Assessment Before Moving and Handling
Original Editors - Naomi O'Reilly and Vidya Acharya
Top Contributors - Naomi O'Reilly, Ewa Jaraczewska, Jess Bell, Tarina van der Stockt, Kim Jackson and Carina Therese Magtibay
Introduction[edit | edit source]
Moving and handling people is a core activity for most rehabilitation professionals. Patients who have difficulty moving may require assistance, ranging from verbal encouragement to using electric hoisting equipment. Every moving and handling situation has a degree of risk for the patient and the rehabilitation professional.
Decisions about the most appropriate rehabilitation techniques and interventions are made following an individual patient risk assessment in accordance with professional guidelines for moving and handling. While adequate training is a key element of safe moving and handling, having a clear understanding of the range of factors that can impact moving and handling is also vital to providing a safe environment.
This article will explore the factors that directly impact the patient and assist the healthcare professional in ensuring a patient's safety during moving and handling tasks.
| Physical Status | Cardiovascular Status | Respiratory Status | Emotional Status | Medical Status | Communication | Cognitive Status | Sensory Status | Other |
|---|---|---|---|---|---|---|---|---|
| Height | Heart Rate | Respiratory Rate | Resistive | Diagnosis | Language | Memory | Sensation | Time of Day |
| BMI | Blood Pressure | Oxygen Saturation | Unpredictable | Medication | Speech | Judgment | Hearing | Environment |
| Range of Motion | Breathing Pattern | Unco-operative | Assistive Devices | Hearing | Concentration | Vision | ||
| Strength | Depression | Fatigue | Vision | Decision making | Touch | |||
| Balance | Agression | Culture | Impulsivity | Pressure | ||||
| Coordination | Confusion | Ability to Follow Instructions | Body Awareness | |||||
| Tone | Agitated | Pain | ||||||
| Skin Integrity |
Communication[edit | edit source]
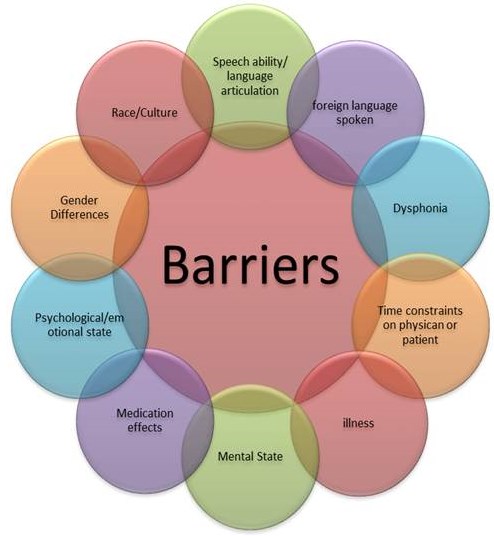
Communication is a: "Two-way process of reaching mutual understanding, in which participants not only exchange information, news, ideas and feelings but also create and share meaning."[1] We can transfer information using verbal communication, such as speech and listening; non-verbal communication, including body language, eye contact, gestures and expressions;[2] and visual communication, such as diagrams, illustrations and charts.[3] Effective clinical communication skills can improve health outcomes and are important to high-quality healthcare.[4]
Communication can impact a healthcare professional's interactions with their patients in various ways. Poor communication can lead to adverse patient outcomes and reduced compliance with treatment. Conversely, effective communication leads to productive health changes and higher satisfaction among patients.[5]
The communication cycle can be affected by a number of factors.[6]
For Patients:
- Language barriers
- Cultural barriers
- Physical and cognitive impairments, including hearing or vision loss
- Environmental factors, including a noisy environment or a lack of privacy[7]
- Effect of medication
- Emotional state, i.e. anxiety, pain and physical discomfort
For Healthcare Professionals:[8]
- Time Management
- Inability to build rapport with patients
- High patient load
- Emotional state, i.e. stress and anxiety
- Knowledge insecurity, lack of specialised training
Before any moving and handling task, it is vital to assess whether your patient has any problem expressing themselves or understanding your requests. You must identify each patient's specific communication needs, including access to interpreters or assistive technology. Where you have specific concerns about communication, a referral to speech and language therapy or psychology may be warranted to better understand the patient's communication difficulties and their causes.
For more information on communication types, please see Modes of Communication.
Cognitive Status[edit | edit source]
We must consider cognitive status when determining if a patient can safely participate in moving and handling interventions. It is important to explore whether the patient has trouble concentrating, understanding instructions, and performing tasks in the correct order or if they are missing out or forgetting elements of the task.
A cognitive status assessment is a quick and simple method to determine a patient's level of orientation at the time of the initial assessment and during manual handling tasks. It provides some basic information on their ability to answer questions and possibly follow instructions.[9]
Assessing orientation can be accomplished by the following:
- Asking the patient a series of standard questions:
- Person - "Can you tell me your name and date of birth?
- Place - "Can you tell me where you are right now?" or "Can you tell me what city we are in?
- Time/date - "Can you tell me today's date?" or "What day of the week is it?" or "What year is it?
- Situation - "Can you tell me what brought you to the hospital or health centre?" or "What surgery did you have?"
- Administering a Mini-Mental State Examination:
- Used primarily to screen for cognitive impairment in older adults, estimate the severity of cognitive impairment at a given point in time, and assess a number of subsets of cognitive status including attention, language, memory, orientation, and visuospatial proficiency.[10] [11]
- A Mini Mental State Score of 0 - 17 represents severe cognitive impairment. It may impact participation in rehabilitation activities.[12]
Emotional Status[edit | edit source]
Emotions are physical and instinctive and can result in immediate bodily reactions.[13] The following signs and symptoms can indicate changes in a patient's emotional status:
- Confusion, agitation or depression
- Euphoria or tearfulness
- Inappropriate behaviour (verbal and/or physical)
- Lack of cooperation during the assessment
When faced with any of these situations, the rehabilitation professional should:
- Liaise with relevant members of the multidisciplinary team to ensure a more comprehensive assessment that can determine if any specific factors are impacting emotional status, and/or
- Utilise outcome measures like the Richmond Agitation-Sedation Scale (RASS) - the RASS is designed to assess the level of alertness and agitated behaviour in critically-ill patients[14]
- A RASS Score between -1 and +1 generally indicates that the patient is sufficiently alert to participate in rehabilitation with minimal risk of adverse effects[15]
Assessing Emotional Status - Suggestions of Questions to Ask about a Person with Cognitive Impairment is a useful tool to support your assessment of cognitive status.
Sensory Status[edit | edit source]
Vision[edit | edit source]
The health consequences of vision loss extend beyond the eye and visual system. Vision loss has been shown to affect quality of life,[16][17] independence,[18][19] and mobility. It has been linked to falls,[20][21] injury[21][22] and worsened status in domains from mental health[23] to cognition,[24][25] social function, employment, and education.[26][27]
Assessing vision is a key part of the assessment before moving or handling a patient. You might ask the following questions as part of your assessment:
- When did you last have a vision test?
- Do you wear glasses? If so, are your glasses up to date?
- What do you wear your glasses for?
- e.g. reading/distance/everything [bifocals/varifocals]
- Have you got your glasses with you?
- Do you have any eye conditions? If so, are you using any prescribed treatment?
- e.g. eyedrops for glaucoma
- Do you see the television clearly at home? Can you describe what is in this picture?
- Are you able to read newspaper print? Medicine labels? Can you please read the following paragraph...
The following resources can assist with vision assessments by healthcare professionals:
- "Look out! Bedside Vision Check for Falls Prevention" created by the Royal College of Physicians. This resource provides a detailed plan with visual resources for completing a bedside vision assessment. It aims to reduce the risk of falls during moving and handling tasks.
- VISIBLE resource (Vision Screening to Improve Balance & Prevent Falls) created by Health Innovation Network (HIN) South London. This resource provides a stepped approach to implementing vision screening in the community.
Hearing[edit | edit source]
Hearing loss is associated with altered balance[28] and an increased risk of falls,[29][30][31] particularly for older people.[32] Some emerging evidence suggests that hearing aids may improve postural control in individuals with hearing loss, potentially reducing fall risk, although further research is needed.[32][33]
Hearing should be assessed during the subjective assessment. Basic questions to ask (verbally, written or signed) as part of your moving and handling assessment are:
- Do you wear hearing aids?
- Are your hearing aids in and switched on?
If a patient does not use hearing aids, healthcare professionals should consider whether they may be beneficial. However, it is important to recognise that during the assessment, difficulties in concentration or attention may present similarly to hearing loss in some individuals.
Vital Signs[edit | edit source]
Vital signs are measurements of the body's most basic functions, which can detect or monitor medical problems. Typically vital signs monitored by rehabilitation professionals provide information on the cardiovascular and respiratory status and include the following:
- Pulse and Heart Rate
- Blood Pressure
- Respiratory Rate
- Oxygen Saturation
These vital signs can be measured to establish goals and assess a patient's response to activity. Clinical indicators that highlight the need to assess vital signs include dyspnoea, hypertension, fatigue, syncope, chest pain, irregular heart rate, cyanosis, intermittent claudication, nausea, diaphoresis, and pedal oedema.
Cardiovascular Status[edit | edit source]
Pulses and Heart Rate[edit | edit source]
Pulse rate or heart rate is the number of times the heart beats per minute. Pulse refers to the wave of blood in an artery, which is created by the contraction of the left ventricle during a cardiac cycle.
Peripheral pulses can be felt in the periphery of the body by palpating an artery over a bony prominence. Examples in the upper extremity are the radial pulse, ulnar pulse and brachial pulse. Examples in the lower extremity are the posterior tibialis pulse, dorsalis pedis pulse and femoral pulse. Clinicians can also measure the carotid pulse in the neck.
The radial pulse is most frequently used in clinical practice. It can be palpated proximal to the wrist joint, on the radial aspect of the forearm.
- Rate:[34]
- A normal resting heart rate in adults is between 60 and 100 beats per minute
- tachycardia = heart rate above 100 beats per minute
- bradycardia = heart rate below 60 beats per minute
- A normal resting heart rate in adults is between 60 and 100 beats per minute
- Rhythm:[34]
- During an assessment we need to determine if the pulse is regular, irregular or irregularly irregular
- sinus arrhythmia = pulse rate changes with respiration - i.e. pulse rate becomes faster during inspiration and slows down during expiration
- an irregularly irregular pattern often indicates atrial flutter or atrial fibrillation
- During an assessment we need to determine if the pulse is regular, irregular or irregularly irregular
- Volume:[34]
- We can also consider the volume of the pulse
- tissue perfusion indicates the health of the tissue, and is measured by "the volume of blood that flows through a unit quantity of the tissue".[35] A low-volume pulse can suggest inadequate tissue perfusion.[36]
- When taken manually, the volume/strength of the pulse can be described using a 0-4+ scale (please note, some authors discuss a 0-3+ scale):
- 0 = no palpable pulse; 1 + = faint, but detectable pulse; 2 + = pulse slightly diminished compared to normal; 3 + = normal pulse; and 4 + = a bounding pulse.[37]
- We can also consider the volume of the pulse
- Symmetry:[34]
- It is important to check for symmetry of the pulses
- asymmetrical pulses can occur in aortic dissection, aortic coarctation, Takayasu arteritis, and subclavian steal syndrome
- It is important to check for symmetry of the pulses
- Amplitude and Rate of Increase:[34]
- Low amplitude and low rate of increase can occur in conditions such as aortic stenosis
- High amplitude and rapid rise might suggest aortic regurgitation, mitral regurgitation, and hypertrophic cardiomyopathy[34]
If the heart rate increases or decreases significantly beyond what is considered optimal for that patient, and the patient experiences shortness of breath, chest pain, or faints, then the activity should be stopped at that time.
Action: Stop the activity, return the patient to rest, and monitor heart rate until it stabilises.
Please note, the optimal heart rate may differ among populations and, for patients with specific conditions, may be determined by the medical team. Interdisciplinary communication is, therefore, key.
Blood Pressure[edit | edit source]
Blood pressure (BP) is "the force of circulating blood on the walls of the arteries",[38] mainly in large arteries of the systemic circulation. Blood pressure incorporates two measurements:
- Systolic Pressure[39]
- Describes the maximum pressure in the large arteries when the heart contracts to pump blood around the body
- Measured when the heart beats
- Diastolic Pressure[39]
- Describes the lowest pressure within the large arteries when the heart relaxes between beats
- Measured between heart beats
Blood pressure is usually assessed with auscultation and a mercury-tube sphygmomanometer. The sphygmomanometer is measured in millimetres of mercury. Blood pressure is expressed in terms of the systolic pressure over diastolic pressure, e.g. 120/60.[39] Semiautomated and automated devices that use the oscillometry method, which detects the amplitude of blood pressure oscillations on the arterial wall, are now frequently used in clinical practice. The brachial artery is the most common site to measure blood pressure.
Blood pressure response to exercise in healthy individuals:
- Initial rise in systolic blood pressure, followed by a linear increase as the intensity of exercise increases
- Diastolic blood pressure tends to remain stable or only slightly increase at higher levels of exercise intensity
In a clinical setting, recent changes in blood pressure are most relevant when determining if it is safe to continue with mobilisation. An acute increase or decrease in blood pressure of at least 20% indicates haemodynamic instability and is likely to delay mobilisation.
There are two important things to consider:
- An excessive rise in systolic or diastolic blood pressure during mobilisation, especially if prolonged, may restrict mobility progress.
- Failure of systolic blood pressure to increase or a sustained fall in blood pressure during mobilisation may reflect orthostatic intolerance or an inability of the patient’s cardiovascular system to meet the increased demands of the imposed task.
Action: stop mobilisation or modify the task to a less demanding level where blood pressure can be maintained at appropriate levels.
| Reduce Accuracy | Systolic | Diastolic |
|---|---|---|
| Hypotension | <90 | <60 |
| Normal | 90 - 129 | 60 - 79 |
| Hypertension; Stage 1 | 130 - 139 | 80 - 89 |
| Hypertension: Stage 2 | 140 - 179 | 90 - 109 |
| Hypertension: Critical | >180 | >110 |
Respiratory Status[edit | edit source]
"Work of breathing is the amount of energy or [oxygen] consumption needed by the respiratory muscles to produce enough ventilation and respiration to meet the metabolic demands of the body".[40]
Respiratory Rate[edit | edit source]
Respiratory rate (RR) is the number of breaths per minute. Each breath = the movement of air in and out of the lungs.
The average respiratory rate in adults is around 12 to 20 breaths per minute.[34] The respiratory rate in children can be higher than in adults,[41] but it varies depending on their age. You can find out more about respiratory rates for different age groups here.
Evidence suggests that respiratory rate is one of the first vital signs to change when the body has a problem. It is, therefore, key to closely monitor respiration during rehabilitation interventions, focusing on aspects like respiratory rate, depth of breathing and breathing pattern.
- Rate:[34]
- Tachypnoea: respiratory rate is more than 20 breaths per minute
- Physiological causes: exercise, emotional changes, pregnancy etc
- Pathological causes: pain, pneumonia, pulmonary embolism, and asthma etc
- Bradypnoea: respiratory rate is less than 12 breaths per minute
- Causes include: worsening of underlying respiratory conditions, resulting in respiratory failure; central nervous system depressants such as alcohol, narcotics, benzodiazepines etc
- Apnoea: "complete cessation of airflow to the lungs for a total of 15 seconds"[34]
- Causes include: cardiopulmonary arrest, airway obstruction, overdose of narcotics and benzodiazepines.
- Tachypnoea: respiratory rate is more than 20 breaths per minute
- Depth of Breathing:[34]
- Hyperpnoea: increase in the depth of breathing
- Hyperventilation: increase in both the rate and depth of breathing
- Hypoventilation: decrease in the rate and depth of ventilation
- Also look at which muscles the patient is using - i.e. accessory muscles (e.g. sternocleidomastoid) and abdominal muscles - and check for the symmetry in the chest wall movements[42]
- Also remember that an inability to speak in full sentences or an increased effort to speak can indicate discomfort when breathing.[43]
Breathing Pattern[edit | edit source]
Many conditions can influence an individual's breathing pattern:[44][34]
- Biot’s Respiration: periods where breathing rate and depth are increased, followed by periods where there is no breathing / apnoea
- Cheyne-Stokes Respiration: periods where depth of ventilation increases, followed by periods of no breathing / apnoea
- Kussmaul’s Breathing: breathing rate is regular, but depth of ventilation increases
- Orthopnoea: an individual has breathlessness in lying, but it improves when they sit up or stand
- Paradoxical Ventilation: inward movement of the abdominal or chest wall on inspiration and outward movement on expiration. Occurs with: diaphragmatic paralysis, muscle fatigue, chest wall trauma
Oxygen Saturation[edit | edit source]
Oxygen saturation is a crucial measure of how well the lungs are working. It is an essential vital sign to check when assessing and monitoring a patient for positioning, transferring or mobilising. Oxygen saturation refers to the percentage of oxygen circulating in an individual's blood.
"There is no set standard of oxygen saturation where hypoxemia occurs."[45] However, it is usually accepted that a resting oxygen saturation of less than 95% is "abnormal".[45] During exercise, there is a temporary decrease in saturation level, but the saturation level rises quickly as the respiratory rate increases.[42]
Pulse oximetry is a painless, noninvasive method of measuring the saturation of oxygen in a person’s blood.[46] Most pulse oximeters are accurate to within 2-4% of the actual blood oxygen saturation level (SaO2). This means that a pulse oximeter reading (SpO2) may be anywhere from 2-4% higher or lower than the SaO2. For example, an SpO2 of 92% can be an SaO2 of 88-96% depending on the accuracy of the pulse oximeter. However, it has been found that pulse oximetry readings are less accurate when arterial oxygen saturation (i.e. SaO2) is below 90%.[47]
Factors that can affect the accuracy of pulse oximetry:[45][48]
- Cold hands
- Poor circulation or low perfusion state
- Wearing artificial nails
- Wearing nail polish (especially darker colours like black, blue or purple)
- Very low oxygen saturation (i.e. <80%)
- Skin pigment - accuracy reduces in individuals with darker skin pigmentation
- Skin thickness
- Anaemia
- Motion artefact - excessive motion or shaking of the probe
- Intravascular dyes
- Smoking
Ways to increase the accuracy of pulse oximetry:[45][48]
- Warm up skin
- Apply topical vasodilator
- Place patient's hand below the level of the heart
- Probe location (e.g. ear vs finger)
- Probe type - transmission vs reflectance probe
- Probe size - paediatric vs adult
Environment[edit | edit source]
You must consider the area or environment in which you will complete movement and handling tasks. In particular, look at how this space could make the task unsafe. An environmental assessment identifies any problems and offers solutions to environmental hazards. [49]
Questions to consider during the assessment before moving and handling include:
- Are there any space constraints?
- Is the floor slippery or uneven?
- Is there sufficient lighting?
- Are there any trip hazards?
- Does the patient have any attachments?
Attachments[edit | edit source]
Patients often have various attachments in the hospital setting, including electrocardiogram (ECG) leads, arterial and venous lines, central venous catheters, urinary catheters, pulse oximetry, and underwater sealed drains.
Prior to performing a moving or handling task, consult with the nursing staff to find out which attachments can be safely disconnected for the activity. Attachments that provide vital physiological data, like ECG leads and pulse oximeters, must often remain connected for safety, particularly when the patient is moved for the first time.
Care must be exercised during mobilisation to avoid dislodging attachments. It is important to remove or avoid kinks and twists in the lines and watch out that drains (e.g. urinary catheter or chest drains) remain below the level of tube insertion in the body. It is important to check there is no excessive drainage or pressure swing in the water seal level of a drain before and after treatment, as these factors can impact the performance of the drain.[42]
Other Factors[edit | edit source]
Pain[edit | edit source]
Pain can be a significant barrier that must be addressed during a moving and handling assessment. To address pain, the healthcare provided should do one or all of the following:
- Assess the pain:[44]
- When assessing pain, it is important to recognise the difference between acute and persistent pain and the implications for assessing and managing the patient.
- Pain is a subjective experience, and self-report of pain is the most reliable indicator of a patient’s experience.
- If a patient has sufficient cognition and communication abilities, pain can be assessed using a standard self-report tool such as a Numeric Pain Rating Scale or Visual Analogue Scale.
- However, these scales are not suitable for many critical care patients because of sedation or mechanical ventilation. In these instances, several objective measures of pain (see below) have been found to be valid and effective.
- Always assess pain at the beginning of any physical assessment to determine the patient’s comfort level and the potential need for pain relief prior to moving the patient.
Pain Assessment Tools[edit | edit source]
Critical Care Pain Observation Tool (CPOT): The CPOT is an 8-point measure that utilises 4 basic behaviours (facial expression, body movement, muscle tension, and ventilator compliance (intubated patients) or vocalisations (extubated patients) to provide an assessment of pain.[44]
Behavioural Pain Scale (BPS): The BPS is intended for use in patients receiving mechanical ventilation. The BPS is a 12-point scale that uses 3 basic behaviours (facial expression, upper extremity movement, and ventilator compliance) to assess pain.[44]
Medication[edit | edit source]
Rehabilitation professionals should be aware of the patient's medications, as these can impact the patient's safety during manual handling tasks. While medication management is not the role of most rehabilitation professionals, understanding the potential impact of some medications can be very valuable. Assessment and rehabilitation interventions should be timed to coincide with the peak effectiveness of medication.[50]
The following classes of drugs can increase the risks of falls as they can affect the brain, heart and circulatory system:
- Drugs Acting on the Central Nervous System, e.g. psychotropic drugs
- Drugs or other substances that affect the brain can cause changes in mood, thoughts, perception, behaviour, levels of alertness, reflexes, reaction times, muscle tone, balance, etc.
- Drugs Acting on the Heart and Circulatory System
- Drugs that are used to treat different heart disorders (e.g. congestive heart failure, angina, or arrhythmia) or vascular conditions (e.g. hypertension) can cause hypotension, orthostatic hypotension, syncope, bradycardia, muscle weakness or muscle spasms secondary to hyponatremia.
- Drugs Acting on Glycemic Control
- Hypoglycemia and hyperglycemia have been associated with an increased risk of falls in hospitalised individuals.
Conclusion[edit | edit source]
These safety assessments should be considered before and during any moving or handling activity to maximise safety and minimise risk for both the patient and rehabilitation professionals involved. However, it is important to recognise that we do not necessarily have to conduct each assessment during every assessment. Instead, we must carefully consider the patient, their condition and their environment and use our clinical reasoning and judgment to choose the most appropriate assessments to ensure their safety during moving and handling tasks.
Resources[edit | edit source]
- The Handling of People: A Systems Approach
- Clinical Procedures for Safer Patient Care
- Patient Handling and Mobility Assessments, 2nd Edition
- Guidance on Manual Handling in Physiotherapy (4th edition)
- Guidance for Physiotherapists - Paediatric Manual Handling
References [edit | edit source]
- ↑ Zafar Z. Communication. Available from https://medium.com/@zahrazafarullah786/communication-3d612d633daf. [last access 26.05.2023]
- ↑ Mata ÁNS, de Azevedo KPM, Braga LP, de Medeiros GCBS, de Oliveira Segundo VH, Bezerra INM, Pimenta IDSF, Nicolás IM, Piuvezam G. Training in communication skills for self-efficacy of health professionals: a systematic review. Hum Resour Health. 2021 Mar 6;19(1):30.
- ↑ Giesbrecht J. Modes of Communication Course. Plus, 2023.
- ↑ Iversen ED, Wolderslund MO, Kofoed PE, Gulbrandsen P, Poulsen H, Cold S, Ammentorp J. Codebook for rating clinical communication skills based on the Calgary-Cambridge Guide. BMC Med Educ. 2020 May 6;20(1):140.
- ↑ Cannity KM, Banerjee SC, Hichenberg S, Leon-Nastasi AD, Howell F, Coyle N, Zaider T, Parker PA. Acceptability and efficacy of a communication skills training for nursing students: Building empathy and discussing complex situations. Nurse Educ Pract. 2021 Jan;50:102928.
- ↑ Amoah VMK, Anokye R, Boakye DS, Gyamfi N, Lee A (Reviewing Editor). Perceived barriers to effective therapeutic communication among nurses and patients at Kumasi South Hospital, Cogent Medicine. 2018;5:1.
- ↑ Al-Kalaldeh M, Amro N, Qtait M, Alwawi A. Barriers to effective nurse-patient communication in the emergency department. Emerg Nurse. 2020;28(3):29-35.
- ↑ Albahri AH, Abushibs AS, Abushibs NS. Barriers to effective communication between family physicians and patients in the walk-in centre setting in Dubai: a cross-sectional survey. BMC Health Serv Res. 2018;18(1):637.
- ↑ Fruth SJ. Fundamentals of the Physical Therapy Examination: Patient Interview and Test & Measures. 2nd Ed. Burlington: Jones & Bartlett Learning, 2018.
- ↑ Folstein MF, Folstein SE, McHugh PR "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov; 12(3):189-98.
- ↑ Sleutjes DK, Harmsen IJ, van Bergen FS, Oosterman JM, Dautzenberg PL, Kessels RP. Validity of the Mini-Mental State Examination-2 in Diagnosing Mild Cognitive Impairment and Dementia in Patients Visiting an Outpatient Clinic in the Netherlands. Alzheimer's disease and associated disorders. 2020 Jul;34(3):278.
- ↑ Faber RA. The neuropsychiatric mental status examination. Semin Neurol. 2009 Jul;29(3):185-93.
- ↑ Farnsworth B. How to measure emotions and feelings (and their differences). Available from https://imotions.com/blog/learning/best-practice/difference-feelings-emotions/. [last access 26.05.2023]
- ↑ Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA, Tesoro EP, Elswick RK. The Richmond Agitation–Sedation Scale: validity and reliability in adult intensive care unit patients. American Journal of Respiratory and Critical Care Medicine. 2002 Nov 15;166(10):1338-44.
- ↑ Green M, Marzano V, Leditschke IA, Mitchell I, Bissett B. Mobilization of intensive care patients: a multidisciplinary practical guide for clinicians. J Multidiscip Healthc 2016; 25(9): 247-56.
- ↑ Chaudry I, Brown GC, Brown MM. Medical student and patient perceptions of quality of life associated with vision loss. Can J Ophthalmol. 2015 Jun;50(3):217-24.
- ↑ Cheng HC, Guo CY, Chen MJ, Ko YC, Huang N, Liu CJL. Patient-reported vision-related quality of life differences between superior and inferior hemifield visual field defects in primary open-angle glaucoma. JAMA Ophthalmology. 2015;133(3):269–275.
- ↑ Christ SL, Zheng DD, Swenor BK, Lam BL, West SK, Tannenbaum SL, Muñoz BE, Lee DJ. Longitudinal relationships among visual acuity, daily functional status, and mortality: the Salisbury Eye Evaluation Study. JAMA Ophthalmol. 2014 Dec;132(12):1400-6.
- ↑ Haymes SA, Johnston AW, Heyes AD. Relationship between vision impairment and ability to perform activities of daily living. Ophthalmic Physiol Opt. 2002 Mar;22(2):79-91.
- ↑ Crews JE, Chiu-Fung Chou CF, Stevens JA, Saadine JB. Falls among persons aged > 65 years with and without severe vision impairment—United States, 2014. Morbidity and Mortality Weekly Report. 2016a;65(17):433–437.
- ↑ 21.0 21.1 de Boer MR, Pluijm SM, Lips P, Moll AC, Volker-Dieben HJ, Deeg DJ, van Rens GH. Different aspects of visual impairment as risk factors for falls and fractures in older men and women. Journal of Bone and Mineral Research. 2004;19(9):1539–1547.
- ↑ Coleman AL, Cummings SR, Ensrud KE, Yu F, Gutierrez P, Stone KL, Cauley JA, Pedula KL, Hochberg MC, Mangione CM; Study of Osteoporotic Fractures. Visual field loss and risk of fractures in older women. J Am Geriatr Soc. 2009 Oct;57(10):1825-32.
- ↑ Garaigordobil M, Bernarás E. Self-concept, self-esteem, personality traits and psychopathological symptoms in adolescents with and without visual impairment. Spanish Journal of Psychology. 2009;12(01):149–160.
- ↑ Pham TQ, Kifley A, Mitchell P, Wang JJ. Relation of age-related macular degeneration and cognitive impairment in an older population. Gerontology. 2006;52(6):353–358.
- ↑ Rogers MA, Langa KM. Untreated poor vision: a contributing factor to late-life dementia. Am J Epidemiol. 2010 Mar 15;171(6):728-35.
- ↑ Bibby SA, Maslin ER, McIlraith R, Soong GP. Vision and self-reported mobility performance in patients with low vision. Clinical and Experimental Optometry. 2007;90(2):115–123.
- ↑ Brown JC, Goldstein JE, Chan TL, Massof R, Ramulu P; Low Vision Research Network Study Group. Characterizing functional complaints in patients seeking outpatient low-vision services in the United States. Ophthalmology. 2014 Aug;121(8):1655-62.e1.
- ↑ Lubetzky AV. Balance, falls, and hearing loss: is it time for a paradigm shift? JAMA Otolaryngology–Head & Neck Surgery. 2020 Jun 1;146(6):535-6.
- ↑ Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010 Sep;21(5):658-68.
- ↑ Gopinath B, McMahon CM, Burlutsky G, Mitchell P. Hearing and vision impairment and the 5-year incidence of falls in older adults. Age Ageing. 2016 May;45(3):409-14.
- ↑ Jiam NT, Li C, Agrawal Y. Hearing loss and falls: A systematic review and meta-analysis. Laryngoscope. 2016 Nov;126(11):2587-2596.
- ↑ 32.0 32.1 Riska KM, Peskoe SB, Kuchibhatla M, Gordee A, Pavon J, Kim SE, West JS, Smith SL. Impact of hearing aid use on falls and falls-related injury: Health and Retirement Study Results. Ear and hearing. 2022 Mar;43(2):487.
- ↑ Ernst A, Basta D, Mittmann P, Seidl RO. Can hearing amplification improve presbyvestibulopathy and/or the risk-to-fall ? Eur Arch Otorhinolaryngol. 2021 Aug;278(8):2689-2694.
- ↑ 34.00 34.01 34.02 34.03 34.04 34.05 34.06 34.07 34.08 34.09 34.10 Sapra A, Malik A, Bhandari P. Vital Sign Assessment. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from https://www.ncbi.nlm.nih.gov/books/NBK553213/ [last access 28.05.2023]
- ↑ Tissue perfusion. In: Biology Dictionary. Available from https://www.biologyonline.com/search/tissue+perfusion. [last access 12.06.2023]
- ↑ Hill RD, Smith RB III. Examination of the Extremities: Pulses, Bruits, and Phlebitis. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 30. Available from: https://www.ncbi.nlm.nih.gov/books/NBK350/
- ↑ Zimmerman B, Williams D. Peripheral Pulse. [Updated 2023 Apr 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542175/
- ↑ Dictionary of cancer terms. Blood pressure. National Cancer Institute. Available from https://www.cancer.gov/publications/dictionaries/cancer-terms/def/blood-pressure [last access 28.05.2023]
- ↑ 39.0 39.1 39.2 Shahoud JS, Sanvictores T, Aeddula NR. Physiology, Arterial Pressure Regulation. [Updated 2022 Aug 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538509/
- ↑ Dekerlegand RL, Cahalin LP, Perme C. Chapter 26 - Respiratory Failure. Editor(s):Cameron MH, Monroe LG. In: Physical Rehabilitation, W.B. Saunders, 2007: Pages 689-717.
- ↑ Park SB, Khattar D. Tachypnea. [Updated 2023 Feb 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541062/
- ↑ 42.0 42.1 42.2 Acharya V. Assessment Before Moving and Handling Course. Plus, 2023.
- ↑ Rolfe S. The importance of respiratory rate monitoring. British Journal of Nursing. 2019 Apr 25;28(8):504-8.
- ↑ 44.0 44.1 44.2 44.3 Kotfis K, Zegan-Barańska M, Szydłowski Ł, Żukowski M, Ely EW. Methods of pain assessment in adult intensive care unit patients - Polish version of the CPOT (Critical Care Pain Observation Tool) and BPS (Behavioral Pain Scale). Anaesthesiol Intensive Ther 2017; 49(1): 66-72.
- ↑ 45.0 45.1 45.2 45.3 Hafen B, Sharma S. Oxygen Saturation. [Updated 2021 Aug 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan- [cited 2022 Oct 15]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525974/
- ↑ Hafen B, Sharma S. Oxygen Saturation. [Updated 2021 Aug 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan- [cited 2022 Oct 15]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525974/
- ↑ Jubran A. Pulse Oximetry. Critical Care. 1999 Apr;3:1-7.
- ↑ 48.0 48.1 American Thoracic Society. Pulse-oximetry. Available from https://www.thoracic.org/patients/patient-resources/resources/pulse-oximetry.pdf [last access 28.05.2023]
- ↑ Pighills AC, Torgerson DJ, Sheldon TA, Drummond AE, Bland JM. Environmental assessment and modification to prevent falls in older people. Journal of the American Geriatrics Society. 2011 Jan;59(1):26-33.
- ↑ Stiller K. Safety issues should be considered when mobilising critically ill patients. Critical care clinics. 2007 Jan 1;23(1):35-53.