Sciatica: Difference between revisions
Rosie Swift (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "</big>" to "") |
||
| (30 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:User Name|Daan Vandebriel]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:User Name|Daan Vandebriel]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== | == Introduction == | ||
Sciatica refers to radiating pain along the course of the [[Sciatic Nerve|sciatic nerve]] from the lower back or buttock to one or both legs or an associated [[Sacral Plexus|lumbosacral nerve root]]. | |||
Sciatica | |||
= | A common mistake is referring to any [[Low Back Pain|low back pain]] or [[Radiculopathy|radicular]] leg pain as sciatica<ref name=":6" />. | ||
Sciatica is a clinical diagnosis based on the presence of radiating pain in one leg, with or without the associated neurological deficits of parasthesia and muscle weakness<ref name=":3">Jensen RK, Kongsted A, Kjaer P, Koes B. Diagnosis and treatment of sciatica. BMJ. 2019 Nov 19;367:l6273. </ref>, which are the direct result of sciatic nerve or sciatic nerve root pathology. | |||
Spinal causes: | Sciatica pain often is worsened with flexion of the [[Lumbar Anatomy|lumbar spine]], twisting, bending, or coughing<ref name=":6" />. | ||
[[File:Sciatic_nerve.png|alt=|right|frameless|372x372px]] | |||
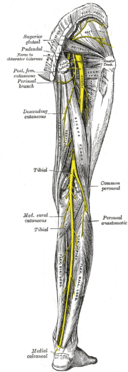
== Anatomy == | |||
The sciatic nerve is made up of the L4 through S2 nerve roots which coalesce at the [[pelvis]] to form the sciatic nerve. At up to 2 cm in diameter, the sciatic nerve is easily the largest nerve in the body. | |||
The sciatic nerve provides direct motor function to the [[hamstrings]], lower extremity [[Hip Anatomy|adductors]], and indirect motor function to the [[Gastrocnemius|calf muscles]], [[Tibialis Anterior|anterior lower leg muscles]], and some intrinsic [[Foot Anatomy|foot]] muscles. | |||
Indirectly through its terminal branches, the sciatic nerve provides sensation to the posterior and lateral lower leg as well as the plantar foot. | |||
== Etiology == | |||
Any condition that may structurally impact or compress the sciatic nerve may cause sciatica symptoms. | |||
[[Sciatic Nerve Injury|Sciatic nerve injury]] can also result in sciatica symptoms (such as pain, muscle weakness and paresthesia) and is usually caused by a traumatic injury (pressure, stretching or cutting), rather than compression or irritation of the nerve. Please read our [[Sciatic Nerve Injury|sciatic nerve injury]] page for more information. | |||
The causes of sciatica can be categorised into spinal or non-spinal causes or iatrogenic<ref name=":10" />: | |||
'''Spinal causes:''' | |||
* [[Spinal Stenosis|Spinal stenosis]] (due to degenerative bone disorders, trauma, inflammatory disease) | * [[Spinal Stenosis|Spinal stenosis]] (due to degenerative bone disorders, trauma, inflammatory disease) | ||
* [[Spondylolisthesis]] | * [[Spondylolisthesis]] | ||
* | * [[Lumbar Discogenic Pain|Herniated or bulging lumbar intervertebral disc]] | ||
* Spinal or paraspinal mass ([[Oncology|malignancy]], [[Overview of Traumatic Brain Injury|epidural hematoma]] or abscess)<ref name=":0">Davis DH, Wilkinson JT, Teaford AK, Smigiel MR. Sciatica produced by a sacral perineurial cyst. Tex Med. 1987 Mar;83(3):55-6.</ref> | |||
Non Spinal causes: | '''Non Spinal causes:''' | ||
*[[Piriformis Syndrome|Piriformis]] | *[[Piriformis Syndrome|Piriformis syndrome]] | ||
*[[Pregnancy Related Pelvic Pain|Pregnancy]] | *[[Pregnancy Related Pelvic Pain|Pregnancy]] | ||
*[[Lumbar Radiculopathy]] | *[[Lumbar Radiculopathy]] | ||
* Pelvic tumours | |||
* Trauma to leg | * Trauma to leg | ||
'''Iatrogenic causes:''' | |||
*Direct surgical trauma | |||
*Faulty positioning during anaesthesia | |||
*Injection of neurotoxic substances | |||
*Tourniquets | |||
*Dressings, casts or faulty fitting orthotics | |||
*Radiation | |||
== Epidemiology == | |||
* Annual incidence of 1% to 5%<ref name=":6">Davis D, Maini K, Vasudevan A. Sciatica. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2020. PMID: 29939685.</ref> | |||
* Lifetime incidence reported between 10% to 40%<ref name=":6" /> | |||
* No gender predominance<ref name=":6" /> | |||
* | * Peak incidence occurs in patients in their fourth decade<ref name=":6" /> | ||
* Rarely occurs before age 20 (unless traumatic)<ref name=":6" /> | |||
* No association with body height has been established except in the age 50 to 60 group<ref name=":6" /> | |||
* Increased incidence in those with poor general health (including presence of co-morbidities and smoking) and the presence of psychological factors such as depression<ref name=":4">Parreira P, Maher CG, Steffens D, Hancock MJ, Ferreira ML. Risk factors for low back pain and sciatica: an umbrella review. Spine J. 2018 Sep;18(9):1715-1721.</ref> | |||
* [[Physical Activity|Physical activity]] increases incidence in those with prior sciatic symptoms and decreased in those with no prior symptoms<ref name=":6" />. | |||
* Occupational predisposition has been shown in machine operators, truck drivers, and jobs where workers are subject to physically awkward positions<ref name=":0" /> or physical stress on the spine such as vibration<ref name=":4" /> | |||
== Clinical Presentation == | |||
* No gender predominance | |||
* Peak incidence occurs in patients in their fourth decade | |||
* | |||
* No association with body height has been established except in the age 50 to 60 group | |||
* | |||
* [[Physical Activity|Physical activity]] increases incidence in those with prior sciatic symptoms and decreased in those with no prior symptoms. | |||
* Occupational predisposition has been shown in machine operators, truck drivers, and jobs where workers are subject to physically awkward positions<ref name=":0" /> | |||
== Clinical Presentation | |||
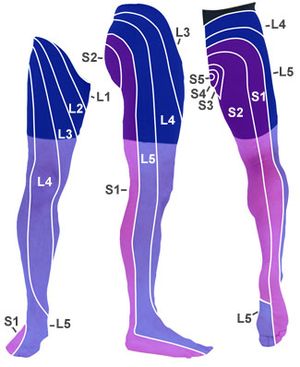
[[File:Lower-dermatomes.jpg|right|frameless]] | [[File:Lower-dermatomes.jpg|right|frameless]] | ||
Patients with sciatica can present with neurological symptoms such as: | |||
* | *Radicular pain in the distribution of the lumbosacral nerve root | ||
*Sensory impairment/disturbance, such as hot and cold or tingling/ burning sensations in the legs or numbness | |||
*Muscular weakness | |||
*[[Reflexes|Reflex]] impairment | |||
*[[Gait and Lower Limb Observation of Paediatrics - (GALLOP)|Gait]] dysfunction | |||
* | |||
* | |||
* | |||
Sciatica symptoms of paresthesias or dysesthesias and oedema in the lower extremity can differ, depending on which nerve is affected<ref name="Koes" /><ref name="Kika" /> | |||
*L4: When the L4 nerve is compressed or irritated, the patient feels pain, tingling and numbness in the thigh. The patient also feels weak when straightening the leg and may have a diminished knee jerk reflex. | *'''L4:''' When the L4 nerve is compressed or irritated, the patient feels pain, tingling and numbness in the thigh. The patient also feels weak when straightening the leg and may have a diminished knee jerk reflex. | ||
*L5: When the L5 nerve is compressed or irritated, the pain, tingling and numbness may extend to the foot and big toes. | *'''L5:''' When the L5 nerve is compressed or irritated, the pain, tingling and numbness may extend to the foot and big toes. | ||
*S1: When the S1 nerve is compressed or irritated, the patient feels pain, tingling and numbness on the outer part of the foot. The patient also experiences weakness when elevating the heel off the ground and standing on tiptoes. The ankle jerk reflex may be diminished. | *'''S1:''' When the S1 nerve is compressed or irritated, the patient feels pain, tingling and numbness on the outer part of the foot. The patient also experiences weakness when elevating the heel off the ground and standing on tiptoes. The ankle jerk reflex may be diminished. | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
A thorough differential list is important in considering a diagnosis of sciatica and should include | A thorough differential list is important in considering a diagnosis of sciatica and should include: | ||
* Herniated lumbosacral [[Disc Herniation|disc]] | * Herniated lumbosacral [[Disc Herniation|disc]] | ||
* [[Cauda Equina Syndrome|Cauda Equina]] syndrome | |||
* [[Muscle Injuries|Muscle]] spasm | * [[Muscle Injuries|Muscle]] spasm | ||
* Nerve root impingement | * Nerve root impingement | ||
| Line 78: | Line 80: | ||
* [[Renal Cancer|Tumor]] | * [[Renal Cancer|Tumor]] | ||
* [[Pott's Disease|Potts Disease]], also known as spinal tuberculosis | * [[Pott's Disease|Potts Disease]], also known as spinal tuberculosis | ||
* [[Piriformis Syndrome|Piriformis syndrome]] | * [[Piriformis Syndrome|Piriformis syndrome]] | ||
== Evaluation == | == Evaluation == | ||
Sciatica is most commonly diagnosed by: | Sciatica is most commonly diagnosed by: | ||
* Pain generally radiates below the knee, into the foot<ref name="Kika"> | '''History:''' | ||
* Patients complain about low back pain, which is usually less severe than the leg pain<ref name="Koes" /> | Complaints of radiating pain in the leg, which follows a [[Dermatomes|dermatomal pattern]]<ref name="Koes">Koes BW, van Tulder MW, Peul WC. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1895638/pdf/bmj-334-7607-cr-01313.pdf Diagnosis and treatment of sciatica]. BMJ. 2007 Jun 23;334(7607):1313-7. </ref> | ||
* Pain generally radiates below the knee, into the foot<ref name="Kika">Konstantinou K, Lewis M, Dunn KM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3481089/pdf/586_2012_Article_2398.pdf Agreement of self-reported items and clinically assessed nerve root involvement (or sciatica) in a primary care setting.] Eur Spine J. 2012 Nov;21(11):2306-15.</ref> | |||
* Patients complain about low back pain, which is usually less severe than the leg pain<ref name="Koes" /> | |||
* Patients may also report sensory symptoms. | * Patients may also report sensory symptoms. | ||
'''Special tests:''' | |||
* [[X-Rays|Plain films]] of the lumbosacral spine may evaluate for fracture or spondylolisthesis | |||
* Noncontrast [[CT Scans|CT scan]] may be performed to evaluate fracture if plain films are negative | Clinicians should always look for and inquire about [[The Flag System|red flags]] when evaluating sciatica or in patients who present with any low back pain. Patients with signs of urinary retention or decreased anal sphincter tone should be urgently referred for investigation as this suggests [[Cauda Equina Syndrome|cauda equina syndrome]]. | ||
*'''Lasègue’s test''' | |||
Also called as [[Straight Leg Raise Test|straight leg raising test]] (SLR) is the most commonly performed physical test for diagnosis of sciatica and lumbar disc hernia . The SLR is considered positive when it evokes radiating pain along the course of the sciatic nerve and below the knee between '''30''' and '''70''' degrees of '''hip flexion'''. Studies of its capacity to diagnose lumbar disc hernia show high sensitivity but low specificity.<ref name=":7">Kamath SU, Kamath SS. Lasègue’s sign. J Clin Diagn Res [Internet]. 2017 [cited 2023 Mar 27];11(5):RG01–2. Available from: <nowiki>http://dx.doi.org/10.7860/JCDR/2017/24899.9794</nowiki></ref> | |||
{{#ev:youtube|JmvGHszR_X4}} | |||
<ref>Clinical Examination Videos. Straight leg raise test - Lasegue’s sign [Internet]. Youtube; 2017 [cited 2023 Mar 27]. Available from: https://www.youtube.com/watch?v=JmvGHszR_X4 | |||
</ref> | |||
* '''Bragard test''' | |||
[[Bragard's Sign|Bragard test]] is a modification of the SLR, where ankle dorsiflexion is applied at the end of the SLR. Dorsiflexion reduces the SLR angle at which the test is positive and can be used to differentiate neural symptoms from musculoskeletal symptoms.<ref name=":7" /> | |||
[[File:Bragard test.jpg|center|thumb|Distal structural differentiation for proximal symptoms with ankle dorsiflexion (also known as Bragard test)]] | |||
* '''[[Bowstring Sign|Bowstring test]]''' | |||
Also known as the popliteal compression test or posterior tibial nerve stretch sign. The patient can be examined in sitting or in a supine position. The examiner flexes the knee and applies pressure on the popliteal fossa, evoking sciatica. Some examiners do it after SLRT by flexing the knee to relieve the buttock pain. The pain would be reproduced by a quick snap on the posterior tibial nerve in the popliteal fossa.<ref>Das JM, Nadi M. Lasegue Sign. StatPearls Publishing; 2022.</ref> | |||
{{#ev:youtube|v=orb-VI51QF0&t=11s|300}}<ref>CRTechnologies. Bowstring Test (CR). Available from: http://www.youtube.com/watch?v=orb-VI51QF0&t=11s [last accessed 03.04.2023]</ref> | |||
'''Imaging:''' | |||
It may be used if pain persists for more than 12 weeks or the patient develops progressive neurological deficits<ref name=":3" /> | |||
* [[X-Rays|Plain films]] of the lumbosacral spine may evaluate for fracture or spondylolisthesis | |||
* Noncontrast [[CT Scans|CT scan]] may be performed to evaluate fracture if plain films are negative | |||
* In cases where the neurologic deficit is the present or mass effect is suspected, immediate [[MRI Scans|MRI]] is the standard of care in establishing the cause of the pain and ruling out pressing surgical pathology<ref name=":0" /> | * In cases where the neurologic deficit is the present or mass effect is suspected, immediate [[MRI Scans|MRI]] is the standard of care in establishing the cause of the pain and ruling out pressing surgical pathology<ref name=":0" /> | ||
== Outcome Measures == | == Outcome Measures == | ||
Many to choose from, below are but a few, all dependant on cause and assessment | Many to choose from, below are but a few, all dependant on cause and assessment. | ||
* [[36-Item Short Form Survey (SF-36)|Short Form-36]] bodily pain (SF-36 BP) | * [[36-Item Short Form Survey (SF-36)|Short Form-36]] bodily pain (SF-36 BP) | ||
* [https://www.physio-pedia.com/index.php5?title=Oswestry_Disability_Index Oswestry disability index] | * [https://www.physio-pedia.com/index.php5?title=Oswestry_Disability_Index Oswestry disability index] | ||
* [https://www.physio-pedia.com/index.php5?title=Roland%E2%80%90Morris_Disability_Questionnaire Roland-Morris disability index] | * [https://www.physio-pedia.com/index.php5?title=Roland%E2%80%90Morris_Disability_Questionnaire Roland-Morris disability index] | ||
* [[Visual Analogue Scale|VAS-score]]: one of leg pain and one of back pain<ref name=":1">Brouwer, | * [[Visual Analogue Scale|VAS-score]]: one of leg pain and one of back pain<ref name=":1">Brouwer PA, Peul WC, Brand R, Arts MP, Koes BW, van den Berg AA, van Buchem MA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2697136/pdf/1471-2474-10-49.pdf Effectiveness of percutaneous laser disc decompression versus conventional open discectomy in the treatment of lumbar disc herniation; design of a prospective randomized controlled trial.] BMC Musculoskelet Disord. 2009 May 13;10:49. </ref> | ||
* [[McGill Pain Questionnaire|McGill pain Questionnaire]]<ref name=":1" />: this questionnaire looks at the location, intensity, quality and pattern of the pain as well as alleviating and | * [[McGill Pain Questionnaire|McGill pain Questionnaire]]<ref name=":1" />: this questionnaire looks at the location, intensity, quality and pattern of the pain as well as alleviating and aggravating factors<ref>Ngamkham S, Vincent C, Finnegan L, Holden JE, Wang ZJ, Wilkie DJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3285427/pdf/nihms-260699.pdf The McGill Pain Questionnaire as a multidimensional measure in people with cancer: an integrative review.] Pain Manag Nurs. 2012 Mar;13(1):27-51.</ref> | ||
* [[Timed Up and Go Test (TUG)|TUG]] | * [[Timed Up and Go Test (TUG)|TUG]] | ||
* Tampa Scale for Kinesiophobia<ref name=":2">Monticone M. | * Tampa Scale for Kinesiophobia<ref name=":2">Monticone M, Ferrante S, Teli M, Rocca B, Foti C, Lovi A, Brayda Bruno M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3897823/pdf/586_2013_Article_2889.pdf Management of catastrophising and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis.] A randomised controlled trial. Eur Spine J. 2014 Jan;23(1):87-95. </ref> | ||
* [[Pain Catastrophizing Scale|Pain Catastrophising Scale]]<ref name=":2" /> | * [[Pain Catastrophizing Scale|Pain Catastrophising Scale]]<ref name=":2" /> | ||
== Medical Management == | == Medical Management == | ||
[[File:Massage image.jpg|right|frameless]] | [[File:Massage image.jpg|right|frameless]] | ||
''' | Most patients improve over time with conservative treatment including exercise, manual therapy, and pain management<ref name=":3" /> | ||
* '''Pharmacology:''' a short course of oral [[NSAIDs in the Management of Rheumatoid Arthritis|NSAIDs]]; [[Pain Medications|Opioid and non-opioid analgesics]]; muscle relaxants; anticonvulsants for neurogenic pain; localized corticosteroid injections. | |||
* '''Surgical evaluation:''' to address structural abnormalities such as: disc herniation, epidural hematoma, epidural abscess or tumour may be considered if no improvement following 6-8 weeks of conservative treatment<ref name=":3" />. One study found that although it may speed up recovery, the effect is similar to conservative care at one year<ref name=":3" /> | |||
* '''Physical therapy management''' | |||
* | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
In most cases of sciatica, conservative treatment is favoured. The evidence does not show that one treatment is superior to the other<ref name="p2">Luijsterburg PA, Verhagen AP, Ostelo RW, van Os TA, Peul WC, Koes BW. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2219647/pdf/586_2007_Article_367.pdf Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review.] Eur Spine J. 2007 Jul;16(7):881-99.</ref> | |||
'''Patient Education''': to include information on the nature of low back back, advice on self-management techniques and encouragement to continue normal activities<ref name=":5">National Institute for Health and Care Excellence (NICE). Low back pain and sciatica in over 16s: assessment and management: NICE Guideline [NG59] 2016. Available from <nowiki>https://www.nice.org.uk/guidance/ng59</nowiki> [Accessed 13 Nov 2021]</ref> | |||
'''Promote self management techniques such as''': | |||
# use of [[Thermotherapy|hot]] or [[Cryotherapy|cold packs]] for comfort and to decreased inflammation | |||
# avoidance of inciting activities or prolonged sitting/standing | |||
# Regularly changing position i.e. from sitting to standing | |||
# practicing good erect [[posture]] | |||
# use of proper [[Lifting|lifting techniques]] | |||
'''Exercise:''' | |||
exercises to increase [[Core Strengthening|core strength]], gentle [[stretching]] of the lumbar spine and hamstrings, regular light exercise such as walking, swimming, or [[aquatherapy]] | |||
'''Manual therapy:''' spinal manipulation, mobilisation or soft tissue techniques such as massage - used alongside exercise and patient education<ref name=":5" /> | |||
'''Comprehensive treatment:''' | |||
# [[Disc Herniation]] | # [[Disc Herniation]] | ||
# [[Lumbar Discogenic Pain]] | # [[Lumbar Discogenic Pain]] | ||
| Line 141: | Line 166: | ||
# [[Piriformis Syndrome]] | # [[Piriformis Syndrome]] | ||
# [[Sacroiliac Joint Syndrome|Sacroiliac Joint Dysfunction]] | # [[Sacroiliac Joint Syndrome|Sacroiliac Joint Dysfunction]] | ||
# [[Sciatic Nerve Injury]] | |||
# [[Therapeutic Corticosteroid Injection|Corticosteroid injections]] | # [[Therapeutic Corticosteroid Injection|Corticosteroid injections]] | ||
# [[Acupuncture]] | # [[Acupuncture]] | ||
# [[Massage|Massage therapy]] | # [[Massage|Massage therapy]] | ||
{{#ev:youtube|v=4t8L4zHQ2nQ&t=7s|300}}<ref>Physio Fitness | Physio REHAB | Tim Keeley. Treatment for lumbar spine disc bulge and sciatica - wk 1 | Feat. Tim Keeley | No.58 | Physio REHAB . Available from: http://www.youtube.com/watch?v=4t8L4zHQ2nQ&t=7s [last accessed 03.04.2023]</ref> | |||
== Concluding Remarks == | == Concluding Remarks == | ||
[[File:Exercise group.jpg|right|frameless|450x450px]]There are many causes of sciatica and the disorder is best managed with a team of healthcare professionals that includes an orthopedic surgeon, physical therapist, neurologist, rehabilitation nurse, and a pain specialist. | |||
* | * The key to sciatica is patient education. | ||
* Patients should be encouraged by the clinician and nurse to lose weight, stop smoking and enroll in a physical therapy program. | * The majority of cases of sciatica are best managed conservatively. | ||
* Bed rest should be limited. | * Patients should be encouraged by the clinician and nurse to lose weight, stop smoking and enroll in a physical therapy program. | ||
* Bed rest should be limited. | |||
* The pharmacist should caution the patient against the use of prescription-strength medications to avoid dependence and other adverse effects. | * The pharmacist should caution the patient against the use of prescription-strength medications to avoid dependence and other adverse effects. | ||
* Surgery should only be undertaken when conservative methods have failed. | * Surgery should only be undertaken when conservative methods have failed. | ||
* Regular exercise is essential<ref name=":0" /> | * Regular exercise is essential<ref name=":0" /> | ||
== Summary == | |||
''The following video gives a summary of sciatica:''{{#ev:youtube|https://www.youtube.com/watch?v=VYj-JfX0wT0|width}}<ref name=":10">Osmosis. Sciatica. Available from: https://www.youtube.com/watch?v=VYj-JfX0wT0 (last accessed 15.3.2019)</ref> | |||
== References == | == References == | ||
<references /><br> | <references /><br> | ||
Latest revision as of 11:40, 26 April 2023
Introduction[edit | edit source]
Sciatica refers to radiating pain along the course of the sciatic nerve from the lower back or buttock to one or both legs or an associated lumbosacral nerve root.
A common mistake is referring to any low back pain or radicular leg pain as sciatica[1].
Sciatica is a clinical diagnosis based on the presence of radiating pain in one leg, with or without the associated neurological deficits of parasthesia and muscle weakness[2], which are the direct result of sciatic nerve or sciatic nerve root pathology.
Sciatica pain often is worsened with flexion of the lumbar spine, twisting, bending, or coughing[1].
Anatomy[edit | edit source]
The sciatic nerve is made up of the L4 through S2 nerve roots which coalesce at the pelvis to form the sciatic nerve. At up to 2 cm in diameter, the sciatic nerve is easily the largest nerve in the body.
The sciatic nerve provides direct motor function to the hamstrings, lower extremity adductors, and indirect motor function to the calf muscles, anterior lower leg muscles, and some intrinsic foot muscles.
Indirectly through its terminal branches, the sciatic nerve provides sensation to the posterior and lateral lower leg as well as the plantar foot.
Etiology[edit | edit source]
Any condition that may structurally impact or compress the sciatic nerve may cause sciatica symptoms.
Sciatic nerve injury can also result in sciatica symptoms (such as pain, muscle weakness and paresthesia) and is usually caused by a traumatic injury (pressure, stretching or cutting), rather than compression or irritation of the nerve. Please read our sciatic nerve injury page for more information.
The causes of sciatica can be categorised into spinal or non-spinal causes or iatrogenic[3]:
Spinal causes:
- Spinal stenosis (due to degenerative bone disorders, trauma, inflammatory disease)
- Spondylolisthesis
- Herniated or bulging lumbar intervertebral disc
- Spinal or paraspinal mass (malignancy, epidural hematoma or abscess)[4]
Non Spinal causes:
- Piriformis syndrome
- Pregnancy
- Lumbar Radiculopathy
- Pelvic tumours
- Trauma to leg
Iatrogenic causes:
- Direct surgical trauma
- Faulty positioning during anaesthesia
- Injection of neurotoxic substances
- Tourniquets
- Dressings, casts or faulty fitting orthotics
- Radiation
Epidemiology[edit | edit source]
- Annual incidence of 1% to 5%[1]
- Lifetime incidence reported between 10% to 40%[1]
- No gender predominance[1]
- Peak incidence occurs in patients in their fourth decade[1]
- Rarely occurs before age 20 (unless traumatic)[1]
- No association with body height has been established except in the age 50 to 60 group[1]
- Increased incidence in those with poor general health (including presence of co-morbidities and smoking) and the presence of psychological factors such as depression[5]
- Physical activity increases incidence in those with prior sciatic symptoms and decreased in those with no prior symptoms[1].
- Occupational predisposition has been shown in machine operators, truck drivers, and jobs where workers are subject to physically awkward positions[4] or physical stress on the spine such as vibration[5]
Clinical Presentation[edit | edit source]
Patients with sciatica can present with neurological symptoms such as:
- Radicular pain in the distribution of the lumbosacral nerve root
- Sensory impairment/disturbance, such as hot and cold or tingling/ burning sensations in the legs or numbness
- Muscular weakness
- Reflex impairment
- Gait dysfunction
Sciatica symptoms of paresthesias or dysesthesias and oedema in the lower extremity can differ, depending on which nerve is affected[6][7]
- L4: When the L4 nerve is compressed or irritated, the patient feels pain, tingling and numbness in the thigh. The patient also feels weak when straightening the leg and may have a diminished knee jerk reflex.
- L5: When the L5 nerve is compressed or irritated, the pain, tingling and numbness may extend to the foot and big toes.
- S1: When the S1 nerve is compressed or irritated, the patient feels pain, tingling and numbness on the outer part of the foot. The patient also experiences weakness when elevating the heel off the ground and standing on tiptoes. The ankle jerk reflex may be diminished.
Differential Diagnosis[edit | edit source]
A thorough differential list is important in considering a diagnosis of sciatica and should include:
- Herniated lumbosacral disc
- Cauda Equina syndrome
- Muscle spasm
- Nerve root impingement
- Epidural abscess
- Epidural hematoma
- Tumor
- Potts Disease, also known as spinal tuberculosis
- Piriformis syndrome
Evaluation[edit | edit source]
Sciatica is most commonly diagnosed by:
History:
Complaints of radiating pain in the leg, which follows a dermatomal pattern[6]
- Pain generally radiates below the knee, into the foot[7]
- Patients complain about low back pain, which is usually less severe than the leg pain[6]
- Patients may also report sensory symptoms.
Special tests:
Clinicians should always look for and inquire about red flags when evaluating sciatica or in patients who present with any low back pain. Patients with signs of urinary retention or decreased anal sphincter tone should be urgently referred for investigation as this suggests cauda equina syndrome.
- Lasègue’s test
Also called as straight leg raising test (SLR) is the most commonly performed physical test for diagnosis of sciatica and lumbar disc hernia . The SLR is considered positive when it evokes radiating pain along the course of the sciatic nerve and below the knee between 30 and 70 degrees of hip flexion. Studies of its capacity to diagnose lumbar disc hernia show high sensitivity but low specificity.[8]
- Bragard test
Bragard test is a modification of the SLR, where ankle dorsiflexion is applied at the end of the SLR. Dorsiflexion reduces the SLR angle at which the test is positive and can be used to differentiate neural symptoms from musculoskeletal symptoms.[8]
Also known as the popliteal compression test or posterior tibial nerve stretch sign. The patient can be examined in sitting or in a supine position. The examiner flexes the knee and applies pressure on the popliteal fossa, evoking sciatica. Some examiners do it after SLRT by flexing the knee to relieve the buttock pain. The pain would be reproduced by a quick snap on the posterior tibial nerve in the popliteal fossa.[10]
Imaging:
It may be used if pain persists for more than 12 weeks or the patient develops progressive neurological deficits[2]
- Plain films of the lumbosacral spine may evaluate for fracture or spondylolisthesis
- Noncontrast CT scan may be performed to evaluate fracture if plain films are negative
- In cases where the neurologic deficit is the present or mass effect is suspected, immediate MRI is the standard of care in establishing the cause of the pain and ruling out pressing surgical pathology[4]
Outcome Measures[edit | edit source]
Many to choose from, below are but a few, all dependant on cause and assessment.
- Short Form-36 bodily pain (SF-36 BP)
- Oswestry disability index
- Roland-Morris disability index
- VAS-score: one of leg pain and one of back pain[12]
- McGill pain Questionnaire[12]: this questionnaire looks at the location, intensity, quality and pattern of the pain as well as alleviating and aggravating factors[13]
- TUG
- Tampa Scale for Kinesiophobia[14]
- Pain Catastrophising Scale[14]
Medical Management[edit | edit source]
Most patients improve over time with conservative treatment including exercise, manual therapy, and pain management[2]
- Pharmacology: a short course of oral NSAIDs; Opioid and non-opioid analgesics; muscle relaxants; anticonvulsants for neurogenic pain; localized corticosteroid injections.
- Surgical evaluation: to address structural abnormalities such as: disc herniation, epidural hematoma, epidural abscess or tumour may be considered if no improvement following 6-8 weeks of conservative treatment[2]. One study found that although it may speed up recovery, the effect is similar to conservative care at one year[2]
- Physical therapy management
Physical Therapy Management[edit | edit source]
In most cases of sciatica, conservative treatment is favoured. The evidence does not show that one treatment is superior to the other[15]
Patient Education: to include information on the nature of low back back, advice on self-management techniques and encouragement to continue normal activities[16]
Promote self management techniques such as:
- use of hot or cold packs for comfort and to decreased inflammation
- avoidance of inciting activities or prolonged sitting/standing
- Regularly changing position i.e. from sitting to standing
- practicing good erect posture
- use of proper lifting techniques
Exercise:
exercises to increase core strength, gentle stretching of the lumbar spine and hamstrings, regular light exercise such as walking, swimming, or aquatherapy
Manual therapy: spinal manipulation, mobilisation or soft tissue techniques such as massage - used alongside exercise and patient education[16]
Comprehensive treatment:
- Disc Herniation
- Lumbar Discogenic Pain
- Spinal Stenosis
- Degenerative Disc Disease
- Spondylolisthesis
- Piriformis Syndrome
- Sacroiliac Joint Dysfunction
- Sciatic Nerve Injury
- Corticosteroid injections
- Acupuncture
- Massage therapy
Concluding Remarks[edit | edit source]
There are many causes of sciatica and the disorder is best managed with a team of healthcare professionals that includes an orthopedic surgeon, physical therapist, neurologist, rehabilitation nurse, and a pain specialist.
- The key to sciatica is patient education.
- The majority of cases of sciatica are best managed conservatively.
- Patients should be encouraged by the clinician and nurse to lose weight, stop smoking and enroll in a physical therapy program.
- Bed rest should be limited.
- The pharmacist should caution the patient against the use of prescription-strength medications to avoid dependence and other adverse effects.
- Surgery should only be undertaken when conservative methods have failed.
- Regular exercise is essential[4]
Summary[edit | edit source]
The following video gives a summary of sciatica:
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Davis D, Maini K, Vasudevan A. Sciatica. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2020. PMID: 29939685.
- ↑ 2.0 2.1 2.2 2.3 2.4 Jensen RK, Kongsted A, Kjaer P, Koes B. Diagnosis and treatment of sciatica. BMJ. 2019 Nov 19;367:l6273.
- ↑ 3.0 3.1 Osmosis. Sciatica. Available from: https://www.youtube.com/watch?v=VYj-JfX0wT0 (last accessed 15.3.2019)
- ↑ 4.0 4.1 4.2 4.3 Davis DH, Wilkinson JT, Teaford AK, Smigiel MR. Sciatica produced by a sacral perineurial cyst. Tex Med. 1987 Mar;83(3):55-6.
- ↑ 5.0 5.1 Parreira P, Maher CG, Steffens D, Hancock MJ, Ferreira ML. Risk factors for low back pain and sciatica: an umbrella review. Spine J. 2018 Sep;18(9):1715-1721.
- ↑ 6.0 6.1 6.2 Koes BW, van Tulder MW, Peul WC. Diagnosis and treatment of sciatica. BMJ. 2007 Jun 23;334(7607):1313-7.
- ↑ 7.0 7.1 Konstantinou K, Lewis M, Dunn KM. Agreement of self-reported items and clinically assessed nerve root involvement (or sciatica) in a primary care setting. Eur Spine J. 2012 Nov;21(11):2306-15.
- ↑ 8.0 8.1 Kamath SU, Kamath SS. Lasègue’s sign. J Clin Diagn Res [Internet]. 2017 [cited 2023 Mar 27];11(5):RG01–2. Available from: http://dx.doi.org/10.7860/JCDR/2017/24899.9794
- ↑ Clinical Examination Videos. Straight leg raise test - Lasegue’s sign [Internet]. Youtube; 2017 [cited 2023 Mar 27]. Available from: https://www.youtube.com/watch?v=JmvGHszR_X4
- ↑ Das JM, Nadi M. Lasegue Sign. StatPearls Publishing; 2022.
- ↑ CRTechnologies. Bowstring Test (CR). Available from: http://www.youtube.com/watch?v=orb-VI51QF0&t=11s [last accessed 03.04.2023]
- ↑ 12.0 12.1 Brouwer PA, Peul WC, Brand R, Arts MP, Koes BW, van den Berg AA, van Buchem MA. Effectiveness of percutaneous laser disc decompression versus conventional open discectomy in the treatment of lumbar disc herniation; design of a prospective randomized controlled trial. BMC Musculoskelet Disord. 2009 May 13;10:49.
- ↑ Ngamkham S, Vincent C, Finnegan L, Holden JE, Wang ZJ, Wilkie DJ. The McGill Pain Questionnaire as a multidimensional measure in people with cancer: an integrative review. Pain Manag Nurs. 2012 Mar;13(1):27-51.
- ↑ 14.0 14.1 Monticone M, Ferrante S, Teli M, Rocca B, Foti C, Lovi A, Brayda Bruno M. Management of catastrophising and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomised controlled trial. Eur Spine J. 2014 Jan;23(1):87-95.
- ↑ Luijsterburg PA, Verhagen AP, Ostelo RW, van Os TA, Peul WC, Koes BW. Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review. Eur Spine J. 2007 Jul;16(7):881-99.
- ↑ 16.0 16.1 National Institute for Health and Care Excellence (NICE). Low back pain and sciatica in over 16s: assessment and management: NICE Guideline [NG59] 2016. Available from https://www.nice.org.uk/guidance/ng59 [Accessed 13 Nov 2021]
- ↑ Physio Fitness | Physio REHAB | Tim Keeley. Treatment for lumbar spine disc bulge and sciatica - wk 1 | Feat. Tim Keeley | No.58 | Physio REHAB . Available from: http://www.youtube.com/watch?v=4t8L4zHQ2nQ&t=7s [last accessed 03.04.2023]