Radiculopathy
Original Editor - Daan Vandebriel
Top Contributors - Muhammad Osama, Kim Jackson, Wendy Walker, Khloud Shreif, Daan Vandebriel, Ellen Hopmans, Joao Costa and Amrita Patro
Description[edit | edit source]
Radiculopathy is a clinical condition which involves one or more nerves resulting in impaired function (a neuropathy). The site of injury in radiculopathy is at the level of the spinal nerve root. The result is pain (known as radicular pain), weakness in limbs, numbness/paresthesia, and difficulty in controlling specific muscles.
In radiculopathy, the problem occurs at or near the site of the origin of the nerve root as it exits from the spinal cord, but the pain and accompanying symptoms usually radiate to the part of the body that is supplied by that specific nerve. For example, a nerve root impingement in the cervical spine may result in pain and weakness in the forearm. Similarly, an impingement in the lumbar region can be manifested with symptoms in the foot.
The radicular pain that results from radiculopathy should not be confused with referred pain, which is different both in mechanism and clinical features. Polyradiculopathy is a condition in which more than one spinal nerve root is affected.
Epidemiology[edit | edit source]
Cervical radiculopathy is found to be less prevalent in the USA than lumbar radiculopathy, with an overall occurrence of 83 cases per 100,000 population. The most common age group for cervical radiculopathy is found to be from 40th – 50th. Female gender, white race, and cigarette smoking are considered to be risk factors. With an incidence of 1.79 per 1000, 63.5 per 100,000 for females, and 107.3 per 100,000 for males[1][2]. Private insurance is found to be the paying party in 41.69% of the incidents followed by Medicare in 38.81% incidents. Geographically, the South is the most severely affected region in the US with 39.27% of cases. According to a study conducted in the state of Minnesota, the most common site is the C7 monoradiculopathy, followed by C6 [3]. Lumbar radiculopathy prevalence 3%-5% of the population[4].
Clinically Relevant Anatomy[edit | edit source]
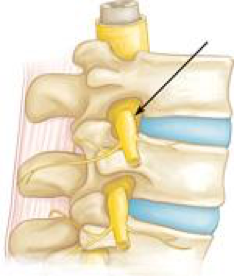
Radiculopathy is a mechanical compression of a nerve root usually at the exit foramen or lateral recess. It may be secondary to degenerative disc disease, osteoarthritis, facet joint degeneration/hypertrophy, ligamentous hypertrophy, spondylolisthesis, or a combination of these factors. Rarer causes of radiculopathy may include radiation, diabetes mellitus, neoplastic disease, or any meningeal-based disease process.
Radiculopathy can occur in any part of the spine but the most common site of radiculopathy is the cervical (Cervical Radiculopathy) and the lumbar spine (Lumbar Radiculopathy). It is less commonly found in the middle portion of the spine (thoracic radiculopathy) [5].
Certain injuries can also lead to radiculopathy. These injuries include lifting heavy objects improperly or suffering from a minor trauma such as a car accident. Less common causes of radiculopathy include injury caused by tumor (which can compress nerve roots locally) and diabetes (which can effectively cause ischemia or lack of blood flow to nerves).
Clinical Presentation[edit | edit source]
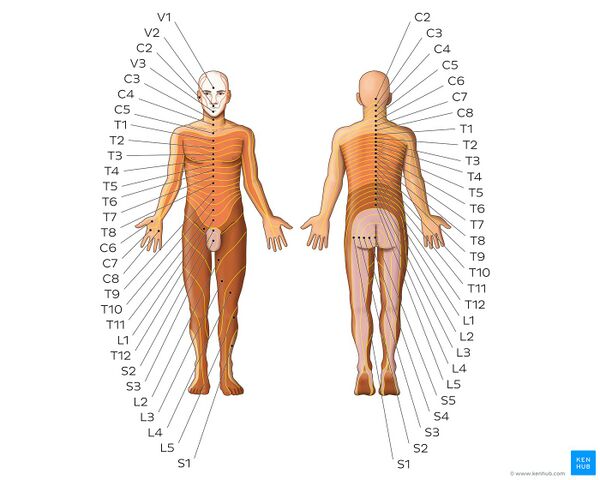
The symptoms of radiculopathy depend on which nerves are affected. The nerves exiting from the neck (cervical spine) control the muscles of the neck and arms and supply sensation there. The nerves from the middle portion of the back (thoracic spine) control the muscles of the chest and abdomen and supply sensation there. The nerves from the lower back (lumbar spine) control the muscles of the buttocks and legs and supply sensation there.
The most common symptoms of radiculopathy are pain, numbness, and tingling in the arms or legs. It is common for patients to also have localized neck or back pain as well. Lumbar radiculopathy that causes pain that radiates down a lower extremity is commonly referred to as sciatica. Thoracic radiculopathy causes pain from the middle back that travels around to the chest, it is often mistaken for shingles.
Some patients develop a hypersensitivity to light touch that feels painful in the area involved. Less commonly, patients can develop weakness in the muscles controlled by the affected nerves. This can indicate nerve damage[6].
Image: Dermatomes - Keegan and Garrett map[7]
Diagnostic Procedures[edit | edit source]
Radiculopathy's diagnosis commonly made by physicians in primary care specialties, Chiropractic, orthopedics, physiatry, and neurology. The diagnosis may be suggested by symptoms of pain, numbness, and weakness in a pattern consistent with the distribution of a particular nerve root. Neck pain or back pain may also be present.
Physical examination may reveal motor and sensory deficits in the distribution of a nerve root. For example, in the case of cervical radiculopathy, Spurling's test may elicit or reproduce symptoms radiating down the arm. In the case of lumbar radiculopathy, a Straight leg raise (SLR) maneuver may exacerbate symptoms. Deep tendon reflexes (also known as a Stretch reflex) may be diminished or absent in areas innervated by a particular nerve root.
For further workup, the American College of Radiology recommends that projectional radiography is the most appropriate initial study in all patients with chronic neck pain. Two additional diagnostic tests that may be of use are magnetic resonance imaging and electrodiagnostic testing, consisting of NCS (Nerve conduction study) and EMG (Electromyography),
On nerve conduction studies, the pattern of diminished compound muscle action potential and normal sensory nerve action potential may be seen given that the lesion is proximal to the Posterior root ganglion. Needle EMG is the more sensitive portion of the test and may reveal active denervation in the distribution of the involved nerve root, and neurogenic-appearing voluntary motor units in more chronic radiculopathies. Given the key role of electrodiagnostic testing in the diagnosis of acute and chronic radiculopathies, the American Association of Neuromuscular & Electrodiagnostic Medicine has issued evidence-based practice guidelines, for the diagnosis of both cervical and lumbosacral radiculopathies[8][9]. The American Association of Neuromuscular & Electrodiagnostic Medicine has also participated in the Choosing Wisely Campaign and several of their recommendations relate to what tests are unnecessary for neck and back pain[10].
Outcome Measures for Cervical Radiculopathy[edit | edit source]
- Neck disability index (NDI)
- Patient Specific Functional Scale (PSFS)
- Numerical Pain Rating Scale (NPRS)
- Neck Pain and Disability Scale (NPAD)
Outcome Measures for Lumbar Radiculopathy[edit | edit source]
- Roland Morris Disability Questionnaire (RMDQ)
- Back Pain Functional Scale
- The Maine-Seattle Back Questionnaire
- Fear Avoidance Belief Questionnaire (FABQ)
- Oswestry Low Back Pain Disability Questionnaire
- The Quebec back pain disability scale (QBPDS)
Medical Management[edit | edit source]
Fortunately, most people can obtain good relief of their symptoms of radiculopathy with conservative treatment. This may include anti-inflammatory medications, physical therapy or chiropractic treatment, and avoiding activity that strains the neck or back. The majority of radiculopathy patients respond well to this conservative treatment.
If patients do not improve with the treatments listed above they may benefit from an epidural steroid injection. With the help of an X-ray machine. It is a rapid short-term treatment to reduce the inflammation, and irritation of the nerve and help reduce the symptoms of radiculopathy[11][12].
While conservative approaches for rehabilitation are ideal, some patients will not improve and surgery is still an option. Patients with large cervical disc bulges may be recommended for surgery, however, most often conservative management will help the herniation regress naturally[13]. The goal of the surgery is to remove the compression from the affected nerve. Depending on the cause of the radiculopathy, this can be done by a laminectomy or a discectomy. A laminectomy removes a small portion of the bone covering the nerve to allow it to have additional space. A discectomy removes the portion of the disc that has herniated out and is compressing a nerve.
Physical Therapy Management[edit | edit source]
Ideally, effective treatment aims to resolve the underlying cause and restores the nerve root to normal function. Common conservative treatment approaches include physical therapy and chiropractic.
A systematic review found moderate-quality evidence that spinal manipulation is effective for the treatment of acute lumbar radiculopathy[9] and cervical radiculopathy [14][15]. But there is no evidence about the safety of cervical spine manipulation.[16] Only low level evidence was found to support spinal manipulation for the treatment of chronic lumbar radiculopathies, and no evidence was found to exist for the treatment of thoracic radiculopathy[16]. Also for patients with lumbar nerve root compression, lumbar traction as extra treatment is not superior to extension-oriented exercises alone[17].
Therapeutic exercises are frequently used in combination with many of the previously mentioned modalities and with great results. Following one of the studies adding mechanical traction to exercise for patients with cervical radiculopathy results in long term positive effects on disability and pain[18]. A variety of exercise regimens are available for patient treatment. An exercise regimen should be modified according to the abilities and weaknesses of the patient [19].
For further details on the management of radiculopathy, read the following articles;
Differential Diagnosis[edit | edit source]
Pathologies which mimic the signs and symptoms of radiculopathy are[20].
- Spinal Tumor
- Systemic diseases known to cause peripheral neuropathies
- Cervical myelopathy
- Ligamentous Instability
- Vertebral Artery Insufficiency (VBI)
- Herniated nucleous pulposos (HNP)
- Shoulder Pathology
- Peripheral nerve disorders
- Thoracic outlet syndrome
- Brachial plexus pathology
- Systemic disease
- Parsonage-Turner syndrome
- Superior pulmonary sulcus tumor
Resources[edit | edit source]
References[edit | edit source]
- ↑ Iyer S, Kim HJ. Cervical radiculopathy. Current reviews in musculoskeletal medicine. 2016 Sep;9(3):272-80.
- ↑ Schoenfeld AJ, George AA, Bader JO, Caram Jr PM. Incidence and epidemiology of cervical radiculopathy in the United States military: 2000 to 2009. Clinical Spine Surgery. 2012 Feb 1;25(1):17-22.
- ↑ Radhakrishnan K, Litchy WJ, O'fallon WM, Kurland LT. Epidemiology of cervical radiculopathy: a population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994 Apr 1;117(2):325-35.
- ↑ Berry JA, Elia C, Saini HS, Miulli DE. A review of lumbar radiculopathy, diagnosis, and treatment. Cureus. 2019 Oct;11(10).
- ↑ Iversen T, Solberg TK, Romner B, Wilsgaard T, Nygaard Ø, Brox JI, Ingebrigtsen T. Accuracy of physical examination for chronic lumbar radiculopathy. BMC musculoskeletal disorders. 2013 Dec;14(1):1-9.
- ↑ Eck, Jason C. "Radiculopathy". MedicineNet.com. Retrieved 12 April 2012.
- ↑ Dermatomes - Keegan and Garrett map image - © Kenhub https://www.kenhub.com/en/library/anatomy/dermatomes
- ↑ Fuglsang-Frederiksen A, Pugdahl K. Current status on electrodiagnostic standards and guidelines in neuromuscular disorders. Clinical Neurophysiology. 2011 Mar 31;122(3):440-55.
- ↑ 9.0 9.1 Cho SC, Ferrante MA, Levin KH, Harmon RL, So YT. Utility of electrodiagnostic testing in evaluating patients with lumbosacral radiculopathy: An evidence‐based review. Muscle & nerve. 2010 Aug;42(2):276-82.
- ↑ Meekins GD, So Y, Quan D. American Association of Neuromuscular & Electrodiagnostic Medicine evidenced‐based review: Use of surface electromyography in the diagnosis and study of neuromuscular disorders. Muscle & Nerve: Official Journal of the American Association of Electrodiagnostic Medicine. 2008 Oct;38(4):1219-24.
- ↑ House LM, Barrette K, Mattie R, McCormick ZL. Cervical epidural steroid injection: techniques and evidence. Physical Medicine and Rehabilitation Clinics. 2018 Feb 1;29(1):1-7.
- ↑ Rivera CE. Lumbar epidural steroid injections. Physical Medicine and Rehabilitation Clinics. 2018 Feb 1;29(1):73-92.
- ↑ Heckmann JG, Lang CJ, Zöbelein I, Laumer R, Druschky A, Neundörfer B. Herniated cervical intervertebral discs with radiculopathy: an outcome study of conservatively or surgically treated patients. Journal of spinal disorders. 1999 Oct 1;12(5):396-401.
- ↑ Leininger B, Bronfort G, Evans R, Reiter T. Spinal manipulation or mobilization for radiculopathy: a systematic review. Physical Medicine and Rehabilitation Clinics. 2011 Feb 1;22(1):105-25.
- ↑ Young IA, Pozzi F, Dunning J, Linkonis R, Michener LA. Immediate and Short-term Effects of Thoracic Spine Manipulation in Patients With Cervical Radiculopathy: A Randomized Controlled Trial. journal of orthopaedic & sports physical therapy. 2019 May;49(5):299-309.
- ↑ 16.0 16.1 Zhu L, Wei X, Wang S. Does cervical spine manipulation reduce pain in people with degenerative cervical radiculopathy? A systematic review of the evidence, and a meta-analysis. Clinical Rehabilitation. 2016 Feb;30(2):145-55.
- ↑ Thackeray A, Fritz JM, Childs JD, Brennan GP. The effectiveness of mechanical traction among subgroups of patients with low back pain and leg pain: a randomized trial. journal of orthopaedic & sports physical therapy. 2016 Mar;46(3):144-54.
- ↑ Fritz JM, Thackeray A, Brennan GP, Childs JD. Exercise only, exercise with mechanical traction, or exercise with over-door traction for patients with cervical radiculopathy, with or without consideration of status on a previously described subgrouping rule: a randomized clinical trial. journal of orthopaedic & sports physical therapy. 2014 Feb;44(2):45-57.
- ↑ Cleland JA, Whitman JM, Fritz JM, Palmer JA. Manual physical therapy, cervical traction, and strengthening exercises in patients with cervical radiculopathy: a case series. Journal of Orthopaedic & Sports Physical Therapy. 2005 Dec;35(12):802-11.
- ↑ Mamula CJ, Erhard RE, Piva SR. Cervical radiculopathy or Parsonage-Turner syndrome: differential diagnosis of a patient with neck and upper extremity symptoms. Journal of Orthopaedic & Sports Physical Therapy. 2005 Oct;35(10):659-64.