Fat Pad Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| (39 intermediate revisions by 10 users not shown) | |||
| Line 2: | Line 2: | ||
'''Original Editor '''- [[User:Mariam Hashem|Mariam Hashem]] | '''Original Editor '''- [[User:Mariam Hashem|Mariam Hashem]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} <br> | ||
</div> | </div> | ||
== | == Introduction== | ||
Infrapatellar | Acute or chronic inflammation of the Infrapatellar Fat Pad (IFP) is a common source of [[Anterior Knee Pain]]; also called Hoffa's disease, fat pad syndrome or hoffitis. Fat pad syndrome was firstly reported by Albert Hoffa in 1904 <ref name=":5">Larbi A, Cyteval C, Hamoui M, Dallaudiere B, Zarqane H, Viala P. et al. Hoffa's disease: A report on 5 cases. Diagnostic and interventional imaging. 2014;95(11):1079-84.</ref>. | ||
== Anatomy/Biomechanics== | |||
The IFP is found in the anterior [[knee]] compartment as a mass of adipose tissue that lies '''intracapsular but is extra synovial (extra-articular)'''<ref name=":5" />'''.''' The IFP distributes pressure across the patellofemoral joint, facilitates flexible deformation in the knee joint and supports patellar stability.<ref>Kitagawa T, Ozaki N, Aoki Y. [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0265333 Effect of physical therapy on the flexibility of the infrapatellar fat pad: A single-blind randomised controlled trial.] PloS one. 2022 Mar 17;17(3):e0265333.</ref>. In addition, the IFP may have a role as a mechoreceptor/proprioceptor due to the relatively high density of nerves within it. <ref>Leese J, Davies DC. [https://onlinelibrary.wiley.com/doi/full/10.1111/joa.13177 An investigation of the anatomy of the infrapatellar fat pad and its possible involvement in anterior pain syndrome: a cadaveric study]. Journal of Anatomy. 2020 Jul;237(1):20-8.</ref><ref>Edama M, Otsuki T, Yokota H, Hirabayashi R, Sekine C, Maruyama S, Kageyama I. [https://www.nature.com/articles/s41598-022-12859-1 Morphological characteristics of the infrapatellar fat pad]. Scientific Reports. 2022 May 27;12(1):1-9.</ref> | |||
<u>'''Boundaries:'''</u> | <u>'''Boundaries:'''</u> | ||
* Superiorly by the inferior pole of the patella | * Superiorly by the inferior pole of the patella and alar folds<ref name=":5" />. | ||
* Inferiorly by the anterior tibia, intermeniscal ligament, meniscal horns and infrapatellar bursa, | * Inferiorly by the anterior tibia, intermeniscal ligament, meniscal horns and infrapatellar bursa<ref name=":0">Mace J, Bhatti W, Anand S. Infrapatellar fat pad syndrome: a review of anatomy, function, treatment and dynamics. Acta Orthopaedica Belgica. 2016;82(1):94-101.</ref> | ||
* Anteriorly by the patellar tendon | * Anteriorly by the patellar tendon<ref name=":0" />, patellar ligament and joint capsule<ref name=":5" /> | ||
* Posteriorly by the femoral condyles | * Posteriorly by the femoral condyles, intercondylar notch<ref name=":0" /> and the synovial membrane<ref name=":5" />. | ||
'''<u>Attachments:</u>''' | '''<u>Attachments:</u>''' | ||
* The intercondylar notch via the ligamentum mucosum, | * The intercondylar notch via the ligamentum mucosum, | ||
* Anterior horns of the menisci | * Anterior horns of the menisci | ||
* The proximal end of the patella tendon | * The proximal end of the patella tendon | ||
* The inferior pole of the patella | * The inferior pole of the patella<ref name=":0" /> | ||
[[File:Infrapatellar Fat Pad Biomechanics.jpg|thumb]] | |||
Innervated mainly by the posterior tibial nerve,<ref>Macchi V, Stocco E, Stecco C, Belluzzi E, Favero M, Porzionato A et al. The infrapatellar fat pad and the synovial membrane: an anatomo-functional unit. J Anat. 2018;233(2):146-54. </ref> the IFP can be a source of both localised and severe knee [[Pain Behaviours|pain]]. This could be attributed to the presence of type VIa nerve endings<ref>Bohnsack M, Wilharm A, Hurschler C, Rühmann O, Stukenborg-Colsman C, Wirth CJ. Biomechanical and kinematic influences of a total infrapatellar fat pad resection on the knee. The American journal of sports medicine. 2004;32(8):1873-80.</ref> which could be activated through mechanical deformation or chemical pain mediators. Substance P-nerve fibers are also present in individuals with anterior knee pain, particularly when the infrapatellar fat pad is inflamed<ref>Bohnsack M, Meier F, Walter GF, Hurschler C, Schmolke S, Wirth CJ. et al. Distribution of substance-P nerves inside the infrapatellar fat pad and the adjacent synovial tissue: a neurohistological approach to anterior knee pain syndrome. Archives of orthopaedic and trauma surgery. 2005;125(9):592-7.</ref>. As a potential source of inflammation and pain, some authors considered the fat pad to be a key structure in [[Patellar Tendinopathy|patellar tendinopathy]]<ref>Culvenor AG, Cook JL, Warden SJ, Crossley KM. Infrapatellar fat pad size, but not patellar alignment, is associated with patellar tendinopathy. Scandinavian journal of medicine & science in sports. 2011;21(6):e405-11.</ref> and [[Knee Osteoarthritis|osteoarthritis]]<ref>Clockaerts S, Bastiaansen-Jenniskens YM, Runhaar J, Van Osch GJ, Van Offel JF, Verhaar JA. et al. The infrapatellar fat pad should be considered as an active osteoarthritic joint tissue: a narrative review. Osteoarthritis and Cartilage. 2010;18(7):876-82.</ref>[[Knee Osteoarthritis|.]] | |||
IFP | The IFP is a dynamic structure. It alters position, pressure, and volume throughout the knee ROM<ref name=":3" />. When the [[knee]] moves into flexion, the superolateral portion of the fat pad becomes relaxed, freely expansive and moves posteriorly. In extension, the IFP lies between the lateral patella facet and quadriceps tendon. Therefore, most commonly observed symptoms are associated with extension. However, it could also be seen in in flexion, where pain is provoked by the trapped IFP between the patella tendon and anterior femur<ref name=":0" />. | ||
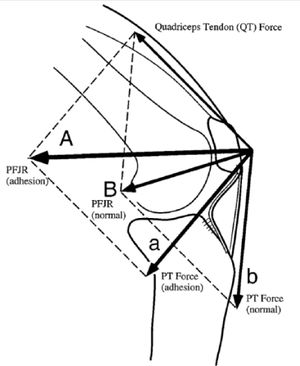
IFP facilitates gliding between the femoral condyles and joint capsule. Knee mechanics can be altered when there is adhesion in the fat pad that changes the position of the patella and patellar tendon. Consequently, the effectiveness of the extensor mechanism is compromised, decreasing the effective moment arm placing greater demands on the quadriceps to produce the same knee extension force. A shorter patellar tendon length affects patellar mobility and creates resistance to lateral translation at full extension<ref name=":3">Hannon J, Bardenett S, Singleton S, Garrison JC. Evaluation, Treatment, and Rehabilitation Implications of the Infrapatellar Fat Pad. Sports health. 2016;8(2):167-71.</ref>. | |||
A study showed reduced coordination between medial and [[Vastus Lateralis|lateral vastus muscle]] motor units in anterior knee pain<ref>Mellor R, Hodges PW. Motor unit syncronization is reduced in anterior knee pain. The Journal of pain. 2005;6(8):550-8.</ref>. Another reported a significantly later activation and reduced amplitude of contraction of quadriceps during stair stepping following injecting the fat pad with a painful hypertonic saline<ref>Hodges PW, Mellor R, Crossley K, Bennell K. Pain induced by injection of hypertonic saline into the infrapatellar fat pad and effect on coordination of the quadriceps muscles. Arthritis Care & Research. 2009;61(1):70-7.</ref>. The inhibited fat pad resulted in increased patellofemoral loading and reduced [[Quadriceps Muscle Contusion|quadriceps]] activation<ref name=":0" />. However, the exact association of fat pad and knee biomechanics needs further investigation. | |||
== | == Metabolic influence of the Infrapatellar fat pad== | ||
Early studies reported the fat pad to be a lubricant structure that facilitated the flow of synovial fluid inside the joint<ref name=":0" />. Subsequently it has become clear that the IFP yields more sophisticated functions due to its complex neurovascularity. | |||
== | The IFP is considered to be a producer of many inflammatory mediating substances found in association with OA.<ref>Jiang LF, Fang JH, Wu LD. [https://www.wjgnet.com/2307-8960/full/v7/i16/2134.htm Role of infrapatellar fat pad in pathological process of knee osteoarthritis: Future applications in treatment]. World Journal of Clinical Cases. 2019 Aug 8;7(16):2134.</ref> As an adipose tissue, IFP mainly secretes fatty acids which are well-known for their pro-inflammatory effects<ref name=":2">Ioan-Facsinay A, Kloppenburg M. An emerging player in knee osteoarthritis: the infrapatellar fat pad. Arthritis research & therapy. 2013;15(6):225.</ref>. Adipose tissue also stores immune cells, another potential source of inflammatory mediator substances<ref name=":2" />. In addition, a study showed that IFP actively secretes IL-6 and its soluble receptor sIL-6R, at relatively higher levels compared to other adipose tissues<ref>Distel E, Cadoudal T, Durant S, Poignard A, Chevalier X, Benelli C. The infrapatellar fat pad in knee osteoarthritis: An important source of interleukin‐6 and its soluble receptor. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology. 2009;60(11):3374-7.</ref>. | ||
IFP has been found to release mesenchymal stem cells with enhanced chondrogenic activity but this finding requires further investigations <ref name=":2" />. | |||
Regulation of glycosaminoglycan release<ref>Caspar-Bauguil S, Cousin B, Galinier A, Segafredo C, Nibbelink M, Andre M et al. Adipose tissues as an ancestral immune organ: site‐specific change in obesity. FEBS letters. 2005;579(17):3487-92.</ref>, a source of reparative cells<ref name=":3" />, release of pro-inflammatory cytokines associated with elevated BMI<ref>Dragoo JL, Samimi B, Zhu M, Hame SL, Thomas BJ, Lieberman JR, et al. Tissue-engineered cartilage and bone using stem cells from human infrapatellar fat pads. The Journal of bone and joint surgery. British volume. 2003;85(5):740-7.</ref> and collagen release<ref>Kim CS, Lee SC, Kim YM, Kim BS, Choi HS, Kawada T. et al. Visceral fat accumulation induced by a high‐fat diet causes the atrophy of mesenteric lymph nodes in obese mice. Obesity. 2008;16(6):1261-9.</ref> are also reported to be functions of IFP. | |||
Duran et al <ref>Duran S, Akşahin E, Kocadal O, Aktekin CN, Hapa O, Genctürk ZB. Effects of body mass index, infrapatellar fat pad volume and age on patellar cartilage defect. Orthopaedic journal of sports medicine. 2014;2(11_suppl3):2325967114S00159.</ref> studied the IFP volume and found it to be decreased in [[Patellar Fractures|patellar]] cartilage defect. | |||
== Pathophysiology/Clinical Picture == | |||
Little is known about the development of fat pad syndrome. The anatomical location of IFP exposes it to mechanical load, especially during extension<ref name=":5" />. Overuse or repeated micro trauma from sports or falls lead to hypertrophy. If the fat pad fails to recover it can become chronically inflamed which, if not properly managed, may result in fibrosis and ossification<ref name=":5" />. | |||
Predominantly seen in young women, jumping sports and ligamentous laxity are also considered to be risk factors for Hoffa's disease<ref name=":5" />. | |||
== Diagnosis/Physical Examination== | |||
The inflamed fat pad is often enlarged, firm in consistency and easy to palpate. '''Hoffa’s test''' can be performed. To avoid pain provocation in adjacent structures and incur false results, Krumar et al <ref name=":1">Kumar D, Alvand A, Beacon JP. Impingement of infrapatellar fat pad (Hoffa’s disease): results of high-portal arthroscopic resection. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2007;23(11):1180-6.</ref> suggested a modification of hoffa’s test. This involves taking the knee into passive forced hyperextension by lifting the heel and keeping anterior pressure on the tibia. This position stimulates pain exclusively in the fat pad, if it is inflamed<ref name=":0" />. | |||
{{#ev:youtube|kbu9nybRV0M}}<ref>Lenny Macrina. Fat Pad Assessment. Available from: https:https://www.youtube.com/watch?v=https://youtu.be/kbu9nybRV0M</ref> | |||
'''Gliding''' the patella in all four directions (medially, laterally, superiorly and inferiorly) is important to detect adhesion or movement restriction during knee movement, particularly in hyperextension. '''Pain in hyperextension is a strong indicator of the presence of inflamed IFP <ref name=":3" />.''' | |||
Examination should aim to exclude any other radiating pathologies particularly from spine and hip | Examination should also aim to exclude any other radiating pathologies particularly from spine and hip. | ||
=== Differentiation === | |||
Fat pad syndrome could be a primary disorder or secondary to other pathologies such as [[Meniscal Lesions|meniscus injuries]] and or ligamentous tear. Prevalence is not widely investigated, however, two studies reported isolated fat pad in 1% <ref name=":4">Ogilvie-Harris DJ, Giddens J. Hoffa's disease: arthroscopic resection of the infrapatellar fat pad. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 1994 ;10(2):184-7.</ref> of anterior knee pain cases and 6.8%<ref name=":1" /> as a secondary disorder. Synovitis and swelling of the fat pad were reported after anterior cruciate ligament (ACL) rupture<ref>Witoński D, Wągrowska-Danielewicz M. Distribution of substance-P nerve fibers in the knee joint in patients with anterior knee pain syndrome A preliminary report. Knee Surgery, Sports Traumatology, Arthroscopy. 1999;7(3):177-83.</ref>. | |||
A detailed history and findings on functional assessment are important to discriminate fat pad syndrome from other conditions such as : patellar lateral femoral friction syndrome, [[Plica Syndrome|impingement of the infrapatellar plica]] and arthrofibrosisor “cyclops syndrome”. [https://www.sciencedirect.com/science/article/pii/S2211568414002009#bib0035 Refer to the discussion in this article to learn about the characteristics of each condition.] | |||
Symptoms of fat pad syndrome are anterior knee pain,<ref>Genin J, Faour M, Ramkumar PN, Yakubek G, Khlopas A, Chughtai M et al. Infrapatellar Fat Pad Impingement: A Systematic Review. J Knee Surg. 2017;30(7):639-46. </ref> often retropatellar and infrapatellar. Patellofemoral crepitus might be present, with knee loading such as in stairs negotiation<ref name=":0" />, squatting, jumping and running<ref name=":3" />. Effusion and decreased ROM are often seen with inflamed IFP. | |||
Pain and/or discomfort from long walks, flat shoes and prolonged standing refer mostly to fat pad syndrome. Pain resulting from up or down hill walking is a characteristic of [[Patellofemoral Pain Syndrome|PFPS]]. | |||
{{#ev:youtube|eiwKkb1SulU}}<ref>Claire Patella. Infographic:Differentiating fat pad and pfj pain. Available from: https://youtu.be/eiwKkb1SulU</ref> | |||
== | === Imaging === | ||
[[MRI Scans|MRI]] is the best imaging technique in diagnosing IFP inflammation<ref name=":5" />. Edema of the superior/posterior fat pad, [[Bursitis|inflamed infrapatellar bursa]] are easily detected by magnetic resonance. However, it is recommended to refer the patient to MRI only to exclude any other pathologies , particularly when there is a history of trauma <ref name=":0" />. | |||
Dynamic sonographic assessment revealed superolateral fat pad impingement associated with association with a perceived [[Iliotibial Band Syndrome|tight Iliotibial band]]<ref name=":0" />. | |||
== Management == | |||
Conservative treatment that have been reported to relieve symptoms include taping, physiotherapy, non-steroidal anti-inflammatory drugs, injections of local anesthetics and/or corticosteroids. When these interventions are not effective, surgery may be the next step.<ref>Kim YM, Joo YB. [http://www.jksrr.org/journal/view.html?doi=10.5792/ksrr.18.026 Arthroscopic treatment of infrapatellar fat pad impingement between the patella and femoral trochlea: comparison of the clinical outcomes of partial and subtotal resection]. Knee surgery & related research. 2019 Mar;31(1):54.</ref> | |||
= | Diagnostic and therapeutic injections of local anesthetics and steroid into the fat pad resulted in immediate pain relief and reconstruction of movement<ref name=":0" />. | ||
Arthroscopic resection In two studies resulted in improvements on both [http://fysio.net/pdf/Knie%20Cincinatti%20Knee%20Rating%20System.pdf Cincinnati rating System] and [http://www.lakarhuset.com/docs/lysholmkneescoringscale.pdf Lysholm knee score]<ref name=":4" /><ref name=":1" />. | |||
An average improvement of 4.83 on [[Visual Analogue Scale|VAS]] was reported following Ultrasound guided alcohol ablation by House and Connell<ref>House CV, Connell DA. Therapeutic ablation of the infrapatellar fat pad under ultrasound guidance: a pilot study. Clinical radiology. 2007;62(12):1198-201.</ref> | |||
[https://www.sciencedirect.com/science/article/pii/S2211568414002009#bib0035 Refer to the case reports in this article to learn about different management approaches.] | |||
=== Management of Acute Fat Pad Syndrome === | |||
* This usually occur as a result of falls, direct knee trauma or after knee surgeries resulting from arthroscopic equipment. | |||
* <u>Ice massage</u> is very useful to relief acute symptoms<ref name=":5" />. It could be followed by taping to alleviate pressure off the fat pad. | |||
* Flat foot wear should be avoided to minimize IFP loading. | |||
* Advice patient to avoid provocative activities till the acute symptoms resolve. | |||
{{#ev:youtube|6CRarRzStrU}}<ref>How to ice massage for knee tendonitis my Physio SA Adelaide Physiotherapist. Available from: | <div class="row"> | ||
<div class="col-md-6"> {{#ev:youtube|6CRarRzStrU|250}} <div class="text-right"><ref>How to ice massage for knee tendonitis my Physio SA Adelaide Physiotherapist. Available from: https://www.youtube.com/watch?v=6CRarRzStrU</ref></div></div> | |||
<div class="col-md-6">{{#ev:youtube|aE6-EGAFkfI|250}} <div class="text-right"><ref>Claire Patella. Ice-It-Away Instructions-Fat Pad Available from: https://www.youtube.com/watch?v=aE6-EGAFkfI</ref></div></div> | |||
</div> | |||
=== | <div class="row"> | ||
<div class="col-md-6"> {{#ev:youtube|Xy7CibqEUtQ|250}} <div class="text-right"><ref>Union Physical Therapy. McConnel fat pad taping. Available from: https://www.youtube.com/watch?v=Xy7CibqEUtQ</ref></div></div> | |||
<div class="col-md-6">{{#ev:youtube|WbHXYnwUwws|250}} <div class="text-right"><ref>McConnell Physiotherapy Group. MCCONNELL KNEE TAPING (OFFICIAL). Available from: https://youtu.be/WbHXYnwUwws</ref></div></div> | |||
</div> | |||
<div class="row"> | |||
<div class="col-md-6"> {{#ev:youtube|KR_peakgyi4|250}} <div class="text-right"><ref>Motion Guidance. infrapatellar fat pad mobilization. Available from: https://www.youtube.com/watch?v=KR_peakgyi4</ref></div></div> | |||
</div> | |||
=== Management of Chronic Fat Pad Syndrome === | |||
* Usually there is no history of trauma | |||
* Biomechanical abnormalities, such as excessive hyperextension, should be addressed to decrease IFP loading | |||
* To correct hyperextension, a relatively elevated shoe is advised | |||
* Movement awareness and education are important in this stage | |||
* Implement knee straightening exercises. | |||
* Quadriceps and anterior hip stretching is found to improve IFP restriction symptoms<ref>Dragoo JL, Johnson C, McConnell J. Evaluation and treatment of disorders of the infrapatellar fat pad. Sports medicine. 2012;42(1):51-67.</ref>. | |||
* There is a significant impact of high BMI and obesity on knee OA and fat pad syndrome. An 18-month RCT investigated the effect of a weight loss program (Exercise and/or diet) on the IFP. The study reported significant reduction in the IFP volume as a result of weigh loss and changes in body fat percentage, mostly achieved by combining exercise and diet<ref>Murillo AL, Eckstein F, Wirth W, Beavers D, Loeser RF, Nicklas BJ. et al. Impact of diet and/or exercise intervention on infrapatellar fat pad morphology: secondary analysis from the intensive diet and exercise for arthritis (IDEA) trial. Cells Tissues Organs. 2017;203(4):258-66.</ref>. | |||
{{#ev:youtube|xPouEzBmVJk}}<ref>Infrapatellar Fat Pad Knee Pain (Hoffa's Syndrome) Clinical Treatment - Dr Mandell. Available from: https://www.youtube.com/watch?v=xPouEzBmVJk</ref> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Knee - Conditions]] | |||
[[Category:Knee]] | |||
[[Category:Conditions]] | |||
[[Category:Course Pages]] | |||
[[Category:Plus Content]] | |||
Latest revision as of 16:06, 15 December 2022
Original Editor - Mariam Hashem
Top Contributors - Mariam Hashem, Tarina van der Stockt, Kim Jackson, Tony Lowe, Simisola Ajeyalemi, Uchechukwu Chukwuemeka, Wanda van Niekerk, Jess Bell, Marleen Moll, Robin Tacchetti and Rishika Babburu
Introduction[edit | edit source]
Acute or chronic inflammation of the Infrapatellar Fat Pad (IFP) is a common source of Anterior Knee Pain; also called Hoffa's disease, fat pad syndrome or hoffitis. Fat pad syndrome was firstly reported by Albert Hoffa in 1904 [1].
Anatomy/Biomechanics[edit | edit source]
The IFP is found in the anterior knee compartment as a mass of adipose tissue that lies intracapsular but is extra synovial (extra-articular)[1]. The IFP distributes pressure across the patellofemoral joint, facilitates flexible deformation in the knee joint and supports patellar stability.[2]. In addition, the IFP may have a role as a mechoreceptor/proprioceptor due to the relatively high density of nerves within it. [3][4]
Boundaries:
- Superiorly by the inferior pole of the patella and alar folds[1].
- Inferiorly by the anterior tibia, intermeniscal ligament, meniscal horns and infrapatellar bursa[5]
- Anteriorly by the patellar tendon[5], patellar ligament and joint capsule[1]
- Posteriorly by the femoral condyles, intercondylar notch[5] and the synovial membrane[1].
Attachments:
- The intercondylar notch via the ligamentum mucosum,
- Anterior horns of the menisci
- The proximal end of the patella tendon
- The inferior pole of the patella[5]
Innervated mainly by the posterior tibial nerve,[6] the IFP can be a source of both localised and severe knee pain. This could be attributed to the presence of type VIa nerve endings[7] which could be activated through mechanical deformation or chemical pain mediators. Substance P-nerve fibers are also present in individuals with anterior knee pain, particularly when the infrapatellar fat pad is inflamed[8]. As a potential source of inflammation and pain, some authors considered the fat pad to be a key structure in patellar tendinopathy[9] and osteoarthritis[10].
The IFP is a dynamic structure. It alters position, pressure, and volume throughout the knee ROM[11]. When the knee moves into flexion, the superolateral portion of the fat pad becomes relaxed, freely expansive and moves posteriorly. In extension, the IFP lies between the lateral patella facet and quadriceps tendon. Therefore, most commonly observed symptoms are associated with extension. However, it could also be seen in in flexion, where pain is provoked by the trapped IFP between the patella tendon and anterior femur[5].
IFP facilitates gliding between the femoral condyles and joint capsule. Knee mechanics can be altered when there is adhesion in the fat pad that changes the position of the patella and patellar tendon. Consequently, the effectiveness of the extensor mechanism is compromised, decreasing the effective moment arm placing greater demands on the quadriceps to produce the same knee extension force. A shorter patellar tendon length affects patellar mobility and creates resistance to lateral translation at full extension[11].
A study showed reduced coordination between medial and lateral vastus muscle motor units in anterior knee pain[12]. Another reported a significantly later activation and reduced amplitude of contraction of quadriceps during stair stepping following injecting the fat pad with a painful hypertonic saline[13]. The inhibited fat pad resulted in increased patellofemoral loading and reduced quadriceps activation[5]. However, the exact association of fat pad and knee biomechanics needs further investigation.
Metabolic influence of the Infrapatellar fat pad[edit | edit source]
Early studies reported the fat pad to be a lubricant structure that facilitated the flow of synovial fluid inside the joint[5]. Subsequently it has become clear that the IFP yields more sophisticated functions due to its complex neurovascularity.
The IFP is considered to be a producer of many inflammatory mediating substances found in association with OA.[14] As an adipose tissue, IFP mainly secretes fatty acids which are well-known for their pro-inflammatory effects[15]. Adipose tissue also stores immune cells, another potential source of inflammatory mediator substances[15]. In addition, a study showed that IFP actively secretes IL-6 and its soluble receptor sIL-6R, at relatively higher levels compared to other adipose tissues[16].
IFP has been found to release mesenchymal stem cells with enhanced chondrogenic activity but this finding requires further investigations [15].
Regulation of glycosaminoglycan release[17], a source of reparative cells[11], release of pro-inflammatory cytokines associated with elevated BMI[18] and collagen release[19] are also reported to be functions of IFP.
Duran et al [20] studied the IFP volume and found it to be decreased in patellar cartilage defect.
Pathophysiology/Clinical Picture[edit | edit source]
Little is known about the development of fat pad syndrome. The anatomical location of IFP exposes it to mechanical load, especially during extension[1]. Overuse or repeated micro trauma from sports or falls lead to hypertrophy. If the fat pad fails to recover it can become chronically inflamed which, if not properly managed, may result in fibrosis and ossification[1].
Predominantly seen in young women, jumping sports and ligamentous laxity are also considered to be risk factors for Hoffa's disease[1].
Diagnosis/Physical Examination[edit | edit source]
The inflamed fat pad is often enlarged, firm in consistency and easy to palpate. Hoffa’s test can be performed. To avoid pain provocation in adjacent structures and incur false results, Krumar et al [21] suggested a modification of hoffa’s test. This involves taking the knee into passive forced hyperextension by lifting the heel and keeping anterior pressure on the tibia. This position stimulates pain exclusively in the fat pad, if it is inflamed[5].
Gliding the patella in all four directions (medially, laterally, superiorly and inferiorly) is important to detect adhesion or movement restriction during knee movement, particularly in hyperextension. Pain in hyperextension is a strong indicator of the presence of inflamed IFP [11].
Examination should also aim to exclude any other radiating pathologies particularly from spine and hip.
Differentiation[edit | edit source]
Fat pad syndrome could be a primary disorder or secondary to other pathologies such as meniscus injuries and or ligamentous tear. Prevalence is not widely investigated, however, two studies reported isolated fat pad in 1% [23] of anterior knee pain cases and 6.8%[21] as a secondary disorder. Synovitis and swelling of the fat pad were reported after anterior cruciate ligament (ACL) rupture[24].
A detailed history and findings on functional assessment are important to discriminate fat pad syndrome from other conditions such as : patellar lateral femoral friction syndrome, impingement of the infrapatellar plica and arthrofibrosisor “cyclops syndrome”. Refer to the discussion in this article to learn about the characteristics of each condition.
Symptoms of fat pad syndrome are anterior knee pain,[25] often retropatellar and infrapatellar. Patellofemoral crepitus might be present, with knee loading such as in stairs negotiation[5], squatting, jumping and running[11]. Effusion and decreased ROM are often seen with inflamed IFP.
Pain and/or discomfort from long walks, flat shoes and prolonged standing refer mostly to fat pad syndrome. Pain resulting from up or down hill walking is a characteristic of PFPS.
Imaging[edit | edit source]
MRI is the best imaging technique in diagnosing IFP inflammation[1]. Edema of the superior/posterior fat pad, inflamed infrapatellar bursa are easily detected by magnetic resonance. However, it is recommended to refer the patient to MRI only to exclude any other pathologies , particularly when there is a history of trauma [5].
Dynamic sonographic assessment revealed superolateral fat pad impingement associated with association with a perceived tight Iliotibial band[5].
Management[edit | edit source]
Conservative treatment that have been reported to relieve symptoms include taping, physiotherapy, non-steroidal anti-inflammatory drugs, injections of local anesthetics and/or corticosteroids. When these interventions are not effective, surgery may be the next step.[27]
Diagnostic and therapeutic injections of local anesthetics and steroid into the fat pad resulted in immediate pain relief and reconstruction of movement[5].
Arthroscopic resection In two studies resulted in improvements on both Cincinnati rating System and Lysholm knee score[23][21].
An average improvement of 4.83 on VAS was reported following Ultrasound guided alcohol ablation by House and Connell[28]
Refer to the case reports in this article to learn about different management approaches.
Management of Acute Fat Pad Syndrome[edit | edit source]
- This usually occur as a result of falls, direct knee trauma or after knee surgeries resulting from arthroscopic equipment.
- Ice massage is very useful to relief acute symptoms[1]. It could be followed by taping to alleviate pressure off the fat pad.
- Flat foot wear should be avoided to minimize IFP loading.
- Advice patient to avoid provocative activities till the acute symptoms resolve.
Management of Chronic Fat Pad Syndrome[edit | edit source]
- Usually there is no history of trauma
- Biomechanical abnormalities, such as excessive hyperextension, should be addressed to decrease IFP loading
- To correct hyperextension, a relatively elevated shoe is advised
- Movement awareness and education are important in this stage
- Implement knee straightening exercises.
- Quadriceps and anterior hip stretching is found to improve IFP restriction symptoms[34].
- There is a significant impact of high BMI and obesity on knee OA and fat pad syndrome. An 18-month RCT investigated the effect of a weight loss program (Exercise and/or diet) on the IFP. The study reported significant reduction in the IFP volume as a result of weigh loss and changes in body fat percentage, mostly achieved by combining exercise and diet[35].
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Larbi A, Cyteval C, Hamoui M, Dallaudiere B, Zarqane H, Viala P. et al. Hoffa's disease: A report on 5 cases. Diagnostic and interventional imaging. 2014;95(11):1079-84.
- ↑ Kitagawa T, Ozaki N, Aoki Y. Effect of physical therapy on the flexibility of the infrapatellar fat pad: A single-blind randomised controlled trial. PloS one. 2022 Mar 17;17(3):e0265333.
- ↑ Leese J, Davies DC. An investigation of the anatomy of the infrapatellar fat pad and its possible involvement in anterior pain syndrome: a cadaveric study. Journal of Anatomy. 2020 Jul;237(1):20-8.
- ↑ Edama M, Otsuki T, Yokota H, Hirabayashi R, Sekine C, Maruyama S, Kageyama I. Morphological characteristics of the infrapatellar fat pad. Scientific Reports. 2022 May 27;12(1):1-9.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 Mace J, Bhatti W, Anand S. Infrapatellar fat pad syndrome: a review of anatomy, function, treatment and dynamics. Acta Orthopaedica Belgica. 2016;82(1):94-101.
- ↑ Macchi V, Stocco E, Stecco C, Belluzzi E, Favero M, Porzionato A et al. The infrapatellar fat pad and the synovial membrane: an anatomo-functional unit. J Anat. 2018;233(2):146-54.
- ↑ Bohnsack M, Wilharm A, Hurschler C, Rühmann O, Stukenborg-Colsman C, Wirth CJ. Biomechanical and kinematic influences of a total infrapatellar fat pad resection on the knee. The American journal of sports medicine. 2004;32(8):1873-80.
- ↑ Bohnsack M, Meier F, Walter GF, Hurschler C, Schmolke S, Wirth CJ. et al. Distribution of substance-P nerves inside the infrapatellar fat pad and the adjacent synovial tissue: a neurohistological approach to anterior knee pain syndrome. Archives of orthopaedic and trauma surgery. 2005;125(9):592-7.
- ↑ Culvenor AG, Cook JL, Warden SJ, Crossley KM. Infrapatellar fat pad size, but not patellar alignment, is associated with patellar tendinopathy. Scandinavian journal of medicine & science in sports. 2011;21(6):e405-11.
- ↑ Clockaerts S, Bastiaansen-Jenniskens YM, Runhaar J, Van Osch GJ, Van Offel JF, Verhaar JA. et al. The infrapatellar fat pad should be considered as an active osteoarthritic joint tissue: a narrative review. Osteoarthritis and Cartilage. 2010;18(7):876-82.
- ↑ 11.0 11.1 11.2 11.3 11.4 Hannon J, Bardenett S, Singleton S, Garrison JC. Evaluation, Treatment, and Rehabilitation Implications of the Infrapatellar Fat Pad. Sports health. 2016;8(2):167-71.
- ↑ Mellor R, Hodges PW. Motor unit syncronization is reduced in anterior knee pain. The Journal of pain. 2005;6(8):550-8.
- ↑ Hodges PW, Mellor R, Crossley K, Bennell K. Pain induced by injection of hypertonic saline into the infrapatellar fat pad and effect on coordination of the quadriceps muscles. Arthritis Care & Research. 2009;61(1):70-7.
- ↑ Jiang LF, Fang JH, Wu LD. Role of infrapatellar fat pad in pathological process of knee osteoarthritis: Future applications in treatment. World Journal of Clinical Cases. 2019 Aug 8;7(16):2134.
- ↑ 15.0 15.1 15.2 Ioan-Facsinay A, Kloppenburg M. An emerging player in knee osteoarthritis: the infrapatellar fat pad. Arthritis research & therapy. 2013;15(6):225.
- ↑ Distel E, Cadoudal T, Durant S, Poignard A, Chevalier X, Benelli C. The infrapatellar fat pad in knee osteoarthritis: An important source of interleukin‐6 and its soluble receptor. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology. 2009;60(11):3374-7.
- ↑ Caspar-Bauguil S, Cousin B, Galinier A, Segafredo C, Nibbelink M, Andre M et al. Adipose tissues as an ancestral immune organ: site‐specific change in obesity. FEBS letters. 2005;579(17):3487-92.
- ↑ Dragoo JL, Samimi B, Zhu M, Hame SL, Thomas BJ, Lieberman JR, et al. Tissue-engineered cartilage and bone using stem cells from human infrapatellar fat pads. The Journal of bone and joint surgery. British volume. 2003;85(5):740-7.
- ↑ Kim CS, Lee SC, Kim YM, Kim BS, Choi HS, Kawada T. et al. Visceral fat accumulation induced by a high‐fat diet causes the atrophy of mesenteric lymph nodes in obese mice. Obesity. 2008;16(6):1261-9.
- ↑ Duran S, Akşahin E, Kocadal O, Aktekin CN, Hapa O, Genctürk ZB. Effects of body mass index, infrapatellar fat pad volume and age on patellar cartilage defect. Orthopaedic journal of sports medicine. 2014;2(11_suppl3):2325967114S00159.
- ↑ 21.0 21.1 21.2 Kumar D, Alvand A, Beacon JP. Impingement of infrapatellar fat pad (Hoffa’s disease): results of high-portal arthroscopic resection. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2007;23(11):1180-6.
- ↑ Lenny Macrina. Fat Pad Assessment. Available from: https:https://www.youtube.com/watch?v=https://youtu.be/kbu9nybRV0M
- ↑ 23.0 23.1 Ogilvie-Harris DJ, Giddens J. Hoffa's disease: arthroscopic resection of the infrapatellar fat pad. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 1994 ;10(2):184-7.
- ↑ Witoński D, Wągrowska-Danielewicz M. Distribution of substance-P nerve fibers in the knee joint in patients with anterior knee pain syndrome A preliminary report. Knee Surgery, Sports Traumatology, Arthroscopy. 1999;7(3):177-83.
- ↑ Genin J, Faour M, Ramkumar PN, Yakubek G, Khlopas A, Chughtai M et al. Infrapatellar Fat Pad Impingement: A Systematic Review. J Knee Surg. 2017;30(7):639-46.
- ↑ Claire Patella. Infographic:Differentiating fat pad and pfj pain. Available from: https://youtu.be/eiwKkb1SulU
- ↑ Kim YM, Joo YB. Arthroscopic treatment of infrapatellar fat pad impingement between the patella and femoral trochlea: comparison of the clinical outcomes of partial and subtotal resection. Knee surgery & related research. 2019 Mar;31(1):54.
- ↑ House CV, Connell DA. Therapeutic ablation of the infrapatellar fat pad under ultrasound guidance: a pilot study. Clinical radiology. 2007;62(12):1198-201.
- ↑ How to ice massage for knee tendonitis my Physio SA Adelaide Physiotherapist. Available from: https://www.youtube.com/watch?v=6CRarRzStrU
- ↑ Claire Patella. Ice-It-Away Instructions-Fat Pad Available from: https://www.youtube.com/watch?v=aE6-EGAFkfI
- ↑ Union Physical Therapy. McConnel fat pad taping. Available from: https://www.youtube.com/watch?v=Xy7CibqEUtQ
- ↑ McConnell Physiotherapy Group. MCCONNELL KNEE TAPING (OFFICIAL). Available from: https://youtu.be/WbHXYnwUwws
- ↑ Motion Guidance. infrapatellar fat pad mobilization. Available from: https://www.youtube.com/watch?v=KR_peakgyi4
- ↑ Dragoo JL, Johnson C, McConnell J. Evaluation and treatment of disorders of the infrapatellar fat pad. Sports medicine. 2012;42(1):51-67.
- ↑ Murillo AL, Eckstein F, Wirth W, Beavers D, Loeser RF, Nicklas BJ. et al. Impact of diet and/or exercise intervention on infrapatellar fat pad morphology: secondary analysis from the intensive diet and exercise for arthritis (IDEA) trial. Cells Tissues Organs. 2017;203(4):258-66.
- ↑ Infrapatellar Fat Pad Knee Pain (Hoffa's Syndrome) Clinical Treatment - Dr Mandell. Available from: https://www.youtube.com/watch?v=xPouEzBmVJk