MRI Scans
Original Editor - Rachael Lowe
Top Contributors - Lucinda hampton, Andeela Hafeez, Admin, Kim Jackson, Rachael Lowe, Scott Buxton, Naomi O'Reilly, Karen Wilson and Claire Knott
Introduction[edit | edit source]
Magnetic Resonance Imaging (MRI) is a map of hydrogen atoms within the body. Hydrogen atoms are ideal for MRI because they possess a single proton and a large magnetic moment.
- In simple terms, an MRI scanner consists of a large, powerful magnet in which the patient lies.
- The magnetic field created by the magnets causes resonance from each proton in the hydrogen atom and the machine is able to obtain the proton’s position.
- Since approximately 75% of our bodies are made of water molecules, MR imaging is able to capture precise and detailed images of the viewed body region.
- The signal emitted by each type of cell is distinct, allowing the identification of various types of tissue, including bone, joints, muscle and cartilage. Imaging of any part of the body can be obtained in any plane[1]
- The MRI takes a detailed "picture" of all hydrogen molecules in the body and is computed into an accurate representation of that body region.
There are multiple types of MRI based on if the image is captured at a different decay of signal. A T1 weighted MRI captures early signal decay, that is, early after the protons are positioned. A T2 weighted MRI captures the late stage of signal decay, or after a small amount of proton migration from the original resonsance.[2]
Why Use[edit | edit source]
MRI scans have a wide range of application in medical diagnosis.[3]
Uses include:
- Neuroimaging: MRI is the investigative tool of choice for neurological cancers as it is more sensitive than CT for small tumours and offers better visualization of the posterior fossa. The contrast provided between grey and white matter makes it the optimal choice for many conditions of the central nervous system including demyelinating diseases (eg MS), dementia, cerebrovascular disease, infectious diseases and epilepsy[4]
2. Functional magnetic resonance imaging (fMRI): fMRI is based on the same technology as magnetic resonance imaging (MRI), a noninvasive test that uses a strong magnetic field and radio waves to create detailed images of the body. But instead of creating images of organs and tissues like MRI, fMRI looks at blood flow in the brain to detect areas of activity. These changes in blood flow, which are captured on a computer, help doctors understand more about how the brain works and shows which parts of the brain are most active. An fMRI can detect brain problems, such as the effects of a stroke, or it can be used for brain mapping if you need brain surgery for epilepsy or tumors.[5]
3. Cardiovascular Image 3: Cardiac MRI flow visualization
- Cardiac MRI is complementary to other imaging techniques, such as echocardiography, cardiac CT and nuclear medicine. Its applications include assessment of myocardial ischemia and viability, cardiomyopathies, myocarditis, iron overload, vascular diseases and congenital heart disease[6].
- Magnetic resonance angiography: (usually shortened to MR angiography or MRA) is an alternative to conventional angiography and CT angiography, eliminating the need for ionising radiation and iodinated contrast media, and sometimes contrast media altogether. It has evolved into several techniques with different advantages and applications:
- contrast enhanced MR angiography (MRA)
- non-contrast enhanced MR angiography (MRA)[7]
4. Musculoskeletal: Applications in the musculoskeletal system include spinal imaging, assessment of joint disease and soft tissue tumors[8]
5. Oncology: MRI is the investigation of choice in the preoperative staging of colorectal and prostate cancer, and has a role in the diagnosis, staging, and follow-up of other tumors.[9] Cancerous tissue contains more water than healthy tissue. The excess water resonates for longer in an MRI machine, making the tumor distinct from surrounding tissue in the image generated.[10]
6. Liver and gastrointestinal MRI: Hepatobiliary MRI is used to detect and characterize lesions of the liver, pancreas and bile ducts. Extracellular contrast agents are widely used in liver MRI and newer hepatobiliary contrast agents also provide the opportunity to perform functional biliary imaging.[11]
Key Points[edit | edit source]
- MRIs are a superior imaging modality for viewing soft tissues.
- T1 and T2 weighted images (see below) represent the core types of MR images.
- T1 and T2 images may be adjusted: fat-suppressed, gadolinium-enhanced and inversion recovery.
- The different sequences tell you what is in the lesion and how it is behaving. Using these features, the location of the lesion, and the clinical history, we can make a diagnosis[12]
Advantages and Disadvantages of MRI[edit | edit source]
Advantages of MRI[edit | edit source]
- ability to image without the use of ionising x-rays, in contradistinction to CT scanning
- images may be acquired in multiple planes (axial, sagittal, coronal, or oblique) without repositioning the patient. CT images have only relatively recently been able to be reconstructed in multiple planes with the same spatial resolution (i.e. isotropic voxels)
- MRI images demonstrate superior soft-tissue contrast as compared to CT scans and plain radiographs making it the ideal examination of the brain, spine, joints, and other soft tissue body parts
- some angiographic images can be obtained without the use of contrast material, unlike CT or conventional angiography
- advanced techniques such as diffusion, spectroscopy, and perfusion allow for precise tissue characterisation rather than merely 'macroscopic' imaging
- functional MRI allows visualisation of active parts of the brain during certain activities and also understanding of the underlying networks
Disadvantages of MRI
- MRI scans are more expensive than CT scans
- MRI scans take significantly longer to acquire than CT and patient comfort can be an issue, maybe exacerbated by:
- MR image acquisition is noisy compared to CT
- MRI scanner bores tend to be more enclosed than CT with associated claustrophobia. NB The creation of open MRI machines has made the experience more pleasant for children and those who suffer symptoms of claustrophobia.[10]
- MR images are subject to unique artifacts that must be recognised and mitigated against (see MRI artifacts)
- MRI scanning is not safe for patients with some metal implants and foreign bodies. Careful attention to safety measures is necessary to avoid serious injury to patients and staff, and this requires special MRI compatible equipment and stringent adherence to safety protocols (see MRI safety).[9]
Common Abbreviations Used for MRI[edit | edit source]
T1 and T2 images demonstrate different tissues based on the timing of the RF pulses. Between the two, the key differences you need to be aware of are:
- T1 – ONE tissue is bright: fat
- T2 – TWO tissues are bright: fat and water (WW2 – Water is White in T2)
- T1 is the most ‘anatomical’ image (Figure 1). Conversely, the cerebrospinal fluid (CSF) is bright in T2 due to its’ water content.
- T2 is generally the more commonly used, but T1 can be used as a reference for anatomical structures or to distinguish between fat vs. water bright signals.
Additional features of T1/T2 weighted images
- Fat suppressed (FS): The fat signal can be suppressed to enable a better view of pathology in and around anatomical structures – particularly oedema. This is useful in adrenal tumours or bone marrow pathology, where the image will appear homogenous with surrounding tissue due to fat content.
- Gadolinium-enhanced (Gad): Gadolinium enhances vasculature (i.e. arteries) or pathologically-vascular tissues (e.g. intracranial metastases, meningiomas). This process involves injecting 5-15ml of contrast intravenously, with images taken shortly thereafter. Gadolinium appears bright in signal, allowing for detection of detailed abnormalities (e.g. intracranial pathologies).
Inversion recovery (IR) sequences
These types of images are manipulations of T1 and T2. They nullify certain tissue types based on their inversion timings, thereby stopping tissues such as fat and CSF from appearing as bright signals. This is helpful to identify pathological signals. The two main types are discussed below.
- Short tau inversion recovery (STIR): based on a T2 image, but the image is manipulated in a way that results in fat (and any other materials with similar signals) being nullified. Unlike fat-suppressed images, however, STIR can not be used with gadolinium contrast.4 As previously discussed, fat can make the interpretation of oedematous areas and bone marrow difficult.
- Fluid attenuated inversion recovery (FLAIR): similar to T2, however, the CSF signal is nullified. This is particularly useful for evaluating structures in the central nervous system (CNS), including the periventricular areas, sulci, and gyri. For example, FLAIR can be used to identify plaques in multiple sclerosis, subtle oedema after a stroke, and pathology in other conditions whereby CSF may interfere with interpretation[12]
Hybrid MRI Sequences occurs with manipulation to the type and frequency of radio frequency and cause echoes. A gradient echo adds sensitivity or iron-complexes such as articular cartilage defects and haemorrhaging in muscle, but conversely decreases resolution on metal hardware (such as pins or screws) from a surgery. Spin echo adds the benefit of increased tissue contrast and better visualisation of meniscal tears. Stimulated echo reduce interference of signal and therefore may be used to look at specific molecular movements within tissue.[5]
Proton density images
- An image simply of the density of protons
- A more dense area of protons will appear white (cortical bone, bone marrow)
- A less dense region will appear darker (fluids, soft tissues)
Contraindications for MRI[edit | edit source]
- Pacemakers, aneurysm clips, cochlear implants, and orbital foreign bodies
- Projectiles in the room (includes oxygen tanks, IV poles, stethoscopes, hair pins, etc)
Historical Note[edit | edit source]
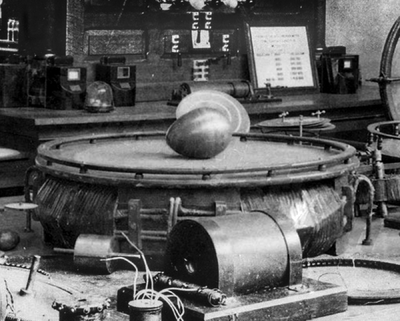
Nikola Tesla first discovered the rotating magnetic field, the phenomenon that made magnetic resonance imaging possible, in Budapest, Hungary in 1882. Seventy-four years later scientists commemorated his discovery by naming the Tesla Unit as the official measure of the strength of a magnetic field.[10]
Image: Nikola Tesla's "Egg of Columbus", a device used by the inventor to demonstrate the rotating magnetic field, that drove his new alternating current induction motor, by using that magnetic field to spin a copper egg on end.
Neurophysiology Fact[edit | edit source]
Charles Limb, a hearing specialist at Johns Hopkins and a faculty member of the Peabody Conservatory, wanted to know how some musicians are able to produce concert-length pieces of music that are entirely improvised, from beginning to end. So he had jazz pianists and rappers inside an MRI and let them perform. The resulting imaging showed that the most prolific improvisers somehow managed to shut off parts of their brains that handled self-monitoring, leading Limb to conclude what many musicians can probably intuit: don't worry if you make a mistake.[13]
Difference between MRI and CT[edit | edit source]
Like CT, MRI traditionally creates a two dimensional image of a thin "slice" of the body and is therefore considered a tomographic imaging technique. Modern MRI instruments are capable of producing images in the form of 3D blocks, which may be considered a generalisation of the single-slice, tomographic, concept. Unlike CT, MRI scans do not use X-rays so the possible concerns associated with X-ray pictures and CT scans (which use X-rays) are not associated with MRI scans.[14] For example, because MRI has only been in use since the early 1980s, there are no known long-term effects of exposure to strong static fields (this is the subject of some debate; see 'Safety' in MRI) and therefore there is no limit to the number of scans to which an individual can be subjected, in contrast with X-ray and CT. However, there are well-identified health risks associated with tissue heating from exposure to the RF field and the presence of implanted devices in the body, such as pacemakers. These risks are strictly controlled as part of the design of the instrument and the scanning protocols used.
Because CT and MRI are sensitive to different tissue properties, the appearance of the images obtained with the two techniques differs markedly. In CT, X-rays must be blocked by some form of dense tissue to create an image, so the image quality when looking at soft tissues will be poor. In MRI, while any nucleus with a net nuclear spin can be used, the proton of the hydrogen atom remains the most widely used, especially in the clinical setting, because it is so ubiquitous and returns a large signal. This nucleus, present in water molecules, allows the excellent soft-tissue contrast achievable.
Reference[edit | edit source]
- ↑ Radiopedia MRI Available from:https://radiopaedia.org/articles/mri-2?lang=gb (accessed 5.1.2021)
- ↑ McMahon KL, Cowin G, Galloway G. Magnetic resonance imaging: the underlying principles. The Journal of orthopaedic and sports physical therapy. 2011;41(11):806-19. Available at: http://www.ncbi.nlm.nih.gov/pubmed/21654095. Accessed March 16, 2012.
- ↑ Wikipedia,fckLRthe free encyclopedia http://en.wikipedia.org/wiki/Magnetic_resonance_imaging
- ↑ ACR–ASNR–SPR PRACTICE GUIDELINE FOR THE PERFORMANCE AND fckLRINTERPRETATION OF MAGNETIC RESONANCE IMAGING (MRI) OF THE fckLRBRAIN http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/MRI_Brain.pdf
- ↑ How stuff works fMRI Available from:https://science.howstuffworks.com/fmri.htm (accessed 5.1.2021)
- ↑ "ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 Appropriateness Criteria for Cardiac Computed Tomography and Cardiac Magnetic Resonance Imaging". Journal of the American College of Radiology 3 (10): 751–771. 2006.
- ↑ Radiopedia MR angiography Available from: https://radiopaedia.org/articles/mr-angiography-2?lang=gb(accessed 5.1.2021)
- ↑ Helms, C (2008). Musculoskeletal MRI. Saunders. ISBN 1416055347.
- ↑ 9.0 9.1 Giussani C, Roux FE, Ojemann J, Sganzerla EP, Pirillo D, Papagno C (2010). "Is preoperative functional magnetic resonance imaging reliable for language areas mapping in brain tumor surgery? Review of language functional magnetic resonance imaging and direct cortical stimulation correlation studies". Neurosurgery 66 (1): 113–20. doi:10.1227/01.NEU.0000360392.15450.C9. PMID 19935438.
- ↑ 10.0 10.1 10.2 Medical island Facts MRI Available from:https://www.medicalisland.net/medical-technology/five-fun-facts-about-mris (accessed 5.1.2021)
- ↑ Frydrychowicz A, Lubner MG, Brown JJ, Merkle EM, Nagle SK, Rofsky NM, Reeder SB (2012). "Hepatobiliary MR imaging with gadolinium-based contrast agents". J Magn Reson Imaging 35 (3): 492–511. doi:10.1002/jmri.22833. PMC 3281562. PMID 22334493.
- ↑ 12.0 12.1 Geekymedics MRI Available from: https://geekymedics.com/the-basics-of-mri-interpretation/ (accessed 5.1.2021)
- ↑ The Atlantic MRI Available from:https://www.theatlantic.com/health/archive/2012/04/6-cool-things-people-have-done-inside-mri-scanners/256416/ (accessed 5.1.2021)
- ↑ patient co uk trusted medical information and support http://www.patient.co.uk/health/mri-scan