Preeclampsia: Difference between revisions
No edit summary |
(Corrected text hyperlinks) |
||
| Line 5: | Line 5: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
Preeclampsia is one of the leading causes of maternal and perinatal morbidity and mortality, causing difficulties in 2-8% of all pregnancies worldwide. Left untreated, women with preeclampsia are at lasrge risk risk for [[Epilepsy|seizures]] (eclampsia), [[Pulmonary Oedema|pulmonary edema]], [[stroke]], [[Liver Disease|liver]] and [[Chronic Kidney Disease|kidney failure]], and death. <ref name=":1">Spracklen CN, Ryckman KK, Triche EW, Saftlas AF. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5538351/ Physical activity during pregnancy and subsequent risk of preeclampsia and gestational hypertension: a case control study. | Preeclampsia is one of the leading causes of maternal and perinatal morbidity and mortality, causing difficulties in 2-8% of all pregnancies worldwide. Left untreated, women with preeclampsia are at lasrge risk risk for [[Epilepsy|seizures]] (eclampsia), [[Pulmonary Oedema|pulmonary edema]], [[stroke]], [[Liver Disease|liver]] and [[Chronic Kidney Disease|kidney failure]], and death. <ref name=":1">Spracklen CN, Ryckman KK, Triche EW, Saftlas AF. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5538351/ Physical activity during pregnancy and subsequent risk of preeclampsia and gestational hypertension: a case control study]. Maternal and child health journal. 2016 Jun;20:1193-202.</ref> | ||
# Preeclampsia is a life-threatening [[Cardiovascular Disease|cardiovascular disorder]] associated with pregnancy. Preeclampsia is marked by [[hypertension]] and proteinuria at 20 weeks of gestation. The underlying cause is not precisely known but likely heterogenous. Ample research suggests that for some women with preeclampsia, both maternal and placental vascular impairment plays a role in its' evolution and may carry on into the postpartum period. | # Preeclampsia is a life-threatening [[Cardiovascular Disease|cardiovascular disorder]] associated with pregnancy. Preeclampsia is marked by [[hypertension]] and proteinuria at 20 weeks of gestation. The underlying cause is not precisely known but likely heterogenous. Ample research suggests that for some women with preeclampsia, both maternal and placental vascular impairment plays a role in its' evolution and may carry on into the postpartum period. | ||
# Preeclampsia is one of three conditions that constitute the syndrome of ischaemic placental disease, a group of pathologies that also includes placental abruption and intrauterine growth restriction.<ref>Parker SE, Werler MM, Gissler M, Tikkanen M, Ananth CV. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4400232/ Placental Abruption and Subsequent Risk of Pre‐eclampsia: A Population‐Based Case–Control Study. Paediatric and perinatal epidemiology. | # Preeclampsia is one of three conditions that constitute the syndrome of ischaemic placental disease, a group of pathologies that also includes placental abruption and intrauterine growth restriction.<ref>Parker SE, Werler MM, Gissler M, Tikkanen M, Ananth CV. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4400232/ Placental Abruption and Subsequent Risk of Pre‐eclampsia: A Population‐Based Case–Control Study]. Paediatric and perinatal epidemiology. 2015 May;29(3):211-9.</ref>.<ref>Opichka MA, Rappelt MW, Gutterman DD, Grobe JL, McIntosh JJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8616535/ Vascular dysfunction in preeclampsia]. Cells. 2021 Nov 6;10(11):3055.</ref> | ||
Note: [[Hypertension in Pregnancy|Hypertensive disorders of pregnancy]] are a leading cause of maternal and neonatal morbidity and mortality. Hypertension in pregnancy should be defined as a hospital systolic [[Blood Pressure|blood pressure]] (SBP) ⩾ 140 mmHg and/or diastolic blood pressure (DBP) ⩾ 90 mmHg, based on the average of at least two measurements, taken at least 15 min apart, using the same arm. To see Physiopedia's comprehensive page on Hypertensive disorders of pregnancy [[Hypertension in Pregnancy|see here]] | Note: [[Hypertension in Pregnancy|Hypertensive disorders of pregnancy]] are a leading cause of maternal and neonatal morbidity and mortality. Hypertension in pregnancy should be defined as a hospital systolic [[Blood Pressure|blood pressure]] (SBP) ⩾ 140 mmHg and/or diastolic blood pressure (DBP) ⩾ 90 mmHg, based on the average of at least two measurements, taken at least 15 min apart, using the same arm. To see Physiopedia's comprehensive page on Hypertensive disorders of pregnancy [[Hypertension in Pregnancy|see here]] | ||
| Line 15: | Line 15: | ||
Preeclampsia may happen at any time during the second half of pregnancy or the first few days after the birth. The signs of preeclampsia are high blood pressure, [[Proteins|protein]] in [[urine]] and sudden excessive swelling of the face, hands and feet. Sudden blurred vision is also a symptom. It is also possible to have preeclampsia without having any symptoms at all. | Preeclampsia may happen at any time during the second half of pregnancy or the first few days after the birth. The signs of preeclampsia are high blood pressure, [[Proteins|protein]] in [[urine]] and sudden excessive swelling of the face, hands and feet. Sudden blurred vision is also a symptom. It is also possible to have preeclampsia without having any symptoms at all. | ||
Women seen as high-risk individuals for developing preeclampsia should have administration of low-dose aspirin on a daily basis from early pregnancy as this is currently the most effective way to prevent preeclampsia. For preeclamptic females, specific information and counseling should be provided and appointments with a specialist made. In pregnancies complicated with preeclampsia, closer monitoring and antepartum surveillance ( eg.Doppler ultrasound blood flow study, biophysical profile, non-stress test, and oxytocin challenge test). Early intervention and aggressive therapy should be considered if tests indicate this action. <ref>Chang KJ, Seow KM, Chen KH. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9962022/ Preeclampsia: | Women seen as high-risk individuals for developing preeclampsia should have administration of low-dose aspirin on a daily basis from early pregnancy as this is currently the most effective way to prevent preeclampsia. For preeclamptic females, specific information and counseling should be provided and appointments with a specialist made. In pregnancies complicated with preeclampsia, closer monitoring and antepartum surveillance ( eg.Doppler ultrasound blood flow study, biophysical profile, non-stress test, and oxytocin challenge test). Early intervention and aggressive therapy should be considered if tests indicate this action. <ref>Chang KJ, Seow KM, Chen KH. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9962022/ Preeclampsia: recent advances in predicting, preventing, and managing the maternal and fetal life-threatening condition]. International journal of environmental research and public health. 2023 Feb 8;20(4):2994.</ref> | ||
[[File:Preeclampsia.jpg|center|frameless|538x538px]] | [[File:Preeclampsia.jpg|center|frameless|538x538px]] | ||
| Line 22: | Line 22: | ||
* An increased relative risk for the development of [[Chronic Kidney Disease|end-stage kidney disease]] (ESKD) in the mother. | * An increased relative risk for the development of [[Chronic Kidney Disease|end-stage kidney disease]] (ESKD) in the mother. | ||
* Research shows that women with a history of preeclampsia are 60% more likely to experience [[Stroke|ischemic strok]]<nowiki/>e and also have an increased risk of [[Hemorrhagic Stroke: Intracerebral Hemorrhage|hemorrhagic stroke]] and venous [[Thrombosis|thromboembolism]]<ref name=":0">Turbeville HR, Sasser JM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7311709/ Preeclampsia beyond pregnancy: long-term consequences for mother and child.] American Journal of Physiology-Renal Physiology. 2020 Jun 1;318(6):F1315-26. | * Research shows that women with a history of preeclampsia are 60% more likely to experience [[Stroke|ischemic strok]]<nowiki/>e and also have an increased risk of [[Hemorrhagic Stroke: Intracerebral Hemorrhage|hemorrhagic stroke]] and venous [[Thrombosis|thromboembolism]]<ref name=":0">Turbeville HR, Sasser JM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7311709/ Preeclampsia beyond pregnancy: long-term consequences for mother and child.] American Journal of Physiology-Renal Physiology. 2020 Jun 1;318(6):F1315-26.</ref>. | ||
* Women with a history of preeclampsia have increased an increased risk of [[Cerebral Small Vessel Disease|cerebral small vessel disease]] that is highly associated with stroke and [[dementia]]. <ref>Miller EC. [https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.118.11513 Preeclampsia and cerebrovascular disease: the maternal brain at risk]. Hypertension. 2019 Jul;74(1):5-13.Available:https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.118.11513 (accessed 5.3.2024)</ref> | * Women with a history of preeclampsia have increased an increased risk of [[Cerebral Small Vessel Disease|cerebral small vessel disease]] that is highly associated with stroke and [[dementia]]. <ref>Miller EC. [https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.118.11513 Preeclampsia and cerebrovascular disease: the maternal brain at risk]. Hypertension. 2019 Jul;74(1):5-13.Available:https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.118.11513 (accessed 5.3.2024)</ref> | ||
== Neonatal Consequences == | == Neonatal Consequences == | ||
The neonatal outcomes of preeclampsia identified are | The neonatal outcomes of preeclampsia identified are: | ||
* Preterm birth, stillbirth, low birth weight (LBW), low Apgar score, intrauterine growth reduction (IUGR), [[Neonatal Intensive Care Unit (NICU)|neonatal intensive care unit]] (NICU) admission.<ref>Atamamen TF, Naing NN, Oyetunji JA, Wan-Arfah N. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8977357/ Systematic literature review on the neonatal outcome of preeclampsia. | * Preterm birth, stillbirth, low birth weight (LBW), low Apgar score, intrauterine growth reduction (IUGR), [[Neonatal Intensive Care Unit (NICU)|neonatal intensive care unit]] (NICU) admission.<ref>Atamamen TF, Naing NN, Oyetunji JA, Wan-Arfah N. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8977357/ Systematic literature review on the neonatal outcome of preeclampsia]. Pan African Medical Journal. 2022 Jan 31;41(1).</ref> | ||
* Other differences include delayed [[Child Development|child physical development]] and sensorimotor reflex maturation( see [[Stages of Cognitive Development]]) , increased [[Body Mass Index|body mass index]], changes in [[Introduction to Neuroanatomy|neuroanatomy]] and reductions in cognitive function, and [[Hormones|hormonal]] changes.<ref name=":0" /> | * Other differences include delayed [[Child Development|child physical development]] and sensorimotor reflex maturation( see [[Stages of Cognitive Development]]) , increased [[Body Mass Index|body mass index]], changes in [[Introduction to Neuroanatomy|neuroanatomy]] and reductions in cognitive function, and [[Hormones|hormonal]] changes.<ref name=":0" /> | ||
Revision as of 11:52, 18 March 2024
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Ayodeji Mark-Adewunmi and Kirenga Bamurange Liliane
Introduction[edit | edit source]
Preeclampsia is one of the leading causes of maternal and perinatal morbidity and mortality, causing difficulties in 2-8% of all pregnancies worldwide. Left untreated, women with preeclampsia are at lasrge risk risk for seizures (eclampsia), pulmonary edema, stroke, liver and kidney failure, and death. [1]
- Preeclampsia is a life-threatening cardiovascular disorder associated with pregnancy. Preeclampsia is marked by hypertension and proteinuria at 20 weeks of gestation. The underlying cause is not precisely known but likely heterogenous. Ample research suggests that for some women with preeclampsia, both maternal and placental vascular impairment plays a role in its' evolution and may carry on into the postpartum period.
- Preeclampsia is one of three conditions that constitute the syndrome of ischaemic placental disease, a group of pathologies that also includes placental abruption and intrauterine growth restriction.[2].[3]
Note: Hypertensive disorders of pregnancy are a leading cause of maternal and neonatal morbidity and mortality. Hypertension in pregnancy should be defined as a hospital systolic blood pressure (SBP) ⩾ 140 mmHg and/or diastolic blood pressure (DBP) ⩾ 90 mmHg, based on the average of at least two measurements, taken at least 15 min apart, using the same arm. To see Physiopedia's comprehensive page on Hypertensive disorders of pregnancy see here
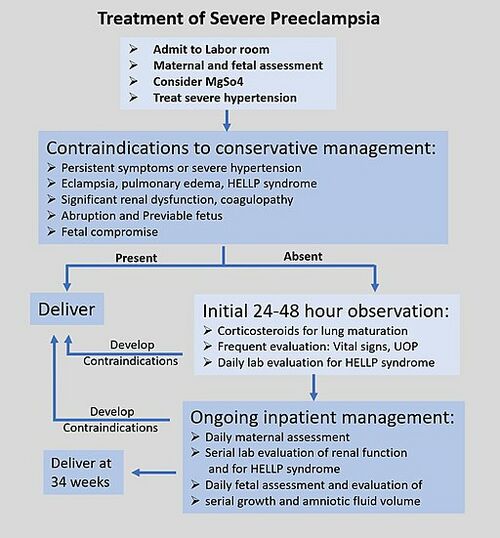
Treatment[edit | edit source]
Preeclampsia may happen at any time during the second half of pregnancy or the first few days after the birth. The signs of preeclampsia are high blood pressure, protein in urine and sudden excessive swelling of the face, hands and feet. Sudden blurred vision is also a symptom. It is also possible to have preeclampsia without having any symptoms at all.
Women seen as high-risk individuals for developing preeclampsia should have administration of low-dose aspirin on a daily basis from early pregnancy as this is currently the most effective way to prevent preeclampsia. For preeclamptic females, specific information and counseling should be provided and appointments with a specialist made. In pregnancies complicated with preeclampsia, closer monitoring and antepartum surveillance ( eg.Doppler ultrasound blood flow study, biophysical profile, non-stress test, and oxytocin challenge test). Early intervention and aggressive therapy should be considered if tests indicate this action. [4]
Maternal Consquences[edit | edit source]
Preeclampsia is associated with:
- An increased relative risk for the development of end-stage kidney disease (ESKD) in the mother.
- Research shows that women with a history of preeclampsia are 60% more likely to experience ischemic stroke and also have an increased risk of hemorrhagic stroke and venous thromboembolism[5].
- Women with a history of preeclampsia have increased an increased risk of cerebral small vessel disease that is highly associated with stroke and dementia. [6]
Neonatal Consequences[edit | edit source]
The neonatal outcomes of preeclampsia identified are:
- Preterm birth, stillbirth, low birth weight (LBW), low Apgar score, intrauterine growth reduction (IUGR), neonatal intensive care unit (NICU) admission.[7]
- Other differences include delayed child physical development and sensorimotor reflex maturation( see Stages of Cognitive Development) , increased body mass index, changes in neuroanatomy and reductions in cognitive function, and hormonal changes.[5]
Physiotherapy[edit | edit source]
Women with higher levels of physical activity(PA) during pregnancy seem to have a lower risk of preeclampsia, conversely women with increased levels of sedentary activity were at increased risk. Promotion of PA during pregnancy may be a promising approach for reducing the risk of the disease. However, additional research is needed to confirm the protective effect of PA on preeclampsia risk.[1]
In 2012 the American College of Obstetricians and Gynecologists does not recommend exercise therapy during pregnancy for women at risk of certain gestational complications, such as gestational hypertension and preeclampsia. Research suggests that exercise therapy has deleterious effects on uteroplacental perfusion in at-risk pregnancies. Although several studies observed a beneficial effect of exercise therapy on preeclampsia risk, they were not randomized studies and the mechanisms involved in these effects are unknown.[8]
References[edit | edit source]
- ↑ 1.0 1.1 Spracklen CN, Ryckman KK, Triche EW, Saftlas AF. Physical activity during pregnancy and subsequent risk of preeclampsia and gestational hypertension: a case control study. Maternal and child health journal. 2016 Jun;20:1193-202.
- ↑ Parker SE, Werler MM, Gissler M, Tikkanen M, Ananth CV. Placental Abruption and Subsequent Risk of Pre‐eclampsia: A Population‐Based Case–Control Study. Paediatric and perinatal epidemiology. 2015 May;29(3):211-9.
- ↑ Opichka MA, Rappelt MW, Gutterman DD, Grobe JL, McIntosh JJ. Vascular dysfunction in preeclampsia. Cells. 2021 Nov 6;10(11):3055.
- ↑ Chang KJ, Seow KM, Chen KH. Preeclampsia: recent advances in predicting, preventing, and managing the maternal and fetal life-threatening condition. International journal of environmental research and public health. 2023 Feb 8;20(4):2994.
- ↑ 5.0 5.1 Turbeville HR, Sasser JM. Preeclampsia beyond pregnancy: long-term consequences for mother and child. American Journal of Physiology-Renal Physiology. 2020 Jun 1;318(6):F1315-26.
- ↑ Miller EC. Preeclampsia and cerebrovascular disease: the maternal brain at risk. Hypertension. 2019 Jul;74(1):5-13.Available:https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.118.11513 (accessed 5.3.2024)
- ↑ Atamamen TF, Naing NN, Oyetunji JA, Wan-Arfah N. Systematic literature review on the neonatal outcome of preeclampsia. Pan African Medical Journal. 2022 Jan 31;41(1).
- ↑ Genest DS, Falcao S, Gutkowska J, Lavoie JL. Impact of exercise training on preeclampsia: potential preventive mechanisms. Hypertension. 2012 Nov;60(5):1104-9.Available:https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.112.194050 (accessed 6.3.2024)