Osteitis Pubis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 38: | Line 38: | ||
* Dynamic instability of the pubic symphysis can be observed on the flamingo view (obtained by double- and single-legged stance positions bilaterally on a pelvic anterior-posterior radiograph). Greater than 2 mm of subluxation is considered a positive finding for symphyseal instability. | * Dynamic instability of the pubic symphysis can be observed on the flamingo view (obtained by double- and single-legged stance positions bilaterally on a pelvic anterior-posterior radiograph). Greater than 2 mm of subluxation is considered a positive finding for symphyseal instability. | ||
* MRI has become the imaging modality of choice. MRI has a high sensitivity for distinguishing between chronic and acute cases.<ref name=":4" /> | * MRI has become the imaging modality of choice. MRI has a high sensitivity for distinguishing between chronic and acute cases.<ref name=":4" /> | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Revision as of 02:07, 8 November 2021
Introduction[edit | edit source]
Osteitis pubis is defined as an idiopathic, inflammatory condition of the pubic symphysis and surrounding structures, but it is most likely related to overuse or trauma[1]. Osteitis pubis was first described in patients who had undergone suprapubic surgery, and it remains a well-known complication of invasive procedures about the pelvis. It may also occur as an inflammatory process in athletes[2].
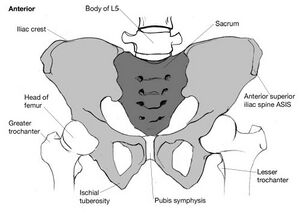
Image 1: anterior view pelvis.
Quick Facts[edit | edit source]
- Osteitis pubis is a rare cause of groin pain but is more common in the athletic patient, specifically soccer players, runners, and rugby players.
- Patients often present with groin pain made worse with activity.
- Plain radiographs and MRI may aid with the diagnosis.
- The condition is usually treated with NSAIDs, activity restriction, and physical therapy.
- In rare cases, surgical intervention may be required[3].
Clinical presentation[edit | edit source]
The presentation is typical with varying degrees of pelvic and/or perineal pain, reproduced on hip adduction.
Pathology[edit | edit source]
Although the aetiology is sometimes unknown, the most common causes are:
- pregnancy/childbirth
- high-level of athletic activity: see athletic pubalgia
- urological or gynaecological surgery
- trauma
- psoriatic arthritis
- ankylosing spondylitis[4]
Pathophysiology[edit | edit source]
The pubic symphysis is a non-synovial amphiarthrodial joint with an interposed fibrocartilaginous disc separating hyaline cartilage. The joint normally has minimal motion due to the static ligamentous complex. The pubic symphysis serves as the insertion point of the rectus abdominis and origin of the adductor complex. The antagonistic nature of the rectus abdominis, which elevates the pubic symphysis while the adductors depress the joint, serves as a nidus for the development of osteitis pubis—the repetitive use of the anterior pelvic musculature results in chronic tendinosis. The chronic muscle imbalance results in abnormal forces across the pubic symphysis, causing symphyseal instability, pubic bone stress reaction, and eventually degeneration of the hyaline cartilage. Another emerging theory poses that osteitis pubis develops secondary to increased compensatory motion across the joint because of limited motion elsewhere in the kinetic chain, such as in femoroacetabular impingement.[3]
Diagnosis[edit | edit source]
Both radiographs and MRI aid in the diagnosis of osteitis pubis. In the early stage, plain radiographs might appear normal.
- In chronic osteitis pubis, the pubic symphysis demonstrates lytic changes, sclerosis, and widening.
- Dynamic instability of the pubic symphysis can be observed on the flamingo view (obtained by double- and single-legged stance positions bilaterally on a pelvic anterior-posterior radiograph). Greater than 2 mm of subluxation is considered a positive finding for symphyseal instability.
- MRI has become the imaging modality of choice. MRI has a high sensitivity for distinguishing between chronic and acute cases.[4]
Differential Diagnosis[edit | edit source]
- Direct inguinal hernia,
- Indirect inguinal hernia,
- Sports hernia
- Athletic pubalgia,
- Adductor or iliopsoas injury,
- Pelvic stress fracture,
- Femoral neck stress fracture,
- Lumbar spine referred pain,
- Ilioinguinal neuralgia,
- Osteomyelitis can be considered but less common cause in athletes.[5]
Epidemiology[edit | edit source]
Osteitis pubis is a common cause of groin pain in athletes. The incidence in athletes is 0.5%–8%, with a higher incidence in distance runners and athletes participating in kicking sports, mostly in male soccer players with 10%–18% of injuries per year.[6]
Management and Return to Sport[edit | edit source]
Osteitis pubis is a self-limiting condition that improves by rest. Groin pain in osteitis pubis takes longer to resolve requiring extended period of rest but this is not possible for athletes. So treatment can vary from a conservative approach to surgical procedures depending upon the condition.
Conservative treatment[edit | edit source]
Conservative treatment includes rest, ice, reduced activity, anti-inflammatory drugs followed by an extensive rehabilitation program. The main aim is to correct muscular imbalances around the pubic symphysis which involves stretching and pelvic muscles strengthening. Physical therapy involving multimodal rehabilitation program is prescribed. In this program, patients are moved through different protocol stages after they are able to exercise without pain.
- Stage 1: This stage focuses on pain control and improving lumbo-pelvic stability. Stretching is performed except adductor and ischiopubic muscles. Cycling on an exercise bike is also started.[6][7]
- Stage 2: It involves using a swiss ball for resistance and strengthening exercises of the pelvis, abdominal, and gluteal muscles.[6][7]
- Stage 3 and 4: These include eccentric hip exercise, lunges, squats, and side-stepping with bands are done. Running is increased that involves a change of direction and pace. Kicking is only allowed at the end of the stage.[6][7] Most athletes return to the pre-injury level within 3 months(4 to 14 weeks) while successful follow-up may take 6 to 14 months.[8]
Injection Therapy[edit | edit source]
For the treatment of osteitis pubis, Corticosteriod injections into pubic symphysis are also used as an additional approach to accelerate return to sport. Some studies have reported pain relief at short-term follow-up but most are non-responders. So there is no strong evidence regarding the efficacy of short and long-term use of corticosteroids.[6]
Surgical Treatment[edit | edit source]
Surgery is performed only after conservative management fails. It may be indicated after at least 3 months of well-conduced rehabilitation program.Surgical intervention is required for 5%–10% of patients refractory to conservative approaches.[6]
References[edit | edit source]
- ↑ Up to date Osteitis Pubis Available:https://www.uptodate.com/contents/osteitis-pubis#! (accessed 8.11.2021)
- ↑ Gomella P, Mufarrij P. Osteitis pubis: a rare cause of suprapubic pain. Reviews in urology. 2017;19(3):156.available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5737342/ (accessed 8.11.2021)
- ↑ 3.0 3.1 Dirkx M, Vitale C. Osteitis Pubis. StatPearls [Internet]. 2021 Jan 1.Available:https://www.ncbi.nlm.nih.gov/books/NBK556168/ (accessed 8.11.2021)
- ↑ 4.0 4.1 Radiopedia Osteitis Pubis Available: https://radiopaedia.org/articles/osteitis-pubis(accessed 8.11.2021)
- ↑ Beatty T. Osteitis pubis in athletes. Current sports medicine reports. 2012 Mar 1;11(2):96-8.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Via AG, Frizziero A, Finotti P, Oliva F, Randelli F, Maffulli N. Management of osteitis pubis in athletes: rehabilitation and return to training–a review of the most recent literature. Open Access Journal of Sports Medicine. 2019;10:1.
- ↑ 7.0 7.1 7.2 Jardí J, Rodas G, Pedret C, Til L, Cusí M, Malliaropoulos N, Del Buono A, Maffulli N. Osteitis pubis: can early return to elite competition be contemplated?. Translational Medicine@ UniSa. 2014 Sep;10:52.
- ↑ Cheatham SW, Kolber MJ, Shimamura KK. The effectiveness of nonoperative rehabilitation programs for athletes diagnosed with osteitis pubis. Journal of sport rehabilitation. 2016 Dec 1;25(4):399-403.
- ↑ Pelvic pain Rehab Video-Osteitis Pubis. Available from: https://www.youtube.com/watch?v=7U5GLjR92Dk
.