Juvenile Idiopathic Arthritis: Difference between revisions
No edit summary |
mNo edit summary |
||
| (31 intermediate revisions by 6 users not shown) | |||
| Line 3: | Line 3: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
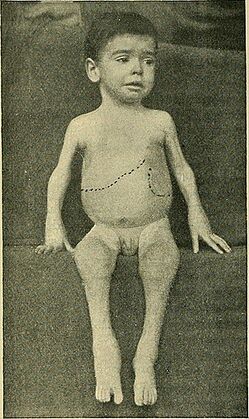
[[File: | [[File:Juvenile arthritis.jpg|alt=|thumb|419x419px|'''Figure.1''' Swollen joints in Patient with JIA]] | ||
''' | Juvenile idiopathic arthritis (JIA) is a term used to describe types of arthritis of unknown cause, where symptoms last for more than 6 weeks, in individuals aged under 16 years at the time of onset.<ref>Rigante D, Bosco A, Esposito S. The Etiology of Juvenile Idiopathic Arthritis. Clin Rev Allergy Immunol. 2015 Oct;49(2):253-61.</ref> | ||
Juvenile idiopathic arthritis (JIA) | |||
JIA | JIA ranges in severity. It affects the joints, as well as other structures such as the eyes, skin, and organs,<ref name=":3" /> and it can be divided into the following subtypes:<ref name=":3">Zaripova LN, Midgley A, Christmas SE, Beresford MW, Baildam EM, Oldershaw RA. [https://ped-rheum.biomedcentral.com/articles/10.1186/s12969-021-00629-8 Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches]. Pediatr Rheumatol Online J. 2021 Aug 23;19(1):135. </ref> | ||
* Oligoarticular | |||
* Polyarticular | |||
* Systemic | |||
* Psoriatic | |||
* Enthesitis-related | |||
* Undifferentiated | |||
== Aetiology == | |||
The aetiology of JIA is unclear.<ref name=":1">Thatayatikom A, Modica R, De Leucio A. [https://www.ncbi.nlm.nih.gov/books/NBK554605/ Juvenile Idiopathic Arthritis]. [Updated 2023 Jan 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan.</ref> A range of factors have been proposed, including:<ref name=":3" /> | |||
* Genetic associations, genetic factors classified into: HLA genes and non-HLA-related genes. | |||
** HLA class II molecules (A2, DRB1, DPB1) are associated with certain non-systemic JIA types, while systemic JIA is not linked to HLA genes. | |||
* Autoimmune factors<ref name=":4">Al-Mayouf SM, Al Mutairi M, Bouayed K, Habjoka S, Hadef D, Lotfy HM, Scott C, Sharif EM, Tahoun N. [https://ped-rheum.biomedcentral.com/articles/10.1186/s12969-021-00650-x Epidemiology and demographics of juvenile idiopathic arthritis in Africa and Middle East]. Pediatr Rheumatol Online J. 2021 Dec 2;19(1):166. </ref> | |||
* Environmental factors (e.g. infectious agents, antibiotics, stress etc.) may be risk factors | |||
** maternal factors (e.g. smoking<ref name=":3" /><ref>França CMP, Sallum AM, Silva CAA, Aikawa NE, Braga AL, Farhat SC. [https://www.jrheum.org/content/45/2/248 Risk factors for juvenile idiopathic arthritis: exposure to tobacco and environmental factors during and before pregnancy]. Pediatr Rheumatol Online J. 2014 Sep 17;12(Suppl 1):P27. </ref>) may be involved, but breastfeeding / having household siblings may reduce risk. | |||
* Infectious viruses (e.g., Epstein-Barr virus, Parvovirus B), bacteria (e.g., Salmonella spp., Shigella spp.) have been linked to the development of JIA, in addition, vaccinations, antibiotics, vitamin D deficiency, stress, and trauma may be causal factors. | |||
* Gastrointestinal infections that result in reduced diversity in the gut microbiome and disturbances in tryptophan metabolism can elevate the susceptibility to developing enthesitis-related arthritis (ERA). | |||
== Epidemiology == | == Epidemiology == | ||
JIA is the most common | JIA is the most common chronic heterogenous rheumatologic condition in children.<ref name=":1" /><ref name=":4" /> It is estimated that around 3 million children and young adults have JIA. The global prevalence is believed to range from 3.8 to 400/100,000; the incidence is estimated to be 1.6 to 23/100,000.<ref name=":4" /> | ||
* | * Females are at higher risk of JIA than males<ref name=":4" /> | ||
* The oligoarticular subtype is more common<ref name=":4" /> | |||
* The | |||
== | == Characteristics and Clinical Presentation == | ||
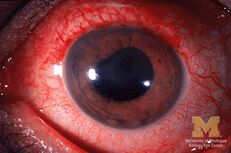
[[ | [[File:Anterior-uveitis.jpg|thumb|231x231px|Anterior-uveitis]] | ||
Symptoms of JIA vary depending on the type of arthritis.<ref name=":2">better Health [https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile Juvenile Arthritis] Available: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile<nowiki/>(accessed 18.10.2021)</ref> It has an unpredictable course - it can be self-limiting or cause joint damage. But there is a general pattern of inflammatory joint disease in one or more joints:<ref name=":1" /><ref name=":2" /> | |||
* Synovitis | |||
* Joint effusion | |||
* Swelling of soft tissues | |||
* Osteopenia | |||
* Bone oedema, erosions | |||
Certain features of JIA will depend on the age of the child affected (e.g. involvement of epiphyseal growth plates, early physeal fusion or the development of discrepancies in limb length).<ref name=":1" /> | |||
2. | Individuals may also experience:<ref name=":2" /><ref>National Institute of Arthritis and Musculoskeletal and Skin Diseases. [https://www.niams.nih.gov/health-topics/juvenile-arthritis/basics/symptoms-causes Juvenile Idiopathic Arthritis (JIA) Basics]. (last accessed 1 May 2023).</ref><ref name=":5">Eskay K. Paediatric Conditions – Autism, Developmental Coordination Disorder, Spina Bifida, Juvenile Idiopathic Arthritis, Haemophilia Course. Plus, 2023.</ref> | ||
* Pain and stiffness, including morning stiffness | |||
* Fatigue | |||
* | *[[Fever]] | ||
* | * Skin rash | ||
* | * Generally feeling unwell (malaise) | ||
* Uveitis (see image) | |||
* Decreased range of motion and soft tissue contractures | |||
* Muscle atrophy | |||
* Weakness, or reduced muscular endurance | |||
* Gait deviations | |||
== Diagnostic Tests == | |||
There is no definitive test to diagnose JIA,<ref name=":1" /> so JIA is a diagnosis based on exclusion. The following evaluations are often included:<ref name=":1" /><ref name=":2" /> | |||
* Medical history | |||
* Physical examination | |||
*[[Blood Tests|Laboratory tests]] - typical inflammatory markers are said to be common, particularly in oligoarthritis<ref name=":1" /> | |||
* Imaging | |||
** Radiography for symptomatic joints (in early JIA, there are no detectable changes on x-ray, but indirect signs may be present, increased soft tissue density etc<ref name=":1" />) | |||
** Ultrasound | |||
** MRI (the gold standard) | |||
* Eye examination | |||
[[ | == Pathology == | ||
[[Image:JIA-prevalence.jpg|399x399px|'''Figure.2''' Prevalence of Major Subtypes of JIA<ref>Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. 3rd ed. . St. Louis, MO: Saunders, an imprint of Elsevier Inc, 2009.</ref>|alt=|thumb]]There are several subtypes of JIA:<ref name=":1" /><ref name=":2" /><ref name=":0" /> | |||
* | |||
* | |||
* | |||
* | |||
* | |||
* | |||
# Oligoarticular JIA (also known as pauciarticular) | |||
#* affects four or fewer joints in the first six months of disease | |||
#* peak age for oligoarticular JIA is 1-6 years | |||
#* more common in females | |||
#* tends to impact medium and large joints | |||
#* risk of uveitis | |||
# Polyarticular JIA | |||
#* affects more than 5 joints | |||
#* peak ages for polyarticular JIA are 1-4 years and 7-10 years | |||
#* more common in females | |||
#* tends to impact small and medium joints | |||
# Systemic onset JIA | |||
#* also known as Still's disease | |||
#* associated with fever, other signs of systemic inflammation and arthritis<ref>Hedrich CM, Günther C, Aringer M. Morbus Still im Kindes- und Erwachsenenalter [Still's disease in children and adults]. Z Rheumatol. 2017 Sep;76(7):595-608. German. </ref> | |||
#* arthritis may begin weeks / months after the initial symptoms<ref name=":0">Radiopedia [https://radiopaedia.org/articles/juvenile-idiopathic-arthritis JIA] Available: https://radiopaedia.org/articles/juvenile-idiopathic-arthritis (accessed 18.10.2021)</ref> | |||
#* affects females / males equally | |||
#[[Psoriatic Arthritis|Psoriatic]] JIA | |||
#* causes psoriasis and inflammatory arthritis (these can develop at different times) | |||
#* more common in females | |||
#* occurs in preschool-aged children and at around 10 years | |||
#* tends to impact fingers, wrists, toes, but not exclusively | |||
# Enthesitis-related JIA | |||
#* inflammation of entheses | |||
#* more common in males | |||
#* tends to occur in older children / adolescents | |||
#* association with acute uveitis | |||
# Undifferentiated JIA | |||
#* JIA that does not fit into another category | |||
== Differential Diagnosis == | |||
Conditions that might be considered in a differential diagnosis include:<ref name="eMedicine" /><ref name="NCBI">National Center for Biotechnology Information, U.S. National Library of Medicine. Disease fact sheet: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001487/ (10 March 2011)</ref> | |||
*[http://www.physio-pedia.com/index.php5?title=Lyme_Disease Lyme Disease] | |||
*Rheumatic fever | |||
*[http://www.physio-pedia.com/index.php5?title=Osteomyelitis Osteomyelitis] | |||
*[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001450/ Psoriatic arthritis] | |||
*Inflammatory bowel disease | |||
*Leukemia | |||
*[http://emedicine.medscape.com/article/406697-overview#a01 Caffey Disease] | |||
*[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001133/ Chronic Eosinophilic Granuloma] | |||
*[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001400/ Osteoporosis] | |||
*[http://www.physio-pedia.com/index.php5?title=Lyme_Disease Lyme Disease] | |||
*Rheumatic fever | |||
*[http://www.physio-pedia.com/index.php5?title=Osteomyelitis Osteomyelitis] | |||
*[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001450/ Psoriatic arthritis] | |||
*Inflammatory bowel disease | |||
*Leukemia | |||
*[http://emedicine.medscape.com/article/406697-overview#a01 Caffey Disease] | |||
*[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001133/ Chronic Eosinophilic Granuloma] | |||
*[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001400/ Osteoporosis] | |||
*Involutional Osteoarthritis | *Involutional Osteoarthritis | ||
{{#ev:youtube|https://www.youtube.com/watch?v=YGO9pAIhoJg&t=72s}} | |||
== Management == | |||
==='''Pharmacology'''=== | |||
The choice of medication depends on type and severity of JIA and if there are other conditions present. Common medications include analgesics, non-steroidal anti-inflammatory drugs ([[NSAIDs in the Management of Rheumatoid Arthritis|NSAIDs]]), corticosteroids, disease modifying anti-rheumatic medications, [[BDMARDs in the Management of Rheumatoid Arthritis|biologics]] and biosimilar medicines and eye drops.<ref name=":1" /><ref name=":2" /> | |||
== | === Physiotherapy Management === | ||
Physiotherapy interventions focus on maintaining joint function and strength and teaching joint preservation strategies. Exercise programmes should incorporate low-impact, weight-bearing exercises (e.g. aquatic or bike programmes, gentle resistance exercises).<ref name=":5" /> | |||
Rehabilitation might include:<ref name=":5" /><ref name="eMedicine">eMedicine. Disease fact sheet: juvenile rheumatoid arthritis. http://emedicine.medscape.com/article/409980-overview (accessed 10 March 2011)</ref><ref>Bosques G, Singh MP. Juvenile Idiopathic Arthritis [Internet]. 2011, updated 2020 (cited 1 May 2023). Available from: https://now.aapmr.org/juvenile-idiopathic-arthritis/#rehabilitation-management-and-treatments</ref> | |||
* | *[[Strength Training|strengthening]] | ||
*[[Range of Motion|range of motion]] exercises and [[stretching]] | |||
*education on joint protection and pain reducing techniques | |||
*[[Adherence to Home Exercise Programs|home exercise programme]] | |||
*muscle relaxation techniques | |||
*splints / orthotics to help maintain bone and joint alignment / prevent deformities<ref name="NIAMS">National Institute of Arthritis and Musculoskeletal and Skin Diseases. Health information: juvenile arthritis. http://www.niams.nih.gov/Health_Info/Juv_Arthritis/default.asp (accessed 10 March 2011)</ref> | |||
*adaptive equipment | |||
Some modalities that might be used to help symptoms such as pain include: | |||
*[[Ultrasound therapy|ultrasound]] | |||
*paraffin wax dips (primarily for hands and feet) | |||
*moist compress ([[Thermotherapy|hot packs]]) | |||
*[[Aquatherapy|hydrotherapy]] | |||
*cold packs | |||
== | == Other Professionals involved in Managment of Juvenile Arthritis == | ||
JIA is a chronic inflammatory disease that affects children and adolescents. It is important to note that prompt diagnosis and proper treatment are crucial in preventing joint damage and promoting healthy growth and development<ref name=":6">Zaripova, L.N., Midgley, A., Christmas, S.E. ''et al.'' [https://ped-rheum.biomedcentral.com/articles/10.1186/s12969-021-00629-8 Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches]. ''Pediatr Rheumatol'' 19, 135 (2021).</ref><ref>Upadhyay J, Lemme J, Cay M, Van Der Heijden H, Sibai D, Goodlett B, Lo J, Hoyt K, Taylor M, Hazen MM, Halyabar O, Meidan E, Schreiber R, Chang MH, Nigrovic PA, Jaimes C, Henderson LA, Ecklund K, Sundel RP. [https://pubmed.ncbi.nlm.nih.gov/34139523/ A multidisciplinary assessment of pain in juvenile idiopathic arthritis.] Semin Arthritis Rheum. 2021 Aug;51(4):700-711. </ref>. | |||
Due to its complex and diverse nature, a team of healthcare experts from various disciplines should regularly evaluate and manage JIA. While there is no cure for JIA, achieving better clinical outcomes is possible. New biological disease-modifying antirheumatic drugs have effectively treated severe cases but come with an increased risk of infection <ref name=":6" />. The British Society for Paediatric and Adolescent Rheumatology has published care standards for children and young people with JIA. In managing JIA, it is crucial to involve multiple healthcare professionals, including physicians and allied health professionals (AHP)<ref name=":6" /> <ref name=":7">Fingerhutova, S., Saifridova, M., Vranova, M. ''et al.'' [https://ped-rheum.biomedcentral.com/articles/10.1186/1546-0096-12-S1-P177 Is there an evidence for the role of multidisciplinary team in the management of active juvenile idiopathic arthritis?.] ''Pediatr Rheumatol'' 12 (Suppl 1), P177 (2014).</ref>. A team of multidisciplinary healthcare experts, such as family doctors, rheumatologists, nurses, physiotherapists, occupational therapists, podiatrists, and social workers, should provide comprehensive JIA management, including drug treatment, physiotherapy/occupational therapy, education, and counselling <ref name=":7" />. | |||
== References == | |||
<references /> | <references /> | ||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]] | ||
[[Category:Paediatrics]] | [[Category:Paediatrics]] | ||
[[Category:Paediatrics - Conditions]] | [[Category:Paediatrics - Conditions]] | ||
[[Category:Autoimmune Disorders]] | [[Category:Autoimmune Disorders]] | ||
[[Category:Rheumatology]] | |||
Latest revision as of 13:45, 27 September 2023
Original Editors - Emily Betz from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Emily Betz, Lucinda hampton, Jess Bell, Ines Musabyemariya, Admin, Naomi O'Reilly, Khloud Shreif, Kim Jackson, Elaine Lonnemann, Mande Jooste, Wendy Walker, George Prudden, WikiSysop and Meaghan Rieke
Introduction[edit | edit source]
Juvenile idiopathic arthritis (JIA) is a term used to describe types of arthritis of unknown cause, where symptoms last for more than 6 weeks, in individuals aged under 16 years at the time of onset.[1]
JIA ranges in severity. It affects the joints, as well as other structures such as the eyes, skin, and organs,[2] and it can be divided into the following subtypes:[2]
- Oligoarticular
- Polyarticular
- Systemic
- Psoriatic
- Enthesitis-related
- Undifferentiated
Aetiology[edit | edit source]
The aetiology of JIA is unclear.[3] A range of factors have been proposed, including:[2]
- Genetic associations, genetic factors classified into: HLA genes and non-HLA-related genes.
- HLA class II molecules (A2, DRB1, DPB1) are associated with certain non-systemic JIA types, while systemic JIA is not linked to HLA genes.
- Autoimmune factors[4]
- Environmental factors (e.g. infectious agents, antibiotics, stress etc.) may be risk factors
- Infectious viruses (e.g., Epstein-Barr virus, Parvovirus B), bacteria (e.g., Salmonella spp., Shigella spp.) have been linked to the development of JIA, in addition, vaccinations, antibiotics, vitamin D deficiency, stress, and trauma may be causal factors.
- Gastrointestinal infections that result in reduced diversity in the gut microbiome and disturbances in tryptophan metabolism can elevate the susceptibility to developing enthesitis-related arthritis (ERA).
Epidemiology[edit | edit source]
JIA is the most common chronic heterogenous rheumatologic condition in children.[3][4] It is estimated that around 3 million children and young adults have JIA. The global prevalence is believed to range from 3.8 to 400/100,000; the incidence is estimated to be 1.6 to 23/100,000.[4]
Characteristics and Clinical Presentation[edit | edit source]
Symptoms of JIA vary depending on the type of arthritis.[6] It has an unpredictable course - it can be self-limiting or cause joint damage. But there is a general pattern of inflammatory joint disease in one or more joints:[3][6]
- Synovitis
- Joint effusion
- Swelling of soft tissues
- Osteopenia
- Bone oedema, erosions
Certain features of JIA will depend on the age of the child affected (e.g. involvement of epiphyseal growth plates, early physeal fusion or the development of discrepancies in limb length).[3]
Individuals may also experience:[6][7][8]
- Pain and stiffness, including morning stiffness
- Fatigue
- Fever
- Skin rash
- Generally feeling unwell (malaise)
- Uveitis (see image)
- Decreased range of motion and soft tissue contractures
- Muscle atrophy
- Weakness, or reduced muscular endurance
- Gait deviations
Diagnostic Tests[edit | edit source]
There is no definitive test to diagnose JIA,[3] so JIA is a diagnosis based on exclusion. The following evaluations are often included:[3][6]
- Medical history
- Physical examination
- Laboratory tests - typical inflammatory markers are said to be common, particularly in oligoarthritis[3]
- Imaging
- Radiography for symptomatic joints (in early JIA, there are no detectable changes on x-ray, but indirect signs may be present, increased soft tissue density etc[3])
- Ultrasound
- MRI (the gold standard)
- Eye examination
Pathology[edit | edit source]
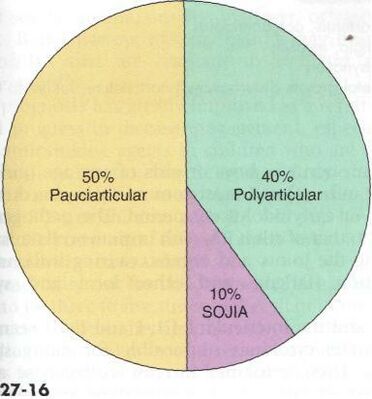
There are several subtypes of JIA:[3][6][10]
- Oligoarticular JIA (also known as pauciarticular)
- affects four or fewer joints in the first six months of disease
- peak age for oligoarticular JIA is 1-6 years
- more common in females
- tends to impact medium and large joints
- risk of uveitis
- Polyarticular JIA
- affects more than 5 joints
- peak ages for polyarticular JIA are 1-4 years and 7-10 years
- more common in females
- tends to impact small and medium joints
- Systemic onset JIA
- Psoriatic JIA
- causes psoriasis and inflammatory arthritis (these can develop at different times)
- more common in females
- occurs in preschool-aged children and at around 10 years
- tends to impact fingers, wrists, toes, but not exclusively
- Enthesitis-related JIA
- inflammation of entheses
- more common in males
- tends to occur in older children / adolescents
- association with acute uveitis
- Undifferentiated JIA
- JIA that does not fit into another category
Differential Diagnosis[edit | edit source]
Conditions that might be considered in a differential diagnosis include:[12][13]
- Lyme Disease
- Rheumatic fever
- Osteomyelitis
- Psoriatic arthritis
- Inflammatory bowel disease
- Leukemia
- Caffey Disease
- Chronic Eosinophilic Granuloma
- Osteoporosis
- Involutional Osteoarthritis
Management[edit | edit source]
Pharmacology[edit | edit source]
The choice of medication depends on type and severity of JIA and if there are other conditions present. Common medications include analgesics, non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, disease modifying anti-rheumatic medications, biologics and biosimilar medicines and eye drops.[3][6]
Physiotherapy Management[edit | edit source]
Physiotherapy interventions focus on maintaining joint function and strength and teaching joint preservation strategies. Exercise programmes should incorporate low-impact, weight-bearing exercises (e.g. aquatic or bike programmes, gentle resistance exercises).[8]
Rehabilitation might include:[8][12][14]
- strengthening
- range of motion exercises and stretching
- education on joint protection and pain reducing techniques
- home exercise programme
- muscle relaxation techniques
- splints / orthotics to help maintain bone and joint alignment / prevent deformities[15]
- adaptive equipment
Some modalities that might be used to help symptoms such as pain include:
- ultrasound
- paraffin wax dips (primarily for hands and feet)
- moist compress (hot packs)
- hydrotherapy
- cold packs
Other Professionals involved in Managment of Juvenile Arthritis[edit | edit source]
JIA is a chronic inflammatory disease that affects children and adolescents. It is important to note that prompt diagnosis and proper treatment are crucial in preventing joint damage and promoting healthy growth and development[16][17].
Due to its complex and diverse nature, a team of healthcare experts from various disciplines should regularly evaluate and manage JIA. While there is no cure for JIA, achieving better clinical outcomes is possible. New biological disease-modifying antirheumatic drugs have effectively treated severe cases but come with an increased risk of infection [16]. The British Society for Paediatric and Adolescent Rheumatology has published care standards for children and young people with JIA. In managing JIA, it is crucial to involve multiple healthcare professionals, including physicians and allied health professionals (AHP)[16] [18]. A team of multidisciplinary healthcare experts, such as family doctors, rheumatologists, nurses, physiotherapists, occupational therapists, podiatrists, and social workers, should provide comprehensive JIA management, including drug treatment, physiotherapy/occupational therapy, education, and counselling [18].
References[edit | edit source]
- ↑ Rigante D, Bosco A, Esposito S. The Etiology of Juvenile Idiopathic Arthritis. Clin Rev Allergy Immunol. 2015 Oct;49(2):253-61.
- ↑ 2.0 2.1 2.2 2.3 Zaripova LN, Midgley A, Christmas SE, Beresford MW, Baildam EM, Oldershaw RA. Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches. Pediatr Rheumatol Online J. 2021 Aug 23;19(1):135.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Thatayatikom A, Modica R, De Leucio A. Juvenile Idiopathic Arthritis. [Updated 2023 Jan 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan.
- ↑ 4.0 4.1 4.2 4.3 4.4 Al-Mayouf SM, Al Mutairi M, Bouayed K, Habjoka S, Hadef D, Lotfy HM, Scott C, Sharif EM, Tahoun N. Epidemiology and demographics of juvenile idiopathic arthritis in Africa and Middle East. Pediatr Rheumatol Online J. 2021 Dec 2;19(1):166.
- ↑ França CMP, Sallum AM, Silva CAA, Aikawa NE, Braga AL, Farhat SC. Risk factors for juvenile idiopathic arthritis: exposure to tobacco and environmental factors during and before pregnancy. Pediatr Rheumatol Online J. 2014 Sep 17;12(Suppl 1):P27.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 better Health Juvenile Arthritis Available: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile(accessed 18.10.2021)
- ↑ National Institute of Arthritis and Musculoskeletal and Skin Diseases. Juvenile Idiopathic Arthritis (JIA) Basics. (last accessed 1 May 2023).
- ↑ 8.0 8.1 8.2 Eskay K. Paediatric Conditions – Autism, Developmental Coordination Disorder, Spina Bifida, Juvenile Idiopathic Arthritis, Haemophilia Course. Plus, 2023.
- ↑ Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. 3rd ed. . St. Louis, MO: Saunders, an imprint of Elsevier Inc, 2009.
- ↑ 10.0 10.1 Radiopedia JIA Available: https://radiopaedia.org/articles/juvenile-idiopathic-arthritis (accessed 18.10.2021)
- ↑ Hedrich CM, Günther C, Aringer M. Morbus Still im Kindes- und Erwachsenenalter [Still's disease in children and adults]. Z Rheumatol. 2017 Sep;76(7):595-608. German.
- ↑ 12.0 12.1 eMedicine. Disease fact sheet: juvenile rheumatoid arthritis. http://emedicine.medscape.com/article/409980-overview (accessed 10 March 2011)
- ↑ National Center for Biotechnology Information, U.S. National Library of Medicine. Disease fact sheet: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001487/ (10 March 2011)
- ↑ Bosques G, Singh MP. Juvenile Idiopathic Arthritis [Internet]. 2011, updated 2020 (cited 1 May 2023). Available from: https://now.aapmr.org/juvenile-idiopathic-arthritis/#rehabilitation-management-and-treatments
- ↑ National Institute of Arthritis and Musculoskeletal and Skin Diseases. Health information: juvenile arthritis. http://www.niams.nih.gov/Health_Info/Juv_Arthritis/default.asp (accessed 10 March 2011)
- ↑ 16.0 16.1 16.2 Zaripova, L.N., Midgley, A., Christmas, S.E. et al. Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches. Pediatr Rheumatol 19, 135 (2021).
- ↑ Upadhyay J, Lemme J, Cay M, Van Der Heijden H, Sibai D, Goodlett B, Lo J, Hoyt K, Taylor M, Hazen MM, Halyabar O, Meidan E, Schreiber R, Chang MH, Nigrovic PA, Jaimes C, Henderson LA, Ecklund K, Sundel RP. A multidisciplinary assessment of pain in juvenile idiopathic arthritis. Semin Arthritis Rheum. 2021 Aug;51(4):700-711.
- ↑ 18.0 18.1 Fingerhutova, S., Saifridova, M., Vranova, M. et al. Is there an evidence for the role of multidisciplinary team in the management of active juvenile idiopathic arthritis?. Pediatr Rheumatol 12 (Suppl 1), P177 (2014).