Sleep in Children with Attention Deficit Hyperactivity Disorder (ADHD)
Background[edit | edit source]
Attention Deficit Hyperactivity Disorder (ADHD) is one of the most prevalent neurodevelopmental disorders in childhood. The prevalence of ADHD among preschool children is around 8%[1], with the disorder being three to nine times more common in males than females[2].
Quality sleep plays a crucial role in body repair, memory integration, brain information processing, and emotional regulation. All these aspects collectively have substantial effects on children's physical development, cognitive growth, emotional regulation, attention, behaviour, metabolism, and immune function[3][4]. Poor sleep is associated with worse academic performance[5]. At a neurobiological level, the effect of sleep disorders is to heighten activity in the brain networks associated with emotions, potentially resulting in increased emotional lability[6].
Sleep problems are more common in children with ADHD (prevalence range from 30 to 74.6%, based on gender, age, ADHD subtype, co-morbidities, and use of medication[7]) than in children without ADHD[8][9][10][11][12][13][14][15][16][17]. Poor sleep quality and delayed bedtime can result in daytime fatigue, impacting mood, concentration, behaviour, and physical health[18]. Numerous studies have indicated a connection between sleep issues and heightened severity of ADHD symptoms or behavioural challenges in school-aged children with ADHD[8][17][19][20][21][22][23]. It is also associated with depressive symptoms[24], and poorer mental health of primary caregivers[25]. Sleep problems also have a significant impact on a child's quality of life[4][26][27][28]. Children experiencing moderate to severe sleep difficulties are more prone to miss school or be late for school, and their caregivers are more likely to be late for work when compared to children who didn't have sleep issues[25].
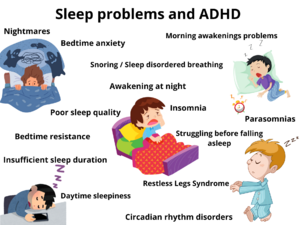
Sleep problems[edit | edit source]
The higher the ADHD symptoms, the more sleep problems a child has[17]. behavioural disruptions may affect sleep at night and functioning in the daytime in the following ways:
- Awakening at night[12][15][29][30][31][32]
- Bedtime anxiety[33][34]
- Bedtime resistance[15][25][35][36]
- Circadian rhythm sleep-wake disorders[35][37]
- Insomnia[8][26][33][38][37]
- Insufficient sleep duration[8][11][17][39][40][41]
- Nightmares[29][34][42]
- Parasomnias[33][34][37]
- Poor sleep quality[8][38][43][44]
- Restless Legs Syndrome (RLS)[15][37][45][46][47]
- Snoring and Sleep Disordered Breathing[15][25][29][37][48]
- Struggling before falling asleep[8][16][17][49][50][51]
- Daytime sleepiness[15][26][27][30]
- Morning awakenings problems[15][35][36]
The influence of sleep issues in children with ADHD can be intensified by their impact on parents[52][53]. Parents usually require their children to sleep for ten hours to have some personal time, and at least eight hours to maintain the patience needed for raising a child with ADHD[54]. When a child sleeps considerably less than this, and the parent must be awake while the child is to ensure their safety, the impact on parental well-being is significant[54]. The link between child sleep problems and family functioning may be directional, where parent behaviour influences child sleep, in turn, impacts parent mental health, thereby influencing family functioning[55].
The following issues can be experienced by their parents:
- Clinically depression or anxiety[25][53]
- Decreased level of effective parenting[56]
- Less sleep for the parents[51][56]
- Mood disturbances in parents[56]
- Parental daytime fatigue[56]
- Poorer parent-related daily functioning[20]
Physiological factors[edit | edit source]
There are several factors that can play a role in the sleep problems in children with ADHD:
- It is possible that factors such as rapid eye movement (REM) sleep abnormalities, which are frequently observed in children with ADHD[57], may play a significant role. This is because REM is linked to parasomnias like nightmare disorder, which often lead to awakenings[58], and it also affects neurobehavioural functioning in children with ADHD[59]. Behaviours indicative of parasomnias often include night terrors, confusional arousals, episodes of waking up screaming, increased motor activity such as sleepwalking, and enuresis (bedwetting)[37][60]. The use of medication and comorbidities (like anxiety) also increase the risk of parasomnias[37].
- Melatonin, a neurohormone, and its byproducts play a crucial role in circadian physiology, particularly in the initiation and maintenance of sleep. It is suggested that changes in melotonin levels contribute to disorders related to insomnia. Irregularities in the circadian release of melatonin have been observed in children with ADHD[45]. Apart from the melatonergic system, heightened activity in the orexinergic system and decreased serotonin activity are believed to contribute to insomnia in children with ADHD[61].
- Children with ADHD spend relatively more time in shallow sleep compared to typically developing children[43]. Due to the diminished sleep quality, children may experience heightened daytime sleepiness[26][62].
- Children with ADHD can develop nutritional deficiencies due to poor eating habits. The reduction in appetite caused by stimulant medication used for treating ADHD symptoms can result in inadequate food intake, which may also be a contributing factor to Restless Legs Syndrome. This disorder is associated with insomnia, poor sleep efficiency and daytime sleepiness[37].
- Sleep-related breathing disorders can have a significant impact on the symptoms of ADHD. Risk factors include low muscle tone, motor delays, and obesity, which are also common in ADHD[37]. Sleep disordered breathing often results in sleep fragmentation and excessive daytime sleepiness[45].
- It has been observed that children with ADHD have a difficulty transitioning from a state of stimulus-seeking alertness to the passive state of sleep. This difficulty in transitioning contributes to the onset of sleep insomnia[54].
Environmental factors[edit | edit source]
Environmental factors also play a significant role in the initiation of sleep[16][63]:
- Bedtime rituals
- Exposure to light
- Meal times
- Socials cues
Gender[edit | edit source]
The occurrence of symptoms related to sleep problems differs based on gender. In the age group of 6-14 years, parents report a higher prevalence of sleep disorder symptoms in boys (5.19%) compared to girls of the same age (3.67%)[64]. However, there is also evidence indicating that there is no significant difference between male and female children with sleep disorders[8]. Other literature provides information suggesting that girls have poorer sleep functioning than boys across most sleep functioning domains[65].
Sleep and medication[edit | edit source]
Certain medications, like stimulants prescribed for addressing hyperactivity/impulsivity symptoms or other psychotropic drugs used to manage concurrent psychiatric symptoms like anxiety, can potentially disrupt and prolong the time it takes to fall asleep[66][67][68][69][70]. Among children, an elevated dose of Methylphenidate is linked to an increase in sleep-related issues, especially among those with lower weight or BMI[71]. The degree of time it takes to fall asleep varies with different drugs, the dosis and the time of administration[67]. Commonly reported are >30 minutes[72][73]. For some children it is easier to fall asleep while on stimulants than off[54]. There are various reasons for this, firstly, for some children, the act of going to bed is an attention-demanding activity or routine that is more manageable when they are medicated. Another possible explanation is that the mechanism through which stimulants disrupt sleep may be linked not only to the alerting properties of the medication but also to interference with the onset of sleep as the drug's effects diminish and the child experiences a 'rebound' effect. Rebound is characterized by a period in which children become more irritable, reactive, and agitated, all of which may be considered contrary to the state of restfulness and calm required for inducing sleep[54].
Sleep hygiene[edit | edit source]
Sleep hygiene involves a series of behavioural, environmental, or cognitive adjustments designed to enhance sleep. There seems to be a relationship between poor sleep hygiene practices and sleep problems in children with ADHD[40][74]. Poor sleep hygiene is associated with increased bedtime resistance, increased daytime sleepiness and increased sleep duration problems[75].
There are several sleep hygiene factors associated with the sleep quality of children with ADHD:
- Co-sleeping (bed and room sharing): it has been linked to various sleep problems in children[76]
- Caffeinated drinks just before bedtime[77]
- Delayed or irregular bedtimes[77]
- Inconsistend bedtime routine[77]
- Television in the bedroom[77]
Sleep and screen time[edit | edit source]
Children with ADHD are found to have high amounts of screen time[39][78][79]. These children are less likely than typically developing children to stop playing at their own[80][81]. Parents may have difficulty in limiting screen time. Children with ADHD are especially susceptible to excessive media use, potentially influenced by altered reinforcement mechanisms[82]. There is a moderate association between ADHD and excessive internet use[83][84]. Media use might be employed as a coping mechanism to alleviate stress of handle negative emotions[85]. Children and adolescents with media devices in their bedroom have a shorter sleep duration and more daytime sleepiness[40][86][87]. Technology use is associated with more sleep problems and less time in bed[78].
Sleep and physical activity[edit | edit source]
Evidence suggests that participation in regular physical activity is associated with improved sleep problems[39][88]. Participation in physical activity and exercise may facilitate sleep regulation. It stimulates alterations in body temperature and triggers the production of melatonin before sleep, leading to subsequent changes in body thermoregulation during sleep cycles[89]. The rise in body temperature during exercise stimulates increased melatonin production, leading to a reduction in time it takes to fall asleep and an enhancement in both the quality and quantity of sleep[90].
Other poor sleep associated factors[edit | edit source]
There are more factors that might contribute to sleep problems in children with ADHD:
- Co-morbidities: mood disorders, anxiety disorders and tic disorders have been linked with significant sleep problems[40][91][92][93]. In children with ADHD, psychiatric comorbidities are very common: up to 87% have a comorbidity and 20% have three or more comorbidities[94]. Problems with sleep may also contribute to the development of comorbid anxiety or depression[95]. Depression is also associated with increased daytime sleepiness and overall sleep problems[65].
- Obesity: there seems to be an association between ADHD and obesity[39][96]. Obesity is correlated with sleep-disordered breachting and other sleep disorders[97], a short sleep duration[35] and a shorter time in bed[98].
- Sensory difficulties are associated with sleep difficulties in children with ADHD[99]. The challenges in regulation sensory perceptions result in difficulties when trying to initiate and sustain sleep[100].
- Children with more severe ADHD symptoms and lower motor proficiency may face an elevated risk of encountering sleep problems[101]. ADHD severity is associated with greater sleep problems[17].
- Parents' own sleep behaviour (sleep timing) might be associated with poorer quality sleep[102].
- Parents with ADHD themselfs often have troubles fostering healthy sleep habits and limiting screen time[103][104][105]. Consistent parenting has shown to decrease bedtime resistance and sleep anxiety[92].
- Poorer parent mental health is associated with child sleep problems[106].
- Parents tend to be less diligent in enforcing their children's bedtime routines on days without school compared to school days[16][75]. This inconsistency may impact the circadian rhythm and contribute to delayed sleep onset in general.
- Irregular schedules[34][107].
- Exposure at night to blue light sources (LED lights and light-emitting sources like smartphones or tablets[108][109][110]) and social media activities delay bedtimes and lead to shorter sleep duration[111].
- Children (ages 12-14) are 2.47 times more likely to consume more caffeine (soda, coffee, energy drinks) than their peers during later times of the day. Also, their caffeine use is associated with poorer subjective sleep functioning[112]. They may be using caffeine as a form of self-medication to enhance concentration[112][113].
Measurements of sleep functioning[edit | edit source]
Recognizing connections between sleep problems and ADHD is crucial for a comprehensive care plan in managing children with ADHD. Practitioners should regularly assess clinicall sleep issues by conducting a thorough sleep history and baseline measurements of sleep functioning[54]. There are several tools available, such as psychometrically validated questionnaires for both parents and children, and sleep diaries[114]. These tools can aid in identifying sleep problems:
- Questionnaires:
- Sleep diaries: these diaries entail having the parent or child (or both) document a child's sleeping and waking times along with relevant information, typically spanning over a period of several weeks[54]. Two weeks of baseline sleep diary recordings are adequate for outlining sleep patterns[120].
- Clinical Interviews: a simple user-friendly screening tool is the BEARS. B = Bedtime issues, E = Excessive day-time sleepiness, A = Awakenings, R = Regularity and duration of sleep, S = Snoring[121]. By using this format, every therapist can easily screen children for the most common sleep problems[54] and this tool significantly increased the amount of sleep information compared to other checklists[122].
- Tools for Sleep Hygiene: sleep hygiene training begins with a baseline assessment of sleep patterns with the help of an assessment tool such as:
Interventions[edit | edit source]
Correct treatment of sleep problems increase the life quality of the child with ADHD and also of the family[30]. The severity of ADHD can be reduced by improving the sleep of children with behaviouroral sleep interventions[8], or a sleep extension intervention[125], but using conventional interventions designed for typically developing children without addressing the fundamental deficits in ADHD may prove ineffective and might potentially exacerbate sleep-related challenges[37]. Sleep interventions may increase total sleep time and slightly increase quality of life, while behaviouroral sleep interventions probably decrease sleep disturbances and slightly decrease ADHD symptoms[126]. Even a brief behaviouroral sleep intervention can improve sleep problems[127][128].
Possible interventions might be:
- Drug treatments: medication management is frequently employed alongside behaviouroral and non-pharmacological interventions.
- Melatonin: studies of melatonin treatment demonstrate that in children with ADHD the use of melatonin is associated with increased sleep duration and decreased sleep latency[129][130][131][132]. Prolonged use of melatonin has been considered safe for children with ADHD[130][133]. Side effects are: bedwetting, headaches, nightmares, daytime sedation, abdominal pain or constipation[37].
- Clonidine: studies involving clonidine in children with ADHD have indicated reductions in sleep latency en nighttime awakenings[37]. Clonidine is classified as an alpha agonist. Side effects are: severe sedation at night, morning fatique, rebound awakening, early morning awakening and inability to return to sleep[37].
- Iron supplements: in children with ADHD and increased motor symptoms in sleep who have low ferritin levels, supplementation with iron might be beneficial[134].
- Suggested approaches for adressing sleep disruptions while using ADHD medication[135]:
- Monitoring: insomnia linked with stimulant use may diminish after 1-2 months[136].
- Assessing the possibility to discontinue using the medication.
- Implementing sleep hygiene and behaviouroral measures.
- Reviewing potential causes of sleep issues.
- Treating Restless Legs Syndrome.
- Adding small, short-acting stimulant doses in the early evening (if a rebound effects occurs).
- Reducing stimulant dosage.
- Switching to an alternative class of stimulant.
- Switching to an alternative formulation of the stimulant.
- Contemplating the use of a non-stimulant (for example: atomoxetine).
- Considering starting a melatonin treatment.
- Non-pharmacological sleep-related interventions might be important for treating sleep problems including those that focus on sleep hygiene, sensory based factors, parental stress and education[37].
- Sleep hygiene interventions seek to enhance sleep by education caregivers about factors that influence both the duration and quality of sleep[125]. Established sleep hygiene practices tailored for children have demonstrated to be effective for children with ADHD[92][137][138][139][140][141]. These practices include maintaining a consistent sleep-wake schedule, engaging in calming bedtime routines, having a appropriate bedroom environment (dark, quiet and comfortable in temperature), implementing a structured transition to sleep, steering clear of caffeine and excessive liquids, avoiding naps, refraining from strenuous exercise right before bedtime, minimizing exposure to electronic media close to bedtime, using the bed solely for sleeping and exposure to natural light during the daytime[37][54][142].
- Children with ADHD could benefit from strategies aimed at reducing problematic media use, such as removing screens from bedrooms and limiting late-night screen time. Studies have shown associations between problematic screen use and sleep issues[143][144].
- Relaxation strategies can be used to engage in calming bedtime routines[145][146][147]. Insomnia can be managed with progressive muscle relaxation techniques and visual imagery[148].
- Faded bedtime is a strategy where parents adjust the child's sleep schedule, moving this 15 minutes earlier each night[145][149][150]. It is important that children are not allowed to take a nap and parents set a time to wake up in the morning, making sure the child is exposed to sun in the morning. This strategy is helpful for children with a delayed sleep phase[148].
- Weekly feedback and reviewing the day's highlights in bed[146].
- Rewards for succesful nights of sleep[145][147][150][151]. For example: a child can earn tokens for a succesful night and ''cash-out'' for special rewards[148].
- Behaviouroral therapy is an intervention based on modifying behaviour to enhance individual well-being[148]. A behavioural sleep intervention is associated with small sustained improvements in child well-being[152]. Children who are not using ADHD medication or have parents experiencing depression might benefit from additional follow-up sleep sessions[152]. Research also suggest that a brief, individualized intervention might be more effective than a standardized intervention[128].
- Key behavioural sleep management strategies[153]:
- Sleep-onset problems: 'Adult fading' (a phased reduction of parental presence in the child's bedroom over a span of 7-10 days) and 'Checking method' (parents periodically check on the child at specified time intervals (2, 5, or 10 minutes, with increasing intervals over time)).
- Delayed sleep phase: 'Bedtime fading' (the child's bedtime is temporarily adjusted to a later time, corresponding with when they typically fall asleep, and is gradually shifted earlier. The child is then awakened at a predetermined morning time) and 'Early morning light exposure'.
- Limit setting sleep problems: 'Parent management strategies': (ignoring the child's protests and reinforcing compliance with bedtime routines. A 'Bedtime pass', allowing the child to leave the bedroom only once before falling asleep, can be utilized to encourage compliant behaviour), 'Bedtime fading' and 'Checking method'.
- Primary insomnia: 'Visual imagery and relaxation techniques', and 'Limiting time spent in bed (temporarily adjusting bedtime according to delayed sleep phase or engaging in a relaxing activity if the child struggles to sleep).
- Night-time anxiety: 'Visual imagery and relaxation techniques', 'Talking about the fears of the child during daytime instead of bedtime', 'Rewarding brave behaviour of the child' and 'Using a book to record worries'.
- Key behavioural sleep management strategies[153]:
- For a succesful behavioural sleep intervention, parent education is also important, as parents of children with sleep problems have high levels of stress and poor sleep. It is essential to tackle parental stress and offer education and training to parents. This is vital not only for minimizing risks but also for succesfully implementing behavioural interventions to address sleep issues in children[37]. Behavioural Parent Training could significantly improve various sleep domains in children with ADHD[154]. A brief parent-based sleep intervention also improves parental sleep and parenting stress[155].
- Sensory interventions are helping children who tend to be easily over-aroused by sensory stimuli. The utilization of tools like weighted blankets[156] or specific items such as ball-blankets, which engage sensory receptors and transmit inhibitory signals to the central nervous system, has demonstrated effectiveness in reducing sleep onset latency and intermittent awakenings[157].
- A weighted blanket is recognized as a cognitive aid that stimulated the senses, providing deep pressure on the body. The pressure exerted by the weighted blanket induces a sensation of being enveloped and enhances body awareness[158]. Parents noted positive effects when their children used weighted blankets, including: experiencing satisfactory sleep with improvements in falling asleep, uninterrupted sleep, and better sleep routines, achieving overall well-being with increased relaxation and reduced anxiety, and excelling in daily life with improvements in life balance, family functioning, and participation in school and leisure activities[159]. Children's experiences revealed that using weighted blankets improved their sleep, sleeping patterns, and the balance between sleep and activity, emotional regulation and daily functioning[160].
- For children with hyperactivity, it is crucial to emphasize the importance of steering clear of activities that may stimulate behaviour that result in motor activity and challenges in 'settling down'. Establishing calming routines is key to aiding these children in making an effective transition from wakefulness to sleep[37].
- For children with anxiety, it could be helpful to get treated with cognitive behavioural therapy for their anxiety, because this leads to a significant decrease in anxiety and improvements in sleep latency[161].
- Cognitive behavioural play therapy is an approach for teaching coping skills to children by combining cognitive behavioural therapy with pretend play[162]. Cognitive behavioural play therapy results could be effective for reducing anxiety and sleeping problems[162].
- Mindfulness meditation is a new approach to sleep disturbances and insomnia-related problems[163][164]. Evidence has demonstrated that mindfulness interventions significantly enhance attention and reduce hyperactivity and impulsivity in individuals with ADHD[165]. The Headspace digital mindfulness application significantly reduced anxiety and increased sleep in children with ADHD[166].
- Exercise interventions: since serveral studies linked exercise to better sleep it could be beneficial to provide an exercise intervention for children with ADHD[39][88]. Exercise interventions with higher levels of intensities should be provided to improve sleep quality[167]. Physical activity could improve sleep efficiency, sleep onset latency and wake after sleep onset[168][169].
- White noise (75dB of continuous white noise) decrease bedtime sleep latency and awakenings during the night. Results are the same wheter or not children were on ADHD medication[170].
- Other specific interventions:
- Better Nights/Better Days is a distance intervention for insomnia in school-aged children (with and without ADHD). Research demonstrate a significant reduction in sleep problems and it improved psychosocial functioning[151].
- MOBERO is a smartphone-based system to help families establish healthy morning and bedtime routines. It is associated with improvement in sleep habits, less bedtime resistance, increased sleep duration, less sleep anxiety and night wakenings, less parasomnias, less sleep disordered breathing and less daytime sleepiness[171].
- Sleep hygiene interventions seek to enhance sleep by education caregivers about factors that influence both the duration and quality of sleep[125]. Established sleep hygiene practices tailored for children have demonstrated to be effective for children with ADHD[92][137][138][139][140][141]. These practices include maintaining a consistent sleep-wake schedule, engaging in calming bedtime routines, having a appropriate bedroom environment (dark, quiet and comfortable in temperature), implementing a structured transition to sleep, steering clear of caffeine and excessive liquids, avoiding naps, refraining from strenuous exercise right before bedtime, minimizing exposure to electronic media close to bedtime, using the bed solely for sleeping and exposure to natural light during the daytime[37][54][142].
References[edit | edit source]
- ↑ Addanki SS, Chandradekaran V, Kandasamy P. Attention Deficit Hyperactivity Disorder in Preschool Children: A Cross-Sectional Study of Clinical Profile and Co-morbidity. Indian Journal of Psychological Medicine. 2023; 45(3): 257-262
- ↑ Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics. 2015; 135: e994-1001
- ↑ Ophoff D, Slaats MA, Boudewyns A, Glazemakers I, Van Hoorenbeeck K, Verhulst SL. Sleep disorders during childhood: a practical review. European Journal of Pediatrics. 2018; 177: 641-648
- ↑ 4.0 4.1 Medic G, Wille M, Hemels ME. Short- and long-term health consequences of sleep disruption. Nature and Science of Sleep. 2017; 19(9): 151-161
- ↑ Matsuoka M, Nagamitsu S, Iwasaki M, Iemura A, Yamashita Y, Maeda M. High incidence of sleep problems in children with developmental disorders: results of a questionnaire survey in a Japanese elementary school. Brain & Development. 2014; 36(1): 35-44
- ↑ Reynold KC, Patriquin M, Alfona CA, Loveland KA, Pearson DA. Parent-reported problematic sleep behaviors in children with comorbid autism spectrum disorder and attention-deficit/hyperactivity disorder. Research in Autism Spectrum Disorders. 2017; 39: 20-32
- ↑ Tsai MH, Hsu JF, Huang YS. Sleep problems in children with attention deficit/hyperactivity disorder: current status of knowledge and appropriate management. Current Psychiatry Reports. 2016; 18(8): 76
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 Yin H, Yang D, Yang L, Wu G. Relationship between sleep disorders and attention-deficit-hyperactivity disorder in children. Frontiers in Pediatrics. 2022; 10: 919572
- ↑ Hosiri T, Punyapas S, Sawangsri W. The Prevalence and Patterns of Sleep Problem in Children with ADHD. Journal of the Medical Association of Thailand. 2018; 101(1): s34-40
- ↑ Chiraphadhanakul K, Jaimchariyatam N, Pruksananonda C, Chonchaiya W. Increased Sleep Disturbances in Thai Children With Attention-Deficit Hyperactivity Disorder Compared With Typically Developing Children. Behavioral Sleep Medicine. 2016; 14(6): 677-86
- ↑ 11.0 11.1 Lee SH, Kim HB, Lee KW. Association between sleep duration and attention-deficit hyperactivity disorder: a systematic review and meta-analysis of observational studies. Journal of Affective Disorders. 2019; 256: 62-9
- ↑ 12.0 12.1 Bondopadhyay U, Diaz-Orueta U, Coogan AN. A Systematic Review of Sleep and Circadian Rhythms in Children with Attention Deficit Hyperactivity Disorder. Journal of Attention Disorders. 2022; 26(2): 149-224
- ↑ Virring A, Lambek R, Jennum PJ, Moller LR, Thomsen PH. Sleep problems and Daily Functioning in Children with ADHD: An Investigation of the Role of Impairment, ADHD Presentations, and Psychiatric Comorbidity. Journal of Attention Disorders. 2017; 21(9): 731-740
- ↑ Liang X, Qiu H, Li SX. Objectively measured sleep continuity in children and adolescents with ADHD: A systematic review and meta-analysis. Psychiatry Research. 2023; 328:115447
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 Joseph AA, Gupta A, Hazari N, Kalaivani M, Pandey RM, Sagar R, Mehta M, Shukla G. A Cross-Sectional Comparative Study of Sleep Disturbances in Children with ADHD and Matched Controls. Brain Science. 2022; 12(9): 1158
- ↑ 16.0 16.1 16.2 16.3 Ziegler M, Kaiser A, Igel C, Geissler J, Mechler K, Holz NE, Becker K, Döpfner M, Romanos M, Brandeis D, Hohmann S, Millenet S, Banaschewski T. Actigraphy-Derived Sleep Profiles of Children with and without Attention-Deficit/Hyperactivity Disorder (ADHD) over Two Weeks- Comparison, Precursur Symptoms, and the Chronotype. Brain Science. 2021; 11(12): 1564
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 Bond L, McTiernan D, Connaughton M, Heron EA, Coogan AN, McGrath J. Sleep problems in children and adolescents in an attention deficit hyperactivity disorder service. Irish Journal of Psychological Medicine. 2023; 1-9
- ↑ Sciberras E, DePetro A, Mensah F, Hiscock H. Association between sleep and working memory in children with ADHD: a cross-sectional study. Sleep Medicine. 2015; 16(10), 1192–1197.
- ↑ Harris U, Svedberg P, Aili K, Nygren J, Larsson I. Parents' Experiences of Direct and Indirect Implications of Sleep Quality on the Health of Children with ADHD: A Qualitative Study. International Journal of Environmental Research and Public Health. 2022; 19(22): 15099
- ↑ 20.0 20.1 Lucas I, Mulraney M, Sciberras E. Sleep problems and daytime sleepiness in children with ADHD: associations with social, emotional, and behavioral functioning at school, a cross-sectional study. Behavioral Sleep Medicine. 2019; 17: 411-22
- ↑ Waldon J, Vriend J, Davidson F, Corkum P. Sleep and Attention in Children With ADHD and Typically Developing Peers. Journal of Attention Disorders. 2018; 22(10): 933-941
- ↑ Le Cornu Knight F, Dimitriou D. Poor Sleep Has Negative Implications for Children With and Without ADHD, but in Different Ways. Behavioral Sleep Medicine. 2019; 17(4): 423-436
- ↑ Bijlenga D, Vollebregt MA, Kooij JJS, Arns M. The role of the circadian system in the etiology and pathophysiology of ADHD: time to redefine ADHD? ADHD Attention Deficit and Hyperactivity Disorders. 2019; 11(1): 5–19.
- ↑ Becker SP, Langberg JM, Evans SW. Sleep problems predict comorbid externalizing behaviors and depression in young adolescents with attention deficit/hyperactivity disorder. European Child & Adolescent Psychiatry. 2015; 24(8): 897-907
- ↑ 25.0 25.1 25.2 25.3 25.4 Sung V, Hiscock H, Sciberras E, Efron D. Sleep problems in children with attention-deficit/hyperactivity disorder: prevalence and the effect on the child and family. Archives of Pediatrics and Adolescents Medicine. 2008; 162(4): 336-42
- ↑ 26.0 26.1 26.2 26.3 Craig SG, Weiss MD, Hudec KL, Gibbons C. The Functional Impact of Sleep Disorders in Children With ADHD. Journal of Attention Disorders. 2017; 24(4)
- ↑ 27.0 27.1 Langberg JM, Molitor SJ, Oddo LE, Eadeh HM, Dvorsky MR, Becker SP. Prevalence, patterns, and predictors of sleep problems and daytime sleepiness in young adolescents with ADHD. Journal of Attention Disorders. 2020; 24(4): 509-523
- ↑ Amaral MO, de Al,eida Garrido AJ, de Figueiredo Pereira C, Master NV, de Rosario Delgado Nunes C, Sakellarides CT. Quality of life, sleepiness and depressive symptoms in adolescents with insomnia: A cross-sectional study. Atencion Primaria. 2017; 49(1): 35-41
- ↑ 29.0 29.1 29.2 Stickley A, Shirama A, Kitamura S, Kamio Y, Takahashi H, Saito A. Attention deficit/hyperactivity disorder symptoms and sleep problems in preschool children: the role of autistic traits. Sleep Medicine. 2021; 83: 214-21
- ↑ 30.0 30.1 30.2 Yürümez E, Kilic BG. Relationship Between Sleep Problems and Quality of Life in Children With ADHD. Journal of Attention Disorders. 2016; 20(1): 34-40
- ↑ Eyuboglu M, Eyuboglu D. Behavioural sleep problems in previously untreated children with attention deficit hyperactivity disorder. Psychiatry and Clinical Psychopharmacolohy. 2018; 28: 19-24
- ↑ Vigliano P, Battista Galloni G, Bagnasco I, Delia G, Moletto A, Mana M, Cortese S. Sleep in children with attention-deficit/hyperactivity disorder (ADHD) before and after 6-month treatment with methylphenidate: a pilot study. European Journal of Pediatrics. 2016; 175: 695-704
- ↑ 33.0 33.1 33.2 Shur-Fen GS. Prevalence of sleep problems and their association with inattention/hyperactivity among children aged 6–15 in Taiwan. Journal of Sleep Research. 2006;15:403–414.
- ↑ 34.0 34.1 34.2 34.3 Spruyt K, Gozal D. Sleep disturbances in children with attention-deficit/hyperactivity disorder. Expert Review of Neurotherapeutics. 2011; 11(4): 565-577
- ↑ 35.0 35.1 35.2 35.3 Hvolby A. Associations of sleep disturbance with ADHD: implications for treatment. Attention Deficit and Hyperactivity Disorders. 2015; 7(1): 1-18
- ↑ 36.0 36.1 Cortese S, Faraone SV, Konofal E, Lecendreux M. Sleep in children with attention deficit/hyperactivity disorder: meta-analysis of subjective and objective studies. Journal of the American Academy of Child & Adolescent Psychiatry, 2009; 48(9): 894-908
- ↑ 37.00 37.01 37.02 37.03 37.04 37.05 37.06 37.07 37.08 37.09 37.10 37.11 37.12 37.13 37.14 37.15 37.16 Ramtekkar UP. DSM-5 changes in attention deficit hyperactivity disorder and autism spectrum disorder: implications for comorbid sleep issues. Children. 2017; 4: 62
- ↑ 38.0 38.1 Um YH, Jeong JH, Hong SC, Kim TW, Lim HK, Seo HJ. Association between sleep parameters and cognitive function in drug-naïve children with attention-deficit hyperactivity disorder: a polysomnographic study. Sleep Medicine. 2016; 21: 165-70
- ↑ 39.0 39.1 39.2 39.3 39.4 Tandon PS, Sasser T, Gonzalez ES, Whitlock KB, Christakis DA, Stein MA. Physical Activity, Screen Time, and Sleep in Children With ADHD. Journal of Physical Activity and Health. 2019; 16(6): 1–7.
- ↑ 40.0 40.1 40.2 40.3 Van der Heijden KB, Stoffelsen RJ, Popma A, Swaab H. Sleep, chronotype, and sleep hygiene in children with attention-deficit/hyperactivity disorder, autism spectrum disorder, and controls. European Child & Adolescent Psychiatry. 2018; 27(1): 99–111
- ↑ Melegari MG, Vittori E, Mallia L, Devoto A, Lucidi F, Ferri R, Bruni O. Actigraphic Sleep Pattern of Preschoolers With ADHD. Journal of Attention Disorders. 2020; 24(4): 611-624.
- ↑ Hvolby A, Jørgensen J, Bilenberg N. Parental rating of sleep in children with attention deficit/hyperactivity disorder. European Child & Adolescent Psychiatry. 2009; 18(7): 429–438
- ↑ 43.0 43.1 Diaz-Roman A, Hita-Yanez E, Buela-Casal G. Sleep characteristics in children with attention deficit hyperactivity disorder: systematic review and meta-analyses. Journal of Clinical Sleep Medicine. 2016; 12(5): 747-756
- ↑ Hong GCC, Conduit R, Wong J, Di Benedetto M, Lee E. Diet, Physical Activity, and Screen Time to Sleep Better: Multiple Mediation Analysis of Lifestyle Factors in School-Aged Children with and without Attention Deficit Hyperactivity Disorder. Journal of Attention Disorders. 2021; 25(13): 1847-1858
- ↑ 45.0 45.1 45.2 Van der Heijden KB, Smits MG, Van Someren EJW, Gunning WB. Idiopathic chronic sleep onset insomnia in attention-deficit/hyperactivity disorder: a circadian rhythm sleep disorder. Chronobiology International. 2005; 22(3): 559-70
- ↑ Cameli N, BeatriceA, Cinnante EM, Gullace C, Lentini G, Occhipinti S, Ferri R, Bruni O. Restless Sleep Disorder and the Role of Iron in Other Sleep-Related Movement Disorders and ADHD. Clinical and Translational Neuroscience. 2023; 7(3): 18
- ↑ Srifuengfung, M. Restless legs syndrome in children with ADHD: A common and treatable condition, but forgotten by psychiatrists? Asian Journal of Psychiatry. 2020; 54: 102446.
- ↑ Alessandri-Bonetti A, Guglielmi F, Deledda G, Sangalli L, Brogna C, Gallenzi P. Malocclusions, Sleep Bruxism, and Obstructive Sleep Apnea Risk in Pediatric ADHD Patients: A Prospective Study. Journal of Attention Disorders. 2024
- ↑ Thoma VK, Shulz-Zhecheva Y, Oser C, Fleischhaker C, Biscaldi M, Klein C. Media Use, Sleep Quality, and ADHD Symptoms in a Community Sample and a Sample of ADHD Patients Aged 8 to 18 Years. Journal of Attention Disorders. 2020; 24(4): 576-589
- ↑ Cao H, Yan S, Gu CG, Wang S, Ni L, Tao H, Shao T, Xu Y, Tao F. Prevalence of attention-deficit/hyperactivity disorder symptoms and their associations with sleep schedules and sleep-related problems among preschoolers in mainland China. BMC Pediatrics. 2018; 18(70)
- ↑ 51.0 51.1 Bondopadhyay U, McGrath J, Coogan AN. ''Tell Me More About Your Child's Sleep'': A Qualitative Investigation of Sleep Problems in Children With ADHD. Behavioral Sleep Medicine. 2023
- ↑ Lycett K, Sciberras E, Hiscock H, Mensah FK. Sleep problem trajectories and well-being in children with attention-deficit hyperactivity disorder: a prospective cohort study. Journal of Developmental and Behavioral Pediatrics: JDBP. 2016; 37(5): 405e14.
- ↑ 53.0 53.1 Martin CA, Mulraney M, Papadopoulos N, Rinehart NJ, Sciberras E. Bidirectional Associations Between Maternal Mental Health and Child Sleep Problems in Children With ADHD: A Longitudinal Study. Journal of Attention Disorders. 2021; 25(11): 1603-1604
- ↑ 54.0 54.1 54.2 54.3 54.4 54.5 54.6 54.7 54.8 Weiss MD, Salpekar J. Sleep problems in the child with attention-deficit hyperactivity disorder: defining aetiology and appropriate treatments. CNS Drugs. 2010; 24(10): 811-28
- ↑ El-Sheikh M, Kelly RJ. Family functioning and children’s sleep. Child Development Perspectives. 2017; 11(4), 264–269
- ↑ 56.0 56.1 56.2 56.3 Gelman VS, King NJ. Wellbeing of mothers with children exhibiting sleep disturbance. Australian Journal of Psychology. 2001; 53(1): 18-22
- ↑ Scarpelli S, Gorgoni M, D'atri A, Reda F, De Gennaro L. Advances in understanding the relationship between sleep and attention deficit-hyperactivity disorder (ADHD). Journal of Clinical Medicine. 2019; 8(10): 1737
- ↑ Bruni O, DelRosso LM, Melegari MG, Ferri R. The parasomnias. Child and Adolescent Psychiatric Clinics of North America. 2021; 30(1): 131-142
- ↑ Kirov R, Brand S, Banaschewski T, Rothenberger A. Opposite impact of REM sleep on neurobehavioral functioning in children with common psychiatric disorders compared to typically developing children. Frontiers in Psychology. 2017; 7: 2059
- ↑ Silvestri R, Gagliano A, Aricò I, Cedro C, Bruni O, Condurso R, Germano E, Siracusano R, Vita G, Bramanti P. Sleep disorders in children with Attention-Deficit/Hyperactivity Disorder (ADHD) recorded overnight by video-polysomnography. Sleep Medicine. 2009; 10: 1132–1138
- ↑ Kohyama J. Possible neuronal mechanisms of sleep disturbances in patients with autism spectrum disorders and attention-deficit/hyperactivity disorder. Medical Hypotheses. 2016; 97: 131-133
- ↑ Velez-Galarraga R, Guillen-Grima F, Crespo-Eguilaz N, Sanchez-Carpintero R. Prevalence of sleep disorders and their relationship with core symptoms of inattention and hyperactivity in children with attention-defcit/hyperactivity disorder. European Journal of Paediatric Neurology EJPN. 2016; 20: 925–937
- ↑ Malow BA, Byars K, Johnson K, Weiss S, Bernal P, Goldman SE, Panzer R, Coury DL, Glaze DG. A Practice Pathway for the Identification, Evaluation, and Management of Insomnia in Children and Adolescents With Autism Spectrum Disorders. Pediatrics. 2012; 130: 106-124
- ↑ Huang MM, Qian Z, Wang J, Vaughn MG, Lee YL, Dong GH. Validation of the sleep disturbance scale for children and prevalence of parent-reported sleep disorder symptoms in Chinese children. Sleep Medicine. 2014; 15: 923-8
- ↑ 65.0 65.1 Becker SP, Cusick CN, Sidol CA. The impact of comorbid mental health symptoms and sex on sleep functioning in children with ADHD. European Child & Adolescent Psychiatry. 2018; 27: 353-365
- ↑ Coghill DR, Caballero B, Sorooshian S, Civil RA. Systematic review of the safety of lisdexamfetamine dimesylate. CNS Drugs. 2014; 28: 497–511.
- ↑ 67.0 67.1 Stein MA, Weiss M, Leventhal BL. ADHD by night: sleep problems and ADHD medications. Child and Adolescent Psychopharmacology News. 2007; 12(6): 1-5
- ↑ Vélez-Galarraga R, Guillén-Grima F, Crespo-Eguílaz N, Sánchez-Carpintero R. Prevalence of sleep disorders and their relationship with core symptoms of inattention and hyperactivity in children with attention-deficit/hyperactivity disorder. European Journal of Paediatric Neurology. 2016; 20(6): 925-37
- ↑ Kidwell KM, Van Dyk TR, Lundahl A, Nelson TD. Stimulant Medications and Sleep for Youth with ADHD: A Meta-analysis. Pediatrics. 2015; 136(6): 1144-1153
- ↑ Morash-Conway J, Gendron M, Corkum P. The role of sleep quality and quantity in moderating the effectiveness of medication in the treatment of children with ADHD. ADHD Attention Deficit and Hyperactivity Disorder. 2017; 9: 31–38
- ↑ Becker SP, Froehlich TE, Epstein JN. Effects of methylphenidate on sleep functioning in children with attention-deficit/hyperactivity disorder. Journal of Developmental and Behavioral Pediatrics. 2016; 37(5): 395–404
- ↑ O’Brien LM, Ivanenko A, Crabtree VM, Holbrook CR, Bruner JL, Klaus CJ, Gozal D. The effect of stimulants on sleep characteristics in children with attention deficit/hyperactivity disorder. Sleep Medicine. 2003; 4: 309-316
- ↑ Sangal RB, Owens J, Allen AJ, Sutton V, Schuh K, Kelsey D. Effects of atomoxetine and methylphenidate on sleep in children with ADHD. Sleep. 2006; 29(12): 1573-85
- ↑ Martin CA, Hiscock H, Rinehart N, Heussler HS, Hyde C, Fuller-Tyszkiewicz Mm McGillivray J, Austin DW, Chalmers A, Sciberras E. Associations Between Sleep Hygiene and Sleep Problems in Adolescents with ADHD: A Cross-Sectional Study. Journal of Attention Disorders. 2020; 24(4): 545-554
- ↑ 75.0 75.1 Sciberras E, Song JC, Mulraney M, Schuster T, Hiscock H. Sleep problems in children with attention-deficit hyperactivity disorder: associations with parenting style and sleep hygiene. European child and Adolescent Psychiatry. 2017; 26: 1129-1139
- ↑ Li S, Jin X, Yan C, Wu S, Jiang F, Shen X. Bed- and room-sharing in Chinese school-aged children: prevalence and association with sleep behaviors. Sleep Medicine. 2008; 9: 555-63
- ↑ 77.0 77.1 77.2 77.3 Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD. Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Medicine. 2009; 10: 771–779
- ↑ 78.0 78.1 Bourchtein E, Langberg JM, Cusick CN, Breaux RP, Smith ZR, Becker SP. Technology Use and Sleep in Adolescents With and Without Attention-Deficit/Hyperactivity Disorder. Journal of Pediatric Psychology. 2019; 44(5): 517-526
- ↑ Kaur D, Patani S, Verma R, Ghildiyal R. Profile of sleep pattern, psychiatric comorbidity and problematic electronic gadget use in children and adolescents with autism and ADHD. BJPysch Open. 2021; 7(S1): S34-S34
- ↑ Mazurek MO, Engelhardt CR. Video game use in boys with autism spectrum disorder, ADHD, or typical development. Pediatrics. 2013; 132(2): 260–266.
- ↑ Bioulac S, Arfi L, Bouvard MP. Attention deficit/hyperactivity disorder and video games: a comparative study of hyperactive and control children. European Psychiatry. 2008; 23(2): 134–141.
- ↑ Tripp G, Wickens JR. Research review: dopamine transfer deficit: a neurobiological theory of altered reinforcement mechanisms in ADHD. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2008; 49(7): 691–704.
- ↑ Wang B, Yao N, Zhou X, Liu J, Lv Z. The association between attention deficit/hyperactivity disorder and Internet addiction: A systematic review and meta-analysis. BMC Psychiatry. 2017; 17: 260
- ↑ Anderson EL, Steen E, Stavropoulos V. Internet use and problematic internet use: A systematic review of longitudinal research trends in adolescents and emergent adulthood. International Journal of Adolescence and Youth. 2017; 22: 430-454
- ↑ Elhai JD, Dvorak RD, Levine JC, Hall BJ. Problematic smartphone use: A conceptual overview and systematic review of relations with anxiety and depression psychopathology. Journal of Affective Disorders in Press. 2017; 207: 251–259.
- ↑ Tong L, Xiong X, Tan H. Attention-deficit/hyperactivity disorder and lifestyle-related behaviors in children. PLoS One. 2016; 11(9): e0163434.
- ↑ Cavalli E, Anders R, Chaussoy L, Herbillon V, Franco P, Putois B. Screen exposure exacerbates ADHD symptoms indirectly through increased sleep disturbance. Sleep Medicine. 2021; 83(4): 241-247
- ↑ 88.0 88.1 Stone MR, Stevens D, Faulkner GEJ. Maintaining recommended sleep throughout the week is associated with increased physical activity in children. Preventive Medicine. 2013; 56(2): 112–7
- ↑ Atkinson G, Davenne D. Relationships between sleep, physical activity and human health. Psychiology & Behavior. 2007; 90(0): 229-235
- ↑ Garcia S, Gunstad J. Sleep and physical activity as modifiable risk factors in age-associated cognitive decline. Sleep and Biological Rhythms. 2016; 14: 3–11.
- ↑ American Academy of Pediatrics (AAP). Clinical practice guideline: diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. Pediatrics 2000; 105: 1158-70
- ↑ 92.0 92.1 92.2 Nikles J, Mitchell GK, de Miranda Araújo R, Harris T, Heussler HS, Punja S, Senior HEJ. A systematic review of the effectiveness of sleep hygiene in children with ADHD. Psychology, Health & Medicine. 2020; 1–23.
- ↑ Thomas S, Lycett K, Papadopoulos N, Sciberras E, Rinehart N. Exploring behavioral sleep problems in children with ADHD and comorbid autism spectrum disorder. Journal of Attention Disorders. 2018; 22(10): 947–958.
- ↑ Hodgkins P, Setyawan J, Mitra D, Davis K, Quintero J, Fridman M, Shaw M, Harpin V. Management of ADHD in children across Europe: patient demographics, physician characteristics and treatment patterns. European Journal of Pediatrics. 2013; 172(7): 895-906
- ↑ Hvolby A, Jorgensen J, Bilenberg N. Actigraphic and parental reports of sleep difficulties in children with attention-deficit/hyperactivity disorder. Archives of Pediatrics & Adolescent Medicine. 2008; 162: 323–329.
- ↑ Cortese S, Angriman M, Maffeis C, Isnard P, Konofal E, Lecendreux M, Purper-Ouakil D, Vincenzi B, Bernardina BD, Mouren MC. Attention-deficit/hyperactivity disorder (ADHD) and obesity: a systematic review of the literature. Critical Reviews in Food Science and Nutrition. 2008; 48(6): 524-37
- ↑ Cortese S, Konofal E, Dalla Bernardina B, Mouren MC, Lecendreux M. Does excessive daytime sleepiness contribute to explaining the association between obesity and ADHD symptoms? Medical Hypotheses. 2008; 70(1): 12–16.
- ↑ Hart CN, Larose JG, Fava JL, James BL, Wing RR. The association between time in bed and obesity risk in young adults. Behavioural Sleep Medicine. 2013; 11(5): 321–327.
- ↑ Mimouni-Bloch A, Offek H, Engel-Yeger B, Rosenblum S, Posener E, Silman Z, Tauman R. Association between sensory modulation and sleep difficulties in children with Attention Deficit Hyperactivity Disorder (ADHD). Sleep Medicine. 2021; 84: 107-113
- ↑ Shochat T, Tzischinsky O, Engel-Yeger E. Sensory Hypersensitivity as a Contributing Factor in the Relation Between Sleep and Behavioral Disorders in Normal Schoolchildren. Behavioral Sleep Medicine. 2009; 7(1): 53-62
- ↑ Papadopoulos N, Stavropoulos V, McGinley J, Bellgrove M, Tonge B, Murphy A, Cornish K, Rinehart N. Moderating Effect of Motor Proficiency on the Relationship Between ADHD Symptoms and Sleep Problems in Children With Attention Deficit Hyperactivity Disorder-Combined Type. Behavioral Sleep Medicine. 2019; 17(5): 646-656
- ↑ Iwata S, Iwata O, Matsuishi T. Sleep patterns of Japanese preschool children and their parents: implications for co-sleeping. Acta Peadiatrica. 2013; 102: e257-62
- ↑ Peasgood T, Bhardwaj A, Biggs K. The impact of ADHD on the health and well-being of ADHD children and their siblings. European Child and Adolescent Psychiatry. 2016; 25: 1217-1231
- ↑ Chronis AM, Lahey BB, Pelham Jr WE, Kipp HL, Baumann BL, Lee SS. Psychopathology and substance abuse in parents of young children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2003; 42(12): 1424-32
- ↑ Gray L, Loring W, Malow BA, Pryor E, Turner-Henson, A, Rice M. Do Parent ADHD Symptoms Influence Sleep and Sleep Habits of Children with ADHD? A Pilot Study. Pediatric Nursing. 2020; 46(1): 18
- ↑ Martin CA, Papadopoulos N, Chellew T, Rinehart NJ, Sciberras E. Associations between parenting stress, parent mental health and child sleep problems for children with ADHD and ASD: Systematic review. Research in Developmental Disabilities. 2019; 93: 103463.
- ↑ Noble GS, O’Laughlin L, Brubaker B. Attention deficit hyperactivity disorder and sleep disturbances: Consideration of parental influence. Behavioral Sleep Medicine. 2012; 10(1): 41–53.
- ↑ Chaste P, Clement N, Botros HG, Guillaume J-L, Konyukh M, Pagan C, Scheid I, Nygren G, Anckarsäter H, Rastam M, Stahlberg O, Gillberg IC, Melke J, Delorme R, Leblond C, Toro R, Huguet G, Fauchereau F, Durand C, Boudarene L, Serrano E, Lemière N, Launay JM, Leboyer M, Jockers R, Gillberg C, Bourgeron T. Genetic variations of the melatonin pathway in patients with attention-defcit and hyperactivity disorders. Journal of Pineal Research. 2011; 51(4): 394–399
- ↑ Bijlenga D, van der Heijden KB, Breuk M, van Someren EJW, Lie MEH, Boonstra AM, Swaab HJT, Kooij JJS. Associations between sleep characteristics, seasonal depressive symptoms, lifestyle, and adhd symptoms in adults. Journal of Attention Disorders. 2013; 17(3): 261–275
- ↑ Roenneberg T, Merrow M. The circadian clock and human health. Current Biology. 2016; 26(10): R432–R443
- ↑ Walch OJ, Cochran A, Forger DB. A global quantifcation of “normal” sleep schedules using smartphone data. Science Advances. 2016; 2(5): e1501705
- ↑ 112.0 112.1 Cusick CN, Langberg JM, Breaux R, Green CD, Becker SP. Caffeine Use and Associations With Sleep in Adolescents With and Without ADHD. Journal of Pediatric Psychology. 2020; 45(6): 643-653
- ↑ Bryant Ludden A, Wolfson AR. Understanding adolescent caffeine use: Connecting use patterns with expectancies, reasons, and sleep. Health Education & Behavior. 2010; 37: 330-342
- ↑ Morgenthaler TI, Lee-Chiong T, Alessi C, Friedman L, Aurora RN, Boehlecke B, Brown T, Chesson AL, Kapur V, Maganti R, Owens J, Pancer J, Swick TJ, Zak R. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report. Sleep. 2007; 30(11): 1445-59
- ↑ Douglass AB, Bornstein R, Nino-Murcia G, Keenan S, Miles L, Zarcone Jr VP, Guilleminault C, Dement WC. The Sleep Disorders Questionnaire: I. Creation and multivariate structure of SDQ. Sleep. 1994; 17(2): 160-7
- ↑ Chervin RD, Hedger K, Dillon JE, Pituch KJ. Pediatric Sleep Questionnaire (PSQ): validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems. Sleep Medicine. 2000; 1(1): 21-32
- ↑ 117.0 117.1 Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep 2001; 23: 1043-51
- ↑ Bruni O, Ottaviano S, Guidetti V, Romoli M, Innocenzi M, Cortesi F, Giannotti F. The Sleep Disturbance Scale for Children (SDSC): construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. Journal of Sleep Research. 1996; 5(4): 251-61
- ↑ Henderson JA, Jordan SS. Development and preliminary evaluation of the Bedtime Routines Questionnaire. Journal of Psychopathology and Behavioral Assessment. 2009; 32(2): 271–280
- ↑ Mindell JA, Owens JA. A clinical guide to pediatric sleep: diagnosis and management of sleep problems. Baltimore (MD): Lippincott Williams & Wilkins. 2003
- ↑ Kivisto LR, Casey JE. Clinical utility of the BEARS as a sensitive screener for sleep problems in ADHD. Journal of the International Neuropsychological Society. 2023; 29(S1): 644-645
- ↑ Owens JA, Dalzell V. Use of the ‘BEARS’ sleep screening tool in a pediatric residents’ continuity clinic: a pilot study. Sleep Medicine. 2005; 6(1): 63-9
- ↑ Harsh JR, Easley A, LeBourgeois MK. An instrument to measure children’s sleep hygiene. Sleep. 2002; 25: A316
- ↑ Mastin DF, Bryson J, Corwyn R. Assessment of sleep hygiene using the Sleep Hygiene Index. Journal of Behavioral Medicine. 2006; 29: 223-7
- ↑ 125.0 125.1 Cremone-Caira A, Root H, Harvey EA, McDermott JM, Spencer RMC. Effects of Sleep Extension on Inhibitory Control in Children With ADHD: A Pilot Study. Journal of Attention Disorders. 2020; 24(4): 601-610
- ↑ Larsson I, Aili K, Löhn M, Svedberg P, Nygren JM, Ivarsson A, Johansson P. Sleep interventions for children with attention deficit hyperactivity disorder (ADHD): A systematic literature review. Sleep Medicine. 2023; 102: 64-75
- ↑ Papadopoulos N, Sciberras E, Hiscock H, Mulraney M, McGillivray J, Rinehart N. The Efficacy of a Brief Behavioral Sleep Intervention in School-Aged Children With ADHD and Comorbid Autism Spectrum Disorder. Journal of Attention Disorders. 2019; 23(4): 341-350
- ↑ 128.0 128.1 Malkani MK, Pestell CF, Sheridan AM, Crichton A, Horsburgh GC, Bucks RS. Behavioral Sleep Interventions for Children With ADHD: A Systematic Review and Meta-Analysis. Journal of Attention Disorders. 2022; 26: 1805-1821
- ↑ Van der Heijden KB, Smits MG, van Someren EJW, Ridderinkhof KR, Gunning WB. Effect of Melatonin on Sleep, Behavior, and Cognition in ADHD and Chronic Sleep-Onset Insomnia. Journal of the American of Child and Adolescent Psychiatry. 2007; 46(2): 233–241.
- ↑ 130.0 130.1 Hoebert M, Van Der Heijden KB, Van Geijlswijk IM, Smits MG. Long-term follow-up of melatonin treatment in children with ADHD and chronic sleep onset insomnia. Journal of Pineal Research. 2009; 47(1): 1–7.
- ↑ Coogan AN, McGowan NM. A systematic review of circadian function, chronotype and chronotherapy in attention deficit hyperactivity disorder. ADHD Attention Deficit and Hyperactivity Disorders. 2017; 9: 129–147
- ↑ Checa-Ros A, Munoz-Hoyos A, Molina-Carballo A, Viejo-Boyano I, Chacín M, Bermúdez V, D'Marco L. Low Doses of Melatonin to Improve Sleep in Children with ADHD: An Open-Label Trial. Children. 2023; 10(7): 1121
- ↑ Abdelgadir IS, Gordon MA, Akobeng AK. Melatonin for the management of sleep problems in children with neurodevelopmental disorders: a systematic review and meta-analysis. Archives of Disease in Childhood. 2018; 103: 1155-1162
- ↑ Villagomez A, Ramtekkar U. Iron, Magnesium, Vitamin D, and Zinc Deficiencies in Children Presenting with Symptoms of Attention-Deficit/Hyperactivity Disorder. Children. 2014; 1(3): 261-279
- ↑ Cortese S, Holtman M, Banaschewski T, Buitelaar J, Coghill D, Danckaerts M, Dittman RW, Graham J, Taylor E, Sergeant J. Practitioner review: current best practice in the management of adverse events during treatment with ADHD medications in children and adolescents. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2013; 54(3): 227–246.
- ↑ Lecendreux M, Cortese S. Sleep problems associated with ADHD: a review of current therapeutic options and recommendations for the future. Expert Review of Neurotherapeutics. 2007; 7(12): 1799–1806
- ↑ Hiscock H, Mulraney M, Heussler H, Rinehart N, Schuster T, Grobler AC, Gold L, Mudiyanselage SB, Hayes N, Sciberras E. Impact of a behavioral intervention, delivered by pediatricians or psychologists, on sleep problems in children with ADHD: a cluster-randomized, translational trial. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2019; 60(11): 1230-1241
- ↑ Scantlebury A, McDavid C, Dawson V, Elphick H, Fairhurst C, Hewitt C, Parker A, Spiers G, Thomas M, Wright K, Beresford B. Non-pharmacological interventions for non-respiratory sleep disturbance in children with neurodisabilities: a systematic review. Developmental Medicine and Child Neurology. 2018; 60(11): 1076-1092
- ↑ Rigney G, Ali NS, Corkum PV, Brown CA, Constantin E, Godbout R, Hanlon-Dearman A, Ipsiroglu O, Reid GJ, Shea S, Smith IM, Van der Loos HFM, Weiss SK. A systematic review to explore the feasibility of a behavioural sleep intervention for insomnia in children with neurodevelopental disorders: A transdiagnostic approach. Sleep Medicine Reviews. 2018; 41: 244-254
- ↑ Peppers KH, Eisbach S, Atkins S, Poole JM, Derouin A. An intervention to promote sleep and reduce ADHD symptoms. Journal of Pediatric Health Care. 2016; 30(6): e43–e48
- ↑ Shah H, Dani AA. A Study on Effect of Sleep Training Program in Children with ADHD: A Comparative Prospective Study. Journal of Indian Association for Child and Adolescent Mental Health. 2023; 19(4): 370-377
- ↑ Owens JA. The ADHD and sleep conundrum redux: Moving forward. Sleep Medicine Reviews. 2006; 10: 377–379.
- ↑ Becker SP, Lienesch JA. Nighttime media use in adolescents with ADHD: links to sleep problems and internalizing symptoms. Sleep Medicine. 2018; 51: 171–178
- ↑ Engelhardt CR, Mazurek MO, Sohl K. Media use and sleep among boys with autism spectrum disorder, ADHD, or typical development. Pediatrics. 2013; 132(6): 1081–1089
- ↑ 145.0 145.1 145.2 Hiscock H, Sciberras E, Mensah F, Gerner B, Efron D, Khano S, Oberklaid F. Impact of a behavioural sleep intervention on symptoms and sleep in children with attention deficit hyperactivity disorder, and parental mental health: Randomised controlled trial. BMJ. 2015; 350: h68
- ↑ 146.0 146.1 Keshavarzi A, Bajoghli H, Mohammadi MR, Salmanian M, Kirov R, Gerber M, Holsboer-Trachsler E, Brand S. In a randomized case-control trial with 10-year old suffering from attention deficit/hyperactivity disorder (ADHD) sleep and psychological functioning improved during a 12-week sleep-training program. The World Journal of Biological Psychiatry. 2014; 15(8): 609-19
- ↑ 147.0 147.1 Sciberras E, Fulton M, Efron D, Oberklaid F, Hiscock H. Managing sleep problems in school aged children with ADHD: A pilot randomised controlled trial. Sleep Medicine. 2011; 12(9), 932–935
- ↑ 148.0 148.1 148.2 148.3 Pratiwi RD, Fitn SY, Mulya AP. The Interventions for Sleep Disorders in Children With Attention Deficit and Hyperactivity Disorder: A Narrative Review. Open Acces Macedonian Journal of Medical Sciences. 2021
- ↑ Mullane J, Corkum P. Case series: Evaluation of a behavioral sleep intervention for three children with attention-deficit/hyperactivity disorder and dyssomnia. Journal of Attention Disorders. 2006; 10(2): 217–227
- ↑ 150.0 150.1 Vetrayan J, Othman S, Victor Paulraj SJP. Case series: Evaluation of Behavioral Sleep Intervention for Medicated Children With ADHD. Journal of Attention Disorders. 2017; 21(2): 168–179.
- ↑ 151.0 151.1 Corkum P, Lingley-Pottie P, Davidson F, McGrath P, Chambers CT, Mullane J, Laredo S, Woodford K, Weiss SK. Better nights/better days—Distance intervention for insomnia in school-aged children with/without ADHD: A randomized controlled trial. Journal of Pediatric Psychology. 2016; 41(6): 701–713
- ↑ 152.0 152.1 Sciberras E, Mulraney F, Mensah F, Oberklaid F, Efron D, Hiscock H. Sustained impact of a sleep intervention and moderators of treatment outcome for children with ADHD: a randomised controlled trial. Psychological Medicine. 2020; 50(2): 210-219
- ↑ Sciberras E, Mulraney M, Heussler H, Rinehart N, Schuster T, Gold L, Hiscock H. Does a brief, behavioural intervention, delivered by paediatricians or psychologists improve sleep problems for children with ADHD? Protocol for a cluster-randomised, translational trial. BMJ Open. 2017; 7(4): e014158.
- ↑ Mehri M, Chehrzad MM, Mardani A, Maleki M, Dianatinasab M, Kousha M, Assari S. The effect of behavioral parent training on sleep problems of school-age children with ADHD: A parallel randomized controlled trial. Archives of Psychiatric Nursing. 2020; 34(4): 261-267
- ↑ Li X, Lau FLF, Chiu WV, Wong CKD, Li AM, Wing YK, Lay YCK, Shea KSC, Li SX. An Open-Label Pilot Trial of a Brief, Parent-Based Sleep Intervention in Children with ADHD. Journal of Attention Disorders. 2024; 5: 10870547241233731
- ↑ Eron K, Kohnert L, Watters A, Logan C, Weisner-Rose M, Mehler PS. Weighted blanket use: A systematic review. The American Journal of Occupational Therapy. 2020; 74(2): 7402205010p1–7402205010p14
- ↑ Hvolby A, Bilenberg N. Use of Ball Blanket in attention-deficit/hyperactivity disorder sleeping problems. Nordic Journal of Psychiatry. 2011; 65: 89–94.
- ↑ Champagne T, Mullen B, Dickson D, Krishnamurty S. Evaluating the safety and effectiveness of the weighted blanket with adults during an inpatient mental health hospitalization. Occupational Therapy in Mental Health. 2015; 31: 211-233
- ↑ Larsson I, Aili K, Nygren JM, Jarbin H, Svedberg P. Parents' Experiences of Weighted Blankets' Impact on Children with Attention-Deficit/Hyperactivity Disorder (ADHD) and Sleep Problems - A Qualitative Study. International Journal of Environmental Research and Public Health. 2021; 18(24): 12959
- ↑ Löhn M, Aili K, Svedberg P, Nygren J, Jarbin H, Larsson I. Experiences of Using Weighted Blankets among Children with ADHD and Sleeping Difficulties. Occupational Therapy International. 2023
- ↑ Bériault M, Turgeon L, Labrosse M, Berthiaume C, Verreault M, Berthiaume C, Godbout R. Comorbidity of ADHD and anxiety disorders in school-age children: Impact on sleep and response to a cognitive-behavioral treatment. Journal of Attention Disorders. 2018; 22(5): 414–424.
- ↑ 162.0 162.1 Fehr KK, Russ SW, Ievers-Landis CE. Treatment of Sleep problems in young children: A case series report of a cognitive-behavioral play intervention. Clinical Practice in Pediatric Psychology. 2016; 4(3): 306-17
- ↑ Gong H, Ni C-X, Liu Y-Z, Zhang Y, Su W-J, Lian Y-J, Peng W, Jiang C-L. Mindfulness meditation for insomnia: A meta-analysis of randomized controlled trials. Journal of Psychosomatic Research. 2016; 89: 1–6
- ↑ Zaccari V, Santonastaso O, Mandolesi L, De Crescenzo F, Foti F, Crescentini C, Fabbro F, Vicari S, Curcio G, Menghini D. Clinical application of mindfulness-oriented meditation in children with ADHD: a preliminary study on sleep and behavioral problems. Psychology & Health. 2022; 37(5): 563-579
- ↑ Cairncross M, Miller CJ. The effectiveness of mindfulness-based therapies for ADHD: A meta-analytic review. Journal of Attention Disorders. 2020; 24(5): 627–643.
- ↑ Fried R, DiSalvo M, Farrell A, Biederman J. Using a Digital Meditation Application to Mitigate Anxiety and Sleep Problems in Children with ADHD. Journal of Attention Disorders. 2022; 26(7): 1033-1039.
- ↑ Liang X, Li R, Wrong SHS, Sum RKW, Wang P, Yang B, Sit CHP. Physical Activity and Executive Function in Children With ADHD: The Mediating Role of Sleep. Frontiers in Pediatrics. 2022; 9
- ↑ Liu HLV, Sun F, Tse CYA. Examining the Impact of Physical Activity on Sleep Quality in Children With ADHD. Journal of Attention Disorders. 2023; 27(10): 1099-1106
- ↑ Qiu H, Liang X. Change in Sleep Latency as a Mediator of the Effect of Physical Activity Intervention on Executive Functions Among Children with ADHD: A Secondary Analysis from a Randomized Controlled Trial. Journal of Autism and Developmental Disorders. 2023
- ↑ Rosalez E, Johnson CM, Bradley-Johnson SB, Kanouse S. Effects of White Noise on Off-Task Behavior and Sleep for Elementary-Age Students with ADHD. Child & Family Behavior Therapy. 2020; 42(1): 20-36
- ↑ Sonne T, Müller J, Marshall P, Obel C, Grønbæk K. Changing family practices with assistive technology: MOBERO improves morning and bedtime routines for children with ADHD. In Proceedings of the 2016 CHI conference on human factors in computing systems, Santa Clara. 2016