Foot and Ankle Assessment: Difference between revisions
No edit summary |
No edit summary |
||
| (32 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Ewa Jaraczewska|Ewa Jaraczewska]] | '''Original Editor '''- [[User:Ewa Jaraczewska|Ewa Jaraczewska]] based on the course presented by [https://members.physio-pedia.com/course_tutor/helene-simpson/ Helene Simpson] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Assessment Goal == | ||
[[File:Ankle image.jpeg|right|frameless|250x250px|Ankle]] | |||
The goal of the assessment is to: | |||
* Determine the extent of the injury | |||
* Identify what has been injured | |||
* Establish a framework that can be negotiated with the patient regarding: | |||
** Timeline | |||
** Further referral | |||
** Treatment plan | |||
** Treatment strategy | |||
== Subjective == | |||
=== Patient Intake === | === Patient Intake === | ||
Gathering information during the history provides the clinician with clues as to what structure is likely affected, further guiding the physical examination. For example, the mechanism of injury is important as it provides information on what forces went through what structure, and in what direction. This will further provide information on what tissues and/or structures are likely stretched or damaged. | Gathering information during the history provides the clinician with clues as to what structure is likely affected, further guiding the physical examination. For example, the mechanism of injury is important as it provides information on what forces went through what structure, and in what direction. This will further provide information on what tissues and/or structures are likely stretched or damaged. | ||
''Example'': | ''Example'': a valgus force may indicate a deltoid [[ligament]] sprain, whereas a varus force may be suggestive of injury to the anterior talofibular ligament (ATFL) and/or calcaneofibular ligament (CFL). | ||
The patient's history should include questions related to: | The patient's history should include questions related to: | ||
* | * The time of the injury (acute vs subacute vs chronic) | ||
* | * The mechanism of the injury and forces involved in the injury (loose vs locked position) | ||
* | * The activity that leads to the injury (an athletic event vs recreational activity vs [[Activities of Daily Living|activity of daily living]]) | ||
* | * Contributing factors (shoes, terrain, medical history, medications, general health) | ||
* | * Training history | ||
* | * Previous treatment (successes vs failures) | ||
The results from the interview should assist with establishing risk factors and precautions during objective assessment.<blockquote>At the end of the patient's interview, the physiotherapist must have a good idea of what needs to be examined objectively. The clinician must later determine if the results of the assessment match the subjective signs and symptoms the patient complained about. | The results from the interview should assist with establishing risk factors and precautions during the objective assessment.<blockquote>"At the end of the patient's interview, the physiotherapist must have a good idea of what needs to be examined objectively. The clinician must later determine if the results of the assessment match the subjective signs and symptoms the patient complained about." | ||
''Helene Simpson''</blockquote> | ''Helene Simpson''</blockquote> | ||
== Special Questions == | |||
Red [[The Flag System|flags]] are signs and symptoms found in the patient history and clinical examination that may be suggestive of serious pathology. If serious pathology is suspected, immediate referral to a medical doctor is indicated and the physiotherapist's concerns should be noted. | Red [[The Flag System|flags]] are signs and symptoms found in the patient history and clinical examination that may be suggestive of serious pathology. If serious pathology is suspected, immediate referral to a medical doctor is indicated and the physiotherapist's concerns should be noted. | ||
[[The Flag System|Red Flags]] specific to foot and ankle assessment | [[The Flag System|Red Flags]] specific to foot and ankle assessment: | ||
*Unable to bear weight | *Unable to bear weight: rule out fracture ([[Ottawa Ankle Rules|Ottawa Rule]]) | ||
*Bilateral pins and needles or numbness in the lower | *Bilateral pins and needles or numbness in the lower limbs | ||
*Bowel and bladder dysfunction (i.e. | *Bowel and bladder dysfunction (i.e. the patient is unable to feel themselves going to the toilet) | ||
*[[Incontinence]] | *[[Urinary Incontinence]] | ||
*Paraesthesia in the groin region | *Paraesthesia in the groin region | ||
*Loss of pulses in the lower leg (vascular compromise) | *Loss of pulses in the lower leg (vascular compromise) | ||
*Obvious deformity | *Obvious deformity | ||
*Joint dislocation | |||
*Positive [[Babinski Sign|Babinski sign]] | *Positive [[Babinski Sign|Babinski sign]] | ||
*Unable to calf raise: rule out [[Achilles Tendon|Achilles tendon]] rupture | |||
[[The Flag System|Yellow Flags]] specific to foot and ankle assessment | [[The Flag System|Yellow Flags]] specific to foot and ankle assessment: | ||
* Severity of symptoms do not match the subjective | * Severity of symptoms do not match the subjective information→more tests | ||
* Pain preventing objective | * Pain preventing objective assessment→detailed assessment delayed | ||
== Objective == | == Objective == | ||
| Line 60: | Line 63: | ||
* Observation | * Observation | ||
** | ** Perform with the patient in supine, sitting or standing | ||
** | ** Watch for the presence of swelling | ||
** | ** Assess [[skin]] colour | ||
** | ** Check skin temperature | ||
** | ** Watch for signs of muscle wasting | ||
** | ** Notice foot and toes deformities: bunions, hammertoes, claw toes, calluses | ||
* Posture | * Posture assessment | ||
** If the patient is able to stand: observe in quiet stance and assess weight-bearing distribution; pay attention to foot arches; observe walking with or without assistive device: watch for back deformity: scoliosis, lordosis, kyphosis; observe gait pathology, eg., Trendelenburg; notice any changes in the lower leg alignment: knee valgus or varus, foot pronation or supination; observe gait cycle: heel strike, toe-off. | ** If the patient is able to stand: observe in quiet stance and assess [[Weight bearing|weight-bearing]] distribution; pay attention to [[Arches of the Foot|foot arches]]; observe walking with or without [[Assistive Devices|assistive device]]: watch for back deformity: [[scoliosis]], [[Low Back Pain Related to Hyperlordosis|lordosis]], [[kyphosis]]; observe gait pathology, eg., [[Trendelenburg Gait|Trendelenburg]]; notice any changes in the lower leg alignment: knee valgus or varus, foot pronation or supination; observe [[Gait Cycle|gait cycle]]: heel strike, toe-off. | ||
** If the patient is unable to stand: observe in sitting, feet flat on the floor, assess the weight-bearing distribution and the patient's ability to take a load while preparing for sit to stand transition | ** If the patient is unable to stand: observe in sitting, feet flat on the floor, assess the weight-bearing distribution and the patient's ability to take a load while preparing for a sit to stand transition | ||
{{#ev: youtube|v=QnX5J-j79qQ|300}}<ref>Complete Musculoskeletal Exam of the Foot and Ankle. 2013. Available from: https://www.youtube.com/watch?v=QnX5J-j79qQ [last accessed 4/01/2022]</ref> | {{#ev: youtube|v=QnX5J-j79qQ|300}}<ref>Complete Musculoskeletal Exam of the Foot and Ankle. 2013. Available from: https://www.youtube.com/watch?v=QnX5J-j79qQ [last accessed 4/01/2022]</ref> | ||
[[File:Helene Simpson - Squeeze Test.jpg|thumb|Squeeze test]] | [[File: Helene Simpson - Squeeze Test.jpg|thumb|Squeeze test]] | ||
[[File:Helene Simpson - External Rotation Test.jpg|thumb|250x250px|External rotation test]] | [[File:Helene Simpson - External Rotation Test.jpg|thumb|250x250px|External rotation test]] | ||
[[File:Helene Simpson - Anterior Drawer Test.jpg|thumb|300x300px|Anterior Drawer Test]] | [[File:Helene Simpson - Anterior Drawer Test.jpg|thumb|300x300px|Anterior Drawer Test]] | ||
| Line 89: | Line 92: | ||
* Step-up | * Step-up | ||
* Step down + step overs | * Step down + step overs | ||
* [[Knee to Wall Test|Knee to wall test]] | * [[Knee to Wall Test|Knee to wall test]] - knee extended might relate more to the range of dorsiflexion in gait: helps to assess ankle dorsiflexion range of motion | ||
* [[Squeeze Test]]: helps to diagnose the syndesmotic ankle sprain | * [[Squeeze Test|Squeeze test]]: helps to diagnose the syndesmotic ankle sprain | ||
* External | * External rotation test: assesses the integrity of the syndesmotic ligaments | ||
* [[Anterior Drawer of the Ankle|Anterior drawer test]]: defines ankle mechanical instability | * [[Anterior Drawer of the Ankle|Anterior drawer test]]: defines ankle mechanical instability | ||
For | For high-level performance athletes, additional tests may include a jump or a hop. | ||
Additional details can be found on the [[Foot and Ankle Assessment-Investigations and Tests]] page. | Additional details can be found on the [[Foot and Ankle Assessment-Investigations and Tests]] page. | ||
==== Balance Assessment ==== | ==== Balance Assessment ==== | ||
The results of the [[balance]] assessment in the foot and ankle injury help to develop a sensory targeted rehabilitation programme that stimulates sensory receptors.<ref name=":2" /> The following are the examples of balance tests: | |||
* Static postural control : | |||
**[[Balance Error Scoring System]] (BESS) | |||
** Airplane balance test | |||
{{#ev: youtube|v=WysXgJNVOnk |300}}<ref>Doctors of Physical Therapy. Airplane Test. 2019. Available from: https://www.youtube.com/watch?v=WysXgJNVOnk [last accessed 18/01/2022]</ref> | |||
* Dynamic postural control | * Dynamic postural control | ||
** [[Star Excursion Balance Test]] (SEBT) | **[[Star Excursion Balance Test]] (SEBT)<ref name=":2">Wikstrom EA, McKeon PO. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5359082/pdf/nihms818000.pdf Predicting balance improvements following STARS treatments in chronic ankle instability participants]. J Sci Med Sport. 2017 Apr;20(4):356-361. doi: 10.1016/j.jsams.2016.09.003. Epub 2016 Sep 20. </ref> | ||
=== Palpation === | === Palpation === | ||
Palpation can be performed in supine, prone and or seated position. The clinician checks for points of tenderness: | |||
* On the medial, lateral, posterior and anterior part of the lower leg and around calcaneus | * On the medial, lateral, posterior and anterior part of the lower leg and the around [[calcaneus]] | ||
* Along joint lines | * Along joint lines | ||
| Line 118: | Line 124: | ||
=== Neurologic Assessment === | === Neurologic Assessment === | ||
The neurologic | The [[Neurological Assessment|neurologic assessment]] can assist the clinician to identify a potential neurological aetiology for the observed ankle or foot pathology. It includes peripheral [[Neuropathies|neuropathy]] or [[Introduction to Neuroanatomy|central nervous system]] impairment.<ref>Akoh CC, Phisitkul P. [https://books.google.pl/books?hl=en&lr=&id=OsyWDwAAQBAJ&oi=fnd&pg=PA183&dq=foot+and+ankle+neuro+examination&ots=Fa49SkztOY&sig=zczpRrRD0E0Ff1LMoRNKFoCLB40&redir_esc=y#v=onepage&q&f=false Clinical examination and radiographic assessment of the cavus foot.] Foot Ankle Clin. 2019 Jun 1;24(2):183-93.</ref> | ||
The complete neurological examination should include: | The complete neurological examination should include: | ||
| Line 130: | Line 136: | ||
* Plantar response (also known as the [[Babinski Sign|Babinski]] response) | * Plantar response (also known as the [[Babinski Sign|Babinski]] response) | ||
* [[Clonus of the Ankle Test|Clonus]] | * [[Clonus of the Ankle Test|Clonus]] | ||
This video demonstrates | This video demonstrates the anatomy of the dermatomes of the lower extremities. The sensory testing needs to be performed when pathology or referral from the lumbar spine is suspected: | ||
{{#ev: youtube|v= | {{#ev: youtube|v=jpcuPz9y7f4|300}}<ref>Anatomy - Dermatomes of the Lower Extremity. 2017. Available from: https://www.youtube.com/watch?v=jpcuPz9y7f4 [last accessed 5/01/2022]</ref> | ||
=== Vascular Assessment === | === Vascular Assessment === | ||
| Line 141: | Line 147: | ||
=== Movement Testing === | === Movement Testing === | ||
*''' | * When assessing ankle and foot '''active [[Range of Motion|range of motion]]''' (AROM) and '''passive range of motion''' (PROM), all testing positions must be comfortable for the patient. For example, ankle dorsiflexion and plantarflexion are assessed when the patient is prone. If the patient cannot get into the desired position, the clinician can modify the position and document this for future testing. When an ankle fracture is ruled out, but the patient cannot fully participate in the range of motion assessment because of pain, the best option is to immobilise the ankle joint and delay the examination for a few days until the pain subsides. | ||
** | |||
** | *The following are the basic range of motion testing in foot and ankle injury: | ||
** | **Plantarflexion(PF)/ dorsiflexion (DF) | ||
** | **Toe extension/ flexion | ||
**Pronation/supination | |||
**Big toe extension/ flexion | |||
This video demonstrates a complete foot and ankle ROM assessment: | This video demonstrates a complete foot and ankle ROM assessment: | ||
| Line 151: | Line 159: | ||
{{#ev: youtube|v=XkZp15vYNT0|300}}<ref>Foot & Ankle: Overview of ROM Assessment. 2020. Available from: https://www.youtube.com/watch?v=XkZp15vYNT0 [last accessed 5/01/2022]</ref> | {{#ev: youtube|v=XkZp15vYNT0|300}}<ref>Foot & Ankle: Overview of ROM Assessment. 2020. Available from: https://www.youtube.com/watch?v=XkZp15vYNT0 [last accessed 5/01/2022]</ref> | ||
* '''Joint mobility''': test each individual joint with a glide and compare to contralateral side and to normal values | * '''Joint mobility''': test each individual joint with a glide and compare to the contralateral side and to normal values | ||
These videos demonstrate specific joint mobility | These videos demonstrate specific joint mobility assessments: | ||
<div class="row"> | <div class="row"> | ||
| Line 166: | Line 174: | ||
</div> | </div> | ||
*'''Muscle Strength''': Specific active muscle tests (isometric and through range): [[Gastrocnemius]], [[ | *'''Muscle Strength''': Specific active muscle tests (isometric and through range): [[Gastrocnemius]], [[soleus]], [[Tibialis Posterior|tibialis posterior]], [[Tibialis Anterior|tibialis anterior]], [[Extensor Hallucis Longus|extensor hallucis longus]] and [[Extensor Hallucis Brevis|brevis]]/[[Flexor Hallucis Brevis|flexor hallucis brevis]], intrinsics. The strength of toe or digital purchase can be evaluated using the paper pullout test. <ref>Nery C, Raduan FC, Catena F, Mann TS, de Andrade MA, Baumfeld D. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4653840/pdf/13018_2015_Article_318.pdf Plantar plate radiofrequency and Weil osteotomy for subtle metatarsophalangeal joint instablity.] J Orthop Surg Res. 2015 Nov 19;10:180. doi: 10.1186/s13018-015-0318-1. </ref> | ||
This video demonstrates | This video demonstrates manual muscle testing of the lower extremities: | ||
{{#ev: youtube|v= | {{#ev: youtube|v=_DK0KupWCyc|300}}<ref>Manual Muscle Testing of the Lower Extremities. 2015. Available from: https://www.youtube.com/watch?v=_DK0KupWCyc[last accessed 5/01/2022]</ref> | ||
== Biomechanical Evaluation == | == Biomechanical Evaluation == | ||
A foot assessment can be used to classify foot type as well as to identify possible | A foot assessment can be used to classify foot type, as well as to identify possible aetiological factors relating to injury in order to properly prescribe therapeutic interventions. | ||
Details can be found on the [[Biomechanical Assessment of Foot and Ankle|Biomechanical Assessment of the Foot and Ankle]] page. | Details can be found on the [[Biomechanical Assessment of Foot and Ankle|Biomechanical Assessment of the Foot and Ankle]] page. | ||
| Line 179: | Line 187: | ||
=== Patient-Reported Outcomes (PROs) === | === Patient-Reported Outcomes (PROs) === | ||
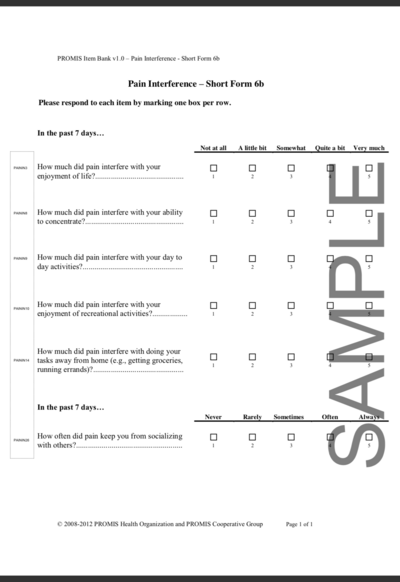
Patient-reported outcome measures allow clinicians to prioritise the outcomes most important to patients. In the foot and ankle assessment, it | Patient-reported [[Outcome Measures|outcome measures]] allow clinicians to prioritise the outcomes most important to patients. In the foot and ankle assessment, it has been determined that physical performance and pain interference were at the top of the patients' priorities when assessing their satisfaction with treatment.<ref name=":1" /><ref>Promis. Northwestern University 2022. Health Measures (Internet). Available from<nowiki/>https://www.healthmeasures.net/explore-measurement-systems/promis. Last access 6/01/2022</ref> | ||
[[File:PROMIS PI.png|thumb|582x582px|Patient Reported Outcome Measure: Pain Interference]] | [[File:PROMIS PI.png|thumb|582x582px|Patient Reported Outcome Measure: Pain Interference]] | ||
==== Patient-Reported Outcomes Measurement Information System Pain Interference (PROMIS PI) ==== | ==== Patient-Reported Outcomes Measurement Information System Pain Interference (PROMIS PI) ==== | ||
One | One PRO is the Patient-Reported Outcomes Measurement Information System (PROMIS) which takes information from multiple domains to assess patient-reported outcomes. Pain and function are two domains measured by [https://www.sralab.org/rehabilitation-measures/promis-pain-interference PROMIS PI], a patient-reported outcome measure that defines patients' satisfaction with foot and ankle treatment in response to improvement with these two domains. PROMIS PI detects pain at lower levels than the Visual Analogue Scale, a standard patient-reported pain scale. .<ref>Kendall R, Wagner B, Brodke D, Bounsanga J, Voss M, MS, Gu Y, Spiker R, Lawrence B, Hung M. [https://watermark.silverchair.com/pnx310.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAAtAwggLMBgkqhkiG9w0BBwagggK9MIICuQIBADCCArIGCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQMB_OQoTuwyPyH1wM2AgEQgIICg7_wj67xDZ6gkeSBM0LCdIRNhnfyq2TIY1gG_dtQc0UMn9bSiiJGR6cUitla2VpsQaaUrP_CPVhdNuS8DV7f8vJRuN6AJSsNIz90E6fF7J2VbxmZCT-TNf3r_tYyVKhCRpg9mnrwhk3HTcZCcukd1EvtWUjyT0i6Y-Z6P2yDKHPNpGl-6FM1zJKDgXZfysyZL8NOSCeHj-bd1DZnBTL0NK6E7UheHuDqp4QcL9ALCYj6rlIwxYwKlTLQIW9SxHYXgEnXNIjoK-n1ild4M5lFYfbesGmOur819tyIZ9auQO5_MNhSAOA_Mm1LqcPwBsOZFLn7L5Oc4bl6y-p0yWqvqpQw6faGzNw9Yu5uiRr0pftvtrzSamy9HB5yWcjRqUSiYiOp0u8YBikB9X5_2tWVt7Mk3_phLvvD6Rw0VtHKQsN4Xb5WZKmTCkPHlmonF2n3jJXiT37bYxUrhVxtmbNFmucbwpIGdavZopTxMKEpCw5J0iQbzFwexSaOGFGRvVpRSs-TH0Lu5TZCuRAmpVtihjTc_Wj3KAWW9jyYXVgn3-pPPbApM6WQipPmM4YJ5oDUlkoHBGzoD6vdiJpDbQOLbcQUKWYRBBeOf7sZq69-iMYTwM_b_OrAggDpLsg1_Ka9PSE-qcwGj867q-jF4horFg1zs6HYnMVanC9kxRVdMz6XBTSRuVQNIZ27dSXlCJ8WrLpMq56NxUQYEPxrQ_1XHqvYpxy6BIvX9y7BeM7CltH6lR2MqeCxvAg6JO7IO8URTmtMnvpkGAG5yhey57Y5nIoLGpODZFbdtsC1j_Z1QJDtDtsGmrNuBAy0UG1m5_mEJj-O1TwM95IwQRgC2bTN7sZbk-k The Relationship of PROMIS Pain Interference and Physical Function Scales]. Pain Medicine 2018 Sep; 19(9):1720–1724.</ref> <ref name=":1">Bernstein DN, Kelly M, Houck JR, Ketz JP, Flemister AS, DiGiovanni BF, Baumhauer JF, Oh I. [https://journals.sagepub.com/doi/pdf/10.1177/1071100718803314 PROMIS pain interference is superior vs numeric pain rating scale for pain assessment in foot and ankle patients.] Foot & ankle international. 2019 Feb;40(2):139-44.</ref> | ||
==== Visual Analogue Scale (VAS) ==== | ==== Visual Analogue Scale (VAS) ==== | ||
The [[Visual Analogue Scale]] (VAS) is a generic patient-reported pain scale that is used to assess the patient's perception of pain only. The scale may not be reliable in the assessment of the elderly population presenting with mild cognitive deficits or | The [[Visual Analogue Scale]] (VAS) is a generic patient-reported pain scale that is used to assess the patient's perception of pain only. The scale may not be reliable in the assessment of the elderly population presenting with mild cognitive deficits or who show difficulties in understanding the instructions for the VAS.<ref>Shazadeh Safavi P, Janney C, Jupiter D, Kunzler D, Bui R, Panchbhavi VK. [https://journals.sagepub.com/doi/pdf/10.1177/1938640018803747 A systematic review of the outcome evaluation tools for the foot and ankle]. Foot & ankle specialist. 2019 Oct;12(5):461-70.</ref> | ||
==== Foot and Ankle Ability Measure (FAAM) ==== | |||
The Foot and Ankle Ability Measure (FAAM) is a self-report outcome instrument developed to assess physical function for individuals with foot and ankle related impairments. This self-report outcome instrument is available in English, German, French and Persian. The Foot and Ankle Ability Measure is a 29-item questionnaire divided into two subscales: the Foot and Ankle Ability Measure, [https://cdn-links.lww.com/permalink/jg9/a/jg9_2021_10_25_shah_21-00103_sdc2.pdf 21-item Activities of Daily Living Subscale] and the Foot and Ankle Ability Measure, [https://cdn-links.lww.com/permalink/jg9/a/jg9_2021_10_25_shah_21-00103_sdc2.pdf 8-item Sports Subscale]. | |||
Detailed information is available on the [[Foot and Ankle Ability Measure]] page. | |||
== Conclusion == | == Conclusion == | ||
=== What→ so what→ now what === | === What→ so what→ now what === | ||
At the end of the examination, the clinician should return to the initial list of potential problems/suspected diagnoses and choose the three most likely diagnoses. | At the end of the examination, the clinician should return to the initial list of potential problems/suspected diagnoses and choose the three most likely diagnoses. | ||
The foot and ankle assessment is completed when the clinician is able to provide a response to | The foot and ankle assessment is completed when the clinician is able to provide a response to the following questions: | ||
* What has happened? | * ''What has happened?'' | ||
* ''What were the consequences of the incident?'' | |||
* What were the consequences of the incident? | |||
* ''How are the consequences of the incident going to be treated?'' | |||
* How the consequences of the incident | |||
** What is the treatment plan? | ** What is the treatment plan? | ||
** What is the treatment strategy? | ** What is the treatment strategy? | ||
| Line 212: | Line 219: | ||
== Virtual Foot and Ankle Assessment == | == Virtual Foot and Ankle Assessment == | ||
Telehealth is a well-established alternative to in-person visits as a response to the COVID pandemic and beyond.<ref name=":0">Eble SK, Hansen OB, Ellis SJ, Drakos MC. [https://journals.sagepub.com/doi/pdf/10.1177/1071100720941020 The Virtual Foot and Ankle Physical Examination]. Foot & Ankle International. 2020;41(8):1017-1026. </ref> Development of | Telehealth is a well-established alternative to in-person visits as a response to the COVID pandemic and beyond.<ref name=":0">Eble SK, Hansen OB, Ellis SJ, Drakos MC. [https://journals.sagepub.com/doi/pdf/10.1177/1071100720941020 The Virtual Foot and Ankle Physical Examination]. Foot & Ankle International. 2020;41(8):1017-1026. </ref> Development of objective assessment tools for telehealth is a priority in order to demonstrate the outcome of treatments provided via telehealth. | ||
Virtual | Virtual assessments for foot and ankle pathology have been developed and tested.<ref name=":0" /> The following is the guideline for the virtual examination. | ||
=== Pre-Visit === | === Pre-Visit === | ||
| Line 222: | Line 229: | ||
* Patient's past and present medical and surgical history | * Patient's past and present medical and surgical history | ||
* Medication and allergies | * Medication and allergies | ||
* Social history | * Social history | ||
Additional information may include biometrics (height and weight) and vital signs (HR, blood pressure, body temperature). | Additional information may include biometrics (height and weight) and vital signs (HR, blood pressure, body temperature). | ||
| Line 232: | Line 239: | ||
#* Patient in standing and seated | #* Patient in standing and seated | ||
#* Camera set up to provide front, side and back view of the foot and ankle | #* Camera set up to provide front, side and back view of the foot and ankle | ||
#* The elements of inspection are as | #* The elements of inspection are as follows: alignment, muscle atrophy, joint deformity, incisions, scarring, rash, swelling, ecchymosis, erythema. In addition, the plantar aspect of the foot must be examined for ulcers, abrasions, and skin breakdown. | ||
# Palpation | # Palpation | ||
#* Patient uses one finger to point to the area of maximal pain or discomfort | #* Patient uses one finger to point to the area of maximal pain or discomfort | ||
# Range of motion testing | # Range of motion testing | ||
#* Use web-based goniometer<ref>Ravi B, Kapoor M, Player D. Feasibility and reliability of a web-based smartphone application for joint position measurement. J Rehabil Med. 2021 May 10;53(5):jrm00188. </ref> | #* Use a web-based goniometer<ref>Ravi B, Kapoor M, Player D. Feasibility and reliability of a web-based smartphone application for joint position measurement. J Rehabil Med. 2021 May 10;53(5):jrm00188. </ref> | ||
#* Performed actively (patient's own muscle power) and passively (family member manipulates the joint) | #* Performed actively (patient's own muscle power) and passively (family member manipulates the joint) | ||
# Strength testing | # Strength testing | ||
| Line 243: | Line 250: | ||
# Functional assessment | # Functional assessment | ||
#* Gait observation | #* Gait observation | ||
# Neurovascular assessment | # Neurovascular assessment | ||
#* Patient touches the skin on both sides and reports differences, however sensory feedback from the patient’s own fingers touching the skin is a limitation. | #* Patient touches the skin on both sides and reports differences, however sensory feedback from the patient’s own fingers touching the skin is a limitation. | ||
Additional tests for flatfoot, cavovarus foot, hallux rigidus, and Achilles rupture may be added if the pathology is suspected.<ref name=":0" /> | Additional tests for flatfoot, cavovarus foot, hallux rigidus, and Achilles rupture may be added if the pathology is suspected.<ref name=":0" /> | ||
| Line 260: | Line 267: | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Rehabilitation]] | [[Category:Rehabilitation]] | ||
[[Category: | [[Category:Plus Content]] | ||
Latest revision as of 18:42, 17 January 2023
Original Editor - Ewa Jaraczewska based on the course presented by Helene Simpson
Top Contributors - Ewa Jaraczewska, Kim Jackson, Jess Bell, Lucinda hampton, Aminat Abolade, Nupur Smit Shah, Robin Leigh Tacchetti and Robin Tacchetti
Assessment Goal[edit | edit source]
The goal of the assessment is to:
- Determine the extent of the injury
- Identify what has been injured
- Establish a framework that can be negotiated with the patient regarding:
- Timeline
- Further referral
- Treatment plan
- Treatment strategy
Subjective[edit | edit source]
Patient Intake[edit | edit source]
Gathering information during the history provides the clinician with clues as to what structure is likely affected, further guiding the physical examination. For example, the mechanism of injury is important as it provides information on what forces went through what structure, and in what direction. This will further provide information on what tissues and/or structures are likely stretched or damaged.
Example: a valgus force may indicate a deltoid ligament sprain, whereas a varus force may be suggestive of injury to the anterior talofibular ligament (ATFL) and/or calcaneofibular ligament (CFL).
The patient's history should include questions related to:
- The time of the injury (acute vs subacute vs chronic)
- The mechanism of the injury and forces involved in the injury (loose vs locked position)
- The activity that leads to the injury (an athletic event vs recreational activity vs activity of daily living)
- Contributing factors (shoes, terrain, medical history, medications, general health)
- Training history
- Previous treatment (successes vs failures)
The results from the interview should assist with establishing risk factors and precautions during the objective assessment.
"At the end of the patient's interview, the physiotherapist must have a good idea of what needs to be examined objectively. The clinician must later determine if the results of the assessment match the subjective signs and symptoms the patient complained about." Helene Simpson
Special Questions[edit | edit source]
Red flags are signs and symptoms found in the patient history and clinical examination that may be suggestive of serious pathology. If serious pathology is suspected, immediate referral to a medical doctor is indicated and the physiotherapist's concerns should be noted.
Red Flags specific to foot and ankle assessment:
- Unable to bear weight: rule out fracture (Ottawa Rule)
- Bilateral pins and needles or numbness in the lower limbs
- Bowel and bladder dysfunction (i.e. the patient is unable to feel themselves going to the toilet)
- Urinary Incontinence
- Paraesthesia in the groin region
- Loss of pulses in the lower leg (vascular compromise)
- Obvious deformity
- Joint dislocation
- Positive Babinski sign
- Unable to calf raise: rule out Achilles tendon rupture
Yellow Flags specific to foot and ankle assessment:
- Severity of symptoms do not match the subjective information→more tests
- Pain preventing objective assessment→detailed assessment delayed
Objective[edit | edit source]
Observation[edit | edit source]
- Observation
- Perform with the patient in supine, sitting or standing
- Watch for the presence of swelling
- Assess skin colour
- Check skin temperature
- Watch for signs of muscle wasting
- Notice foot and toes deformities: bunions, hammertoes, claw toes, calluses
- Posture assessment
- If the patient is able to stand: observe in quiet stance and assess weight-bearing distribution; pay attention to foot arches; observe walking with or without assistive device: watch for back deformity: scoliosis, lordosis, kyphosis; observe gait pathology, eg., Trendelenburg; notice any changes in the lower leg alignment: knee valgus or varus, foot pronation or supination; observe gait cycle: heel strike, toe-off.
- If the patient is unable to stand: observe in sitting, feet flat on the floor, assess the weight-bearing distribution and the patient's ability to take a load while preparing for a sit to stand transition
Functional Tests[edit | edit source]
The choice of functional tests is based on the patient's signs and symptoms and the physiotherapist's initial list of suspected pathologies. It may include:
- Sit to stand
- Squat: defines the integrity of the syndesmosis joint
- Deep squat
- Tandem stance
- Lounge position
- Step forward and backwards: weight transfer
- Single leg stance: assess postural and balance control
- Step-up
- Step down + step overs
- Knee to wall test - knee extended might relate more to the range of dorsiflexion in gait: helps to assess ankle dorsiflexion range of motion
- Squeeze test: helps to diagnose the syndesmotic ankle sprain
- External rotation test: assesses the integrity of the syndesmotic ligaments
- Anterior drawer test: defines ankle mechanical instability
For high-level performance athletes, additional tests may include a jump or a hop.
Additional details can be found on the Foot and Ankle Assessment-Investigations and Tests page.
Balance Assessment[edit | edit source]
The results of the balance assessment in the foot and ankle injury help to develop a sensory targeted rehabilitation programme that stimulates sensory receptors.[2] The following are the examples of balance tests:
- Static postural control :
- Balance Error Scoring System (BESS)
- Airplane balance test
- Dynamic postural control
Palpation[edit | edit source]
Palpation can be performed in supine, prone and or seated position. The clinician checks for points of tenderness:
- On the medial, lateral, posterior and anterior part of the lower leg and the around calcaneus
- Along joint lines
- At the attachments of the medial and lateral ligaments
- At the Achilles tendon, peronei and other extrinsic muscles
Neurologic Assessment[edit | edit source]
The neurologic assessment can assist the clinician to identify a potential neurological aetiology for the observed ankle or foot pathology. It includes peripheral neuropathy or central nervous system impairment.[5]
The complete neurological examination should include:
- Inspection
- Reflex testing
- Achilles Tendon (S1)
- Patella Ligament (L3/L4)
- Muscle tone assessment
- Sensory testing (proprioception, light touch, sharp/dull)
- Plantar response (also known as the Babinski response)
- Clonus
This video demonstrates the anatomy of the dermatomes of the lower extremities. The sensory testing needs to be performed when pathology or referral from the lumbar spine is suspected:
Vascular Assessment[edit | edit source]
If compromised circulation is suspected, the clinician should palpate to assess pulses of the dorsalis pedis artery. The state of the vascular system can also be assessed by the response of symptoms to positions of dependence and elevation of the lower limbs.
Movement Testing[edit | edit source]
- When assessing ankle and foot active range of motion (AROM) and passive range of motion (PROM), all testing positions must be comfortable for the patient. For example, ankle dorsiflexion and plantarflexion are assessed when the patient is prone. If the patient cannot get into the desired position, the clinician can modify the position and document this for future testing. When an ankle fracture is ruled out, but the patient cannot fully participate in the range of motion assessment because of pain, the best option is to immobilise the ankle joint and delay the examination for a few days until the pain subsides.
- The following are the basic range of motion testing in foot and ankle injury:
- Plantarflexion(PF)/ dorsiflexion (DF)
- Toe extension/ flexion
- Pronation/supination
- Big toe extension/ flexion
This video demonstrates a complete foot and ankle ROM assessment:
- Joint mobility: test each individual joint with a glide and compare to the contralateral side and to normal values
These videos demonstrate specific joint mobility assessments:
- Muscle Strength: Specific active muscle tests (isometric and through range): Gastrocnemius, soleus, tibialis posterior, tibialis anterior, extensor hallucis longus and brevis/flexor hallucis brevis, intrinsics. The strength of toe or digital purchase can be evaluated using the paper pullout test. [13]
This video demonstrates manual muscle testing of the lower extremities:
Biomechanical Evaluation[edit | edit source]
A foot assessment can be used to classify foot type, as well as to identify possible aetiological factors relating to injury in order to properly prescribe therapeutic interventions.
Details can be found on the Biomechanical Assessment of the Foot and Ankle page.
Additional Testing[edit | edit source]
Patient-Reported Outcomes (PROs)[edit | edit source]
Patient-reported outcome measures allow clinicians to prioritise the outcomes most important to patients. In the foot and ankle assessment, it has been determined that physical performance and pain interference were at the top of the patients' priorities when assessing their satisfaction with treatment.[15][16]
Patient-Reported Outcomes Measurement Information System Pain Interference (PROMIS PI)[edit | edit source]
One PRO is the Patient-Reported Outcomes Measurement Information System (PROMIS) which takes information from multiple domains to assess patient-reported outcomes. Pain and function are two domains measured by PROMIS PI, a patient-reported outcome measure that defines patients' satisfaction with foot and ankle treatment in response to improvement with these two domains. PROMIS PI detects pain at lower levels than the Visual Analogue Scale, a standard patient-reported pain scale. .[17] [15]
Visual Analogue Scale (VAS)[edit | edit source]
The Visual Analogue Scale (VAS) is a generic patient-reported pain scale that is used to assess the patient's perception of pain only. The scale may not be reliable in the assessment of the elderly population presenting with mild cognitive deficits or who show difficulties in understanding the instructions for the VAS.[18]
Foot and Ankle Ability Measure (FAAM)[edit | edit source]
The Foot and Ankle Ability Measure (FAAM) is a self-report outcome instrument developed to assess physical function for individuals with foot and ankle related impairments. This self-report outcome instrument is available in English, German, French and Persian. The Foot and Ankle Ability Measure is a 29-item questionnaire divided into two subscales: the Foot and Ankle Ability Measure, 21-item Activities of Daily Living Subscale and the Foot and Ankle Ability Measure, 8-item Sports Subscale.
Detailed information is available on the Foot and Ankle Ability Measure page.
Conclusion[edit | edit source]
What→ so what→ now what[edit | edit source]
At the end of the examination, the clinician should return to the initial list of potential problems/suspected diagnoses and choose the three most likely diagnoses.
The foot and ankle assessment is completed when the clinician is able to provide a response to the following questions:
- What has happened?
- What were the consequences of the incident?
- How are the consequences of the incident going to be treated?
- What is the treatment plan?
- What is the treatment strategy?
- What are the short and long term goal?
- What is the timeline for goal completion?
Virtual Foot and Ankle Assessment[edit | edit source]
Telehealth is a well-established alternative to in-person visits as a response to the COVID pandemic and beyond.[19] Development of objective assessment tools for telehealth is a priority in order to demonstrate the outcome of treatments provided via telehealth.
Virtual assessments for foot and ankle pathology have been developed and tested.[19] The following is the guideline for the virtual examination.
Pre-Visit[edit | edit source]
Prior to the virtual visit, the patient should obtain a pre-visit form and information regarding wardrobe expectations and the camera set up during the examination. The pre-visit form needs to be completed by the patient or the caregiver and it consists of the questions regarding:[19]
- Patient's chief complaint and reason for the visit
- Patient's past and present medical and surgical history
- Medication and allergies
- Social history
Additional information may include biometrics (height and weight) and vital signs (HR, blood pressure, body temperature).
Virtual Assessment[edit | edit source]
The foot and ankle examination includes:
- Inspection
- Patient in standing and seated
- Camera set up to provide front, side and back view of the foot and ankle
- The elements of inspection are as follows: alignment, muscle atrophy, joint deformity, incisions, scarring, rash, swelling, ecchymosis, erythema. In addition, the plantar aspect of the foot must be examined for ulcers, abrasions, and skin breakdown.
- Palpation
- Patient uses one finger to point to the area of maximal pain or discomfort
- Range of motion testing
- Use a web-based goniometer[20]
- Performed actively (patient's own muscle power) and passively (family member manipulates the joint)
- Strength testing
- Assisted by the family member
- Exam performed on both sides at the same time and differences reported
- Functional assessment
- Gait observation
- Neurovascular assessment
- Patient touches the skin on both sides and reports differences, however sensory feedback from the patient’s own fingers touching the skin is a limitation.
Additional tests for flatfoot, cavovarus foot, hallux rigidus, and Achilles rupture may be added if the pathology is suspected.[19]
Resources[edit | edit source]
References[edit | edit source]
- ↑ Complete Musculoskeletal Exam of the Foot and Ankle. 2013. Available from: https://www.youtube.com/watch?v=QnX5J-j79qQ [last accessed 4/01/2022]
- ↑ 2.0 2.1 Wikstrom EA, McKeon PO. Predicting balance improvements following STARS treatments in chronic ankle instability participants. J Sci Med Sport. 2017 Apr;20(4):356-361. doi: 10.1016/j.jsams.2016.09.003. Epub 2016 Sep 20.
- ↑ Doctors of Physical Therapy. Airplane Test. 2019. Available from: https://www.youtube.com/watch?v=WysXgJNVOnk [last accessed 18/01/2022]
- ↑ Ascension Via Christi. Musculoskeletal Physical Exam: Ankle. 2011. Available from: https://www.youtube.com/watch?v=QiSm8rz2cmo&t=270 [last accessed 4/01/2022]
- ↑ Akoh CC, Phisitkul P. Clinical examination and radiographic assessment of the cavus foot. Foot Ankle Clin. 2019 Jun 1;24(2):183-93.
- ↑ Anatomy - Dermatomes of the Lower Extremity. 2017. Available from: https://www.youtube.com/watch?v=jpcuPz9y7f4 [last accessed 5/01/2022]
- ↑ Vascular assessment of the lower limb and clinical diagnostics. 2011. Available from: https://www.youtube.com/watch?v=nhmBL3N_igg&t=136s [last accessed 5/01/2022]
- ↑ Foot & Ankle: Overview of ROM Assessment. 2020. Available from: https://www.youtube.com/watch?v=XkZp15vYNT0 [last accessed 5/01/2022]
- ↑ Kris Porter DPT.Ankle Exam and Manual Therapy. 2016. https://www.youtube.com/watch?v=VN55vtFJOgc[last accessed 7/01/2022]
- ↑ Kris Porter DPT. Sub-Talar Exam and Manual Therapy. 2016. Available from:https://www.youtube.com/watch?v=_cRTUWlX-Tk [last accessed 7/01/2022]
- ↑ Kris Porter DPT.Mid-Foot (mid-tarsal) Examination. 2016. Available from: https://www.youtube.com/watch?v=qv62Qhn7DN8 [last accessed 7/01/2022]
- ↑ Kris Porter DPT. Hallux (Great Toe) Examination (1st MTP). 2016. Available from: https://www.youtube.com/watch?v=tH5gZ3My5Q0 [last accessed 7/01/2022]
- ↑ Nery C, Raduan FC, Catena F, Mann TS, de Andrade MA, Baumfeld D. Plantar plate radiofrequency and Weil osteotomy for subtle metatarsophalangeal joint instablity. J Orthop Surg Res. 2015 Nov 19;10:180. doi: 10.1186/s13018-015-0318-1.
- ↑ Manual Muscle Testing of the Lower Extremities. 2015. Available from: https://www.youtube.com/watch?v=_DK0KupWCyc[last accessed 5/01/2022]
- ↑ 15.0 15.1 Bernstein DN, Kelly M, Houck JR, Ketz JP, Flemister AS, DiGiovanni BF, Baumhauer JF, Oh I. PROMIS pain interference is superior vs numeric pain rating scale for pain assessment in foot and ankle patients. Foot & ankle international. 2019 Feb;40(2):139-44.
- ↑ Promis. Northwestern University 2022. Health Measures (Internet). Available fromhttps://www.healthmeasures.net/explore-measurement-systems/promis. Last access 6/01/2022
- ↑ Kendall R, Wagner B, Brodke D, Bounsanga J, Voss M, MS, Gu Y, Spiker R, Lawrence B, Hung M. The Relationship of PROMIS Pain Interference and Physical Function Scales. Pain Medicine 2018 Sep; 19(9):1720–1724.
- ↑ Shazadeh Safavi P, Janney C, Jupiter D, Kunzler D, Bui R, Panchbhavi VK. A systematic review of the outcome evaluation tools for the foot and ankle. Foot & ankle specialist. 2019 Oct;12(5):461-70.
- ↑ 19.0 19.1 19.2 19.3 Eble SK, Hansen OB, Ellis SJ, Drakos MC. The Virtual Foot and Ankle Physical Examination. Foot & Ankle International. 2020;41(8):1017-1026.
- ↑ Ravi B, Kapoor M, Player D. Feasibility and reliability of a web-based smartphone application for joint position measurement. J Rehabil Med. 2021 May 10;53(5):jrm00188.