Mental Health Issues and Rehabilitation: Difference between revisions
mNo edit summary |
Rucha Gadgil (talk | contribs) No edit summary |
||
| (14 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> '''Original Editor '''- [[User:Khloud Shreif|Khloud Shreif]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
'''Original Editor '''- [[User:Khloud Shreif|Khloud Shreif]] | |||
== Introduction == | == Introduction == | ||
A person who experiences an injury or trauma, usually have psychological and emotional response to this injury and mental health issues such [[depression]], [https://www.physio-pedia.com/Generalized_Anxiety_Disorder?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal anxiety] and [[Stress and Health|stress]] may appear. | |||
[[Anorexia Nervosa]] may be triggered as well due to the fear of gaining weight. There is evidence supporting that mental health issues may inhibit outcomes of rehabilitation process<ref>Bruijning JE, van Rens GH, Fick M, Knol DL, van Nispen RM. Longitudinal observation, evaluation and interpretation of coping with mental (emotional) health in low vision rehabilitation using the Dutch ICF Activity Inventory. Health and quality of life outcomes. 2014 Dec;12(1):1-6.</ref>. Depression is a common psychological problem that decreases life satisfaction and quality of life, especially in people with [[Introduction to Spinal Cord Injury|spinal cord injury] (SCI)]] . In a systematic review done by Craig et al.<ref>Craig A, Tran Y, Middleton J. Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord. 2009;47(2):108–14. 10.1038/sc.2008.115</ref> revealed that SCI patients in the rehabilitation phase still have a risk of [[depression]] and that almost 30% of those may develop a risk of [[depression]]. In addition, the potential depressive risk may be approximately 27% when [[Spinal Cord Injury|SCI]] patients return to their normal life. So good or sound patients' mental health is pre requisite for better rehabilitation outcomes or results. There is also an increased risk of suicide among people with [[Spinal Cord Injury|SCI]] compared to the general population, attributable to both pre- and post-[[Spinal Cord Injury|SCI]] factors (e.g., psychiatric history prior to SCI, increased duress following SCI, and associated changes in functioning), with estimates of 4–11% of deaths following [[Spinal Cord Injury|SCI]] attributable to suicide<ref>Kennedy P, Garmon-Jones L. [https://www.nature.com/articles/sc2016135 Self-harm and suicide before and after spinal cord injury: a systematic review.] Spinal Cord. 2017 Jan;55(1):2-7. </ref><ref>Khazem LR. [https://www.sciencedirect.com/science/article/abs/pii/S2352250X17301914 Physical disability and suicide: recent advancements in understanding and future directions for consideration]. Curr Opin Psychol. 2018;22:18–22. </ref>. | |||
== Possible psychosocial responses/reactions == | == Possible psychosocial responses/reactions == | ||
The effect of injury on mental health and psychological response isn’t predictable it extends from the time immediately after injury, to the post-injury phase, rehabilitation phase and finally with return to activity. These emotional reactions and mental responses to injury are normal. But if the symptoms are unresolved or worsen over time it becomes a problem<ref> | The effect of injury on mental health and psychological response isn’t predictable it extends from the time immediately after injury, to the post-injury phase, rehabilitation phase and finally with return to activity. These emotional reactions and mental responses to injury are normal. But if the symptoms are unresolved or worsen over time it becomes a problem<ref>[https://journals.lww.com/acsm-msse/Fulltext/2006/11000/Psychological_Issues_Related_to_Injury_in_Athletes.20.aspx Psychological issues related to injury in athletes and the team physician: a consensus statement]. Med Sci Sports Exerc. 2006 Nov;38(11):2030-4.</ref>. | ||
The psychological and social reaction following spinal cord injury in an individual may include the following: | The psychological and social reaction following [[Spinal Cord Injury|spinal cord injury]] in an individual may include the following: | ||
[[File:Mental health thumbnail.jpg|thumb]] | |||
* [[Depression]] | * [[Depression]] | ||
| Line 32: | Line 32: | ||
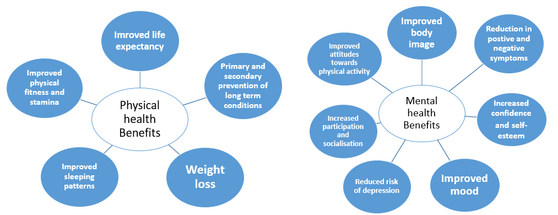
== Intervention for these mental health issues == | == Intervention for these mental health issues == | ||
[[File:Mental health matters.jpeg|thumb]] | |||
* | * Explain to the patient about the injury and the recovery process, the demonstration should be introduced in a way the patient can understand well, in a clear way and if any misinformation try to explain to your best and correct it. You could also provide proofs regarding what are you saying, for example, articles from trusted organisations. | ||
* Build trust and good rapport with individual | * Build trust and good rapport with individual patients, listen carefully to your patient before making a medical diagnosis and also assess and monitor their emotional state. You may experience a range of emotions that make it difficult for care network members to establish a connection. If this happens you could show empathy, actively listen to your patients, not rush them, take as time as needed to listen to them, try to understand them, even if this is not what you feel or think, you do not have to feel or think the same, you just have to let them know you listen and understand them. | ||
* Set goals, help patient to be motivated, to complete their rehabilitation by setting achievable short and long term goals. | * Set goals, help patient to be motivated, to complete their rehabilitation by setting achievable short and long term goals. | ||
* Create a | * Create a network of support between your patient , family members, and friends. | ||
It is important for the [[Rehabilitation Team Members|rehabilitation team members]] to take care of depression symptoms and emotional difficulties as well during the rehabilitation sessions. | |||
It is important for the [[Rehabilitation Team Members|rehabilitation team members]] to take care of depression symptoms and emotional difficulties as | [[File:Physical and mental health benefits.png|center|thumb|558x558px]] | ||
== Clinical implications == | == Clinical implications == | ||
[[File:Stroke 2.jpg|thumb]] | [[File:Stroke 2.jpg|thumb]] | ||
'''[[Stroke]] patients''': depression in stroke | A study demonstrated that functional recovery is associated with psychosocial factors such as motivation during acute hospitalizations. Also, there were associations found between functional recovery and depression during this same period. This suggests that psychosocial factors can affect physical therapy and rehabilitation outcomes. It has been seen that psychosocial factors are involved in the management of patients with spinal cord injury, thus the physical therapist should be aware of these factors and act accordingly when they are encountered in the management of such persons<ref>Psychosocial Guidelines in Spinal Cord Injury Rehabilitation. Jagadamba Press; 2015. Available from: https://ascon.info/wp-content/uploads/2018/05/psychosocial-guidelines15.pdf [Accessed 10 December, 2020]</ref>. | ||
'''[[Stroke]] patients''': depression in stroke patients may consider to be a biological process that correlates with the size and location of the area affected on [[Brain Anatomy|brain]]. It is called post-stroke depression and may slow the recovery rate, hinder patient outcomes, negatively affect lower functional status and stroke survivors’ quality of life, and secondary complications. Post-stroke depression is believed to be caused by changes in brain chemistry and the disruption of neural pathways.<ref>Wijeratne T, Sales C. Understanding why post-stroke depression may be the norm rather than the exception: The anatomical and neuroinflammatory correlates of post-stroke depression. Journal of Clinical Medicine. 2021 Apr 14;10(8):1674.</ref> These changes in brain chemistry and neural pathways can result from the physical damage caused by the stroke itself. Additionally, post-stroke depression can also be influenced by psychological factors such as the emotional impact of experiencing a life-altering event like a stroke. | |||
Depression is believed to be more common in stroke patients with aphasia than those without, and when it was treated medically the studies show a decrease in the mortality rate<ref>Jeong YJ, Kim WC, Kim YS, Choi KW, Son SY, Jeong YG. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4155231/ The relationship between rehabilitation and changes in depression in stroke patients]. Journal of physical therapy science. 2014;26(8):1263-6.</ref><ref>Kincheloe HB. [https://scholarworks.umt.edu/cgi/viewcontent.cgi?article=1277&context=utpp The Impact of Depression on Treatment Outcomes for Patients with Aphasia who Participate in an Intensive Comprehensive Aphasia Program] (ICAP).2018</ref>. Healthcare professionals need to identify and address this condition early on, as it can significantly impact the overall rehabilitation process and the patient's ability to regain independence.<ref>Ezema CI, Akusoba PC, Nweke MC, Uchewoke CU, Agono J, Usoro G. Influence of post-stroke depression on functional independence in activities of daily living. Ethiopian journal of health sciences. 2019;29(1). | |||
</ref> As our overall goal of rehabilitation is to optimize quality of life by improving one’s adaptation to a disability and coping with functional improvement, the physician will sometimes need to deal with depression before dealing with physical rehab. Depression can hinder the progress of physical rehabilitation, as it can lead to decreased motivation and participation in therapy. Therefore, addressing depression can be crucial in achieving successful rehabilitation outcomes. | |||
'''[[Athletes with difficult or longstanding neuromusculoskeletal symptoms|Athletic injury]]''' '''rehab''': the rehab process may be affected by psychological responses such as loss of identity, fear, anxiety, loss of confidence, denial of injury, rapid mood swing, and unreasonable fear of re-injury. Though | '''[[Athletes with difficult or longstanding neuromusculoskeletal symptoms|Athletic injury]]''' '''rehab''': the rehab process may be affected by psychological responses such as loss of identity, fear, anxiety, loss of confidence, denial of injury, rapid mood swing, and unreasonable fear of re-injury. Though goal setting, cognitive structures, maintaining patient motivation and psychological support are helpful strategies for faster recovery and coping with the process of rehabilitation and social strategy. | ||
'''In [[Critical Care Assessment|critical care]]'''[[Critical Care Assessment|:]] after discharge from critical care younger and older patients showed significant incidence of long-term cognitive and psychological dysfunction that impact on long-term function and quality of life<ref>Clancy O, Edginton T, Casarin A, Vizcaychipi MP. | '''In [[Critical Care Assessment|critical care]]'''[[Critical Care Assessment|:]] after discharge from critical care younger and older patients showed significant incidence of long-term cognitive and psychological dysfunction that impact on long-term function and quality of life<ref>Clancy O, Edginton T, Casarin A, Vizcaychipi MP. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5606436/. The psychological and neurocognitive consequences of critical illness]. A pragmatic review of current evidence. Journal of the Intensive Care Society. 2015 Aug;16(3):226-33.</ref>. These findings highlight the importance of follow-up care and rehabilitation programs for patients after discharge from critical care, especially for older patients who may be more vulnerable to cognitive decline. Healthcare providers should also consider implementing strategies to prevent or mitigate these long-term effects. | ||
== References == | == References == | ||
Latest revision as of 17:07, 4 July 2023
Introduction[edit | edit source]
A person who experiences an injury or trauma, usually have psychological and emotional response to this injury and mental health issues such depression, anxiety and stress may appear.
Anorexia Nervosa may be triggered as well due to the fear of gaining weight. There is evidence supporting that mental health issues may inhibit outcomes of rehabilitation process[1]. Depression is a common psychological problem that decreases life satisfaction and quality of life, especially in people with spinal cord injury] (SCI) . In a systematic review done by Craig et al.[2] revealed that SCI patients in the rehabilitation phase still have a risk of depression and that almost 30% of those may develop a risk of depression. In addition, the potential depressive risk may be approximately 27% when SCI patients return to their normal life. So good or sound patients' mental health is pre requisite for better rehabilitation outcomes or results. There is also an increased risk of suicide among people with SCI compared to the general population, attributable to both pre- and post-SCI factors (e.g., psychiatric history prior to SCI, increased duress following SCI, and associated changes in functioning), with estimates of 4–11% of deaths following SCI attributable to suicide[3][4].
Possible psychosocial responses/reactions[edit | edit source]
The effect of injury on mental health and psychological response isn’t predictable it extends from the time immediately after injury, to the post-injury phase, rehabilitation phase and finally with return to activity. These emotional reactions and mental responses to injury are normal. But if the symptoms are unresolved or worsen over time it becomes a problem[5].
The psychological and social reaction following spinal cord injury in an individual may include the following:
- Depression
- Post-traumatic stress disorder
- Suicidal thinking or lack of desire to live
- Apathy and not caring about life
- Inability to provide self-care and follow medical advice
- Marital and relationship conflict
- Lack of motivation for vocational or educational pursuits
- Feeling trapped in the family surroundings
- Unnecessary dependency on others
- Social Isolation
- Negative body image or shame
- Feelings of worthlessness
- Low self-esteem
- Anger and aggression
- Shame and embarrassment
- Feelings of helplessness and hopelessness
- High levels of stress
- Self-Blame
Intervention for these mental health issues[edit | edit source]
- Explain to the patient about the injury and the recovery process, the demonstration should be introduced in a way the patient can understand well, in a clear way and if any misinformation try to explain to your best and correct it. You could also provide proofs regarding what are you saying, for example, articles from trusted organisations.
- Build trust and good rapport with individual patients, listen carefully to your patient before making a medical diagnosis and also assess and monitor their emotional state. You may experience a range of emotions that make it difficult for care network members to establish a connection. If this happens you could show empathy, actively listen to your patients, not rush them, take as time as needed to listen to them, try to understand them, even if this is not what you feel or think, you do not have to feel or think the same, you just have to let them know you listen and understand them.
- Set goals, help patient to be motivated, to complete their rehabilitation by setting achievable short and long term goals.
- Create a network of support between your patient , family members, and friends.
It is important for the rehabilitation team members to take care of depression symptoms and emotional difficulties as well during the rehabilitation sessions.
Clinical implications[edit | edit source]
A study demonstrated that functional recovery is associated with psychosocial factors such as motivation during acute hospitalizations. Also, there were associations found between functional recovery and depression during this same period. This suggests that psychosocial factors can affect physical therapy and rehabilitation outcomes. It has been seen that psychosocial factors are involved in the management of patients with spinal cord injury, thus the physical therapist should be aware of these factors and act accordingly when they are encountered in the management of such persons[6].
Stroke patients: depression in stroke patients may consider to be a biological process that correlates with the size and location of the area affected on brain. It is called post-stroke depression and may slow the recovery rate, hinder patient outcomes, negatively affect lower functional status and stroke survivors’ quality of life, and secondary complications. Post-stroke depression is believed to be caused by changes in brain chemistry and the disruption of neural pathways.[7] These changes in brain chemistry and neural pathways can result from the physical damage caused by the stroke itself. Additionally, post-stroke depression can also be influenced by psychological factors such as the emotional impact of experiencing a life-altering event like a stroke.
Depression is believed to be more common in stroke patients with aphasia than those without, and when it was treated medically the studies show a decrease in the mortality rate[8][9]. Healthcare professionals need to identify and address this condition early on, as it can significantly impact the overall rehabilitation process and the patient's ability to regain independence.[10] As our overall goal of rehabilitation is to optimize quality of life by improving one’s adaptation to a disability and coping with functional improvement, the physician will sometimes need to deal with depression before dealing with physical rehab. Depression can hinder the progress of physical rehabilitation, as it can lead to decreased motivation and participation in therapy. Therefore, addressing depression can be crucial in achieving successful rehabilitation outcomes.
Athletic injury rehab: the rehab process may be affected by psychological responses such as loss of identity, fear, anxiety, loss of confidence, denial of injury, rapid mood swing, and unreasonable fear of re-injury. Though goal setting, cognitive structures, maintaining patient motivation and psychological support are helpful strategies for faster recovery and coping with the process of rehabilitation and social strategy.
In critical care: after discharge from critical care younger and older patients showed significant incidence of long-term cognitive and psychological dysfunction that impact on long-term function and quality of life[11]. These findings highlight the importance of follow-up care and rehabilitation programs for patients after discharge from critical care, especially for older patients who may be more vulnerable to cognitive decline. Healthcare providers should also consider implementing strategies to prevent or mitigate these long-term effects.
References[edit | edit source]
- ↑ Bruijning JE, van Rens GH, Fick M, Knol DL, van Nispen RM. Longitudinal observation, evaluation and interpretation of coping with mental (emotional) health in low vision rehabilitation using the Dutch ICF Activity Inventory. Health and quality of life outcomes. 2014 Dec;12(1):1-6.
- ↑ Craig A, Tran Y, Middleton J. Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord. 2009;47(2):108–14. 10.1038/sc.2008.115
- ↑ Kennedy P, Garmon-Jones L. Self-harm and suicide before and after spinal cord injury: a systematic review. Spinal Cord. 2017 Jan;55(1):2-7.
- ↑ Khazem LR. Physical disability and suicide: recent advancements in understanding and future directions for consideration. Curr Opin Psychol. 2018;22:18–22.
- ↑ Psychological issues related to injury in athletes and the team physician: a consensus statement. Med Sci Sports Exerc. 2006 Nov;38(11):2030-4.
- ↑ Psychosocial Guidelines in Spinal Cord Injury Rehabilitation. Jagadamba Press; 2015. Available from: https://ascon.info/wp-content/uploads/2018/05/psychosocial-guidelines15.pdf [Accessed 10 December, 2020]
- ↑ Wijeratne T, Sales C. Understanding why post-stroke depression may be the norm rather than the exception: The anatomical and neuroinflammatory correlates of post-stroke depression. Journal of Clinical Medicine. 2021 Apr 14;10(8):1674.
- ↑ Jeong YJ, Kim WC, Kim YS, Choi KW, Son SY, Jeong YG. The relationship between rehabilitation and changes in depression in stroke patients. Journal of physical therapy science. 2014;26(8):1263-6.
- ↑ Kincheloe HB. The Impact of Depression on Treatment Outcomes for Patients with Aphasia who Participate in an Intensive Comprehensive Aphasia Program (ICAP).2018
- ↑ Ezema CI, Akusoba PC, Nweke MC, Uchewoke CU, Agono J, Usoro G. Influence of post-stroke depression on functional independence in activities of daily living. Ethiopian journal of health sciences. 2019;29(1).
- ↑ Clancy O, Edginton T, Casarin A, Vizcaychipi MP. The psychological and neurocognitive consequences of critical illness. A pragmatic review of current evidence. Journal of the Intensive Care Society. 2015 Aug;16(3):226-33.