Juvenile Idiopathic Arthritis
Original Editors - Emily Betz from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Emily Betz, Lucinda hampton, Jess Bell, Ines Musabyemariya, Admin, Naomi O'Reilly, Khloud Shreif, Kim Jackson, Elaine Lonnemann, Mande Jooste, Wendy Walker, George Prudden, WikiSysop and Meaghan Rieke
Introduction[edit | edit source]
Juvenile idiopathic arthritis (JIA) is a term used to describe types of arthritis of unknown cause, where symptoms last for more than 6 weeks, in individuals aged under 16 years at the time of onset.[1]
JIA ranges in severity. It affects the joints, as well as other structures such as the eyes, skin, and organs,[2] and it can be divided into the following subtypes:[2]
- oligoarticular
- polyarticular
- systemic
- psoriatic
- enthesitis-related
- undifferentiated
Aetiology[edit | edit source]
The aetiology of JIA is unclear.[3] The following factors have been proposed:[2]
- genetic associations
- autoimmune factors[4]
- environmental factors (e.g. infectious agents, antibiotics, stress etc) may be risk factors
- infectious viruses and bacteria may be causal factors
Epidemiology[edit | edit source]
JIA is the most common chronic heterogenous rheumatologic condition in children.[3][4] It is estimated that around 3 million children and young adults have JIA. The global prevalence is believed to range from 3.8 to 400/100,000; the incidence is estimated to be 1.6 to 23/100,000.[4]
Characteristics and Clinical Presentation[edit | edit source]
Symptoms of JIA vary depending on the type of arthritis.[6] It has an unpredictable course - it can be self-limiting or cause joint damage. But there is a general pattern of inflammatory joint disease in one or more joints:[3][6]
- synovitis
- joint effusion
- swelling of soft tissues
- osteopenia
- bone oedema, erosions
Certain features of JIA will depend on the age of the child affected (e.g. the involvement of epiphyseal growth plates, early physeal fusion or the development of discrepancies in limb length).[3]
Individuals may also experience:[6][7]
- pain
- fatigue
- fever
- rash
- generally feeling unwell (malaise)
- uveitis (see image)
- decreased range of motion
Diagnostic Tests[edit | edit source]
There is no specific test to diagnose JIA,[3] but the following may be included:[3][6]
- medical history
- physical examination
- laboratory tests - typical inflammatory markers are said to be common, particularly in oligoarthritis[3]
- imaging
- radiography for symptomatic joints (in early JIA, there are no detectable changes on x-ray, but indirect signs may be present, increased soft tissue density etc[3])
- ultrasound
- MRI (the gold standard)
- eye examination
Pathology[edit | edit source]
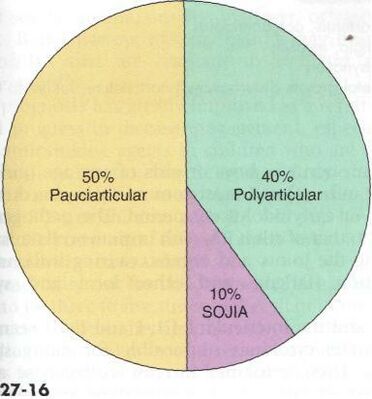
There are several subtypes of JIA:[3][6][9]
- Oligoarticular JIA (also known as pauciarticular)
- affects four or fewer joints in the first six months of disease
- peak age for oligoarticular JIA is 1-6 years
- more common in females
- tends to impact medium and large joints
- risk of uveitis
- Polyarticular JIA
- affects more than 5 joints
- peak ages for polyarticular JIA are 1-4 years and 7-10 years
- more common in females
- tends to impact small and medium joints
- Systemic onset JIA
- Psoriatic JIA
- causes psoriasis and inflammatory arthritis (can develop at different times)
- more common in females
- occurs in preschool-aged children and at around 10 years
- tends to impact fingers, wrists, toes, but not exclusively
- Enthesitis-related JIA
- inflammation of entheses
- more common in males
- tends to occur in older children / adolescents
- association with acute uveitis
- Undifferentiated JIA
- JIA that does not fit into another category
Management[edit | edit source]
Treatment for JIA includes pharmacology, physiotherapy, potentially surgery, and in some cases nutritional and psychosocial support.[3]
Pharmacology[edit | edit source]
The choice of medication depends on type and severity of JIA and if there are other conditions. Common medications include analgesics, eye drops, non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, disease modifying anti-rheumatic medications, biologics and biosimilar medicines.[3][6]
Physiotherapy Management[edit | edit source]
Physical therapy is an important part of the treatment of JIA. It is important for the child to remain active and involved in sports and activities with their peers and friends. While pain may limit the amount of activity a child can handle it is important to encourage involvement during periods or remission and allow rest and symptom reducing therapies during periods of flare-ups. Regular activity and general exercise programs help to maintain range of motion in affective joints, build and maintain strength, maintain function and can even help with symptom reduction.
Aspects that should be focused on during a physical therapy session are as follows[11]:
- Muscle tone
- Strengthening
- Range of motion
- Stretching
- Education on joint protection
- Home exercise plan
- Education on pain reducing techniques
- Muscle relaxation techniques
- Splints or Introduction to Orthotics maybe be beneficial to help maintain normal bone and joint growth/prevent deformities during growth[12]
Some modalities that can be used to help reduce symptoms such as pain are:
- Ultrasound
- Paraffin wax dips (hands and feet primarily)
- Moist compress (hot pack)
- Hydrotherapy (warm)
- Cold packs
Differential Diagnosis[edit | edit source]
Some signs and symptoms of JIA are shared with those of the following diseases[11][13]:
- Lyme Disease
- Rheumatic fever
- Osteomyelitis
- Psoriatic arthritis
- Inflammatory bowel disease
- Leukemia
- Caffey Disease
- Chronic Eosinophilic Granuloma
- Osteoporosis
- Involutional Osteoarthritis
References[edit | edit source]
- ↑ Rigante D, Bosco A, Esposito S. The Etiology of Juvenile Idiopathic Arthritis. Clin Rev Allergy Immunol. 2015 Oct;49(2):253-61.
- ↑ 2.0 2.1 2.2 2.3 Zaripova LN, Midgley A, Christmas SE, Beresford MW, Baildam EM, Oldershaw RA. Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches. Pediatr Rheumatol Online J. 2021 Aug 23;19(1):135.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 Thatayatikom A, Modica R, De Leucio A. Juvenile Idiopathic Arthritis. [Updated 2023 Jan 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554605/
- ↑ 4.0 4.1 4.2 4.3 4.4 Al-Mayouf SM, Al Mutairi M, Bouayed K, Habjoka S, Hadef D, Lotfy HM, Scott C, Sharif EM, Tahoun N. Epidemiology and demographics of juvenile idiopathic arthritis in Africa and Middle East. Pediatr Rheumatol Online J. 2021 Dec 2;19(1):166.
- ↑ França CMP, Sallum AM, Silva CAA, Aikawa NE, Braga AL, Farhat SC. Risk factors for juvenile idiopathic arthritis: exposure to tobacco and environmental factors during and before pregnancy. Pediatr Rheumatol Online J. 2014 Sep 17;12(Suppl 1):P27.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 better Health Juvenile Arthritis Available: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile(accessed 18.10.2021)
- ↑ National Institute of Arthritis and Musculoskeletal and Skin Diseases. Juvenile Idiopathic Arthritis (JIA) Basics. Available from: https://www.niams.nih.gov/health-topics/juvenile-arthritis/basics/symptoms-causes (last accessed 1 May 2023).
- ↑ Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. 3rd ed. . St. Louis, MO: Saunders, an imprint of Elsevier Inc, 2009.
- ↑ 9.0 9.1 Radiopedia JIA Available: https://radiopaedia.org/articles/juvenile-idiopathic-arthritis (accessed 18.10.2021)
- ↑ Hedrich CM, Günther C, Aringer M. Morbus Still im Kindes- und Erwachsenenalter [Still's disease in children and adults]. Z Rheumatol. 2017 Sep;76(7):595-608. German.
- ↑ 11.0 11.1 eMedicine. Disease fact sheet: juvenile rheumatoid arthritis. http://emedicine.medscape.com/article/409980-overview (accessed 10 March 2011)
- ↑ National Institute of Arthritis and Musculoskeletal and Skin Diseases. Health information: juvenile arthritis. http://www.niams.nih.gov/Health_Info/Juv_Arthritis/default.asp (accessed 10 March 2011)
- ↑ National Center for Biotechnology Information, U.S. National Library of Medicine. Disease fact sheet: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001487/ (10 March 2011)






