Juvenile Idiopathic Arthritis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 7: | Line 7: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
[[File:JIA-swollenjoint.jpg|alt=|thumb|'''Figure.1''' Swollen Right Knee in Patient with JIA]]Juvenile idiopathic arthritis (JIA) is used to describe types of arthritis of unknown cause, where symptoms last more than 6 weeks, in individuals aged under 16 years at the time of onset.<ref>Rigante D, Bosco A, Esposito S. The Etiology of Juvenile Idiopathic Arthritis. Clin Rev Allergy Immunol. 2015 Oct;49(2):253-61.</ref> It is divided into the following types of arthritis:<ref name=":3">Zaripova LN, Midgley A, Christmas SE, Beresford MW, Baildam EM, Oldershaw RA. [https://ped-rheum.biomedcentral.com/articles/10.1186/s12969-021-00629-8 Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches]. Pediatr Rheumatol Online J. 2021 Aug 23;19(1):135. </ref> | [[File:JIA-swollenjoint.jpg|alt=|thumb|'''Figure.1''' Swollen Right Knee in Patient with JIA]]Juvenile idiopathic arthritis (JIA) is a term used to describe types of arthritis of unknown cause, where symptoms last for more than 6 weeks, in individuals aged under 16 years at the time of onset.<ref>Rigante D, Bosco A, Esposito S. The Etiology of Juvenile Idiopathic Arthritis. Clin Rev Allergy Immunol. 2015 Oct;49(2):253-61.</ref> It is divided into the following types of arthritis:<ref name=":3">Zaripova LN, Midgley A, Christmas SE, Beresford MW, Baildam EM, Oldershaw RA. [https://ped-rheum.biomedcentral.com/articles/10.1186/s12969-021-00629-8 Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches]. Pediatr Rheumatol Online J. 2021 Aug 23;19(1):135. </ref> | ||
* oligoarticular | * oligoarticular | ||
| Line 21: | Line 21: | ||
== Aetiology == | == Aetiology == | ||
The aetiology of JIA is unclear.<ref name=":1">Thatayatikom A, De Leucio A. | The aetiology of JIA is unclear.<ref name=":1">Thatayatikom A, Modica R, De Leucio A. Juvenile Idiopathic Arthritis. [Updated 2023 Jan 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: <nowiki>https://www.ncbi.nlm.nih.gov/books/NBK554605/</nowiki></ref> The following factors have been proposed:<ref name=":3" /> | ||
* genetic associations | * genetic associations | ||
| Line 37: | Line 37: | ||
== Characteristics and Clinical Presentation == | == Characteristics and Clinical Presentation == | ||
[[Image:Uveitis.jpg|alt=|thumb|'''Figure.3''' Uveitis]] | [[Image:Uveitis.jpg|alt=|thumb|'''Figure.3''' Uveitis]] | ||
Symptoms of JIA vary depending on the type of arthritis.<ref name=":2" /> | Symptoms of JIA vary depending on the type of arthritis.<ref name=":2">better Health [https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile Juvenile Arthritis] Available: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile<nowiki/>(accessed 18.10.2021)</ref> It has an unpredictable course - it can be self-limiting or lead on to joint damage. But there is a general pattern of inflammatory joint disease in one or more joints. Joint signs include:<ref name=":1" /><ref name=":2" /> | ||
* synovitis | * synovitis | ||
| Line 45: | Line 45: | ||
* bone oedema, erosions | * bone oedema, erosions | ||
Individuals may also experience:<ref name=":2" /> | There can be specific features of JIA which are associated with the child's age, including the involvement of epiphyseal growth plates, early physeal fusion and there may be discrepancies in limb length.<ref name=":1" /> | ||
Individuals may also experience:<ref name=":2" /><ref>National Institute of Arthritis and Musculoskeletal and Skin Diseases. Juvenile Idiopathic Arthritis (JIA) Basics. Available from: https://www.niams.nih.gov/health-topics/juvenile-arthritis/basics/symptoms-causes (last accessed 1 May 2023).</ref> | |||
* pain | |||
* fatigue | * fatigue | ||
*[[fever]] | *[[fever]] | ||
* rash | * rash | ||
* feeling | * generally feeling unwell (malaise) | ||
* | * uveitis (see image) | ||
* decreased range of motion | |||
== Diagnostic Tests == | == Diagnostic Tests == | ||
There is no specific test to diagnose JIA,<ref name=":1" /> but the following may be included:<ref name=":1" /><ref name=":2" /> | |||
* medical history | * medical history | ||
* physical examination | * physical examination | ||
*[[Blood Tests| | *[[Blood Tests|laboratory tests]] - typical inflammatory markers are said to be common, particularly in oligoarthritis<ref name=":1" /> | ||
* x- | * imaging | ||
** radiography for symptomatic joints (but in early JIA, there are no detectable changes on x-ray, but indirect signs may be present, including swelling of soft tissues and dislocation of fat folds<ref name=":1" />) | |||
** ultrasound | |||
** MRI (the gold standard) | |||
* eye examination | |||
== Pathology == | == Pathology == | ||
[[Image:JIA-prevalence.jpg|399x399px|'''Figure.2''' Prevalence of Major Subtypes of JIA<ref>Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. 3rd ed. . St. Louis, MO: Saunders, an imprint of Elsevier Inc, 2009.</ref>|alt=|thumb]]There are several subtypes of JIA: | [[Image:JIA-prevalence.jpg|399x399px|'''Figure.2''' Prevalence of Major Subtypes of JIA<ref>Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. 3rd ed. . St. Louis, MO: Saunders, an imprint of Elsevier Inc, 2009.</ref>|alt=|thumb]]There are several subtypes of JIA:<ref name=":1" /><ref name=":2" /><ref name=":0" /> | ||
=== | # Oligoarticular JIA (also known as pauciarticular) | ||
#* affected four joints or less in the first six months of disease | |||
#* peak ages are 1-6 years | |||
#* more common in females | |||
#* tends to impact medium and large joints | |||
#* risk of uveitis | |||
# Polyarticular JIA | |||
#* affects more than 5 joints | |||
#* peak ages are 1-4 years and 7-10 years | |||
#* more common in females | |||
#* tends to impact small and medium joints | |||
# Systemic onset JIA | |||
#* known also as Still's disease | |||
#* associated with fever, other signs of systemic inflammation and arthritis<ref>Hedrich CM, Günther C, Aringer M. Morbus Still im Kindes- und Erwachsenenalter [Still's disease in children and adults]. Z Rheumatol. 2017 Sep;76(7):595-608. German. </ref> | |||
#* arthritis may begin weeks / months after the initial symptoms<ref name=":0">Radiopedia [https://radiopaedia.org/articles/juvenile-idiopathic-arthritis JIA] Available: https://radiopaedia.org/articles/juvenile-idiopathic-arthritis (accessed 18.10.2021)</ref> | |||
#* affects females/males equally | |||
#[[Psoriatic Arthritis|Psoriatic]] JIA | |||
#* causes psoriasis and inflammatory arthritis (can develop at different times) | |||
#* more common in females | |||
#* occurs in preschool-aged children and at around 10 years | |||
#* tends to impact fingers, wrists, toes, but not exclusively | |||
# Enthesitis-related JIA | |||
#* inflammation of entheses | |||
#* more common in males | |||
#* tends to occur in older children/adolescents | |||
#* association with acute uveitis | |||
# Undifferentiated JIA | |||
#* JIA that does not fit into another category | |||
== Management == | |||
Treatment for JIA includes pharmacology, physiotherapy, potentially surgery, and in some cases nutritional and psychosocial support.<ref name=":1" /> | |||
== '''Pharmacology''' == | |||
'''T'''he choice of medication depends on type and severity of JIA and if there are other conditions. Common medications include analgesics, eye drops, non-steroidal anti-inflammatory drugs ([[NSAIDs in the Management of Rheumatoid Arthritis|NSAIDs]]), corticosteroids, disease modifying anti-rheumatic medications, [[BDMARDs in the Management of Rheumatoid Arthritis|biologics]] and biosimilar medicines.<ref name=":1" /><ref name=":2" /> | |||
== Physiotherapy Management == | == Physiotherapy Management == | ||
| Line 135: | Line 137: | ||
*[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001400/ Osteoporosis] | *[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001400/ Osteoporosis] | ||
*Involutional Osteoarthritis | *Involutional Osteoarthritis | ||
== References == | == References == | ||
<references /> | <references /> | ||
Revision as of 03:16, 1 May 2023
Original Editors - Emily Betz from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Emily Betz, Lucinda hampton, Jess Bell, Admin, Ines Musabyemariya, Naomi O'Reilly, Khloud Shreif, Kim Jackson, Elaine Lonnemann, Wendy Walker, George Prudden, WikiSysop, Meaghan Rieke and Mande Jooste
Introduction[edit | edit source]
Juvenile idiopathic arthritis (JIA) is a term used to describe types of arthritis of unknown cause, where symptoms last for more than 6 weeks, in individuals aged under 16 years at the time of onset.[1] It is divided into the following types of arthritis:[2]
- oligoarticular
- polyarticular
- systemic
- psoriatic
- enthesitis-related
- undifferentiated
JIA is "characterized by chronic arthritis and hallmarked by elevated levels of circulating immune complexes (CICs) and associated complement activation by-products in their sera."[3]
JIA ranges in severity. It affects the joints, as well as other structures such as the eyes, skin, and organs.[2]
Aetiology[edit | edit source]
The aetiology of JIA is unclear.[4] The following factors have been proposed:[2]
- genetic associations
- autoimmune factors[5]
- environmental factors (e.g. infectious agents, antibiotics, stress etc) may be risk factors
- infectious viruses and bacteria may be causal factors
- maternal factors (e.g. smoking[2][6]) may be involved, but breastfeeding / having household siblings may reduce risk
Epidemiology[edit | edit source]
JIA is the most common chronic heterogenous rheumatologic condition in children.[4][5] It is estimated that around 3 million children and young adults have JIA. The global prevalence is believed to range from 3.8 to 400/100,000; the incidence is estimated to be 1.6 to 23/100,000.[5]
Characteristics and Clinical Presentation[edit | edit source]
Symptoms of JIA vary depending on the type of arthritis.[7] It has an unpredictable course - it can be self-limiting or lead on to joint damage. But there is a general pattern of inflammatory joint disease in one or more joints. Joint signs include:[4][7]
- synovitis
- joint effusion
- swelling of soft tissues
- osteopenia
- bone oedema, erosions
There can be specific features of JIA which are associated with the child's age, including the involvement of epiphyseal growth plates, early physeal fusion and there may be discrepancies in limb length.[4]
Individuals may also experience:[7][8]
- pain
- fatigue
- fever
- rash
- generally feeling unwell (malaise)
- uveitis (see image)
- decreased range of motion
Diagnostic Tests[edit | edit source]
There is no specific test to diagnose JIA,[4] but the following may be included:[4][7]
- medical history
- physical examination
- laboratory tests - typical inflammatory markers are said to be common, particularly in oligoarthritis[4]
- imaging
- radiography for symptomatic joints (but in early JIA, there are no detectable changes on x-ray, but indirect signs may be present, including swelling of soft tissues and dislocation of fat folds[4])
- ultrasound
- MRI (the gold standard)
- eye examination
Pathology[edit | edit source]
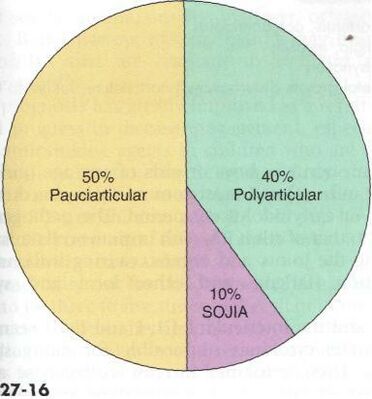
There are several subtypes of JIA:[4][7][10]
- Oligoarticular JIA (also known as pauciarticular)
- affected four joints or less in the first six months of disease
- peak ages are 1-6 years
- more common in females
- tends to impact medium and large joints
- risk of uveitis
- Polyarticular JIA
- affects more than 5 joints
- peak ages are 1-4 years and 7-10 years
- more common in females
- tends to impact small and medium joints
- Systemic onset JIA
- Psoriatic JIA
- causes psoriasis and inflammatory arthritis (can develop at different times)
- more common in females
- occurs in preschool-aged children and at around 10 years
- tends to impact fingers, wrists, toes, but not exclusively
- Enthesitis-related JIA
- inflammation of entheses
- more common in males
- tends to occur in older children/adolescents
- association with acute uveitis
- Undifferentiated JIA
- JIA that does not fit into another category
Management[edit | edit source]
Treatment for JIA includes pharmacology, physiotherapy, potentially surgery, and in some cases nutritional and psychosocial support.[4]
Pharmacology[edit | edit source]
The choice of medication depends on type and severity of JIA and if there are other conditions. Common medications include analgesics, eye drops, non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, disease modifying anti-rheumatic medications, biologics and biosimilar medicines.[4][7]
Physiotherapy Management[edit | edit source]
Physical therapy is an important part of the treatment of JIA. It is important for the child to remain active and involved in sports and activities with their peers and friends. While pain may limit the amount of activity a child can handle it is important to encourage involvement during periods or remission and allow rest and symptom reducing therapies during periods of flare-ups. Regular activity and general exercise programs help to maintain range of motion in affective joints, build and maintain strength, maintain function and can even help with symptom reduction.
Aspects that should be focused on during a physical therapy session are as follows[12]:
- Muscle tone
- Strengthening
- Range of motion
- Stretching
- Education on joint protection
- Home exercise plan
- Education on pain reducing techniques
- Muscle relaxation techniques
- Splints or Introduction to Orthotics maybe be beneficial to help maintain normal bone and joint growth/prevent deformities during growth[13]
Some modalities that can be used to help reduce symptoms such as pain are:
- Ultrasound
- Paraffin wax dips (hands and feet primarily)
- Moist compress (hot pack)
- Hydrotherapy (warm)
- Cold packs
Differential Diagnosis[edit | edit source]
Some signs and symptoms of JIA are shared with those of the following diseases[12][14]:
- Lyme Disease
- Rheumatic fever
- Osteomyelitis
- Psoriatic arthritis
- Inflammatory bowel disease
- Leukemia
- Caffey Disease
- Chronic Eosinophilic Granuloma
- Osteoporosis
- Involutional Osteoarthritis
References[edit | edit source]
- ↑ Rigante D, Bosco A, Esposito S. The Etiology of Juvenile Idiopathic Arthritis. Clin Rev Allergy Immunol. 2015 Oct;49(2):253-61.
- ↑ 2.0 2.1 2.2 2.3 Zaripova LN, Midgley A, Christmas SE, Beresford MW, Baildam EM, Oldershaw RA. Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches. Pediatr Rheumatol Online J. 2021 Aug 23;19(1):135.
- ↑ Moore TL. Immune complexes in juvenile idiopathic arthritis. Frontiers in immunology. 2016 May 20;7:177.Available:https://www.frontiersin.org/articles/10.3389/fimmu.2016.00177/full (accessed 18.10.2021)
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 Thatayatikom A, Modica R, De Leucio A. Juvenile Idiopathic Arthritis. [Updated 2023 Jan 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554605/
- ↑ 5.0 5.1 5.2 5.3 5.4 Al-Mayouf SM, Al Mutairi M, Bouayed K, Habjoka S, Hadef D, Lotfy HM, Scott C, Sharif EM, Tahoun N. Epidemiology and demographics of juvenile idiopathic arthritis in Africa and Middle East. Pediatr Rheumatol Online J. 2021 Dec 2;19(1):166.
- ↑ França CMP, Sallum AM, Silva CAA, Aikawa NE, Braga AL, Farhat SC. Risk factors for juvenile idiopathic arthritis: exposure to tobacco and environmental factors during and before pregnancy. Pediatr Rheumatol Online J. 2014 Sep 17;12(Suppl 1):P27.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 better Health Juvenile Arthritis Available: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile(accessed 18.10.2021)
- ↑ National Institute of Arthritis and Musculoskeletal and Skin Diseases. Juvenile Idiopathic Arthritis (JIA) Basics. Available from: https://www.niams.nih.gov/health-topics/juvenile-arthritis/basics/symptoms-causes (last accessed 1 May 2023).
- ↑ Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. 3rd ed. . St. Louis, MO: Saunders, an imprint of Elsevier Inc, 2009.
- ↑ 10.0 10.1 Radiopedia JIA Available: https://radiopaedia.org/articles/juvenile-idiopathic-arthritis (accessed 18.10.2021)
- ↑ Hedrich CM, Günther C, Aringer M. Morbus Still im Kindes- und Erwachsenenalter [Still's disease in children and adults]. Z Rheumatol. 2017 Sep;76(7):595-608. German.
- ↑ 12.0 12.1 eMedicine. Disease fact sheet: juvenile rheumatoid arthritis. http://emedicine.medscape.com/article/409980-overview (accessed 10 March 2011)
- ↑ National Institute of Arthritis and Musculoskeletal and Skin Diseases. Health information: juvenile arthritis. http://www.niams.nih.gov/Health_Info/Juv_Arthritis/default.asp (accessed 10 March 2011)
- ↑ National Center for Biotechnology Information, U.S. National Library of Medicine. Disease fact sheet: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001487/ (10 March 2011)






