Disc Herniation
Definition/Description[edit | edit source]
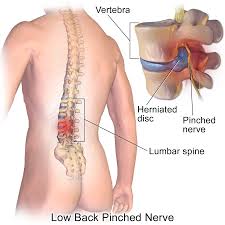
A herniated disc in the spine is a condition during which a nucleus pulposus is displaced from intervertebral space. It is a common cause of back pain. The patient's who experience pain related to a herniated disc often remember an inciting event that caused their pain. Unlike mechanical back pain, herniated disc pain is often burning or stinging, and may radiate into the lower extremity. Furthermore, in more severe cases, there can be associated with weakness or sensation changes. In some instances, a herniated disc injury may compress the nerve or the spinal cord causing pain consistent with nerve compression or spinal cord dysfunction, also known as myelopathy.[1].
Herniated Disc's:
- Can be very painful.
- Within a few weeks, most cases of painful disc herniation heal.
- In many instances, the herniation of the disc does not cause that patient any pain.
- Herniated discs are often seen on MRI of asymptomatic patients (MRI is the imaging modality of choice).
- The management of disc herniation requires an interprofessional team. The initial treatment should be conservative, unless a patient has severe neurological compromise.
- Surgery is usually the last resort as it does not always result in predictable results. Patients are often left with residual pain and neurological deficits, which are often worse after surgery.
- Physical therapy is the key for most patients. The outcomes depend on many factors but those who particpate in regular exercise and maintain a healthy body weight have better outcomes than people who are sedentary[2].
Clinically Relevant Anatomy[edit | edit source]
See Lumbar Anatomy for great detail
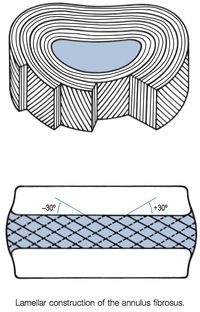
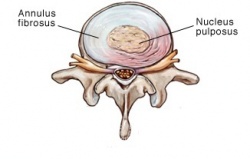
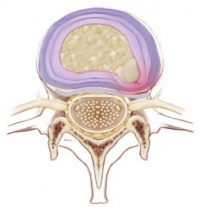
Intervertebral discs: Two adjacent vertebral bodies are linked by an intervertebral disc. Together with the corresponding facet joints, they form the ‘functional unit of Junghans’. The disc consists of an annulus fibrosus, a nucleus pulposus and two cartilaginous endplates. The distinction between annulus and nucleus can only be made in youth, because the consistency of the disc becomes more uniform in the elderly. For this reason, nuclear disc protrusions are rare after the age of 70. From a clinical point of view, it is important to consider the disc as one integrated unit, the normal function of which depends largely on the integrity of all the elements. That means that damage to one component will create adverse reactions in the others[4].
The disc contain an: Endplate; Annulus fibrosus; Nucleus pulposus
Etiology[edit | edit source]
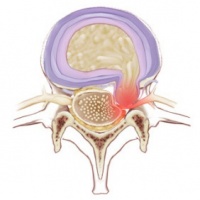
An intervertebral disc is composed of annulus fibrous which is a dense collagenous ring encircling the nucleus pulposus.
- Disc herniation occurs when part or all the nucleus pulposus protrudes through the annulus fibrous. This herniation process begins from failure in the innermost annulus rings and progresses radially outward.
- The damage to the annulus of the disc appears to be associated with fully flexing the spine for a repeated or prolonged period of time.
- A herniation may develop suddenly, or gradually over weeks or months.
- Causes
- Most common cause of disc herniation the degenerative process (as humans age, the nucleus pulposus becomes less hydrated and weakens and may lead to progressive disc herniation).
- The second most common cause of disc herniation is trauma.
- Other causes include connective tissue disorders and congenital disorders such as short pedicles.
- Disc herniation is:
- Most common in the lumbar spine
- Followed by the cervical spine. A high rate of disc herniation in the lumbar and cervical spine can be explained by an understanding of the biomechanical forces in the flexible part of the spine.
- The thoracic spine has a lower rate of disc herniation[2].
- Repetitive mechanical activities like twisting, bending, without breaks can lead to disc damage.
- Living a sedentary lifestyle, poor posture, obesity, tobacco abuse can also cause disc prolapse.
Pathophysiology[edit | edit source]
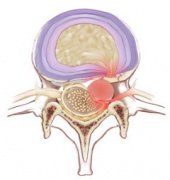
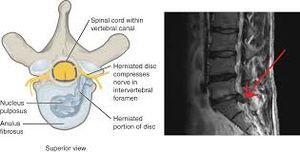
- The disc consists of the annulus fibrosus (a complex series of fibrous rings) and the nucleus pulposus (a gelatinous core containing collagen fibers, elastin fibers and a hydrated gel)[5]. The vertebral canal is formed by the vertebral bodies, intervertebral discs and ligaments on the anterior wall and by the vertebral arches and ligaments on the lateral wall. The spinal cord lies in this vertebral canal[6].
- The pathophysiology of herniated discs is believed to be a combination of the mechanical compression of the nerve by the bulging nucleus pulposus and the local increase in inflammatory chemokines.[2]
- A tear can occur within the annulus fibrosus. The material of the nucleus pulposus can track through this tear and into the intervertebral or vertebral foramen to impinge neural structure[6].
- The changes consists of nuclear degeneration, nuclear displacement and stage of fibrosis.
Types Of Herniations[edit | edit source]
- Posterolateral Disc Herniation - Protrusion is usually posterolateral into vertebral canal. Protruded disc usually compresses next lower nerve as the nerve crosses the level of disc in its path to its foramen. (Example: protrusion of L5 usually affects S1)
- Cental (posterior) Herniation - It is less frequent. A protruded disc above 2nd vertebra may compress the spinal cord itself or may lead to Cauda Equina Syndrome.
- Lateral Disc Herniation - Nerve root compression happens above the level of herniation. L4 nerve root is most often involved.
Stages Of Herniation[edit | edit source]
There are four stages of herniated discs [7] : Bulging; Protrusion; Extrusion; Sequestration (see image below)
Epidemiology[edit | edit source]
- The incidence of herniated disc is about 5 to 20 cases per 1000 adults annually and is most common in people in their third to the fifth decade of life, with a male to female ratio of 2:1.
- In 95% of the lumbar disc herniation the L4-L5 and L5-S1 discs are affected[8].
- Lumbar disc herniation occurs 15 times more than cervical disc herniation, and is an important cause of lower back pain[9][10].
- The prevalence of a symptomatic herniated lumbar disc is about 1% to 3% with the highest prevalence among people aged 30 to 50 years, with a male to female ratio of 2:1.
- In individuals aged 25 to 55 years, about 95% of herniated discs occur at the lower lumbar spine (L4/5 and L5/S1 level); disc herniation above this level is more common in people aged over 55 years[11].
- It occur rarely in children, and are most common in young and middle-aged adults.
- Recurrent lumbar disc herniation (rLDH) is a common complication following primary discectomy.
- The cervical disc herniation is most affected 8% of the time and most often at level C5-C6 and C6-C7.
History And Examination[edit | edit source]
Cervical Spine[edit | edit source]
History[edit | edit source]
In the cervical spine, the C6-7 is the most common herniation disc that causes symptoms, mostly radiculopathy. History in these patients should include the chief complaint, the onset of symptoms, where the pain starts and radiates. History should include if there are any past treatments.
Physical Examination[edit | edit source]
On physical examination, particular attention should be given to weaknesses and sensory disturbances, and their myotome and dermatomal distribution.
Typical findings of solitary nerve lesion due to compression by herniated disc in cervical spine
- C5 Nerve - neck, shoulder, and scapula pain, lateral arm numbness, and weakness during shoulder abduction, external rotation, elbow flexion, and forearm supination. The reflexes affected are the biceps and brachioradialis.
- C6 Nerve - neck, shoulder, scapula, and lateral arm, forearm, and hand pain, along with lateral forearm, thumb, and index finger numbness. Weakness during shoulder abduction, external rotation, elbow flexion, and forearm supination and pronation is common. The reflexes affected are the biceps and brachioradialis.
- C7 Nerve - neck, shoulder, middle finger pain are common, along with the index, middle finger, and palm numbness. Weakness on the elbow and wrist are common, along with weakness during radial extension, forearm pronation, and wrist flexion may occur. The reflex affected is the triceps.
- C8 Nerve - neck, shoulder, and medial forearm pain, with numbness on the medial forearm and medial hand. Weakness is common during finger extension, wrist (ulnar) extension, distal finger flexion, extension, abduction, and adduction, along with during distal thumb flexion. No reflexes are affected.
- T1 Nerve - pain is common in the neck, medial arm, and forearm, whereas numbness is common on the anterior arm and medial forearm. Weakness can occur during thumb abduction, distal thumb flexion, and finger abduction and adduction. No reflexes are affected.[2]
Lumbar Spine[edit | edit source]
History[edit | edit source]
In the lumbar spine, herniated disc can present with symptoms including sensory and motor abnormalities limited to specific myotome. History in these patients should include chief complaints, the onset of symptoms, where the pain starts and radiates. History should include if there are any past treatments.
Physical Examination[edit | edit source]
A careful neurological examination can help in localizing the level of the compression. The sensory loss, weakness, pain location and reflex loss associated with the different level are described below
Typical findings of solitary nerve lesion due to compression by herniated disc in lumbar spine
- L1 Nerve - pain and sensory loss are common in the inguinal region. Hip flexion weakness is rare, and no stretch reflex is affected.
- L2-L3-L4 Nerves - back pain radiating into the anterior thigh and medial lower leg; sensory loss to the anterior thigh and sometimes medial lower leg; hip flexion and adduction weakness, knee extension weakness; decreased patellar reflex.
- L5 Nerve - back, radiating into buttock, lateral thigh, lateral calf and dorsum foot, great toe; sensory loss on the lateral calf, dorsum of the foot, web space between first and second toe; weakness on hip abduction, knee flexion, foot dorsiflexion, toe extension and flexion, foot inversion and eversion; decreased semitendinosus/semimembranosus reflex.
- S1 Nerve - back, radiating into buttock, lateral or posterior thigh, posterior calf, lateral or plantar foot; sensory loss on posterior calf, lateral or plantar aspect of foot; weakness on hip extension, knee flexion, plantar flexion of the foot; Achilles tendon; Medial buttock, perineal, and perianal region; weakness may be minimal, with urinary and fecal incontinence as well as sexual dysfunction.
- S2-S4 Nerves - sacral or buttock pain radiating into the posterior aspect of the leg or the perineum; sensory deficit on the medial buttock, perineal, and perianal region; absent bulbocavernosus, anal wink reflex[2].
Signs And Symptoms[edit | edit source]
- Severe low back pain, radiating pain.
- Walking can be painful and difficult.
- Velsava Manuever.
- Muscle spasm, tingling sensation, weakness or atrophy.
- loss of bladder or bowel control.
- Some people may be asymptomatic.
- Slow and deliberate, tip-toe walking.
- Spine, trunk deviation.
- Antalgic or Trendelenburg gait.
- Paraspinal muscle spasm.
Special Tests[edit | edit source]
Cervical
Lumbar
- The straight leg raise test:
- The contralateral (crossed) straight leg raise test
- Lasègue’s Test - - see straight leg raise test
- Bowstring test
- Prone knee bending
- Muscle Weakness or Paresis
- Reflexes
- Hyperextension Test The patient needs to passively mobilise the trunk over the full range of extension, while the knees stay extended. The test indicates that the radiant pain is caused by disc herniation if the pain deteriorates.
- Manual Testing and Sensory Testing Look for hypoaesthesia, hypoalgesia, tingling or numbness
Differential Diagnosis[edit | edit source]
There are different pathologies that can imitate a herniated disc from the clinical and the imaging point of view, that should be considered .
These lesions include those originating from the
- vertebral body (osteophytes and metastases),
- intervertebral disc (discal cyst),
- intervertebral foramina (neurinomas)
- interapophyseal joints (synovial cyst)
- epidural space (hematoma and epidural abscess).[12]
Other differential diagnoses include
- Spondylolysis
- Spondylolisthesis
- Cauda equina syndrome
- Muscle spasm
- Mechanical pain
- Myofascial pain[13] (leads to local and/or referred pain, sensory disturbances)
Spinal causes include
- Trauma
- Infection - osteomyelitis
- Inflammation - arachnoiditis, ankylosing spondylitis
- Neoplasm - benign or malignant with nerve root pressure; multiple myeloma, extradural tumour.
Extraspinal causes include
- peripheral vascular disease
- gynacological condition
- OA hip
- sacroiliac joint disease
- peipheral nerve lesions
Complications[edit | edit source]
- Cauda Equina Syndrome
- Chronic pain
- Permanent nerve injury[14]
- Paralysis
Imaging[edit | edit source]
X-rays: These are very accessible at most clinics and outpatient offices. This imaging technique can be used to assess for any structural instability. If x-rays show an acute fracture, it needs to be further investigated using CT scan or MRI.
Narrowed disc space, loss of lumbar lordosis, complementary scoliosis can be observed.
CT Scan: It is preferred study to visualize bony structures in the spine. It can also show calcified herniated discs, size, shape of spinal cord, contents surrounding it including soft tissue. It is less accessible in the office settings compared to x-rays. But, it is more accessible than MRI. In the patients that have non-MRI comparable implanted devices, CT myelography can be performed to visualize herniated disc.
MRI: It is the preferred and most sensitive study to visualize herniated disc. MRI findings will help surgeons and other providers plan procedural care if it is indicated.[2] Disc protrusion and nerve root compression can be identified.
Outcome Measures[edit | edit source]
If the disc herniation is symptomatic different outcome measures can be used:
- Short Form-36 bodily pain (SF-36 BP)
- Oswestry disability index
- Roland-Morris disability index
- VAS-score: one of leg pain and one of back pain[15]
- McGill pain Questionnaire[15]: this questionnaire looks at the location, intensity, quality and pattern of the pain as well as alleviating and aggrevating factors[16].
Management[edit | edit source]
Medical Management[edit | edit source]
Acute cervical and lumbar radiculopathies due to herniated disc are primarily managed with non-surgical treatments.
- NSAIDs and physical therapy are the first-line treatment modalities.
- Oral steroids like prednisone, methyl prednisone.
- Benzodiazepines of low dose.
- Translaminar epidural injections and selective nerve root blocks are the second line modalities. These are good modalities for managing disabling pain.
- Patients who fail conservative treatment or patients with neurological deficits need timely surgical consultation[2].
Surgical Treatment[edit | edit source]
As always surgical treatment is the last resort.
- Surgical treatments for a herniated disc include laminectomies with discectomies, microdisectomies depending on the cervical or lumbar area.
- Patients with a herniated disc in the cervical spine can be managed via an anterior approach that requires anterior cervical decompression and fusion. This patient can also be managed with artificial disks replacement.
- Other alternative surgical approaches to the lumbar spine include a lateral or anterior approach that requires complete discectomy and fusion.[2]
- Intradiscal electrothermic therapy
- Nucleoplasty
- Chemonucleolysis
- Disc arthroplasty
Physical Therapy Management[edit | edit source]
Physical therapy often plays a major role in herniated disc recovery. Involving below key points
- Ambulation and resumption of exercise
- Pain control
- Education re maintaining healthy weight
Physical therapy programmes are often recommended for the treatment of pain and restoration of functional and neurological deficits associated with symptomatic disc herniation.
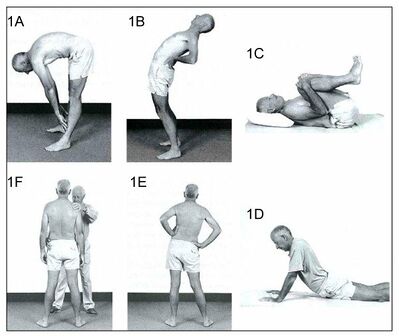
Active exercise therapy[edit | edit source]
It is preferred to passive modalities.
There are a number of exercise programmes for the treatment of symptomatic disc herniation eg
- aerobic activity (eg, walking, cycling)
- directional preference (McKenzie approach)
- flexibility exercises (eg, yoga and stretching)
- proprioception/coordination/balance (medicine ball and wobble/tilt board),
- strengthening exercises.
- motor control exercises MCEs
MCEs (stabilisation/core stability exercises)[edit | edit source]
They are a common type of therapeutic exercise prescribed for patients with symptomatic disc herniation[17].
- designed to re-educate the co-activation pattern of abdominals, paraspinals, gluteals, pelvic floor musculature and diaphragm
- The biological rationale for MCEs is primarily based on the idea that the stability and control of the spine are altered in patients with LBP.
- programme begins with recognition of the natural position of the spine (mid-range between lumbar flexion and extension range of motion), considered to be the position of balance and power for improving performance in various sports
- Initial low-level sustained isometric contraction of trunk-stabilising musculature and their progressive integration into functional tasks is the requirement of MCEs
- MCE is usually delivered in 1:1 supervised treatment sessions and sometimes includes palpation, ultrasound imaging and/or the use of pressure biofeedback units to provide feedback on the activation of trunk musculature
- A core stability program decreases pain level, improves functional status, increases health-related quality of life and static endurance of trunk muscles in lumbar disc herniation patients[18]. Individual high-quality trials found moderate evidence that stabilisation exercises are more effective than no treatment[19].
Different studies have shown that a combination of different techniques will form the optimal treatment for a herniated disc. Exercise and ergonomic programs should be considered as very important components of this combined therapy[20].
General rules for exercise/ Do and Donts[edit | edit source]
- Do exercise slowly. Hold exercise position for slow count of 5. Start with 5 repetition and work upto 10. Relax completely between the repetitions.
- Do exercise for 10 min twice a day.
- Care should be taken while doing exercise which can be painful.
- Exercise daily without fail.
Physiotherapy Modalities and the evidence for their use in disc herniation[edit | edit source]
- Stretching - There is low-quality evidence found to suggest that adding hyperextension to an intensive exercise programme might not be more effective than intensive exercise alone for functional status or pain outcomes. There were also no clinically relevant or statistically significant differences found in disability and pain between combined strength training and stretching, and strength training alone[21].
- Muscle Strengthening - Strong muscles are a great support system for your spine and better handle pain. If core stability is totally regained and fully under control, strength and power can be trained. But only when this is necessary for the patients functioning/activities. This power needs to be avoided during the core stability exercises because of the combination of its two components: force and velocity. This combination forms a higher risk to gain back problems and back pain[22].
- Traditional Chinese Medicine for Low Back Pain - has been demonstrated to be effective. Reviews have demonstrated that acupressure, acupuncture and cupping can be efficacious in pain and disability for chronic low back pain included disc herniation[23][24].
- Spinal Manipulative Therapy and Mobilization - Spinal manipulative therapy and mobilization leads to short-term pain relief when suffering from acute low back pain. When looking at chronic low back pain, manipulation has an effect similar to NSAID[25].
- Behavioural Graded Activity Programme - A global perceived recovery was better after a standard physiotherapy programme than after a behavioural graded activity programme in the short term, however no differences were noted in the long term[21].
- Transcutaneous Electrical Nerve Stimulation (TENS) - TENS therapy contribute to pain relief and improvement of function and mobility of the lumbosacral spine[26].
- Manipulative Treatment - Manipulative treatment on lumbar disc herniation appears to be safe, effective, and it seems to be better than other therapies. However high-quality evidence is needed to be further investigated[27].
- Traction - A recent study has shown that traction therapy has positive effects on pain, disability and SLR on patients with intervertebral disc herniation[28].Also one trial found some additional benefit from adding mechanical traction to medication and electrotherapy[29].
- Aquatic Vertical Traction - In patients with low back pain and signs of nerve root compression this method had greater effects on spinal height, the relieving of pain, lowering the centralisation response and lowering the intensity of pain than the assuming of a supine flexing position on land[30].
- Hot Therapies - may use heat to increase blood flow to the target area. Blood helps heal the area by delivering extra oxygen and nutrients. Blood also removes waste byproducts from muscle spasms[6].
- Cryotherapy - reduces spasm and inflammation in acute phase.
- Shortwave diathermy - pulsed SWD in acute condition and continuous SWD in chronic condition.
- Ultrasound - As phonophoresis, it increases extensibility of connective tissues.
Example of Protocol for Rehabilitation Following a Lumbar Microdiscectomy[edit | edit source]
The following program is an example of a protocol for rehabilitation following a lumbar microdiscectomy[31]:
- Duration of rehabilitation program: 4 weeks
- Frequency: every day
- Duration of one session: approximately 60 minutes
- Treatment: dynamic lumbar stabilization exercises + home exercises
- Exercises: Prior to the DLS training session patients are provided with instruction or technique to ensure and protect a neutral spine position. During the first 15 minutes of each session stretching of back extensors, hip flexors, hamstrings and Achilles tendon should be performed.
(DLS consists of: Quadratus exercises Abdominal strengthening Bridging with ball Straightening of external abdominal oblique muscle Lifting one leg in crawling position Lifting crossed arms and legs in crawling position Lunges)
- Home Exercises - should be added to the treatment. These should be performed every day. 5 repetitions during the first week up to 10-15 reps in the following weeks
Post Surgical Intervention[edit | edit source]
In case of surgery, programmes start regularly 4-6 weeks post-surgery[32]
- offer information about the rehabilitation program they will follow the next few weeks.
- The patients are instructed and accompanied in daily activities such as: coming out of bed, going to the bathroom and clothing
- patients have to pay attention on the ergonomics of the back throughout back school[33][32][31][34].
Studies show various forms of post operation treatment show
- rehabilitation programmes that start four to six weeks post-surgery with exercises versus no treatment found that exercise programmes are more effective than no treatment in terms of short-term follow-up for pain
- high-intensity exercise programmes are slightly more effective for pain and in terms of functional status in the short term compared with low-intensity exercise programmes.
- long-term follow-up results for both pain and functional status showed no significant differences between groups.
- no significant differences between supervised exercise programmes and home exercise programmes in terms of short-term pain relief[21].
Clinical Bottom line[edit | edit source]
- The initial treatment should be conservative, unless a patient has severe neurological compromise. Surgery is usually the last resort as it does not always result in predictable results. Patients are often left with residual pain and neurological deficits, which are often worse after surgery. Physical therapy is the key for most patients. The outcomes depend on many factors but those who particpate in regular exercise and maintain a healthy body weight have better outcomes than people who are sedentary.[2]
- Intervertebral disc herniation is one of most common diseases that produces low back pain and/or leg pain in adults. It often occurs as a result of age-related degeneration of the annulus fibrosis. Disc herniation are most of the time asymptomatic and 75% of the intervertebral disc herniation recover spontaneously within 6 months.
- Disc herniation can occur at different levels in the spine. A herniated disc affects most commonly the lumbar discs between vertebra L4-L5 and L5-S1. Cervical disc herniation are more rare than lumbar disc degeneration. The cervical disc herniation is most locate at level C5-C6 and C6-C7.
Further Reading[edit | edit source]
- Intervertebral disc
- The nerve supply of the lumbar intervertebral disc
- The Degenerated Lumbar Intervertebral Disc is Innervated Primarily by Peptide-Containing Sensory Nerve Fibers in Humans
References[edit | edit source]
- ↑ Dydyk AM, Massa RN, Mesfin FB. Disc Herniation. StatPearls [Internet]. 2020 Apr 22.Available: https://www.statpearls.com/articlelibrary/viewarticle/20584/(accessed 14.6.2021)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Dulebohn SC, Massa RN, Mesfin FB. Disc Herniation.Available from:https://www.ncbi.nlm.nih.gov/books/NBK441822/ (last accessed 25.1.2020)
- ↑ Herniated Disc - Patient Education. Available from:https://www.youtube.com/watch?v=lZm4j6Ls128 (last accessed 13.09.2021)
- ↑ Musculoskeletal key Applied anatomy of the lumbar spine Available from:https://musculoskeletalkey.com/applied-anatomy-of-the-lumbar-spine/ (last accessed 24.1.2020)
- ↑ Raj, P. Prithvi. "Intervertebral Disc: Anatomy‐Physiology‐Pathophysiology‐Treatment." Pain Practice 8.1 (2008): 18-44.
- ↑ 6.0 6.1 6.2 Drake, Richard, A. Wayne Vogl, and Adam WM Mitchell. Gray's anatomy for students. Elsevier Health Sciences, 2014
- ↑ L. G. F. Giles, K. P. Singer. The Clinical Anatomy and Management of Back Pain. Butterworth-Heinemann, 2006.
- ↑ McGill, S. Low Back Disorders: Evidence Based Prevention and Rehabilitation, Second Edition. USA: 2007 Human Kinetics.
- ↑ Jegede KA, etal. Contemporary management of symptomatic lumbar disc herniations. Orthop Clin North Am. 2010;41:217-24. PMID: 20399360 www.ncbi.nlm.nih.gov/pubmed/20399360.
- ↑ Chou R, etal. Nonsurgical interventional therapies for low back pain: a review of the evidence for an American Pain Society clinical practice guideline. Spine. 2009;
- ↑ LaxmaiahManchikanti etal; An Update of Comprehensive Evidence-Based Guidelines for Interventional Techniques in Chronic Spinal Pain. Part II: Guidance and Recommendations. Pain Physician 2013; 16:S49-S283 • ISSN 1533-3159
- ↑ Marcelo Gálvez M.1 , Jorge Cordovez M.1 , Cecilia Okuma P.1 , Carlos Montoya M.2, Takeshi Asahi K.2 Revista Chilena de Radiología. Vol. 23 Nº 2, año 2017; 66-76 Differential diagnoses for disc herniation. Available from:https://www.webcir.org/revistavirtual/articulos/2017/3_agosto/ch/hernia_eng.pdf (last accessed 25.1.2020)
- ↑ Simeone, F.A.; Herkowitz, H.N.; Upper lumbar disc herniations. J Spinal Disord. 1993 Aug;6(4):351-9.
- ↑ Slipped disc. Health line. Available from https://www.healthline.com/health/herniated-disk#:~:text=An%20untreated%2C%20severe%20slipped%20disc,is%20known%20as%20saddle%20anesthesia. [last accessed 13/10/2020]
- ↑ 15.0 15.1 Brouwer, Patrick A., et al. "Effectiveness of percutaneous laser disc decompression versus conventional open discectomy in the treatment of lumbar disc herniation; design of a prospective randomized controlled trial." BMC musculoskeletal disorders 10.1 (2009)
- ↑ Ngamkham, Srisuda, et al. "The McGill Pain Questionnaire as a multidimensional measure in people with cancer: an integrative review." Pain Management Nursing 13.1 (2012): 27- 51. Level of evidence: 2a
- ↑ Pourahmadi MR, Taghipour M, Takamjani IE, Sanjari MA, Mohseni-Bandpei MA, Keshtkar AA. Motor control exercise for symptomatic lumbar disc herniation: protocol for a systematic review and meta-analysis. BMJ open. 2016 Sep 1;6(9). Available from:https://bmjopen.bmj.com/content/6/9/e012426 (last accessed 25.1.2020)
- ↑ Bayraktar D et al., A comparison of water-based and land-based core stability exercises in patients with lumbar disc herniation: a pilot study. Disability and Rehabilitation. 2015 Sep 2:1-9.
- ↑ . Hahne A.J. et al. Conservative management of lumbar disc herniation with associated radiculopathy: a systematic review, Spine, 2010; 15, 35: 488-504.
- ↑ Olson K., Manual Physical Therapy of Spine, Saunders Elsevier, 2009, p114-116.
- ↑ 21.0 21.1 21.2 Oosterhuis, Teddy, et al. "Rehabilitation after lumbar disc surgery." The Cochrane Library (2014).
- ↑ Wong, J. J., et al. "Clinical practice guidelines for the noninvasive management of low back pain: A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration." European Journal of Pain (2016). (Level of evidence: 1A)
- ↑ Olson K., Manual Physical Therapy of Spine, Saunders Elsevier, 2009, p114-116
- ↑ Jioun Choi MS., Influences of spinal decompression therapy and general traction therapy on the pain, disability, and straight leg raising of patients with intervertebral disc herniation, J Phys Ther Sci. 2015 Feb; 27(2): 481–483.
- ↑ Demir S., Effects of dynamic lumbar stabilization exercises following lumbar microdiscectomy on pain, mobility and return to work. Randomized controlled trial., Eur J Phys Rehabil Med. 2014 Dec;50(6):627-40. Epub 2014 Sep 9.
- ↑ Pop, T., et al. "Effect of TENS on pain relief in patients with degenerative disc disease in lumbosacral spine." Ortopedia, traumatologia, rehabilitacja 12.4 (2009): 289-300.
- ↑ Li, L., et al. "[Systematic review of clinical randomized controlled trials on manipulative treatment of lumbar disc herniation]." Zhongguo gu shang= China journal of orthopaedics and traumatology 23.9 (2010): 696-700.
- ↑ . Jioun Choi MS., Influences of spinal decompression therapy and general traction therapy on the pain, disability, and straight leg raising of patients with intervertebral disc herniation, J Phys Ther Sci. 2015 Feb; 27(2): 481–483. Level of evidence: 2B
- ↑ Jordan, Jo, Kika Konstantinou, and John O'Dowd. "Herniated lumbar disc." BMJ clinical evidence 2011 (2011).
- ↑ Simmerman, Susanne M., et al. "Immediate changes in spinal height and pain after aquatic vertical traction in patients with persistent low back symptoms: A crossover clinical trial." PM&R 3.5 (2011): 447-457. Level of evidence: 2b
- ↑ 31.0 31.1 Mustafa Filiz, A. C. (2005). The effectiveness of exercise programmes after lumbar disc surgery: a randomised controlled trial. Clinical Rehabilitation, 4-11.
- ↑ 32.0 32.1 Raymond W. J. G Ostelo et al. Rehabilitation After Lumbar Disc Surgery: An update Cochrane Review. Spine Vol. 34 Nr.2009;17, 1839 - 1848.
- ↑ Ann-Christin Johansson, S. J. (2009). Clinic-based training in comparison to home-based training after first-time lumbar disc surgery: a randomised controlled trial. Eur Spine Journal , 398-409.
- ↑ Cele B. Erdogmus, K.-L. R. (2007 Vol.32 Nr.19). Physiotherapy-Based Rehabilitation Following Disc Herniation Operation. Spine , 2041-2049.