Tensor Fascia Lata: Difference between revisions
No edit summary |
No edit summary |
||
| Line 9: | Line 9: | ||
* The TFL is most important clinically for assisting in [[pelvis]] stability while standing and walking.<ref name=":5">Trammell AP, Nahian A, Pilson H. [https://www.ncbi.nlm.nih.gov/books/NBK499870/ Anatomy, Bony Pelvis and Lower Limb, Tensor Fasciae Latae Muscl]e.Available: https://www.ncbi.nlm.nih.gov/books/NBK499870/ (accessed 27.12.2021)</ref>See [[Lumbo-Pelvic Stability]] | * The TFL is most important clinically for assisting in [[pelvis]] stability while standing and walking.<ref name=":5">Trammell AP, Nahian A, Pilson H. [https://www.ncbi.nlm.nih.gov/books/NBK499870/ Anatomy, Bony Pelvis and Lower Limb, Tensor Fasciae Latae Muscl]e.Available: https://www.ncbi.nlm.nih.gov/books/NBK499870/ (accessed 27.12.2021)</ref>See [[Lumbo-Pelvic Stability]] | ||
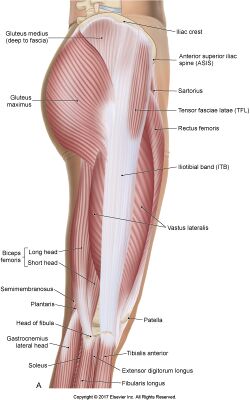
Image 1: TFLs position, lateral aspect thigh. | Image 1: TFLs position, lateral aspect thigh. | ||
==Origin, Insertion and Nerve Supply== | |||
== | [[File:TFL2.jpg|alt=|right|frameless]] | ||
[[File:TFL2.jpg| | |||
The TFL originates from the [[Pelvic Landmarks|anterior superior iliac spine]] (ASIS) and anterior aspect of the [[Ilium|iliac]] crest. It descends between and is attached to the deep [[fascia]] and the superficial fascia of the IT band (5 cm width). The TFL descends on the anterolateral aspect over the thigh, running superficially to the greater trochanter of the femur. | The TFL originates from the [[Pelvic Landmarks|anterior superior iliac spine]] (ASIS) and anterior aspect of the [[Ilium|iliac]] crest. It descends between and is attached to the deep [[fascia]] and the superficial fascia of the IT band (5 cm width). The TFL descends on the anterolateral aspect over the thigh, running superficially to the greater trochanter of the femur. | ||
It inserts distally to the IT track/band, which is comprised of the fascial [[aponeurosis]] of the gluteus maximus and the tensor fascia latae. The IT band then runs along the lateral aspect of the thigh, where it attaches to the lateral condyle of the tibia, specifically the Gerdy tubercle.<ref name=":5" /><ref name=":3">Miller A, Heckert KD, Davis BA.The 3-Minute Musculoskeletal & Peripheral Nerve Exam. New York: Demos Medical Publishing. 2009; p.116-117</ref> | It inserts distally to the IT track/band, which is comprised of the fascial [[aponeurosis]] of the gluteus maximus and the tensor fascia latae. The IT band then runs along the lateral aspect of the thigh, where it attaches to the lateral condyle of the tibia, specifically the Gerdy tubercle.<ref name=":5" /><ref name=":3">Miller A, Heckert KD, Davis BA.The 3-Minute Musculoskeletal & Peripheral Nerve Exam. New York: Demos Medical Publishing. 2009; p.116-117</ref> | ||
Innervation: The Tensor fasciae latae is innervated by superior gluteal nerve, originating from lumbar nerve 4, 5, and first sacral nerve(L4-S1) roots. It also innervates [[Gluteus Minimus|gluteus minimus]] and [[Gluteus Medius|medius]] muscles before terminating with innervation of tensor fasciae latae muscle<ref name=":1">Moore KL, Dalley AF, Agur AM. Clinically oriented anatomy. 7<sup>th</sup> ed. Baltimore, MD: Lippincott Williams & Wilkins, 2014</ref><ref name=":3" /> | |||
The Tensor fasciae latae is innervated by superior gluteal nerve, originating from lumbar nerve 4, 5, and first sacral nerve(L4-S1) roots. It also innervates [[Gluteus Minimus|gluteus minimus]] and [[Gluteus Medius|medius]] muscles before terminating with innervation of tensor fasciae latae muscle<ref name=":1">Moore KL, Dalley AF, Agur AM. Clinically oriented anatomy. 7<sup>th</sup> ed. Baltimore, MD: Lippincott Williams & Wilkins, 2014</ref><ref name=":3" /> | == Function == | ||
Though small in size, the TFL works with several muscle groups to assist in the movement and stabilization of both the hip and the knee: | |||
* Works with the gluteus medius and gluteus minimus to internally rotate and abduct the hip and with the gluteus maximus via the IT band to abduct the hip. It assists the rectus femoris in the flexion of the hip. | |||
* Acts on the tibia via the IT band's attachment to the Gerdy tubercle of the lateral tibia. The TFL is an accessory knee flexor, though its action is only seen once the knee is flexed beyond 30 degrees. Furthermore, it works with the IT band to stabilize the knee when it is in full extension. It also acts via the IT band in the lateral rotation of the tibia. This lateral rotation may be performed while the hip is in the abduction and medial rotation, as is seen when kicking a soccer ball. | |||
Clinically, the main function of the TFL is to assist in walking. The TFL does this by pulling the ilium inferiorly on the weight-bearing side, causing the contralateral hip to rise. The rise in the non-weight-bearing hip allows the leg to swing through without hitting the ground during the swing phase of the gait<ref name=":5" />y | |||
== Physiotherapy == | |||
== | The TFL can become clinically significant in cases of tightening, friction between over bony prominences, or through its attachment to the IT band. The TFL can become tight, especially in situations of prolonged shortening, such as in a seated position. A shortened TFL can lead to an anterior tilt of the pelvis and/or medial rotation of the femur. | ||
External [[Snapping Hip Syndrome|snapping hip syndrome]] is a condition where patients describe a palpable snap on the lateral aspect of their hip that occurs with a variety of movements. Though patients will often not complain of pain from this syndrome, it can progress to become painful. Treatment is typically conservative with oral NSAIDs and physical therapy. See link. | |||
[[Iliotibial Band Syndrome|IT band syndrome]] is a common overuse injury observed in runners and cyclists. Patients describe lateral-sided knee pain. [[File:Hip muscles 2.jpg|thumb]] | |||
== Assessment == | == Assessment == | ||
=== Power<ref name=":0" /><ref name=":3" /> === | === Power<ref name=":0">Hislop HJ, Montgomery J. Daniels and Worthingham's Muscle Testing: Techniques of Manual Examination. 8<sup>th</sup> ed. Missouri: Saunders Elsevier, 2007; p201-204</ref><ref name=":3" /> === | ||
The power test for the TFL is done in side-lying with hip in 45° of flexion for grade 5, 4 and 3 while for grade 2, 1 and 0, it is done in long sitting position. | The power test for the TFL is done in side-lying with hip in 45° of flexion for grade 5, 4 and 3 while for grade 2, 1 and 0, it is done in long sitting position. | ||
| Line 68: | Line 57: | ||
===Length=== | ===Length=== | ||
The TFL muscle is about 15cm in length<ref name=":0" /><ref name=":4" />. | The TFL muscle is about 15cm in length<ref name=":0" /><ref name=":4">Hubmer MG, Schwaiger N, Windisch G, Feigl G, Koch H, Haas, FM, Justich I, Scharnagl E. The vascular anatomy of the tensor fasciae latae perforator flap. Plastic Reconstructive Surgery: 2009;124(1):181-9. Doi: 10.1097/PRS.0b013e3181ab114c. PMID:19568071</ref>. | ||
== Resources == | == Resources == | ||
{| width="100%" cellspacing="1" cellpadding="1" | |||
|- | |||
|{{#ev:youtube|https://https://www.youtube.com/watch?v=C4gXjOyu-hg | |||
|500}} | |||
|} | |||
{| width="100%" cellspacing="1" cellpadding="1" | {| width="100%" cellspacing="1" cellpadding="1" | ||
|- | |- | ||
Revision as of 01:43, 27 December 2021
Description[edit | edit source]
The tensor fasciae latae (TFL) is a muscle of the proximal anterolateral thigh that lies between the superficial and deep fibres of the iliotibial (IT) band. There is high variability in muscle belly length, although, in most patients, the TFL muscle belly ends before the greater trochanter of the femur.
- The TFL works in conjunction with the gluteus maximus, gluteus medius, and gluteus minimus in a wide variety of hip movements, including flexion, abduction, and internal rotation.
- It acts, via the iliotibial (IT) band's attachment to the tibia, to assist with knee flexion and lateral rotation.
- The TFL is most important clinically for assisting in pelvis stability while standing and walking.[1]See Lumbo-Pelvic Stability
Image 1: TFLs position, lateral aspect thigh.
Origin, Insertion and Nerve Supply[edit | edit source]
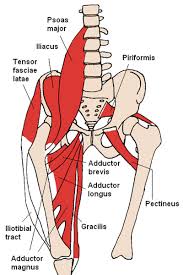
The TFL originates from the anterior superior iliac spine (ASIS) and anterior aspect of the iliac crest. It descends between and is attached to the deep fascia and the superficial fascia of the IT band (5 cm width). The TFL descends on the anterolateral aspect over the thigh, running superficially to the greater trochanter of the femur.
It inserts distally to the IT track/band, which is comprised of the fascial aponeurosis of the gluteus maximus and the tensor fascia latae. The IT band then runs along the lateral aspect of the thigh, where it attaches to the lateral condyle of the tibia, specifically the Gerdy tubercle.[1][2]
Innervation: The Tensor fasciae latae is innervated by superior gluteal nerve, originating from lumbar nerve 4, 5, and first sacral nerve(L4-S1) roots. It also innervates gluteus minimus and medius muscles before terminating with innervation of tensor fasciae latae muscle[3][2]
Function[edit | edit source]
Though small in size, the TFL works with several muscle groups to assist in the movement and stabilization of both the hip and the knee:
- Works with the gluteus medius and gluteus minimus to internally rotate and abduct the hip and with the gluteus maximus via the IT band to abduct the hip. It assists the rectus femoris in the flexion of the hip.
- Acts on the tibia via the IT band's attachment to the Gerdy tubercle of the lateral tibia. The TFL is an accessory knee flexor, though its action is only seen once the knee is flexed beyond 30 degrees. Furthermore, it works with the IT band to stabilize the knee when it is in full extension. It also acts via the IT band in the lateral rotation of the tibia. This lateral rotation may be performed while the hip is in the abduction and medial rotation, as is seen when kicking a soccer ball.
Clinically, the main function of the TFL is to assist in walking. The TFL does this by pulling the ilium inferiorly on the weight-bearing side, causing the contralateral hip to rise. The rise in the non-weight-bearing hip allows the leg to swing through without hitting the ground during the swing phase of the gait[1]y
Physiotherapy[edit | edit source]
The TFL can become clinically significant in cases of tightening, friction between over bony prominences, or through its attachment to the IT band. The TFL can become tight, especially in situations of prolonged shortening, such as in a seated position. A shortened TFL can lead to an anterior tilt of the pelvis and/or medial rotation of the femur.
External snapping hip syndrome is a condition where patients describe a palpable snap on the lateral aspect of their hip that occurs with a variety of movements. Though patients will often not complain of pain from this syndrome, it can progress to become painful. Treatment is typically conservative with oral NSAIDs and physical therapy. See link.
IT band syndrome is a common overuse injury observed in runners and cyclists. Patients describe lateral-sided knee pain.
Assessment[edit | edit source]
Power[4][2][edit | edit source]
The power test for the TFL is done in side-lying with hip in 45° of flexion for grade 5, 4 and 3 while for grade 2, 1 and 0, it is done in long sitting position.
The therapist is situated behind the patient with one hand is placed at the lateral surfece of the topmost thigh immediately above the knee, given downwards pressure and the other hand at the iliac crest for stability. the patient is asked to abduct against resistance.
Grade 5 is given if the patient is able to abduct and maintain position at end range against maximal resistance.
Grade 4 is given if the patient is able to abduct and maintain position at end range against moderate resistance.
Grade 3 is given if the patient is able to abduct and maintain position at end range against no resistance except gravity.
The therapist stands at the side of the limb being assessed one hand is place at the ankle serving to reduced friction between the limb and the plinth while the other hand is placed at the proximal anterolateral thigh. The patient is asked to move the limb towards the therapist.
Grade 3 is given if the patient is able to abduct to 30° and maintain position at end range.
For grade 1 and 0, the starting position is the same for grade 3 assessment but the hand placement of the therapist changes;one hand is placed at the the lateral side of the thigh immediately above the knee while the other hand is placed at the proximal anterolateral thigh for ease of TFL palpation.The patient is asked to move the limb towards the therapist.
Grade 1 is given if therapist is able to feel contraction of the muscle and grade 0 is given if no contraction is palpable.
Palpation[3][4][edit | edit source]
Palpation of TFL can be done in any of the aforementioned starting position in muscle power testing. One hand is placed at the the lateral side of the thigh immediately above the knee while the other hand is placed at the proximal anterolateral thigh and the patient is instructed to abduct(move the limb being tested away from the contralateral limb) the limb being assessed. TFL can then be easily palpable at end range of the motion.
Length[edit | edit source]
The TFL muscle is about 15cm in length[4][5].
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Trammell AP, Nahian A, Pilson H. Anatomy, Bony Pelvis and Lower Limb, Tensor Fasciae Latae Muscle.Available: https://www.ncbi.nlm.nih.gov/books/NBK499870/ (accessed 27.12.2021)
- ↑ 2.0 2.1 2.2 Miller A, Heckert KD, Davis BA.The 3-Minute Musculoskeletal & Peripheral Nerve Exam. New York: Demos Medical Publishing. 2009; p.116-117
- ↑ 3.0 3.1 Moore KL, Dalley AF, Agur AM. Clinically oriented anatomy. 7th ed. Baltimore, MD: Lippincott Williams & Wilkins, 2014
- ↑ 4.0 4.1 4.2 Hislop HJ, Montgomery J. Daniels and Worthingham's Muscle Testing: Techniques of Manual Examination. 8th ed. Missouri: Saunders Elsevier, 2007; p201-204
- ↑ Hubmer MG, Schwaiger N, Windisch G, Feigl G, Koch H, Haas, FM, Justich I, Scharnagl E. The vascular anatomy of the tensor fasciae latae perforator flap. Plastic Reconstructive Surgery: 2009;124(1):181-9. Doi: 10.1097/PRS.0b013e3181ab114c. PMID:19568071