Cryotherapy
Definition/Description[edit | edit source]
Cryotherapy, also known as ice application, is the simplest and oldest way to treat injuries. Its worldwide use spread because of its effectiveness, convenience, low cost and ease of transportation. Ice is believed to control pain by instigating local anaesthesia. It also decreases oedema, nerve conduction velocities, cellular metabolism and local blood flow. The effect of the cryotherapy depends on the method, the duration, temperature of the ice and the depth of the subcutaneous fat. [1][2]
Application Methods[edit | edit source]
Ice Packs: It is most common method of cryotherapy. There are different types of ice used in ice packs. The most common types are ice packs made with cubed, crushed and wetted ice. It was discovered that wetted ice is better to lower surface temperature during treatment and maintaining the lower temperature during recovery. It is also more effective in lowering the intramuscular temperature during treatment.
Commercial Cold Packs: Commercial cold packs, such as ColPac and Elasto-Gel, are an efficient and commonly used method of cryotherapy. Usually filled with a petroleum distillate gel material, these cold packs are quicker to apply and reach lower temperatures than traditional ice packs.
Vapocoolant Spray: Utilized as a superficial, cooling agent for reduction of muscle guarding and release of myofascial trigger points.[3]
Immersion: Simple immersion, such as an ice bath, can be utilized for full concealment of a distal extremity (e.g., foot, ankle, hand, or wrist). Cold whirlpool is a form of immersion that transfers heat via convection
Ice Massage: Ice massage involves applying ice directly to the skin with slow strokes in circular motion for 5-10 mins. To achieve desired cooling effect, move the ice about 5-7cm/second.[3]
Whole Body Cryotherapy: More recently whole-body cryotherapy has become popular for athletes, to help aid recovery, as well as in persistent pain patients such as rheumatological conditions. More research is needed to understand the effect on the body and its relation to pain.
Indications[edit | edit source]
Cryotherapy can be utilized as an adjunct to treatment for the following conditions:[3]
- Acute soft tissue injuries (e.g., ankle sprain, muscular strain, ligament sprain)
- Myofascial trigger points
- Muscle spasm
- Muscle guarding
- Tendinitis
- Tenosynovitis
- Acute swelling
- Bursitis
- Post orthopaedic surgery (e.g., TKR, ACL reconstruction, arthroscopic shoulder surgery.)
- Reducing temperature
- DOMS
Contraindications[edit | edit source]
Be aware of conditions in which cryotherapy is contraindicated:
- CRPS
- Haemoglobinuria
- Cryoglobulinemia
- Peripheral vascular disease
- Impaired circulation
- Raynaud’s disease
- Urticaria
- Hypersensitivity to cold
- Skin anaesthesia
- Over a regenerating peripheral nerve
- Open wounds
Precautions[edit | edit source]
When applying cryotherapy, be cognizant of the following:
- Over a superficial nerve
- Hypertension
- Impaired cognition
- Patients who are very young or very old
Expected Sensations to Cryotherapy[edit | edit source]
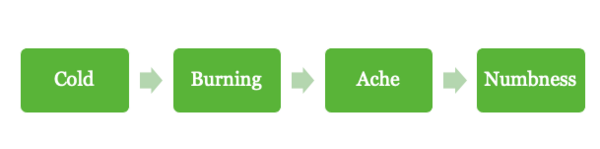
Prior to the application of cryotherapy, it is important to understand the expected sensations that one might expect. While the sensations listed may be uncomfortable, they are both normal and necessary to achieve the desired effects from cryotherapy. Throughout the duration of treatment, the expected sensations begin with a cold feeling and should reach numbness by the end.
Physiological Effects of Cryotherapy[edit | edit source]
The following physiologic effects are the expected responses to cryotherapy:[3]
- Decreased local temperature
- Decreased metabolism
- Vasoconstriction of arterioles and capillaries, initially
- Decreased blood flow, initially
- Decreased nerve conduction velocity
- Decreased delivery of leukocytes and phagocytes
- Decreased lymphatic and venous drainage
- Decreased muscle excitability
- Decreased muscle spindle depolarization
- Decreased formation and accumulation of edema
- Extreme anesthetic effects
Lewis Hunting Reaction[edit | edit source]
The Lewis hunting reaction is a process of alternating vasoconstriction and vasodilation in extremities exposed to cold. The term Lewis reaction is used too, named after Thomas Lewis, who first described the effect in 1930. Vasoconstriction occurs first to reduce heat loss, but also results in strong cooling of the extremities. Approximately five to ten minutes after the start of cold exposure, the blood vessels in the extremities will suddenly vasodilate. This is probably caused by a sudden decrease in the release of neurotransmitters from the sympathetic nerves to the muscular coat of the arteriovenous anastomoses due to local cold. This cold-induced vasodilation increases blood flow and subsequently the temperature of the fingers. A new phase of vasoconstriction follows the vasodilation, after which the process repeats itself.[5]
Vasodilation can be cold induced after initial period of vasoconstriction when cold is maintained for longer than approximately 15 min or when temperature is reduced below 10C.
Joint Mobilization with Cryotherapy[edit | edit source]
Evidence regarding cryotherapy suggests that analgesic effects are achieved when tissues are cooled down to 50°F to 60°F.[6] With decreased pain from the effects of the cyrotherapeutic agent, mobilizations will be accomplished with less pain and more effectiveness.
Along with the increase in pain threshold from cryotherapy, a decrease in muscle spindle activity can be observed with cryotherapy. This allows for a reduction in muscle guarding resulting in the ability to make greater gains in range of motion and joint mobilizations.[3]
Pros[edit | edit source]
- Pain relief[7]
- Swelling reduction[7]
- Decreased surface temperature
- Effective on a wide range of soft tissue injuries
Cons[edit | edit source]
- Little evidence regarding duration and frequency of treatment to be effective.[7]
- Compression has been shown to be more effective post operatively.[7]
- In rare cases bradycardia and frostbite symptoms have been observed. [8]
- Some more advanced cryotherapy devices can reduce range of movement following TKR due to immobilisation of the joint. [9]
Possible Risks/Undesirable Effects[edit | edit source]
- Inhibit Muscle Function
- Ice Burn
- Cryotherapy-induced nerve injuries
- Generalized cooling and decrease in core temperature
- Reduced range of motion
Inhibit Muscle Function[edit | edit source]
- Cooling can temporarily Inhibit muscle function with potential for increased risk of injury/re‐injury
- Be cautious when having patients weight bear/undertake complex exercise after icing a lower extremity
Ice Burn[edit | edit source]
Elderly patients with impaired sensation and/or circulation will be more vulnerable to an ice‐burn, therefore consider using less intense icing techniques (e.g., moderately cold ice pack wrapped in an insulating layer(s) of towel/cloth)
- Younger patients with intact sensation and circulation may benefit most from direct immersion of the limb in cold water then progressively adding ice cubes
- Cold gel packs stored in a freezer have a surface temperature below 0°C (32°F) and thus an insulating layer should be used between the cold pack and the patient’s skin
Cryotherapy‐Induced Nerve Injuries[edit | edit source]
- Most common when cold is applied in combination with compression
- Check capillary refill during application of ice combined with compression therapy to ensure adequate blood flow
Generalized Cooling and Decrease in Core Temperature[edit | edit source]
- Shivering and piloerection are signs of decrease in core temperature which may compromise patient safety (especially in the elderly and those with fever)
- The application of therapeutic cryotherapy should produce only local effects
Reduced ROM[edit | edit source]
Ice may contribute to shortening of collagen fibres in connective tissue
- After gaining ROM by warming, stretching and then strengthening in the newest part of the ROM, it is likely counterproductive to cool the tissue in a shortened position
- If one wishes to cool the tissue post stretch and exercise, it is best to do so with the tissue in a lengthened position
- In patients with significantly restricted ROM due to scar tissue, it may be preferable not to use ice.
Resources[edit | edit source]
- ↑ Bleakley C, McDonough S, MacAuley D. The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. The American journal of sports medicine. 2004 Jan;32(1):251-61.
- ↑ Dykstra JH, Hill HM, Miller MG, Cheatham CC, Michael TJ, Baker RJ. Comparisons of cubed ice, crushed ice, and wetted ice on intramuscular and surface temperature changes. Journal of athletic training. 2009 Mar;44(2):136-41.
- ↑ 3.0 3.1 3.2 3.3 3.4 Use WP, Prentice W. Therapeutic Modalities in Rehabilitation, Sixth Edition. 6th ed. Columbus, OH: McGraw-Hill Education; 2021.
- ↑ George Eliot Hospital. Applying an Icepack - Physiotherapy Advice Video Available from: https://www.youtube.com/watch?v=gJOMV2mZ1B0 [last accessed 28/09/2020]
- ↑ Daanen HA. Finger cold-induced vasodilation: a review. European journal of applied physiology. 2003 Jun 1;89(5):411-26.
- ↑ Speer KP, Warren RF, Horowitz L. The efficacy of cryotherapy in the postoperative shoulder. Journal of shoulder and elbow surgery. 1996 Jan 1;5(1):62-8.
- ↑ 7.0 7.1 7.2 7.3 Hubbard TJ, Denegar CR. Does cryotherapy improve outcomes with soft tissue injury?. Journal of athletic training. 2004 Jul;39(3):278.
- ↑ Galiuto L. The use of cryotherapy in acute sports injuries. Annals of Sports Medicine and Research. 2016;3(2):1060.
- ↑ Thienpont E. Does advanced cryotherapy reduce pain and narcotic consumption after knee arthroplasty?. Clinical Orthopaedics and Related Research®. 2014 Nov 1;472(11):3417-23.