Juvenile Idiopathic Arthritis: Difference between revisions
No edit summary |
(replaced images with another free copy right, added to aetiology section.) |
||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
[[File: | [[File:Juvenile arthritis.jpg|alt=|thumb|419x419px|'''Figure.1''' Swollen joints in Patient with JIA]] | ||
Juvenile idiopathic arthritis (JIA) is a term used to describe types of arthritis of unknown cause, where symptoms last for more than 6 weeks, in individuals aged under 16 years at the time of onset.<ref>Rigante D, Bosco A, Esposito S. The Etiology of Juvenile Idiopathic Arthritis. Clin Rev Allergy Immunol. 2015 Oct;49(2):253-61.</ref> | |||
JIA ranges in severity. It affects the joints, as well as other structures such as the eyes, skin, and organs,<ref name=":3" /> and it can be divided into the following subtypes:<ref name=":3">Zaripova LN, Midgley A, Christmas SE, Beresford MW, Baildam EM, Oldershaw RA. [https://ped-rheum.biomedcentral.com/articles/10.1186/s12969-021-00629-8 Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches]. Pediatr Rheumatol Online J. 2021 Aug 23;19(1):135. </ref> | JIA ranges in severity. It affects the joints, as well as other structures such as the eyes, skin, and organs,<ref name=":3" /> and it can be divided into the following subtypes:<ref name=":3">Zaripova LN, Midgley A, Christmas SE, Beresford MW, Baildam EM, Oldershaw RA. [https://ped-rheum.biomedcentral.com/articles/10.1186/s12969-021-00629-8 Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches]. Pediatr Rheumatol Online J. 2021 Aug 23;19(1):135. </ref> | ||
* | * Oligoarticular | ||
* | * Polyarticular | ||
* | * Systemic | ||
* | * Psoriatic | ||
* | * Enthesitis-related | ||
* | * Undifferentiated | ||
== Aetiology == | == Aetiology == | ||
The aetiology of JIA is unclear.<ref name=":1">Thatayatikom A, Modica R, De Leucio A. Juvenile Idiopathic Arthritis. [Updated 2023 Jan 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan | The aetiology of JIA is unclear.<ref name=":1">Thatayatikom A, Modica R, De Leucio A. [https://www.ncbi.nlm.nih.gov/books/NBK554605/ Juvenile Idiopathic Arthritis]. [Updated 2023 Jan 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan.</ref> A range of factors have been proposed, including:<ref name=":3" /> | ||
* genetic | * Genetic associations, genetic factors classified into: HLA genes and non-HLA-related genes. | ||
* | ** HLA class II molecules (A2, DRB1, DPB1) are associated with certain non-systemic JIA types, while systemic JIA is not linked to HLA genes. | ||
* | * Autoimmune factors<ref name=":4">Al-Mayouf SM, Al Mutairi M, Bouayed K, Habjoka S, Hadef D, Lotfy HM, Scott C, Sharif EM, Tahoun N. [https://ped-rheum.biomedcentral.com/articles/10.1186/s12969-021-00650-x Epidemiology and demographics of juvenile idiopathic arthritis in Africa and Middle East]. Pediatr Rheumatol Online J. 2021 Dec 2;19(1):166. </ref> | ||
** maternal factors (e.g. smoking<ref name=":3" /><ref>França CMP, Sallum AM, Silva CAA, Aikawa NE, Braga AL, Farhat SC. [https://www.jrheum.org/content/45/2/248 Risk factors for juvenile idiopathic arthritis: exposure to tobacco and environmental factors during and before pregnancy]. Pediatr Rheumatol Online J. 2014 Sep 17;12(Suppl 1):P27. </ref>) may be involved, but breastfeeding / having household siblings may reduce risk | * Environmental factors (e.g. infectious agents, antibiotics, stress etc.) may be risk factors | ||
* | ** maternal factors (e.g. smoking<ref name=":3" /><ref>França CMP, Sallum AM, Silva CAA, Aikawa NE, Braga AL, Farhat SC. [https://www.jrheum.org/content/45/2/248 Risk factors for juvenile idiopathic arthritis: exposure to tobacco and environmental factors during and before pregnancy]. Pediatr Rheumatol Online J. 2014 Sep 17;12(Suppl 1):P27. </ref>) may be involved, but breastfeeding / having household siblings may reduce risk. | ||
* Infectious viruses (e.g., Epstein-Barr virus, Parvovirus B), bacteria (e.g., Salmonella spp., Shigella spp.) have been linked to the development of JIA, in addition, vaccinations, antibiotics, vitamin D deficiency, stress, and trauma may be causal factors. | |||
* Gastrointestinal infections that result in reduced diversity in the gut microbiome and disturbances in tryptophan metabolism can elevate the susceptibility to developing enthesitis-related arthritis (ERA). | |||
== Epidemiology == | == Epidemiology == | ||
| Line 32: | Line 35: | ||
== Characteristics and Clinical Presentation == | == Characteristics and Clinical Presentation == | ||
[[ | [[File:Anterior-uveitis.jpg|thumb|231x231px|Anterior-uveitis]] | ||
Symptoms of JIA vary depending on the type of arthritis.<ref name=":2">better Health [https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile Juvenile Arthritis] Available: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile<nowiki/>(accessed 18.10.2021)</ref> It has an unpredictable course - it can be self-limiting or cause joint damage. But there is a general pattern of inflammatory joint disease in one or more joints:<ref name=":1" /><ref name=":2" /> | Symptoms of JIA vary depending on the type of arthritis.<ref name=":2">better Health [https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile Juvenile Arthritis] Available: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile<nowiki/>(accessed 18.10.2021)</ref> It has an unpredictable course - it can be self-limiting or cause joint damage. But there is a general pattern of inflammatory joint disease in one or more joints:<ref name=":1" /><ref name=":2" /> | ||
* | * Synovitis | ||
* | * Joint effusion | ||
* | * Swelling of soft tissues | ||
* | * Osteopenia | ||
* | * Bone oedema, erosions | ||
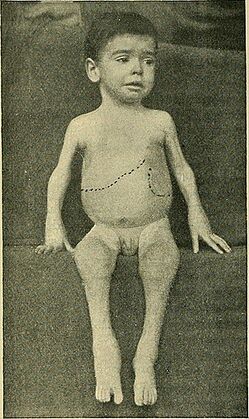
Certain features of JIA will depend on the age of the child affected (e.g. involvement of epiphyseal growth plates, early physeal fusion or the development of discrepancies in limb length).<ref name=":1" /> | Certain features of JIA will depend on the age of the child affected (e.g. involvement of epiphyseal growth plates, early physeal fusion or the development of discrepancies in limb length).<ref name=":1" /> | ||
Individuals may also experience:<ref name=":2" /><ref>National Institute of Arthritis and Musculoskeletal and Skin Diseases. | Individuals may also experience:<ref name=":2" /><ref>National Institute of Arthritis and Musculoskeletal and Skin Diseases. [https://www.niams.nih.gov/health-topics/juvenile-arthritis/basics/symptoms-causes Juvenile Idiopathic Arthritis (JIA) Basics]. (last accessed 1 May 2023).</ref><ref name=":5">Eskay K. Paediatric Conditions – Autism, Developmental Coordination Disorder, Spina Bifida, Juvenile Idiopathic Arthritis, Haemophilia Course. Plus, 2023.</ref> | ||
* | * Pain and stiffness, including morning stiffness | ||
* | * Fatigue | ||
*[[ | *[[Fever]] | ||
* | * Skin rash | ||
* | * Generally feeling unwell (malaise) | ||
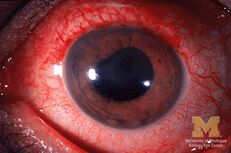
* | * Uveitis (see image) | ||
* | * Decreased range of motion and soft tissue contractures | ||
* | * Muscle atrophy | ||
* | * Weakness, or reduced muscular endurance | ||
* | * Gait deviations | ||
== Diagnostic Tests == | == Diagnostic Tests == | ||
There is no definitive test to diagnose JIA,<ref name=":1" /> so JIA is a diagnosis based on exclusion. The following evaluations are often included:<ref name=":1" /><ref name=":2" /> | There is no definitive test to diagnose JIA,<ref name=":1" /> so JIA is a diagnosis based on exclusion. The following evaluations are often included:<ref name=":1" /><ref name=":2" /> | ||
* | * Medical history | ||
* | * Physical examination | ||
*[[Blood Tests| | *[[Blood Tests|Laboratory tests]] - typical inflammatory markers are said to be common, particularly in oligoarthritis<ref name=":1" /> | ||
* | * Imaging | ||
** | ** Radiography for symptomatic joints (in early JIA, there are no detectable changes on x-ray, but indirect signs may be present, increased soft tissue density etc<ref name=":1" />) | ||
** | ** Ultrasound | ||
** MRI (the gold standard) | ** MRI (the gold standard) | ||
* | * Eye examination | ||
== Pathology == | == Pathology == | ||
Revision as of 22:14, 5 September 2023
Original Editors - Emily Betz from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Emily Betz, Lucinda hampton, Jess Bell, Ines Musabyemariya, Admin, Naomi O'Reilly, Khloud Shreif, Kim Jackson, Elaine Lonnemann, Meaghan Rieke, Mande Jooste, Wendy Walker, George Prudden and WikiSysop
This article is currently under review and may not be up to date. Please come back soon to see the finished work! (05/09/2023)
Introduction[edit | edit source]
Juvenile idiopathic arthritis (JIA) is a term used to describe types of arthritis of unknown cause, where symptoms last for more than 6 weeks, in individuals aged under 16 years at the time of onset.[1]
JIA ranges in severity. It affects the joints, as well as other structures such as the eyes, skin, and organs,[2] and it can be divided into the following subtypes:[2]
- Oligoarticular
- Polyarticular
- Systemic
- Psoriatic
- Enthesitis-related
- Undifferentiated
Aetiology[edit | edit source]
The aetiology of JIA is unclear.[3] A range of factors have been proposed, including:[2]
- Genetic associations, genetic factors classified into: HLA genes and non-HLA-related genes.
- HLA class II molecules (A2, DRB1, DPB1) are associated with certain non-systemic JIA types, while systemic JIA is not linked to HLA genes.
- Autoimmune factors[4]
- Environmental factors (e.g. infectious agents, antibiotics, stress etc.) may be risk factors
- Infectious viruses (e.g., Epstein-Barr virus, Parvovirus B), bacteria (e.g., Salmonella spp., Shigella spp.) have been linked to the development of JIA, in addition, vaccinations, antibiotics, vitamin D deficiency, stress, and trauma may be causal factors.
- Gastrointestinal infections that result in reduced diversity in the gut microbiome and disturbances in tryptophan metabolism can elevate the susceptibility to developing enthesitis-related arthritis (ERA).
Epidemiology[edit | edit source]
JIA is the most common chronic heterogenous rheumatologic condition in children.[3][4] It is estimated that around 3 million children and young adults have JIA. The global prevalence is believed to range from 3.8 to 400/100,000; the incidence is estimated to be 1.6 to 23/100,000.[4]
Characteristics and Clinical Presentation[edit | edit source]
Symptoms of JIA vary depending on the type of arthritis.[6] It has an unpredictable course - it can be self-limiting or cause joint damage. But there is a general pattern of inflammatory joint disease in one or more joints:[3][6]
- Synovitis
- Joint effusion
- Swelling of soft tissues
- Osteopenia
- Bone oedema, erosions
Certain features of JIA will depend on the age of the child affected (e.g. involvement of epiphyseal growth plates, early physeal fusion or the development of discrepancies in limb length).[3]
Individuals may also experience:[6][7][8]
- Pain and stiffness, including morning stiffness
- Fatigue
- Fever
- Skin rash
- Generally feeling unwell (malaise)
- Uveitis (see image)
- Decreased range of motion and soft tissue contractures
- Muscle atrophy
- Weakness, or reduced muscular endurance
- Gait deviations
Diagnostic Tests[edit | edit source]
There is no definitive test to diagnose JIA,[3] so JIA is a diagnosis based on exclusion. The following evaluations are often included:[3][6]
- Medical history
- Physical examination
- Laboratory tests - typical inflammatory markers are said to be common, particularly in oligoarthritis[3]
- Imaging
- Radiography for symptomatic joints (in early JIA, there are no detectable changes on x-ray, but indirect signs may be present, increased soft tissue density etc[3])
- Ultrasound
- MRI (the gold standard)
- Eye examination
Pathology[edit | edit source]
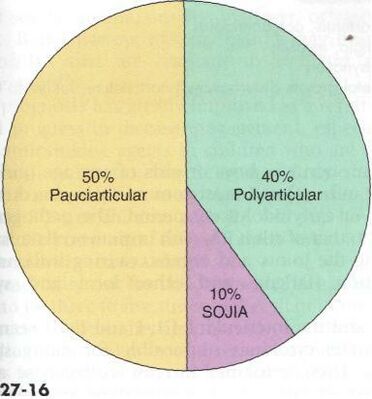
There are several subtypes of JIA:[3][6][10]
- Oligoarticular JIA (also known as pauciarticular)
- affects four or fewer joints in the first six months of disease
- peak age for oligoarticular JIA is 1-6 years
- more common in females
- tends to impact medium and large joints
- risk of uveitis
- Polyarticular JIA
- affects more than 5 joints
- peak ages for polyarticular JIA are 1-4 years and 7-10 years
- more common in females
- tends to impact small and medium joints
- Systemic onset JIA
- Psoriatic JIA
- causes psoriasis and inflammatory arthritis (these can develop at different times)
- more common in females
- occurs in preschool-aged children and at around 10 years
- tends to impact fingers, wrists, toes, but not exclusively
- Enthesitis-related JIA
- inflammation of entheses
- more common in males
- tends to occur in older children / adolescents
- association with acute uveitis
- Undifferentiated JIA
- JIA that does not fit into another category
Differential Diagnosis[edit | edit source]
Conditions that might be considered in a differential diagnosis include:[12][13]
- Lyme Disease
- Rheumatic fever
- Osteomyelitis
- Psoriatic arthritis
- Inflammatory bowel disease
- Leukemia
- Caffey Disease
- Chronic Eosinophilic Granuloma
- Osteoporosis
- Involutional Osteoarthritis
Management[edit | edit source]
Pharmacology[edit | edit source]
The choice of medication depends on type and severity of JIA and if there are other conditions present. Common medications include analgesics, non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, disease modifying anti-rheumatic medications, biologics and biosimilar medicines and eye drops.[3][6]
Physiotherapy Management[edit | edit source]
Physiotherapy interventions focus on maintaining joint function and strength and teaching joint preservation strategies. Exercise programmes should incorporate low-impact, weight-bearing exercises (e.g. aquatic or bike programmes, gentle resistance exercises).[8]
Rehabilitation might include:[8][12][14]
- strengthening
- range of motion exercises and stretching
- education on joint protection and pain reducing techniques
- home exercise programme
- muscle relaxation techniques
- splints / orthotics to help maintain bone and joint alignment / prevent deformities[15]
- adaptive equipment
Some modalities that might be used to help symptoms such as pain include:
- ultrasound
- paraffin wax dips (primarily for hands and feet)
- moist compress (hot packs)
- hydrotherapy
- cold packs
References[edit | edit source]
- ↑ Rigante D, Bosco A, Esposito S. The Etiology of Juvenile Idiopathic Arthritis. Clin Rev Allergy Immunol. 2015 Oct;49(2):253-61.
- ↑ 2.0 2.1 2.2 2.3 Zaripova LN, Midgley A, Christmas SE, Beresford MW, Baildam EM, Oldershaw RA. Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches. Pediatr Rheumatol Online J. 2021 Aug 23;19(1):135.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Thatayatikom A, Modica R, De Leucio A. Juvenile Idiopathic Arthritis. [Updated 2023 Jan 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan.
- ↑ 4.0 4.1 4.2 4.3 4.4 Al-Mayouf SM, Al Mutairi M, Bouayed K, Habjoka S, Hadef D, Lotfy HM, Scott C, Sharif EM, Tahoun N. Epidemiology and demographics of juvenile idiopathic arthritis in Africa and Middle East. Pediatr Rheumatol Online J. 2021 Dec 2;19(1):166.
- ↑ França CMP, Sallum AM, Silva CAA, Aikawa NE, Braga AL, Farhat SC. Risk factors for juvenile idiopathic arthritis: exposure to tobacco and environmental factors during and before pregnancy. Pediatr Rheumatol Online J. 2014 Sep 17;12(Suppl 1):P27.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 better Health Juvenile Arthritis Available: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile(accessed 18.10.2021)
- ↑ National Institute of Arthritis and Musculoskeletal and Skin Diseases. Juvenile Idiopathic Arthritis (JIA) Basics. (last accessed 1 May 2023).
- ↑ 8.0 8.1 8.2 Eskay K. Paediatric Conditions – Autism, Developmental Coordination Disorder, Spina Bifida, Juvenile Idiopathic Arthritis, Haemophilia Course. Plus, 2023.
- ↑ Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. 3rd ed. . St. Louis, MO: Saunders, an imprint of Elsevier Inc, 2009.
- ↑ 10.0 10.1 Radiopedia JIA Available: https://radiopaedia.org/articles/juvenile-idiopathic-arthritis (accessed 18.10.2021)
- ↑ Hedrich CM, Günther C, Aringer M. Morbus Still im Kindes- und Erwachsenenalter [Still's disease in children and adults]. Z Rheumatol. 2017 Sep;76(7):595-608. German.
- ↑ 12.0 12.1 eMedicine. Disease fact sheet: juvenile rheumatoid arthritis. http://emedicine.medscape.com/article/409980-overview (accessed 10 March 2011)
- ↑ National Center for Biotechnology Information, U.S. National Library of Medicine. Disease fact sheet: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001487/ (10 March 2011)
- ↑ Bosques G, Singh MP. Juvenile Idiopathic Arthritis [Internet]. 2011, updated 2020 (cited 1 May 2023). Available from: https://now.aapmr.org/juvenile-idiopathic-arthritis/#rehabilitation-management-and-treatments
- ↑ National Institute of Arthritis and Musculoskeletal and Skin Diseases. Health information: juvenile arthritis. http://www.niams.nih.gov/Health_Info/Juv_Arthritis/default.asp (accessed 10 March 2011)