a 24-hour cycle. The lesser-known phase is the one around the postprandial dip (a term used to refer to mild hypoglycaemia occurring after ingestion of a heavy meal) after lunchtime.[6]
In Mediterranean countries, siestas or a shorter period of sleep during the day is still a common occurrence and the health benefits of their diets and lifestyles can teach us a lot.
Monophasic Sleep[edit | edit source]
- “normal” sleeping period in today’s society
- Individual sleeps once per day, typically between 7 -9 hours a night
- This sleep pattern was influenced by the industrial revolution's longer-than-normal working hours. Other theories argue that the arrival of electricity and the increased exposure to bright lights caused a drop in melatonin levels and this could have a negative impact on sleep duration.[21]
Biphasic Sleep[edit | edit source]
- Typically, people sleep for a long-duration at night (5-6 hours) with a shorter period of sleep or siesta during the day (this period typically lasts about 30 minutes and is seen as an energy booster).
- Siestas can, however, last for longer, up to 90 minutes, and this allows for an individual to have one complete sleep cycle.
- Another form of biphasic sleep is segmented sleep. This includes two sleep periods, both at night.[21]
Polyphasic Sleep[edit | edit source]
- Polyphasic sleepers rest between 4 -6 times a day.[21]
- Various sleep combination categories exist. These are[21]:
- Everyman – long sleep of approximately 3 hours with approximately three 20-minute naps throughout the day
- Uberman – only 3 hours of sleep per day in the form of six 30 -minute naps throughout the day
- Dymaxion – Only 2 hours of sleep per day in the form of 30-minute naps every 6 hours
Assessment of Sleep[edit | edit source]
To promote effective behavioural change in sleeping patterns in ourselves and our patients it is important to have a good awareness of the level of sleepiness. Insomnia is likely to be prevalent in many healthcare workers and patients. Insomnia does not just relate to the inability to sleep, but also to the inability to stay asleep or an increased incidence of early wakefulness[6]. Sleep can be measured objectively and subjectively.
Objective Measures[edit | edit source]
Objective measures provide a measure of sleep latency in sleep laboratories during the day. These types of tests are reckoned to be the gold standard in the assessment of specific sleep-related outcome measures. One test that is commonly used is the Multiple Sleep Latency Test (MSLT). Another test that is less used is the Maintenance of Wakefulness Test (MWT).
Multiple Sleep Latency Test[edit | edit source]
The following facts apply to the Multiple Sleep Latency Test:[23]
- Test to identify excessive daytime sleepiness (such as feeling sleepy in situations where one should be awake or alert, for example driving a truck)
- Determines how long it takes an individual to fall asleep
- Identifies the phases of sleep (how quickly and often an individual enters REM sleep)
- Provides an indication of sleep propensity against the polysomnogram
- Standard test to diagnose idiopathic hypersomnia and narcolepsy
- Measures how quickly an individual fall asleep during the day in a quiet or non-stimulating environment
- Often the MSLT starts the morning following a Polysomnogram (PSG) and lasts one complete day
- With this test the individual tries to sleep in five scheduled naps, separated by two-hour breaks
- Test is often also called a “nap study”
- Each trial is situated in a quiet bedroom/ area
- Individual is connected to a device that detects sleep stages and procedure includes EEG, EOG, EMG and EKG
- MSLT can identify exactly when an individual fall asleep and if the individual entered REM sleep
- If an individual fall asleep, they are awakened after 15 minutes
- Nap trial also ends if an individual does not fall asleep within 20 minutes
- Individuals with narcolepsy – often have two or more REM periods during the MSLT
- Individuals with idiopathic hypersomnia – easily fall asleep, but do not reach REM sleep during nap trial
Maintenance of Wakefulness Test (MWT)[edit | edit source]
The maintenance of wakeful test involves the following:[23]
- Test is performed over a whole day
- Test is conducted while an individual is awake
- Instructs individuals to remain awake rather than fall asleep during periodic tests
- MWT helpful in the management of sleepy patients – especially for driving purposes
- Measures how alert an individual is during the day
- Determines if an individual can remain awake for a period in a quiet, relaxing and non-stimulating environment
- During the test – four to five periods of approximately 40 minutes each, with two-hour breaks in-between, the individual is asked to stay relaxed in a quiet, faintly-lit bedroom
- First trial usually starts 1.5 to 3 hours after the individual’s normal wake-up time
- Individual has breakfast one hour before the first relaxing period, and lunch after the second period
- Between test periods, an individual can read, watch TV, have a meal and move freely inside the test building.
- Individual can not go outside during the test as daylight is a factor that must be eliminated during the test
- During relaxing periods – individuals connected to a set of leads that monitor
- Heart activity (2-3 ECG leads)
- Brain activity (4 EEG leads)
- Chin muscle activity (3 leads)
- Left and right eye movements
- Test is terminated if an individual fall asleep for 90 seconds at any time during the relaxing period
- Sleep specialist analyses the data to determine the individual’s level of sleepiness during the day
Psychomotor Vigilance Task[edit | edit source]
The psychomotor vigilance task (PVT) involves:[24]
- Another way to objectively assess the level of sleepiness
- Well-validated measure of neurobehavioural alertness in sleep research
- Used to quantify the response to sleep loss through measuring the ability to sustain attention and promptly respond to salient signals
- PVT -requires a response to a stimulus (digital counter) by pressing a button as soon as the stimulus appears, this stops the stimulus counter and reaction time is displayed
- Accurate measure of neurobehavioral performance as it is
- Indicative of a fundamental aspect of waking cognitive function
- Easily performed and administered
- Minimally affected by learning/aptitude
- Brief
- Valid, reliable and sensitive
Advantages and Disadvantages of Objective Measurements of Sleep[edit | edit source]
The advantages of these methods include[23]:
- The use of advanced technology that cannot be used at home
- Precise and discrete methods – can distinguish between different sleep phases
- Gold standard for sleep evaluation
The disadvantages are[23]:
- Expensive methods
- Time-consuming methods
- Labour-intensive measures
- Require professional assistance
- Can only be done over a short period of time (one or two days)
- Another important functional disadvantage is that the assessment in a sleep laboratory is not done in the usual seep context of the patient at home, therefore it does not really measure a normal sleep situation.
Sleepiness and Safety[edit | edit source]
Simulated environments are good predictors of levels of sleepiness. Assessment of an individual’s performance (how much they perform and how well they perform) in a non-sleep deprived state versus a sleep-deprived state will provide information on the impact of sleep deprivation on performance. Keep in mind that in some performance assessments there is a significant learning curve effect and that needs to be considered when research is done in the area of sleep deprivation and performance.[6]
The assessment of sleepiness in road traffic accidents and in the aviation industry caused by fatigue has shown that simulation tests are effective. One way of physically assessing sleepiness is by monitoring eye closure measures as this has been shown as an indicator of fatigue. The eyelid position may be a stable physiological measure of drowsiness/sleepiness.[25] Other physiological measurements such as Melatonin metabolite may provide opportunities to assess the Circadian process, but further research is necessary.[6]
Subjective Measurement of Sleep[edit | edit source]
Subjective measures of sleep include sleep questionnaires, sleep diaries/logs, rating scales on the estimated level of sleepiness and hardware devices. These measures can provide a broad overview of the level of hours of sleep, the consistency in sleep, sleep propensity and insomnia. They are also a quick and cost-effective wat to estimate sleepiness.[26]
Epworth Sleepiness Scale[edit | edit source]
The Epworth sleepiness scale:[27]
- One of the most used measurements
- Simple, widely used self-administered questionnaire
- Measures levels of daytime sleepiness
- Individuals are asked to rate their usual chance of dozing off in eight typical situations typically encountered in daily life (such as sitting and reading, watching tv, a passenger in a car, etc)
- Higher scores indicate a higher propensity to fall asleep
- ESS is high in individuals with obstructive sleep apnea (OSA) and narcolepsy and low in individuals with insomnia
- Validation studies indicate a significant correlation between ESS score and sleep latency using PSG
Karolinska Sleepiness Scale[edit | edit source]
- Subjective rating scale that assesses sleepiness by using physiological and behavioural changes when sleepiness ratings are relatively high[26]
- Consists of a 9-point Likert scale
- Self-reported, subjective assessment of an individual’s level of drowsiness at the time
- Often used in research studies of shift work, sleep deprivation and driving
- Good correlation with PSG measurements and performance-based measures (worsening of performance is associated with increased KSS values)
Contact Hardware Devices to Assess Sleep[edit | edit source]
The prevalence of tracking sleep has increased in recent years. Predictive modelling based on heart rate assessment, respiratory rate and movement allows for certain devices to estimate levels of sleep and provide predictions in breakdowns in types of sleep. There are a variety of devices that can do this, such as the iWatch, ring devices and wearable tracker devices – a comparison of the performance and reliability of some of these hardware devices can be found here.
However, there is research indicating that fitness trackers and phone apps have the tendency to underestimate sleep disruptions and to overestimate total sleep times and sleep efficiency.[23]
Although subjective measurements of sleep are useful to highlight the awareness of sleep deficit, we do need objective measures as well. Many healthcare professionals and clinical populations report an increased level of sleep restriction. This leads to many professionals accepting a new baseline of decreased alertness and performance as well as changes in mood. The detriments of this can be reversed, but it can also have long-term ramifications on physical, mental and emotional health. It is not possible to repay sleep debt and the impact of sleep restriction is constant and will most likely remain.[6]
Conclusion[edit | edit source]
There are two separate, but interrelated processes involved in the governing of sleep – the homeostatic sleep drive and the circadian rhythm. These processes can be influenced by external factors such as physical, mental and physiological conditions, the level of lighting and even the work patterns in one’s profession. Both objective and subjective measurement of sleep has a role and is needed in making behavioural changes.[6]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Borbély AA, Daan S, Wirz‐Justice A, Deboer T. The two‐process model of sleep regulation: a reappraisal. Journal of sleep research. 2016 Apr;25(2):131-43.
- ↑ Borbély AA, Daan S, Wirz‐Justice A, Deboer T. The two‐process model of sleep regulation: a reappraisal. Journal of sleep research. 2016 Apr;25(2):131-43.
- ↑ Sleep Health Foundation. Sleep Regulation - the two processes that control when and why we sleep. Published on 20 May 2020. Available from https://www.youtube.com/watch?v=IDs40y11XqI&feature=emb_logo (last accessed 24 July 2020)
- ↑ Bjorness TE, Greene RW. Adenosine and sleep. Current neuropharmacology. 2009 Sep 1;7(3):238-45.
- ↑ Ribeiro JA, Sebastiao AM. Caffeine and adenosine. Journal of Alzheimer's Disease. 2010 Apr 14;20(s1):S3-15.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 Whelehan, D. How we sleep. Course, Plus. 2020
- ↑ Zuccarelli L, Galasso L, Turner R, Coffey EJ, Bessone L, Strapazzon G. Human physiology during exposure to the cave environment: a systematic review with implications for aerospace medicine. Frontiers in physiology. 2019 Apr 24;10:442.
- ↑ Moore RY. Suprachiasmatic nucleus in sleep–wake regulation. Sleep medicine. 2007 Dec 1;8:27-33.
- ↑ Schwartz WJ, Klerman EB. Circadian Neurobiology and the Physiologic Regulation of Sleep and Wakefulness. Neurologic clinics. 2019 Aug 1;37(3):475-86.
- ↑ Dijk DJ, Landolt HP. Sleep physiology, circadian rhythms, waking performance and the development of sleep-wake therapeutics. Sleep-Wake Neurobiology and Pharmacology. 2019:441-81.
- ↑ Ezenwanne EB. Current concepts in the neurophysiologic basis of sleep; a review. Annals of medical and health sciences research. 2011;1(2):173-80.
- ↑ Reid KJ, Kräuchi K, Grimaldi D, Sbarboro J, Attarian H, Zee PC. 0015 Manipulating Body Temperature: Effects on Sleep in Postmenopausal Women. Sleep. 2020 Apr;43(Supplement_1):A6-7.
- ↑ SciShow. Circadian Rhythm and Your Brain's Clock. Published 10 January 2014. Available from https://www.youtube.com/watch?v=UbQ0RxQu2gM (last accessed 24 July 2020)
- ↑ 14.0 14.1 14.2 Daan S, Beersma DG, Borbély AA. Timing of human sleep: recovery process gated by a circadian pacemaker. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology. 1984 Feb 1;246(2):R161-83.
- ↑ 15.0 15.1 de Zeeuw J, Wisniewski S, Papakonstantinou A, Bes F, Wahnschaffe A, Zaleska M, Kunz D, Münch M. The alerting effect of the wake maintenance zone during 40 hours of sleep deprivation. Scientific reports. 2018 Jul 20;8(1):1-1.
- ↑ Crowley SJ, Acebo C, Carskadon MA. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep medicine. 2007 Sep 1;8(6):602-12.
- ↑ The BioClock Studio. The 2-Process Model of Sleep. Published on 30 September 2016. Available from https://www.youtube.com/watch?v=k9iafVwln2Y (last accessed 24 July 2020)
- ↑ Johns MW. Sleepiness in different situations measured by the Epworth Sleepiness Scale. Sleep. 1994 Dec 1;17(8):703-10.
- ↑ Morselli L, Leproult R, Balbo M, Spiegel K. Role of sleep duration in the regulation of glucose metabolism and appetite. Best practice & research Clinical endocrinology & metabolism. 2010 Oct 1;24(5):687-702.
- ↑ St-Onge MP, O'Keeffe M, Roberts AL, RoyChoudhury A, Laferrère B. Short sleep duration, glucose dysregulation and hormonal regulation of appetite in men and women. Sleep. 2012 Nov 1;35(11):1503-10.
- ↑ 21.0 21.1 21.2 21.3 Medical News Today. Types of Sleep Patterns. Available from https://www.medicalnewstoday.com/articles/319425#types-of-sleep-patterns (last accessed 24 July 2020)
- ↑ SciShow. What do scientists really know about polyphasic sleep? Published on 21 June 2018. Available from https://www.youtube.com/watch?v=-wXppi_OfEo. (last accessed 24 July 2020)
- ↑ 23.0 23.1 23.2 23.3 23.4 Ibáñez V, Silva J, Cauli O. A survey on sleep assessment methods. PeerJ. 2018 May 25;6:e4849.
- ↑ Matsangas P, Shattuck NL. Sleep Quality, Occupational Factors, and Psychomotor Vigilance Performance in US Navy Sailors. Sleep. 2020 Jun 12.
- ↑ Jackson ML, Raj S, Croft RJ, Hayley AC, Downey LA, Kennedy GA, Howard ME. Slow eyelid closure as a measure of driver drowsiness and its relationship to performance. Traffic injury prevention. 2016 Apr 2;17(3):251-7.
- ↑ 26.0 26.1 Miley AÅ, Kecklund G, Åkerstedt T. Comparing two versions of the Karolinska Sleepiness Scale (KSS). Sleep and biological rhythms. 2016 Jul 1;14(3):257-60.
- ↑ Walker NA, Sunderram J, Zhang P, Lu SE, Scharf MT. Clinical utility of the Epworth sleepiness scale. Sleep and Breathing. 2020 Jan 14:1-7.