Gait Deviations: Difference between revisions
No edit summary |
(Added physiology, examination, gait types, differential diagnosis and prognosis.) |
||
| Line 10: | Line 10: | ||
Causes of walking/gait disorders can range from arthritis to a neurological condition to something as simple as ill-fitting footwear. The variety of gait disorders call for different treatments. | Causes of walking/gait disorders can range from arthritis to a neurological condition to something as simple as ill-fitting footwear. The variety of gait disorders call for different treatments. | ||
== Etiology | == Etiology == | ||
The causes of gait disorders include neurological conditions (e.g. sensory or motor impairments), orthopedic problems (e.g. osteoarthritis and skeletal deformities) and medical conditions (e.g. heart failure, respiratory insufficiency, peripheral arterial occlusive disease and obesity). | The causes of gait disorders include neurological conditions (e.g. sensory or motor impairments), orthopedic problems (e.g. osteoarthritis and skeletal deformities) and medical conditions (e.g. heart failure, respiratory insufficiency, peripheral arterial occlusive disease and obesity). | ||
* In older age, gait disorders typically have several causes, which may include impaired proprioceptive function in polyneuropathy, poor vision, frontal gait disorder associated with vascular encephalopathy and osteoarthritis of the hips or knees. | * In older age, gait disorders typically have several causes, which may include impaired proprioceptive function in polyneuropathy, poor vision, frontal gait disorder associated with vascular encephalopathy and osteoarthritis of the hips or knees. | ||
* If a gait disorder has an acute onset, cerebrovascular, spinal and neuromuscular causes should be considered, as should adverse drug effects and psychiatric disorders.<ref>Wien Klin Wochenschr. 2017; 129(3): 81–95.Gait disorders in adults and the elderly Published online 2016 Oct Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5318488/#!po=20.3125 (accessed 21.7.2021)</ref> | * If a gait disorder has an acute onset, cerebrovascular, spinal and neuromuscular causes should be considered, as should adverse drug effects and psychiatric disorders.<ref name=":2">Wien Klin Wochenschr. 2017; 129(3): 81–95.Gait disorders in adults and the elderly Published online 2016 Oct Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5318488/#!po=20.3125 (accessed 21.7.2021)</ref> | ||
Some common causes are: | Some common causes are: | ||
| Line 24: | Line 24: | ||
* A [[Neurological Disorders|neurologic condition]] | * A [[Neurological Disorders|neurologic condition]] | ||
* Something as simple as ill-fitting shoes | * Something as simple as ill-fitting shoes | ||
== Epidemiology == | |||
Studies have demonstrated that gait disturbances occur as an individual age; these disturbances stemming from neurological and non-neurological causes. Studies have shown that while 85% of individuals 60-year-old have a normal gait, by the time they reach the age of 85, only 20% maintains normal gait. Gait disturbances are not commonly seen in the younger population unless they stem from a developmental or musculoskeletal etiology.<ref name=":0" /> | |||
== Physiological Basis of Gait == | |||
For normal [[gait]] many all of the following functions and systems are required to be intact: locomotor function (for initiating and sustaining rhythmic gait), balance, postural reflexes, sensory function and sensorimotor integration, motor control, the musculoskeletal apparatus and cardiopulmonary functions. Afferent nerves from the visual, vestibular and proprioceptive systems provide essential information on the position of the body and its parts. Efferent system comprises descending pathways including the pyramidal tract, peripheral nerves, neuromuscular end plate and muscles. | |||
The gait cycle is divided into a stance and swing phase. The stance phase constitutes approximately 60 % of the gait cycle and is subdivided into initial contact, loading response, mid-stance, terminal stance and pre-swing. The swing phase constitutes 40% and is subdivided into initial swing (toe-off), mid-swing (tibia vertical) and terminal swing, terminated by the heel striking the ground. Both feet are on the ground at the beginning and end of the stance phase, these two double support periods lasts for approximately 10–12 % of the gait cycle.<ref name=":2" /> | |||
== What are some types of gait disorders? == | == What are some types of gait disorders? == | ||
The | Gait disorders can be classified into musculoskeletal and neuromuscular | ||
=== Musculoskeletal === | |||
[[Gait: Antalgic|'''Antalgic gait'''.]] This type of gait is seen in patients with leg pain, as the patient weight bears on the painful leg for as short time as possible, resulting in short stance phase on the affected side. The patient appears to be limping.<ref name=":0" /> | |||
'''Vaulting gait.''' This type of gait is common in children with [[Leg Length Discrepancy|leg length discrepancy]]. It is defined by planterflexion, decreased hip and knee flexion of the short leg during stance phase, to ensure toe clearance of the swing limb. <ref name=":0" /><ref>Drevelle X, Villa C, Bonnet X, Loiret I, Fodé P, Pillet H. Vaulting quantification during level walking of transfemoral amputees. Clinical Biomechanics. 2014 Jun 1;29(6):679-83.</ref> | |||
=== Neuromuscular === | |||
'''Spastic hemiparetic gait.''' It is characterized by unilateral leg extension and cirumduction, in which the paretic leg performs a lateral motion (circumduction ) during the swing phase. | |||
'''Spactic diplegic gait (scissors gait).''' It is characterized by bilateral leg extension and adduction, the legs appear to be stiff. When spacitcity in the adductors is marked it results in scissoring gait where the legs cross in scissors-like pattern. | |||
'''Steppage gait.''' In this gait the patient must lift the leg higher than usual and the patient is unable to stand or walk on their heel. It is cause by weakness in the ankle dosriflexors. | |||
'''Waddling gait (myopathic gait).''' In waddling gait weakness in the gluteus medius muscles leads the hip on the swinging side to drop during gait, in an attempt to counteract, the patient bends the trunk towards the other side, resulting in the gait to appear waddling. | |||
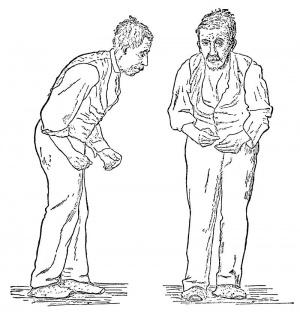
'''Parkinisonism gait.''' The gait is slow with a short step length and a narrow base. The feet are lifted less high than normally resulting in shuffling. Patients with [[Parkinson's|parkinsonism]] can develop a Freezing gait in which there is blockage of movement during turning or when approaching obstacles or narrow passages such as doors | |||
'''Cerebellar ataxic gait.''' The gait is broad based, insecure and lacks coordination. Leg movements and step length are irregular and variable. | |||
'''Senosry Ataxic gait.''' In this gait the patient’s proprioception is disturbed resulting the gait to appear broad based and insecure. The patient uses visual control to compensate for the disturbed proprioception. | |||
'''Hyperkinetic gait.''' this gait is seen in [[Basal Ganglia|basal ganglia]] disorders including [[chorea]], [[dystonia]] and [[Wilson's Disease|Wilson's disease]].<ref name=":0" /><ref name=":2" /> | |||
== Examination == | |||
The gait should be observed from all sides, while the patient walks a distance of at least several meters without obstacles and preferably without shoes. Normal walking appears to be rhythmical, flowing and effortless, with freely swinging legs and with an upright body posture. Normal walking is accompanied by movements of the head, the trunk and the arms. | |||
The parameters that should be clinically examined include step length, stride length, step width, rhythm, speed, posture, swinging of arms and legs and the duration and type of contact with the floor. | |||
A general [[Neurological Assessment|neurological examination]] should follow evaluation of gait. | |||
The examination is advised to be done most of the patient’s clothes removed to detect any orthopedic abnormalities such as asymmetries or postural abnormalities. <ref name=":2" /> | |||
== Treatment == | == Treatment == | ||
| Line 43: | Line 73: | ||
* Maintaining proper [[Foot Anatomy|foot]] alignment may require in-shoe splints or leg braces. A shoe lift may help in cases of an unequal leg length. | * Maintaining proper [[Foot Anatomy|foot]] alignment may require in-shoe splints or leg braces. A shoe lift may help in cases of an unequal leg length. | ||
* Medicines are available to treat [[arthritis]], [[Parkinson's|Parkinson’s]] disease and [[MS Multiple Sclerosis|multiple sclerosis]]. | * Medicines are available to treat [[arthritis]], [[Parkinson's|Parkinson’s]] disease and [[MS Multiple Sclerosis|multiple sclerosis]]. | ||
* [[Surgery and General Anaesthetic|Surgery]] or [[Prosthetics|prostheses]] may be recommended, such as [[Total Hip Replacement|hip]] and [[Total Knee Arthroplasty|knee replacement]] for persons with [[osteoarthritis]]<ref name=":1" /> | * [[Surgery and General Anaesthetic|Surgery]] or [[Prosthetics|prostheses]] may be recommended, such as [[Total Hip Replacement|hip]] and [[Total Knee Arthroplasty|knee replacement]] for persons with [[osteoarthritis]]<ref name=":1">Cleveland Clinic Gait disorders Available:https://my.clevelandclinic.org/health/symptoms/21092-gait-disorders (accessed 21.7.2021)</ref> | ||
See also comprehensive links in Resources below | See also comprehensive links in Resources below | ||
== Differential Diagnosis == | |||
There are numerous etiologies that could lead to gait disturbances. The following potential causes should be ruled out and to come up with a final diagnosis. | |||
'''Neurologic''': [[Parkinson's|Parkinson]], [[dementia]], delirium, [[stroke]], cerebellar dysfunction, [[MS Multiple Sclerosis|multiple sclerosis]], [[Amyotrophic Lateral Sclerosis|amyotrophic lateral sclerosis]] | |||
'''Metabolic''': [[Diabetes|Diabetes mellitus]], encephalopathy, [[obesity]], vitamin B12 deficiency, uremia | |||
'''Psychiatric''': Substance abuse, [[depression]], anxiety, malingering<ref name=":0" /> | |||
== Prognosis == | |||
The prognosis depends on the etiology. Metabolic etiologies of gait disturbances have a relatively good prognosis. If the metabolic disorder is addressed the patient mostly recovers without lasting symptoms. While neurologic conditions often have poor prognosis, as some neurologic conditions have no cure and must be treated symptomatically. <ref name=":0" /> | |||
== Resources == | == Resources == | ||
Revision as of 02:34, 16 August 2021
Original Editor - Lucinda hampton
Top Contributors - DeVonya Brown, Tony Varela, Nupur Smit Shah, Lucinda hampton, Mei Toone, Kim Jackson, Olajumoke Ogunleye, Jose Alvarado, Lilian Ashraf, Cindy John-Chu, Alexander Dettmers, Rucha Gadgil and Aminat Abolade
Introduction[edit | edit source]
Gait disturbances are described as any deviations from normal walking or gait. These disturbances stem from numerous etiologies. Due to their different clinical presentations, a high index of suspicion is required. The etiology can be determined through lab work, clinical presentation, and diagnostic testing. Furthermore, this entity can be subdivided into episodic and chronic disturbances. Gait disturbances have a tremendous impact on patients, especially on the quality of life, morbidity, and mortality.[1]
Causes of walking/gait disorders can range from arthritis to a neurological condition to something as simple as ill-fitting footwear. The variety of gait disorders call for different treatments.
Etiology[edit | edit source]
The causes of gait disorders include neurological conditions (e.g. sensory or motor impairments), orthopedic problems (e.g. osteoarthritis and skeletal deformities) and medical conditions (e.g. heart failure, respiratory insufficiency, peripheral arterial occlusive disease and obesity).
- In older age, gait disorders typically have several causes, which may include impaired proprioceptive function in polyneuropathy, poor vision, frontal gait disorder associated with vascular encephalopathy and osteoarthritis of the hips or knees.
- If a gait disorder has an acute onset, cerebrovascular, spinal and neuromuscular causes should be considered, as should adverse drug effects and psychiatric disorders.[2]
Some common causes are:
- A degenerative disease (such as arthritis)
- An inner ear disorder
- Stroke
- Foot conditions
- A neurologic condition
- Something as simple as ill-fitting shoes
Epidemiology[edit | edit source]
Studies have demonstrated that gait disturbances occur as an individual age; these disturbances stemming from neurological and non-neurological causes. Studies have shown that while 85% of individuals 60-year-old have a normal gait, by the time they reach the age of 85, only 20% maintains normal gait. Gait disturbances are not commonly seen in the younger population unless they stem from a developmental or musculoskeletal etiology.[1]
Physiological Basis of Gait[edit | edit source]
For normal gait many all of the following functions and systems are required to be intact: locomotor function (for initiating and sustaining rhythmic gait), balance, postural reflexes, sensory function and sensorimotor integration, motor control, the musculoskeletal apparatus and cardiopulmonary functions. Afferent nerves from the visual, vestibular and proprioceptive systems provide essential information on the position of the body and its parts. Efferent system comprises descending pathways including the pyramidal tract, peripheral nerves, neuromuscular end plate and muscles.
The gait cycle is divided into a stance and swing phase. The stance phase constitutes approximately 60 % of the gait cycle and is subdivided into initial contact, loading response, mid-stance, terminal stance and pre-swing. The swing phase constitutes 40% and is subdivided into initial swing (toe-off), mid-swing (tibia vertical) and terminal swing, terminated by the heel striking the ground. Both feet are on the ground at the beginning and end of the stance phase, these two double support periods lasts for approximately 10–12 % of the gait cycle.[2]
What are some types of gait disorders?[edit | edit source]
Gait disorders can be classified into musculoskeletal and neuromuscular
Musculoskeletal[edit | edit source]
Antalgic gait. This type of gait is seen in patients with leg pain, as the patient weight bears on the painful leg for as short time as possible, resulting in short stance phase on the affected side. The patient appears to be limping.[1]
Vaulting gait. This type of gait is common in children with leg length discrepancy. It is defined by planterflexion, decreased hip and knee flexion of the short leg during stance phase, to ensure toe clearance of the swing limb. [1][3]
Neuromuscular[edit | edit source]
Spastic hemiparetic gait. It is characterized by unilateral leg extension and cirumduction, in which the paretic leg performs a lateral motion (circumduction ) during the swing phase.
Spactic diplegic gait (scissors gait). It is characterized by bilateral leg extension and adduction, the legs appear to be stiff. When spacitcity in the adductors is marked it results in scissoring gait where the legs cross in scissors-like pattern.
Steppage gait. In this gait the patient must lift the leg higher than usual and the patient is unable to stand or walk on their heel. It is cause by weakness in the ankle dosriflexors.
Waddling gait (myopathic gait). In waddling gait weakness in the gluteus medius muscles leads the hip on the swinging side to drop during gait, in an attempt to counteract, the patient bends the trunk towards the other side, resulting in the gait to appear waddling.
Parkinisonism gait. The gait is slow with a short step length and a narrow base. The feet are lifted less high than normally resulting in shuffling. Patients with parkinsonism can develop a Freezing gait in which there is blockage of movement during turning or when approaching obstacles or narrow passages such as doors
Cerebellar ataxic gait. The gait is broad based, insecure and lacks coordination. Leg movements and step length are irregular and variable.
Senosry Ataxic gait. In this gait the patient’s proprioception is disturbed resulting the gait to appear broad based and insecure. The patient uses visual control to compensate for the disturbed proprioception.
Hyperkinetic gait. this gait is seen in basal ganglia disorders including chorea, dystonia and Wilson's disease.[1][2]
Examination[edit | edit source]
The gait should be observed from all sides, while the patient walks a distance of at least several meters without obstacles and preferably without shoes. Normal walking appears to be rhythmical, flowing and effortless, with freely swinging legs and with an upright body posture. Normal walking is accompanied by movements of the head, the trunk and the arms.
The parameters that should be clinically examined include step length, stride length, step width, rhythm, speed, posture, swinging of arms and legs and the duration and type of contact with the floor.
A general neurological examination should follow evaluation of gait.
The examination is advised to be done most of the patient’s clothes removed to detect any orthopedic abnormalities such as asymmetries or postural abnormalities. [2]
Treatment[edit | edit source]
It depends on the cause. Assistive devices such as canes and walkers may help in some cases in which balance is a problem.
- Physical therapy: may be appropriate in other cases to improve balance, strength and flexibility. You should also receive instruction in fall prevention.
- Maintaining proper foot alignment may require in-shoe splints or leg braces. A shoe lift may help in cases of an unequal leg length.
- Medicines are available to treat arthritis, Parkinson’s disease and multiple sclerosis.
- Surgery or prostheses may be recommended, such as hip and knee replacement for persons with osteoarthritis[4]
See also comprehensive links in Resources below
Differential Diagnosis[edit | edit source]
There are numerous etiologies that could lead to gait disturbances. The following potential causes should be ruled out and to come up with a final diagnosis.
Neurologic: Parkinson, dementia, delirium, stroke, cerebellar dysfunction, multiple sclerosis, amyotrophic lateral sclerosis
Metabolic: Diabetes mellitus, encephalopathy, obesity, vitamin B12 deficiency, uremia
Psychiatric: Substance abuse, depression, anxiety, malingering[1]
Prognosis[edit | edit source]
The prognosis depends on the etiology. Metabolic etiologies of gait disturbances have a relatively good prognosis. If the metabolic disorder is addressed the patient mostly recovers without lasting symptoms. While neurologic conditions often have poor prognosis, as some neurologic conditions have no cure and must be treated symptomatically. [1]
Resources[edit | edit source]
See also
- Gait
- Gait and Lower Limb Observation of Paediatrics - (GALLOP)
- Gait deviations in amputees
- Gait Training in Stroke
- Gait: Antalgic
- Gait Re-education in Parkinson's
- Gait Re-education in Multiple Sclerosis(MS)
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Ataullah AHM, De Jesus O. Gait Disturbances. [Updated 2021 Feb 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan Available:https://www.ncbi.nlm.nih.gov/books/NBK560610/#!po=60.7143 (accessed 21.7.2021)
- ↑ 2.0 2.1 2.2 2.3 Wien Klin Wochenschr. 2017; 129(3): 81–95.Gait disorders in adults and the elderly Published online 2016 Oct Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5318488/#!po=20.3125 (accessed 21.7.2021)
- ↑ Drevelle X, Villa C, Bonnet X, Loiret I, Fodé P, Pillet H. Vaulting quantification during level walking of transfemoral amputees. Clinical Biomechanics. 2014 Jun 1;29(6):679-83.
- ↑ Cleveland Clinic Gait disorders Available:https://my.clevelandclinic.org/health/symptoms/21092-gait-disorders (accessed 21.7.2021)