Hyperalgesia: Difference between revisions
No edit summary |
mNo edit summary |
||
| Line 9: | Line 9: | ||
IASP definition: | IASP definition: | ||
<blockquote>"Increased pain from a stimulus that normally provokes pain."<ref name=":0">IASP. Terminology. Available from: https://www.iasp-pain.org/resources/terminology/ (accessed 12 Dec 2023)</ref> </blockquote>Hyperalgesia is a clinical term used to described the phenomenon of an increased pain response to a painful stimuli (such as pin prick, pressure, extreme heat/cold). It does not imply a single pain mechanism, but is associated with [[Peripheral Sensitisation|peripheral sensitisation]] and [[Central Sensitisation|central sensitisation]].<ref name=":0" /> | <blockquote>"Increased pain from a stimulus that normally provokes pain."<ref name=":0">IASP. Terminology. Available from: https://www.iasp-pain.org/resources/terminology/ (accessed 12 Dec 2023)</ref> </blockquote>Hyperalgesia is a clinical term used to described the phenomenon of an increased pain response to a painful stimuli (such as pin prick, deep pressure, extreme heat/cold). It does not imply a single pain mechanism, but is associated with [[Peripheral Sensitisation|peripheral sensitisation]] and [[Central Sensitisation|central sensitisation]].<ref name=":0" /> | ||
Hyperalgesia is normal protective response after tissue damage and will usually subside as healing occurs.<ref name=":1">Sandkuhler J. [[Models and mechanisms of hyperalgesia and allodynia]]. Physiological reviews. 2009 Apr;89(2):707-58.</ref> It may however increase over time in certain conditions, such as [[Neuropathic Pain|neuropathic pain]] conditions | Hyperalgesia is normal protective response after tissue damage and will usually subside as healing occurs.<ref name=":1">Sandkuhler J. [[Models and mechanisms of hyperalgesia and allodynia]]. Physiological reviews. 2009 Apr;89(2):707-58.</ref> It may however increase over time in certain conditions, such as [[Neuropathic Pain|neuropathic pain]] conditions, and may be present in the absence of tissue injury. | ||
==Aetiology/Mechanism== | ==Aetiology/Mechanism== | ||
Hyperalgesia may involve a reduction in nociceptive firing threshold, and an increase in the supra-threshold response.<ref name=":1" />The end result is amplified nociception and an increase in pain intensity. | Hyperalgesia may involve a reduction in nociceptive firing threshold, and an increase in the supra-threshold response.<ref name=":1" />The end result is amplified [[nociception]] and an increase in pain intensity. | ||
* '''Primary Hyperalgesia:''' Hyperalgesia that occurs at the site of injury and is often a reflection of [[Peripheral Sensitisation|peripheral sensitisation]]. It occurs as a result of reduced activation threshold and increased responsiveness of nociceptors.<ref name=":1" /> | * '''Primary Hyperalgesia:''' Hyperalgesia that occurs at the site of injury and is often a reflection of [[Peripheral Sensitisation|peripheral sensitisation]]. It occurs as a result of reduced activation threshold and increased responsiveness of nociceptors (A-delta and C-fibres).<ref name=":1" /> | ||
* '''Secondary Hyperalgesia:''' Hyperalgesia in an area adjacent to or remote from the site of injury.<ref name=":1" />Maintained by changes in the central processing of sensory information, including sensitisation of the spinal nociceptive neurons and altered descending inhibition.<ref name=":1" /> | * '''Secondary Hyperalgesia:''' Hyperalgesia in an area adjacent to or remote from the site of injury.<ref name=":1" />Maintained by changes in the central processing of sensory information, including sensitisation of the spinal nociceptive neurons and altered descending inhibition.<ref name=":1" /> | ||
It is important to remember, that in acute injuries, the finding of hyperalgesia is a normal adaptive response. Since the injured tissue is vulnerable, the nociceptive system adapts by becoming sensitised to ensure tissue protection.<ref name=":1" />In such a case hyperalgesia would be an appropriate shift in pain threshold. It is however possible for this normal response to be exaggerated and does not always reflect the severity of an injury. | It is important to remember, that in acute injuries, the finding of hyperalgesia is a normal adaptive response. Since the injured tissue is vulnerable, the nociceptive system adapts by becoming sensitised to ensure tissue protection.<ref name=":1" />In such a case hyperalgesia would be an appropriate shift in pain threshold. It is however possible for this normal response to be exaggerated and does not always reflect the severity of an injury. | ||
If hyperalgesia does however occur long after tissue healing has occurred or in the absence of damaged tissue, it is considered maladaptive. | If hyperalgesia does however occur long after tissue healing has occurred or in the absence of damaged tissue, it is considered maladaptive. | ||
=== Nerve Sensitisation === | |||
As mentioned above, hyperalgesia occurs as a result of nociceptive sensitisation. The following mechanisms cause nerve sensitisation<ref name=":2">Train Pain Academy. Principles of Pain (Module 1) - handout. 2017.</ref>: | |||
* [[Neurogenic Inflammation]]: Peripheral nociceptors participate in the inflammatory process by releasing neuropeptides (like Substance P) | |||
* Inflammatory mediators (histamine, prostaglandin, bradykinin) | |||
* Change in pH associated with inflammation | |||
=== Risk Factors === | === Risk Factors === | ||
| Line 28: | Line 33: | ||
* '''Diet:''' There is some evidence from animal studies that a diet rich in omega-3 is associated with stronger heat hyperalgesia.<ref name=":1" /> | * '''Diet:''' There is some evidence from animal studies that a diet rich in omega-3 is associated with stronger heat hyperalgesia.<ref name=":1" /> | ||
* '''Anxiety and chronic stress:''' A sustained stated of stress may enhance pain sensitivity.<ref name=":1" /> | * '''Anxiety and chronic stress:''' A sustained stated of stress may enhance pain sensitivity.<ref name=":1" /> | ||
* Chronic Inflammation: Excess fat results in chronic release of inflammatory mediators | * '''Chronic [[Inflammation Acute and Chronic|Inflammation]]:''' Excess fat results in chronic release of inflammatory mediators | ||
* '''Immune response:''' When an injury occurs while the immune system is active (eg. fighting an acquired infection), exaggerated hyperalgesia is more likely since nociceptors are already sensitised<ref name=":2" /> | |||
* '''Stress:''' Pain pathways are modulated by stress, and exposure to chronic stress can produce maladaptive changes in pain processing leading to stress-induced hyperalgesia. <ref>Jennings EM, Okine BN, Roche M, Finn DP. [https://aran.library.nuigalway.ie/bitstream/handle/10379/15079/Manuscript_text_Combined_Files.pdf Stress-induced hyperalgesia.] Progress in neurobiology. 2014 Oct 1;121:1-8.</ref> | |||
* '''[[Opioids|Opioid]] use:''' Opioid-induced hyperalgesia occurs when opioids paradoxically enhance pain. This can occur with acute or chronic exposure to opioids. [[Opioid Use Disorder|Opioid tolerance]] and withdrawal can also affect pain sensitivity as it affects descending pain modulation. <ref>Wilson SH, Hellman KM, James D, Adler AC, Chandrakantan A. [[Mechanisms, diagnosis, prevention and management of perioperative opioid-induced hyperalgesia.]] Pain Management. 2021 Jul;11(4):405-17.</ref> | |||
== Conditions == | == Conditions == | ||
Listed below are some conditions that may present with hyperalgesia: | |||
* [[/www.physio-pedia.com/Neuropathic Pain|Neuropathic Pain]]: primary and secondary hyperalgesia<ref name=":3">Arendt‐Nielsen L, Morlion B, Perrot S, Dahan A, Dickenson A, Kress HG, Wells C, Bouhassira D, Drewes AM. Assessment and manifestation of central sensitisation across different chronic pain conditions. European Journal of Pain. 2018 Feb;22(2):216-41.</ref> | |||
* Postherpetic Neuralgia: primary hyperalgesia<ref name=":3" /> | |||
* [[/www.physio-pedia.com/Neuropathies|Neuropathies]] | |||
* Polyneuropathy such as [[/www.physio-pedia.com/HIV-related Neuropathy|HIV-related Neuropathy]] and Diabetic Neuropathy | |||
* [[/www.physio-pedia.com/Brachial Plexus Injury|Brachial Plexus Injury]] | |||
* Fibromyalgia<ref name=":4">Jensen TS, Finnerup NB. A[[/www.sciencedirect.com/science/article/pii/S1474442214701024|llodynia and hyperalgesia in neuropathic pain: clinical manifestations and mechanisms.]] The Lancet Neurology. 2014 Sep 1;13(9):924-35.</ref> | |||
* [[Irritable Bowel Syndrome]]<ref name=":3" /> | |||
* [[/www.physio-pedia.com/Chemotherapy-Induced Peripheral Neuropathy (CIPN)|Chemotherapy induced peripheral neuropathy]] | |||
* [[/www.physio-pedia.com/Central Sensitisation|Central Sensitisation]] | |||
* [[/www.physio-pedia.com/Peripheral Sensitisation|Peripheral Sensitisation]] | |||
* [[/www.physio-pedia.com/Complex Regional Pain Syndrome (CRPS)|Complex Regional Pain Syndrome (CRPS)]] | |||
* [[/www.physio-pedia.com/Chronic Low Back Pain|Chronic Low Back Pain]]<ref name=":3" /> | |||
* [[/www.physio-pedia.com/Osteoarthritis|Osteoarthritis]]<ref name=":3" /> | |||
* [[/www.physio-pedia.com/Rheumatoid Arthritis|Rheumatoid Arthritis]] | |||
* [[/www.physio-pedia.com/Amputation Pain Rehabilitation|Post-amputation stump pain]] | |||
* Central nervous system disorders: [[/www.physio-pedia.com/Post-Stroke Pain|Post-stroke pain]], [[/www.physio-pedia.com/Multiple Sclerosis (MS)|Multiple Sclerosis]], [[/www.physio-pedia.com/Spinal Cord Injury|Spinal Cord Injury]]<ref name=":4" /> | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
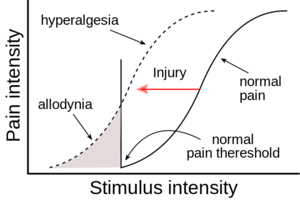
Another clinical term that needs to be differentiated from hyperalgesia, is [[allodynia]]. Where hyperalgesia refers to changes in the '''intensity''' of the sensation of pain, allodynia refers to changes in the '''quality''' of sensation. | |||
[[File:Allodynia.png|thumb|Hyperalgesia vs Allodynia]] | |||
Allodynia occurs when non-nociceptive afferents become sensitised, which results in non-painful stimuli becoming painful. Hyperalgesia involves sensitisation of nociceptors altering the intensity of pain for given painful stimulus. | |||
Although allodynia and hyperalgesia are distinct clinical terms, they can and often do co-exist. | |||
==Assessment== | ==Assessment== | ||
Hyperalgesia to various painful stimuli can be assessed, and forms part of [[Quantitative Sensory Testing (QST)|Quantitative Sensory Testing]] (QST). | Hyperalgesia to various painful stimuli can be assessed, and forms part of [[Quantitative Sensory Testing (QST)|Quantitative Sensory Testing]] (QST). QST is a way to evaluate the excitability of different pain pathways and involves a variety stimuli as part of the assessment.<ref name=":3" /> | ||
Hyperalgesia is regarded as the positive sensory sign of nociception. | |||
* Always compare to the unaffected side or a body site distant from the affected area (especially if there is bilateral involvement) | |||
== Treatment == | == Treatment == | ||
'''Acute injuries''' | '''Acute injuries''' | ||
* The focus is to minimise the development of sustained hyperalgesia | * The focus is to minimise the development of sustained/chronic hyperalgesia. Pain needs to be addressed early to prevent ongoing nociception | ||
'''Chronic pain''' | '''Chronic pain''' | ||
== | ==Conclusion== | ||
Hyperalgesia is a phenomenon that is continually being research and interpretation of this clinical sign may change as research evolves. | |||
==References== | ==References== | ||
<references /> | <references /> | ||
[[Category:Conditions]] | |||
[[Category:Pain]] | |||
[[Category:Neuropathy]] | |||
Revision as of 15:03, 20 December 2023
Original Editor - User Name
Top Contributors - Melissa Coetsee, Kim Jackson, Vidya Acharya and Carina Therese Magtibay
Introduction[edit | edit source]
IASP definition:
"Increased pain from a stimulus that normally provokes pain."[1]
Hyperalgesia is a clinical term used to described the phenomenon of an increased pain response to a painful stimuli (such as pin prick, deep pressure, extreme heat/cold). It does not imply a single pain mechanism, but is associated with peripheral sensitisation and central sensitisation.[1]
Hyperalgesia is normal protective response after tissue damage and will usually subside as healing occurs.[2] It may however increase over time in certain conditions, such as neuropathic pain conditions, and may be present in the absence of tissue injury.
Aetiology/Mechanism[edit | edit source]
Hyperalgesia may involve a reduction in nociceptive firing threshold, and an increase in the supra-threshold response.[2]The end result is amplified nociception and an increase in pain intensity.
- Primary Hyperalgesia: Hyperalgesia that occurs at the site of injury and is often a reflection of peripheral sensitisation. It occurs as a result of reduced activation threshold and increased responsiveness of nociceptors (A-delta and C-fibres).[2]
- Secondary Hyperalgesia: Hyperalgesia in an area adjacent to or remote from the site of injury.[2]Maintained by changes in the central processing of sensory information, including sensitisation of the spinal nociceptive neurons and altered descending inhibition.[2]
It is important to remember, that in acute injuries, the finding of hyperalgesia is a normal adaptive response. Since the injured tissue is vulnerable, the nociceptive system adapts by becoming sensitised to ensure tissue protection.[2]In such a case hyperalgesia would be an appropriate shift in pain threshold. It is however possible for this normal response to be exaggerated and does not always reflect the severity of an injury.
If hyperalgesia does however occur long after tissue healing has occurred or in the absence of damaged tissue, it is considered maladaptive.
Nerve Sensitisation[edit | edit source]
As mentioned above, hyperalgesia occurs as a result of nociceptive sensitisation. The following mechanisms cause nerve sensitisation[3]:
- Neurogenic Inflammation: Peripheral nociceptors participate in the inflammatory process by releasing neuropeptides (like Substance P)
- Inflammatory mediators (histamine, prostaglandin, bradykinin)
- Change in pH associated with inflammation
Risk Factors[edit | edit source]
The following factors may increase the risk of maladaptive hyperalgesia:
- Diet: There is some evidence from animal studies that a diet rich in omega-3 is associated with stronger heat hyperalgesia.[2]
- Anxiety and chronic stress: A sustained stated of stress may enhance pain sensitivity.[2]
- Chronic Inflammation: Excess fat results in chronic release of inflammatory mediators
- Immune response: When an injury occurs while the immune system is active (eg. fighting an acquired infection), exaggerated hyperalgesia is more likely since nociceptors are already sensitised[3]
- Stress: Pain pathways are modulated by stress, and exposure to chronic stress can produce maladaptive changes in pain processing leading to stress-induced hyperalgesia. [4]
- Opioid use: Opioid-induced hyperalgesia occurs when opioids paradoxically enhance pain. This can occur with acute or chronic exposure to opioids. Opioid tolerance and withdrawal can also affect pain sensitivity as it affects descending pain modulation. [5]
Conditions[edit | edit source]
Listed below are some conditions that may present with hyperalgesia:
- Neuropathic Pain: primary and secondary hyperalgesia[6]
- Postherpetic Neuralgia: primary hyperalgesia[6]
- Neuropathies
- Polyneuropathy such as HIV-related Neuropathy and Diabetic Neuropathy
- Brachial Plexus Injury
- Fibromyalgia[7]
- Irritable Bowel Syndrome[6]
- Chemotherapy induced peripheral neuropathy
- Central Sensitisation
- Peripheral Sensitisation
- Complex Regional Pain Syndrome (CRPS)
- Chronic Low Back Pain[6]
- Osteoarthritis[6]
- Rheumatoid Arthritis
- Post-amputation stump pain
- Central nervous system disorders: Post-stroke pain, Multiple Sclerosis, Spinal Cord Injury[7]
Differential Diagnosis[edit | edit source]
Another clinical term that needs to be differentiated from hyperalgesia, is allodynia. Where hyperalgesia refers to changes in the intensity of the sensation of pain, allodynia refers to changes in the quality of sensation.
Allodynia occurs when non-nociceptive afferents become sensitised, which results in non-painful stimuli becoming painful. Hyperalgesia involves sensitisation of nociceptors altering the intensity of pain for given painful stimulus.
Although allodynia and hyperalgesia are distinct clinical terms, they can and often do co-exist.
Assessment[edit | edit source]
Hyperalgesia to various painful stimuli can be assessed, and forms part of Quantitative Sensory Testing (QST). QST is a way to evaluate the excitability of different pain pathways and involves a variety stimuli as part of the assessment.[6]
Hyperalgesia is regarded as the positive sensory sign of nociception.
- Always compare to the unaffected side or a body site distant from the affected area (especially if there is bilateral involvement)
Treatment[edit | edit source]
Acute injuries
- The focus is to minimise the development of sustained/chronic hyperalgesia. Pain needs to be addressed early to prevent ongoing nociception
Chronic pain
Conclusion[edit | edit source]
Hyperalgesia is a phenomenon that is continually being research and interpretation of this clinical sign may change as research evolves.
References[edit | edit source]
- ↑ 1.0 1.1 IASP. Terminology. Available from: https://www.iasp-pain.org/resources/terminology/ (accessed 12 Dec 2023)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Sandkuhler J. Models and mechanisms of hyperalgesia and allodynia. Physiological reviews. 2009 Apr;89(2):707-58.
- ↑ 3.0 3.1 Train Pain Academy. Principles of Pain (Module 1) - handout. 2017.
- ↑ Jennings EM, Okine BN, Roche M, Finn DP. Stress-induced hyperalgesia. Progress in neurobiology. 2014 Oct 1;121:1-8.
- ↑ Wilson SH, Hellman KM, James D, Adler AC, Chandrakantan A. Mechanisms, diagnosis, prevention and management of perioperative opioid-induced hyperalgesia. Pain Management. 2021 Jul;11(4):405-17.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Arendt‐Nielsen L, Morlion B, Perrot S, Dahan A, Dickenson A, Kress HG, Wells C, Bouhassira D, Drewes AM. Assessment and manifestation of central sensitisation across different chronic pain conditions. European Journal of Pain. 2018 Feb;22(2):216-41.
- ↑ 7.0 7.1 Jensen TS, Finnerup NB. Allodynia and hyperalgesia in neuropathic pain: clinical manifestations and mechanisms. The Lancet Neurology. 2014 Sep 1;13(9):924-35.