Hamstring Strain
Description[edit | edit source]
Hamstring strains are caused by a rapid extensive contraction or a violent stretch of the hamstring muscle group which causes high mechanical stress. This results in varying degrees of rupture within the fibres of the musculotendinous unit.[1]
Hamstring strains are common in sports with a dynamic character like sprinting, jumping, contact sports such as Australian Rules football (AFL), American football and soccer where quick eccentric contractions are regular. In soccer, it is the most frequent injury.[1] Hamstring injuries can also occur in recreational sports such as water skiing and bull riding, where the knee is forcefully extended during injury.
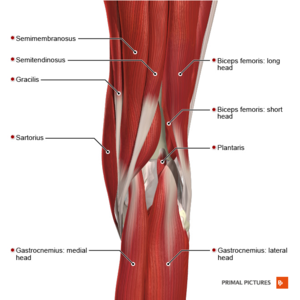
The hamstrings consist of three muscles:
- The biceps femoris
- The semitendinosus and
- The semimembranosus. [2]
For a more detailed review of the anatomy of the hamstrings, please see the Hamstrings article.
Epidemiology/Etiology[edit | edit source]
The cause of a hamstring muscle strain is often obscure. In the second half of the swing phase, the hamstrings are at their greatest length and at this moment, they generate maximum tension [4]. In this phase, hamstrings contract eccentrically to decelerate flexion of the hip and extension of the lower leg [5]. At this point, a peak is reached in the activity of the muscle spindles in the hamstrings. A strong contraction of the hamstring and relaxation of the quadriceps is needed. According to “Klafs and Arnheim”, a breakdown in the coordination between these opposite muscles can cause the hamstring to tear[5]. The greatest musculo-tendon stretch is incurred by the biceps femoris, which may contribute to its tendency to be more often injured than the other 2 hamstring muscles (semimembranosus and semitendinosus) during high-speed running.[6]
Predisposing Factors/Risk Factors[edit | edit source]
There are various proposed risk factors which may play a role in hamstring injuries: [7]
- Older age
- Previous hamstring injury
- Limited hamstring flexibility[8]
- Increased fatigue
- Poor core stability
- Strength imbalance
- Ethnicity
- Previous calf injury
- Previous substantial knee injury
- Osteitis pubis
- Increased quadriceps flexibility was inversely associated with hamstring strain incidence in a group of amateur Australian Rules footballers
- Players presenting certain polymorphisms, IGF2 and CCL2 (specifically its allelic form GG), might be more vulnerable to severe injuries and should be involved in specific prevention programmes
- Tight hip flexors[9]
- Previously associated lumbar spine abnormalities. Kicking and executing abdominal strengthening exercises with straight legs have been identified as possible contributory causes of lordosis. The anatomical reason seems to be that the iliopsoas muscle group is primarily involved in kicking and straight leg raising or straight leg sit-up exercises and contributes to strengthening this muscle'. Therefore, it is possible that certain athletic activities and training methods that exacerbate postural defects may also predispose the player to injury.[10]
During activities like running and kicking, hamstring will lengthen with concurrent hip flexion and knee extension, this lengthening may reach the mechanical limits of the muscle or lead to the accumulation of microscopic muscle damage. [11] There is a possibility that hamstring injuries may arise secondary to the potential uncoordinated contraction of biceps femoris muscle resulting from dual nerve supply. [7]
Another debate is on hamstring variation in muscle architecture. The short head of biceps femoris (BFS) possesses longer fascicles (which allow for greater muscle extensibility and reduce the risk of over lengthening during eccentric contraction) and a much smaller cross-section area compared to the long head of biceps femoris (BFL). Whereas BFL presents with shorter fascicles compared to BFS which undergo repetitive over lengthening and accumulated muscle damage.
Excessive anterior pelvic tilt will place the hamstring muscle group at longer lengths and some studies proposed that this may increase the risk of strain injury. [12]
Characteristics/Clinical Presentation[edit | edit source]
Hamstring strain results in a sudden, minimal to severe pain in the posterior thigh. Also, a "popping" or tearing impression can be described.[13] Sometimes swelling and ecchymosis are possible but they may be delayed for several days after the injury occurs. Rarely symptoms are numbness, tingling, and distal extremity weakness. These symptoms require further investigation into sciatic nerve irritation. Large hematoma or scar tissue can be caused by complete tears and avulsion injuries.
Other possible symptoms:[6]
- Pain
- Tenderness
- Loss of motion
- Decreased strength on isometric contraction
- Decreased length of the hamstrings
Hamstring strains are categorised in 3 groups, according to the amount of pain, weakness, and loss of motion.
- Grade 1 (mild): just a few fibres of the muscle are damaged or have ruptured. This rarely influences the muscle's power and endurance. Pain and sensitivity usually happen the day after the injury (depends from person to person). Normal patient complaints are stiffness on the posterior side of the leg. Patients can walk fine. There can be a small swelling, but the knee can still bend normally. [14] [15]
- Grade 2 (medium): approximately half of the fibres are torn. Symptoms are acute pain, swelling and a mild case of function loss. The walk of the patient will be influenced. Pain can be reproduced by applying precision on the hamstring muscle or bending the knee against resistance. [14] [15]
- Grade 3 (severe): ranging from more than half of the fibres ruptured to complete rupture of the muscle. Both the muscle belly and the tendon can suffer from this injury. It causes massive swelling and pain. The function of the hamstring muscle can't be performed anymore and the muscle shows great weakness. [14] [15]
Differential Diagnosis[edit | edit source]
On examining the patient, the physiotherapist possibly has to differentiate between different injuries e.g.
- adductor strains, avulsion injury, lumbosacral referred pain syndrome, piriformis syndrome, sacroiliac dysfunction, sciatica, Hamstring tendinitis and ischial bursitis.[13]
- Other sources of posterior thigh pain could also be confused with hamstring strains and should be considered during the examination process. Specific tests and imaging are used to assess and exclude those different pain source possibilities.[13]
- Sciatic nerve mobility limitations can contribute to posterior thigh pain and adverse neural tension could in some cases be the only source of pain without any particular muscular injury. In certain cases, it is difficult to determine whether it is the Hamstrings or other muscle groups like hip adductors (eg. M. Gracilis and M. Adductor Magnus and Longus.) that are injured due to their proximity. Sometimes imaging procedures may be required to determine the exact location of the injury.[13]
- Other conditions with similar presentations as hamstring strains are strained popliteus muscle, tendonitis at either origin of the gastrocnemius, sprained posterior cruciate ligament, apophysitis-pain in ischial tuberosity, Lumbar spine disorders and lesions of the upper tibiofibular joint. [13]
Diagnostic Procedures[edit | edit source]
Most of the acute injuries can easily be found by letting the patient tell how the injury occurred. To be sure they must do a little investigation of the hamstrings as well.
When the therapist isn't too sure, he can ask for medical imaging. This will exclude all other possibilities.[11]
- Radiographs: a good thing about radiographs is that with that kind of imaging, it's possible to differentiate the etiology of the pain. It can differentiate in muscular disease (e.g muscle strain) or a disease of the bone (e.g. Stress fracture).[14]
- Ultrasound (US): this kind of imaging is used a lot because it is a cheap method. It is also a good method because it has the ability to image muscles dynamically. A negative point about Ultrasound is that it needs a skilled and experienced clinician. [14] [16]
- Magnetic Resonance Imaging (MRI): MRI gives a detailed view of muscle injury. But sometimes it may not be clear according to the images. If that happens, the therapist must rely on the story that the patient told him (see characteristics/clinical presentation). [14] [16]
MRI study was done to distinguish between two main groups of muscle injuries: Injury by Direct or Indirect trauma.
- Within the group of injuries due to indirect trauma, the classification brings the concept of functional and structural lesions. Functional muscle injuries present alterations without macroscopic evidence of fiber tear. These lesions have multifactorial causes and are grouped into subgroups that reflect their clinical origin, such as overload or neuromuscular disorders. Structural muscle injuries are those whose MRI study presents macroscopic evidence of fibre tear, i.e., structural damage. They are usually located in the Musculotendinous junction, as these areas have biomechanical weak points.[17] Some studies screened patients after hamstring injuries and they concluded that, normalisation of this increased signal intensity in MRI seems not required for a successful return to play (RTP)[18].
| Type of injury | Definition | MRI |
|---|---|---|
| Direct | Contusion: blunt trauma from external factors, with intact muscle tissue
Laceration: blunt trauma from an external factor with muscular rupture |
Hematoma |
| Indirect :Functional | 1A: fatigue-induced muscle disorder Muscle stiffness
1B: delayed onset muscle soreness Acute inflammatory pain Type 2: muscle disorder of neuromuscular origin 2A: spine-related neuromuscular muscle disorder Increased muscle tone due to neurological disorder 2B: muscle-related neuromuscular muscle disorder Increased muscle tone due to altered neuromuscular control |
Negative
Negative or isolated edema |
| Structural | Type 3: Partial muscle tear
3A: minor partial muscle tear: tear involving a small area of the maximal muscle diameter 3B: moderate partial muscle tear: tear involving moderate area of maximum muscle diameter Type 4: (sub)total muscle tear with avulsion: Involvement of the entire muscle diameter, muscle defect |
Fiber rupture Retraction and hematoma Complete discontinuation of fibers |
Outcome Measures[edit | edit source]
- FASH: The FASH(Functional assessment scale for acute Hamstring injuries) questionnaire is a self-administered questionnaire which now can only be used in Greek, English and German languages. Because hamstring injuries represent the most common football injury, they tested the validity and reliability of the FASH-G (G = German version) questionnaire in German-speaking footballers suffering from acute hamstring injuries. The FASH-G is a valid and reliable instrument to assess and determine the severity of hamstring injuries in a population of athletes.[19]
- LEFS: Lower Extremity Functional Scale
- SFMA: The Selective Functional Movement Assessment (SFMA) is a clinical assessment system designed to identify musculoskeletal dysfunction by evaluation of fundamental movements for limitations or symptom provocation.[20]
- PSFS: Patient Specific Functional Scale
- VAS: Visual Analog Scale
- NPRS: Numerical Pain Rating Scale
Examination[edit | edit source]
Running gait: The physical examination begins with an examination of the running gait. Patients with a hamstring strain usually show a shortened walking gait. Swelling and ecchymosis aren’t always detectable at the initial stage of the injury because they often appear several days after the initial injury.
Observation: The physical examination also involves visible examination. The posterior thigh is inspected for asymmetry, swelling, ecchymosis and deformity.
Palpation: Palpation of the posterior thigh is useful for identifying the specific region injured through pain provocation, as well as determining the presence/absence of a palpable defect in the musculotendon unit. With the patient positioned prone, repeated knee flexion-extension movements without resistance through a small range of motion may assist in identifying the location of the individual hamstring muscles and tendons. With the knee maintained in full extension, the point of maximum pain with palpation can be determined and located relative to the ischial tuberosity, in addition to measuring the total length of the painful region. The total length, width and distance between the ischial tuberosity and the area with maximal pain are measured in centimeters.[21]While both of these measures are used, only the location of the point of maximum pain (relative to the ischial tuberosity) is associated with the convalescent period. That is, the more proximal the site of maximum pain, the greater the time needed to return to pre-injury level. The proximity to the ischial tuberosity is believed to reflect the extent of involvement of the proximal tendon of the injured muscle, and therefore a greater recovery period.[6]
Range of motion: Range of motion tests should consider both the hip and knee joints. Passive straight leg raise (hip) and active knee extension test (knee) are commonly used in succession to estimate hamstring flexibility and maximum length. Typical hamstring length should allow the hip to flex 80° during the passive straight leg raise and the knee to extend to 20° on the active knee extension test. When assessing post-injury muscle length, the extent of joint motion available should be based on the onset of discomfort or stiffness reported by the patient. In the acutely injured athlete, these tests are often limited by pain and thus may not provide an accurate assessment of musculotendon extensibility. Once again, a bilateral comparison is recommended.
Hip flexibility The hip flexion test combined a passive unilateral straight leg raise test (SLR) with pain estimation according to the Borg CR-10 scale. The sprinters were placed supine with the pelvis and contralateral leg fixed with straps. A standard flexometer was placed 10 cm cranial to the base of the patella. The foot was plantar flexed and the investigator slowly(approximately 30 degrees) raised the leg with the knee straight until the subject estimated a 3 (“moderate pain”) on the Borg CR-10 scale (0 = no pain and 10 = maximal pain). The hip flexion angle at this point was recorded, and the greatest angle of three repetitions was taken as the test result for Range of Motion (ROM). Values of the injured leg were expressed as a percentage of the uninjured leg for comparisons within and between groups. No warm-up preceded the flexibility measurements.
Knee flexion strength: Isometric knee flexion strength was measured with the sprinter in a prone position and the pelvis and the contralateral leg fixed. A dynamometer was placed at the ankle, perpendicular to the lower leg. The foot was in plantar flexion and the knee in an extended position. Three maximal voluntary isometric knee flexion contractions were performed, each with gradually increasing effort. Each contraction lasted 3 s with 30 s of rest in-between. The highest force value was taken as the test result for strength[22]. Attempts to bias the medial or lateral hamstrings by internal or external rotation of the lower leg, respectively, during strength testing, may assist in the determination of the involved muscles.
Clinical tests:
A systematic review by Reiman et al examined clinical tests for hamstring injuries.[23] The review included patients that presented with hamstring or posterior thigh pain but excluded those with pathology that was associated with a condition that originated elsewhere that referred pain to the hamstring/posterior thigh (i.e. the lumbar spine), The results are listed below[23]:
- Puranen-Orava test – Actively stretching the hamstring muscles in standing position with hip flexed at about 90*, the knee fully extended and foot on a solid surface. Positive – exacerbation of symptoms. (SN 0.76, SP 0.82, +LR 4.2, -LR 0.29)
- Bent-Knee stretch test (SN 0.84, SP 0.87, +LR 6.5, -LR 0.18)
- Modified Bent-knee stretch test (SN 0.89 SP 0.91, +LR 9.9, -LR 0.12)
- Taking off the shoe test/hamstring-drag test (SN 1.00, SP 1.00, +LR 280.0, -LR 0.00)
- Active ROM test (SN 0.55, SP 1.00, +LR 154.6, -LR 0.50)
- Passive ROM test (SN 0.57, SP 1.00, +LR 160.6, -LR 0.43)
- Resisted ROM test (SN 0.61, SP 1.00, +LR 170.6, -LR 0.40)
| Test | Sensitivity | Specificity | +LR | -LR |
| Puranen-Orava | 0.76 | 0.82 | 4.2 | 0.29 |
| Bent-Knee stretch | 0.84 | 0.87 | 6.5 | 0.18 |
| Modified Bent-knee stretch | 0.89 | 0.91 | 9.9 | 0.12 |
| Taking off the shoe | 1.00 | 1.00 | 280 | 0.00 |
| Active ROM | 0.55 | 1.00 | 154.6 | 0.50 |
| Passive ROM | 0.57 | 1.00 | 160.6 | 0.43 |
| Resisted ROM | 0.61 | 1.00 | 170.6 | 0.40 |
LR: Likelihood ratios permit the best use of clinical test results to establish diagnoses for the individual patient.
+LR: Probability that an individual with the target disorder has a positive test probability than an individual without the target disorder has a positive test
-LR: Probability that an individual with the condition has a negative test /probability than an individual without the condition has a negative test
Medical Management[edit | edit source]
Surgical intervention is an extremely rare procedure after a hamstring strain. Only in case of a complete rupture of the hamstrings, surgery is recommended. Almost all patients believed that they had improved with surgery. A study [24]shows that 91% were satisfied after surgery and rated their happiness with 75% or better. Hamstring endurance tests and hamstring strength tests were better and highly scored after a surgical procedure. The muscle strength testing after surgery ranged from 45% to 88%. The hamstrings endurance testing ranged from 26% to 100%. The physical examination and follow-up reveal that all repairs stayed intact.
Physiotherapy Management[edit | edit source]
The primary objective of physical therapy and the rehabilitation program is to restore the patient’s functions to the highest possible degree and/or to return the athlete to sport at the former level of performance and this with minimal risk of re-injury.
Hamstring strain injuries remain a challenge for both athletes and clinicians, given their high incidence rate, slow healing, and persistent symptoms. Moreover, nearly one-third of these injuries recur within the first year following a return to sport, with subsequent injuries often being more severe than the original.[25] The use of a specific and adequate training programme to rehabilitate hamstring strains can be determinant for the healing and prevention of a recurrent hamstring strain injury. Different kinds of therapies are used to rehabilitate hamstring strains, but are they all as effective enough to prevent a recurrence within the first year following a return to sport? Different studies tried to show the impact of eccentric exercises, dry needling, deep stripping massage, etc. on hamstring strain rehabilitation.
The use of eccentric strengthening, at long muscle length exercises, as a rehabilitation tool was used to examine the effects to prevent a recurrence of hamstring injury following the revalidation. The results shown that the use of eccentric strengthening exercises at long muscle had a positive effect.[26]
On the other hand, a study tried to compare eccentric strengthening exercises (STST) with progressive agility and trunk stabilization exercises (PATS). The rehabilitation of the STST group consisted of static stretching, isolated progressive hamstring resistance exercises, and icing. The PATS group consisted of progressive agility and trunk stabilization exercises and icing as treatment. The study found a significantly better result in patients that were rehabilitated with progressive agility and trunk stabilization. Reinjury rate was significantly lower in the PATS group after one year of returning to sport (1 of the 13 athletes instead of 7 on the 11 athletes in the STST group). A rehabilitation program consisting of progressive agility and trunk stabilization exercises is more effective than a program emphasizing isolated hamstring stretching and strengthening in promoting the return to sports and preventing injury recurrence in athletes suffering an acute hamstring strain.[27]
Deep stripping massage is another technique used as rehabilitation for hamstring strain injury. Most of the time it is combined with other rehabilitation techniques. Deep stripping massage (DSMS) alone or with eccentric resistance were used to examine the impact on hamstring length and strength. These results suggest that DSMS increases hamstring length in less than 3 min but has no effect on strength. Furthermore, combining DSMS with eccentric resistance produces more hamstring flexibility gains than DSMS alone and does not affect strength.[28]
Functional dry needling is a technique that has been reported to be beneficial in the management of pain and dysfunction after muscle strains and in combination with an eccentric training program, but there is limited published literature on its effects on rehabilitation or recurrence of injury.[29]
The impact of kinesiotaping has been demonstrated to be efficient at improving muscle flexibility, which can prevent or improve the risk of injuries.[30] Kinesiology tape can be used in combination with other rehabilitation programmes to improve muscle flexibility.
There are lots of techniques and programmes that can be used for the revalidation of hamstring strains injuries but due to a lack of studies, the effectiveness of these techniques can not all been demonstrated. Therefore eccentric exercises are the most known and applied programme for the rehabilitation of hamstring strain injuries. The use of this kind of programme has shown good results. One common criticism of rehabilitation programs that emphasize eccentric strength training, is the lack of attention to musculature adjacent to the hamstrings. It has been suggested that neuromuscular control of the lumbopelvic region is needed to enable optimal functioning of the hamstrings during normal sporting activities.
Example Rehabilitation Protocol[edit | edit source]
Phase I (week 0-3)[edit | edit source]
Goals
- Protect healing tissue
- Minimize atrophy and strength loss
- Prevent motion loss
Precautions
- Avoid excessive active or passive lengthening of the hamstrings
- Avoid antalgic gait pattern
Rehabilitation plan
- Ice – 2-3 times daily
- Stationary bike
- Sub-maximal isometric at 90, 60 and 30
- Single leg balance
- Balance board
- Soft tissue mobilisation (STM)/Instrument-assisted mobilisation (IASTM)
- Pulsed ultrasound (Duty cycle 50%, 1 MHz, 1.2 W/cm2)
- Progressive hip strengthening
- Painfree isotonic knee flexion
- Active sciatic nerve flossing
- Conventional TENS
Criteria for progression to the next phase
- Normal walking stride without pain
- Pain-free isometric contraction against submaximal (50%-75%) resistance during prone knee flexion at 90.
Phase 2 (week 3-12)[edit | edit source]
Goals
- Regain pain-free hamstring strength, progressing through full ROM
- Develop neuromuscular control of trunk and pelvis with a progressive increase in movement and speed preparing for functional movements
Precautions
- Avoid end-range lengthening of hamstring if painful
Rehabilitation plane
- Ice – post-exercise
- Stationary bike
- Treadmill at moderate to high-intensity pain-free speed and stride
- Isokinetic eccentrics in the non-lengthened state
- Single limb balance windmill touches without weight
- Single leg stance with perturbations
- Supine hamstring curls on theraball
- STM/IASTM
- Nordic hamstring Exercise
- Shuttle jumps
- Prone leg drops
- Lateral and retro band walks
- Sciatic nerve tensioning
Eccentric protocol
- Once non-weight bearing exercises are tolerated start low-velocity eccentric activities such as stiff leg deadlifts, eccentric hamstring lowers/Nordic hamstring Exercise, and split squats.
Nordic Hamstring Exercise
Criteria for progression
- Full strength 5/5 without pain during prone knee flexion at 90
- Pain-free forward and backward, jog, moderate-intensity
- Strength deficit less than 20% compared to the uninjured limb
- Pain-free max eccentric in a non-lengthened state
Phase 3 (week 12+)[edit | edit source]
Goals
- Symptom-free during all activities
- Normal concentric and eccentric strength through full ROM and speed
- Improve neuromuscular control of trunk and pelvis
- Integrate postural control into sport-specific movements
Precautions
- Train within symptoms free intensity
Rehabilitation plan
- Ice – Post-exercise – as needed
- Treadmill moderate to high intensity as tolerated
- Isokinetic eccentric training at end ROM (in hyperflexion)
- STM/IASTM
- Plyometric jump training
- 5-10 yard accelerations/decelerations
- Single-limb balance windmill touches with weight on an unstable surface
- Sport-specific drills that incorporate postural control and progressive speed
Eccentric protocol
- Include higher velocity eccentric exercises that include plyometrics and sports-specific activities
- Examples: include squat jumps, split jumps, bounding and depth jumps, single leg bounding, backward skips, lateral hops, lateral bounding, zigzag hops, bounding, plyometric box jumps, eccentric backward steps, eccentric lunge drops, eccentric forward pulls, single and double leg deadlifts, and split stance deadlift (good morning Exercise)
Return to sports criteria
- Full strength without pain in the lengthened state testing position
- Bilateral symmetry in knee flexion angle of peak torque
- Full ROM without pain
- Replication of sport-specific movements at competition speed without symptoms.
- Isokinetic strength testing should be performed under both concentric and eccentric action conditions. Less than a 5% bilateral deficit should exist in the ratio of eccentric hamstring strength (30d/s) to concentric quadriceps strength (240d/s)[36].
Resources[edit | edit source]
| [37] | [38] | [39] |
References[edit | edit source]
- ↑ 1.0 1.1 Sutton G. Hamstrung by hamstring strains: a review of the literature. Journal of Orthopaedic & Sports Physical Therapy. 1984 Jan 1;5(4):184-95.
- ↑ Schünke M, Schulte E, Schumacher U, Voll M, Wesker K. Prometheus: Algemene anatomie en bewegingsapparaat.
- ↑ Biceps Femoris Anatomy, Hamstrings - Everything You Need To Know - Dr. Nabil Ebraheim. Available from :https://www.youtube.com/watch?v=zSby5sZDOSw [last accessed 24 August 2022]
- ↑ Cattrysse E, Provyn S, Scafoflieri A, Van Roy P, Clarijs J.P, Van Noten P, et al. Compendium Topografische en Kinesiologische Ontleedkunde; Vrije Universiteit Brussel; Brussel; 2015-2016
- ↑ 5.0 5.1 Klafs CE, Arnheim DD: Principles of Athletic Training, Ed pp 370-372. St Louis: CV Mosby Co. 1968
- ↑ 6.0 6.1 6.2 Heiderscheit BC, Sherry MA, Silder A, Chumanov ES, Thelen DG. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. journal of orthopaedic & sports physical therapy. 2010 Feb;40(2):67-81.
- ↑ 7.0 7.1 Opar DA, Williams MD, Shield AJ. Hamstring strain injuries. Sports medicine. 2012 Mar;42(3):209-26.
- ↑ Tokutake G, Kuramochi R, Murata Y, Enoki S, Koto Y, Shimizu T. The risk factors of hamstring strain injury induced by high-speed running. Journal of sports science & medicine. 2018 Dec;17(4):650.
- ↑ Prior M, Guerin M, Grimmer K. An evidence-based approach to hamstring strain injury: a systematic review of the literature. Sports health. 2009 Jan;1(2):154-64.
- ↑ Hennessey L, Watson AW. Flexibility and posture assessment in relation to hamstring injury. British Journal of Sports Medicine. 1993 Dec 1;27(4):243-6.
- ↑ 11.0 11.1 Brockett CL, Morgan DL, Proske UW. Predicting hamstring strain injury in elite athletes. Medicine & Science in Sports & Exercise. 2004 Mar 1;36(3):379-87.
- ↑ Abebe ES, Moorman CT, Garrett Jr WE. Proximal hamstring avulsion injuries: injury mechanism, diagnosis and disease course. Operative Techniques in Sports Medicine. 2012 Mar 1;20(1):2-6.
- ↑ 13.0 13.1 13.2 13.3 13.4 Heiderscheit BC, Sherry MA, Silder A, Chumanov ES, Thelen DG. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. journal of orthopaedic & sports physical therapy. 2010 Feb;40(2):67-81.
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 Quadriceps Muscle Strain. Physiopedia. www.physio-pedia.com/Quadriceps_Muscle_Strain
- ↑ 15.0 15.1 15.2 Petersen J, Hölmich P. Preventie van hamstringblessures in de sport. Geneeskunde en Sport 2005; 38: 179-185
- ↑ 16.0 16.1 Muscle Injuries. Physiopedia. www.physio-pedia.com/Muscle_Injuries
- ↑ Ernlund L, Vieira LD. Hamstring injuries: update article. Revista brasileira de ortopedia. 2017 Aug;52(4):373-82.
- ↑ Reurink G, Goudswaard GJ, Tol JL, Almusa E, Moen MH, Weir A, Verhaar JA, Hamilton B, Maas M. MRI observations at return to play of clinically recovered hamstring injuries. British journal of sports medicine. 2014 Sep 1;48(18):1370-6.
- ↑ Malliaropoulos N, Korakakis V, Christodoulou D, Padhiar N, Pyne D, Giakas G, Nauck T, Malliaras P, Lohrer H. Development and validation of a questionnaire (FASH—Functional Assessment Scale for Acute Hamstring Injuries): to measure the severity and impact of symptoms on function and sports ability in patients with acute hamstring injuries. British Journal of Sports Medicine. 2014 Dec 1;48(22):1607-12.
- ↑ Glaws KR, Juneau CM, Becker LC, Di Stasi SL, Hewett TE. Intra- and inter-rater reliability of the selective functional movement assessment (sfma). Int J Sports Phys Ther. 2014 Apr;9(2):195-207.
- ↑ Hamstring protocol apsetar. Available from:http://www.aspetar.com/AspetarFILEUPLOAD/UploadCenter/636209313253275549_Aspetar%20Hamstring%20Protocol.pdf (assessed 10 July 2018)
- ↑ Askling C. Hamstring muscle strain. Karolinska Institutet (Sweden); 2008.
- ↑ 23.0 23.1 Reiman MP, Loudon JK, Goode AP. Diagnostic accuracy of clinical tests for assessment of hamstring injury: a systematic review. journal of orthopaedic & sports physical therapy. 2013 Apr;43(4):222-31.
- ↑ Cross MJ, Vandersluis R, Wood D, Banff M. Surgical repair of chronic complete hamstring tendon rupture in the adult patient. The American Journal of Sports Medicine. 1998 Nov;26(6):785-8.
- ↑ Heiderscheit BC, Sherry MA, Silder A, Chumanov ES, Thelen DG. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. journal of orthopaedic & sports physical therapy. 2010 Feb;40(2):67-81.
- ↑ Tyler TF, Schmitt BM, Nicholas SJ, McHugh MP. Rehabilitation after hamstring-strain injury emphasizing eccentric strengthening at long muscle lengths: Results of long-term follow-up. Journal of sport rehabilitation. 2017 Mar 1;26(2):131-40.
- ↑ Sherry MA, Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. Journal of Orthopaedic & Sports Physical Therapy. 2004 Mar;34(3):116-25.
- ↑ Forman J, Geertsen L, Rogers ME. Effect of deep stripping massage alone or with eccentric resistance on hamstring length and strength. Journal of bodywork and movement therapies. 2014 Jan 1;18(1):139-44.
- ↑ Dembowski SC, Westrick RB, Zylstra E, Johnson MR. Treatment of hamstring strain in a collegiate pole‐vaulter integrating dry needling with an eccentric training program: a resident's case report. International journal of sports physical therapy. 2013 Jun;8(3):328.
- ↑ Farquharson C, Greig M. Temporal efficacy of kinesiology tape vs. traditional stretching methods on hamstring extensibility. International journal of sports physical therapy. 2015 Feb;10(1):45.
- ↑ Christopher Johnson. The Askling L Protocol for Hamstring Strains | Chris Johnson PT Available from : https://www.youtube.com/watch?v=ONCSNxmQTzE [last accessed 24 August 2022]
- ↑ www.sportsinjuryclinic.net. Sports Massage for Hamstrings. Available from : https://www.youtube.com/watch?v=3RbhLL_lTuk [last accessed 24 August 2022]
- ↑ MedStar Health. Eccentric hamstring training in athletes. Available from : https://www.youtube.com/watch?v=Gxs4Pkwvbh0 [last accessed 24 August 2022]
- ↑ British Journal of Sports Medicine. Original hamstring programme by Andy Rolls (video summary). Available from : https://www.youtube.com/watch?v=fdGJ9BQ9IgA [last accessed 24 August 2022]
- ↑ FourFourTwo. Micah Richards gym workout | How to do the Nordic hamstring curl | Injury prevention. Available from : https://www.youtube.com/watch?v=TO47AQuYphE [last accessed 24 August 2022]
- ↑ Bourne MN, Timmins RG, Opar DA, Pizzari T, Ruddy JD, Sims C, et al. An evidence-based framework for strengthening exercises to prevent hamstring injury. Sports Medicine. 2018 Feb;48(2):251-67.
- ↑ www.sportsinjuryclinic.net. How long does it take a Hamstring Strain to heal? Available from : https://www.youtube.com/watch?v=1BjlA8xIgWI [last accessed 24 August 2022]
- ↑ ATLXtv. Common Sports Injuries: Hamstring Pull. Available from : https://www.youtube.com/watch?v=EPYQgwA15Aw[last accessed 24 August 2022]
- ↑ Bob & Brad. Top 3 Treatments for Hamstring Injury or Tear- It is not what you think. Available from : https://www.youtube.com/watch?v=tUQ86Ok69gY[last accessed 24 August 2022]