Hemiplegia
Introduction[edit | edit source]
Hemiplegia is paralysis of the muscles of the lower face, arm, and leg on one side of the body. In addition to motor problems other losses may occur eg.sensation, memory, cognition. The most common cause of hemiplegia is stroke, which damages the corticospinal tracts in one hemisphere of the brain. Other causes of hemiplegia include trauma eg. spinal cord injury; brain tumours; and brain infections.
Hemiplegia is treated by addressing the underlying cause and by various forms of therapy to recover motor function. In particular, motor function in a hemiparetic limb may be improved with physical therapy and with mirror therapy. [1]
Hemiplegia is often used interchangeably with hemiparesis as both produce similar symptoms. An individual living with hemiparesis experiences a weak paralysis on one side of the body, while hemiplegia may cause the person to experience full paralysis on one side of their body, as well as difficulty breathing or speaking.[2]
Etiology[edit | edit source]
- Vascular - Cerebral hemorrhage , Stroke , Diabetic Neuropathy.
- Infective - Encephalitis , Meningitis , Brain abscess.
- Neoplastic - Glioma - meningioma
- Traumatic - Cerebral lacerations , Subdural Hematoma . Rare cause of hemiplegia is due to local anaesthesia injections given intra arterially rapidly , instead of given in a nerve branch .
- Congenital- Cerebral palsy
- Disseminated - Multiple Sclerosis
- Psychological - Parasomnia (Nocturnal hemiplegia).[3]
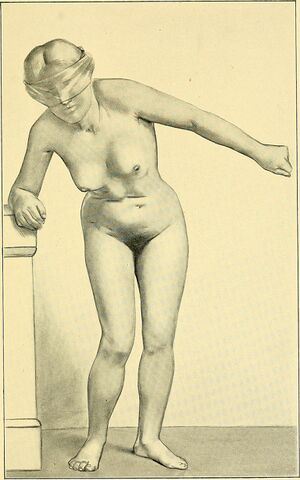
Signs and Symptoms of Hemiplegia[edit | edit source]
Symptoms of hemiplegia range from one person to another and are dependent on the severity of the condition. Symptoms of hemiplegia include:
- Impaired motor skills
- Difficulty grasping or holding on to objects
- Weakness of muscles or stiffness on one side of the body
- Permanently contracted muscles or muscle spasticity
- Poor balance
- Difficulty walking[2]
Treatment[edit | edit source]
People living with hemiplegia usually undergo a combination of rehabilitation therapy, which typically involves physical therapists, mental health professionals, and rehabilitation therapists.[2]
Physiotherapy Approaches[edit | edit source]
a. Conventional therapies (Therapeutic Exercises,Traditional Functional Retraining)
- Range Of Motion (ROM) Exercises
- Muscle Strengthening Exercises
- Mobilization activities
- Fitness training
- Compensatory Techniques
b. Neurophysiological Approaches:
1. Muscle Re-education Approach.
2. Neurodevelopmental Approaches :Neurology Treatment Techniques
- Sensorimotor Approach (Rood, 1940S)
- Movement Therapy Approach (Brunnstrom, 1950S)
- NDT Approach (Bobath, 1960-70S)
- PNF Approach (Knot and Voss,1960-70S)
3. Motor Relearning Program for Stroke (1980S)
4. Contemporary Task Oriented Approach (1990S)
Posture : Primary focus, Potential Treatment, Benefits , Activities[4][edit | edit source]
| Posture/description | Primary focus/benefits/activities |
|---|---|
| Prone on elbow
Prone ,weight bearing on elbows Stable posture Wide BOS Low COM |
Focus on improving upper trunk, UE and neck/head control
Improve ROM in hip extension Improve shoulder stabilizers Activities in posture : holding , weight shifting , UE reaching , assumption of posture Modified prone on elbows can be achieved in sitting and plantigrade positions |
| Quadruped
All four positions (hands and knees) Weight bearing at knees through extended elbows and hands Stable posture Wide BOS Low COM |
Focus on improving trunk , LE , UE and neck/head control
Improve trunk , hip , shoulder and elbow stabilizers Decrease extensor tone at knees by prolonged weight bearing Decrease flexor tone at wrist , elbows and hands by prolonged weightbearing Promote extensor ROM at elbows, wrist and fingers Lead up for I plantigrade activities , floor to standing transfers , antigravity balance control Activities in posture : holding , weight shifting , UE reaching , LE lifts , assumption of posture , locomotion on all fours. |
| Bridging
Weight bearing at feet and ankles , upper trunk Stable posture Wide BOS Low COM |
Focus on improving lower trunk and LE control
Improve hip and ankle stratergies Weight bearing at feet and ankles Lead up for bed mobility , sit to stand transfers , standing and stair climbing Activities in posture : holding weight shifting , assumption of postures , LE lifts |
| Sitting
Weight bearing through trunk and at buttocks , feet Can include weightbearing through extended elbows and on hands Intermediate BOS Intermediate height COM |
Focus on improving upper trunk , lower trunk , LE and head/neck control
Important for upright balance control Lead up for UE ADL skills ; wheelchair locomotion Activities in posture : holding , weight shifting , UE reaching , assumption of posture |
| Kneeling and half kneeling | Focus on improving upper trunk , lower trunk , LE and head/neck control
Weightbearing through hips and at knees ; upright antigrade postion Decrease extensor tone at knee by prolonged weightbearing Improve hip and trunk stabilizers Weightbearing through ankle in half kneeling Lead up for upright balance control , standing and stepping , floor to standing transfers Activities in posture ; holding , weight shifting , UE reaching ,assumption of posture , knee walking |
| Modified plantigrade
Standing with weightbearing on hands through extended elbows (on support surface) and through trunk, LEs Modified upright antigravity position Stable posture Wide BOS High COM |
• Focus on improving head/neck, trunk, and UE/LE control in supported, modified upright posture • Decrease tone in elbow, wrist, and finger flexors by prolonged weightbearing • Increase extensor ROM at elbows, wrists, and fingers • Hips flexed, COM forward of weight bearing line creating an extension moment at the knee • Increased safety for early standing (four-limb posture) • Lead-up for upright balance control, standing and stepping; standing UE ADL tasks • Activities in posture: holding, weight shifting, UE reaching, LE stepping, assumption of posture |
| Standing
Weightbearing through trunk and LEs Full upright, antigravity position Narrow BOS High COM |
• Focus on improving head/neck, trunk, and LE control in
fully upright posture • Hips and knees fully extended • Lead-up for upright balance control, stepping, locomotion, stair climbing; standing UE ADL skills • Activities in posture: holding, weight shifting, UE reaching, LE stepping, assumption of posture |
Programming variables[edit | edit source]
- Duration: The overall duration of the session will be one hour. The total duration of the aerobic/cardiac exercise training should increase from 15 minutes (week one) to 40 minutes by week 12.
- Intensity: The intensity of exercise should aim to be moderate as opposed to low. This effort level is required for all components but will be adjusted for each individual according to health status on a session-by-session basis.
- Frequency: The frequency of the session should be three times per week wherever possible[5].
Functional electrical stimulation (FES)[edit | edit source]
- FES is a modality that applied a short burst of electrical current to the hemiplegic muscle or nerve.
- In Hemiplegia Physical Therapy, FES has been demonstrated to be beneficial to restore motor control, spasticity, and reduction of hemiplegic shoulder pain and subluxation. It is concluded that FES can enhance the upper extremity motor recovery of acute stroke patient.
- FES could reduce spasticity in stroke patient. A recent meta- analysis of randomized controlled trial study showed that FES improves motor strength.
- FES can significantly improve arm function, electromygraphic activity of posterior deltoid, range of motion and reduction of severity of subluxation and pain of hemiplegic shoulder.
Biofeedback[edit | edit source]
- Biofeedback is a modality that facilitates the cognizant of electromyographic activity in selected muscle or awareness of joint position sense via visual or auditory cues. In Hemiplegia Physical Therapy the result of studies in biofeedback is controversial.
- A meta-analysis of 8 randomized controlled trials of biofeedback therapy demonstrated that electromyographic biofeedback could improve motor function in hemiplegic patient.
- Another meta-analysis study on EMG has showed that EMG biofeedbcak is superior to conventional therapy alone for improving ankle dorsiflexion muscle strengthbshowed that biofeedback could improve earlier postural control to improve impaired sitting balance.
Conventional gait training[edit | edit source]
Conventional gait training has focused on part-practice of components of gait in preparation for walking. It includes
- Symetrical Weight bearing training
- Weight shifting
- Stepping training (swinging / clearance )
- Heel strike
- Single leg standing
- Push off / Calf rise. Followed by,
Circuit training (reaching in sitting and standing, sit-to-stand, step-ups, heel lifts, isokinetic strengthening, walking over obstacles, up and down slopes).
Traditional approaches to stroke recovery have a focus on neuro facilitation or neuro developmental techniques (NDT) to inhibit excessive tone, stimulate muscle activity if hypotonia is present and to facilitate normal movement patterns through hands-on techniques. Practice based on the framework advocated by Berta Bobath remains the predominant physical therapy approach to stroke patients in the UK and is also common in many other parts of the world, including Canada, United States, Europe, Australia, Hong Kong and Taiwan. The Bobath framework has evolved from its original foundations, however, therapists surveyed on the core Bobath elements still emphasize normal tone and the necessity of normal movement patterns to perform functional tasks. Strength training to improve walking ability Task-specific training to improve walking ability.
References[edit | edit source]
- ↑ Btiannica Hemiparesis Available:https://www.britannica.com/science/hemiplegia (accessed 19.8.2021)
- ↑ 2.0 2.1 2.2 Hemiplegia – Types, Causes, Symptoms and Treatmentt Available:https://healthtian.com/hemiplegia/ (accessed 19.8.2021)
- ↑ Hemiplegia Dr. V.S.Nandakumarhttps://www.slideshare.net/danny14871/hemiplegia-43636165 (accessed 29 June 2018)
- ↑ O'Sullivan SB, Schmitz TJ. Improving functional outcomes in physical rehabilitation. FA Davis; 2016 Feb 17.
- ↑ Best C, van Wijck F, Dinan-Young S, Dennis J, Smith M, Fraser H, Donaghy M, Mead G. Exercise after Stroke Services.(accessed 29 June 2018)