Differentiating Buttock Pain - Gluteal Tendinopathy: Difference between revisions
No edit summary |
No edit summary |
||
| (36 intermediate revisions by 4 users not shown) | |||
| Line 3: | Line 3: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
| Line 11: | Line 8: | ||
== Introduction == | == Introduction == | ||
[[Differentiating Buttock Pain and Sacroiliac Joint Disorders|Deep Gluteal pain is a complex condition]] that could be the manifestation of different soft tissue pathologies. Due to the complexity of the anatomy the symptoms are overlapping. Scans such as MRI and ultrasound don't rule out the irritating source of pain and the special tests | [[Differentiating Buttock Pain and Sacroiliac Joint Disorders|Deep Gluteal pain is a complex condition]] that could be the manifestation of different soft tissue pathologies. Due to the complexity of the anatomy the symptoms are overlapping. Scans such as [[MRI Scans|MRI]] and [[Ultrasound Scans|ultrasound]] don't rule out the irritating source of [[Pain Behaviours|pain]] and the special tests often don't discriminate the underlying structures that contribute to the symptoms<ref name=":2">Bell-Jenje T. Greater Trochanteric Pain Syndrome – Recommended Exercises & Progressions. Part 2. Groovimovements website. (Feb)2020. Available from: https://www.groovimovements.co.za/greater-trochanteric-pain-syndrome-recommended-exercises-progressions/</ref>. | ||
[[Gluteal Tendinopathy]] is a potential source of deep gluteal pain. The condition has been introduced as a concept very recently in the research compared to other structures that can cause gluteal pain such as [[Sacroiliac Joint Syndrome|Sacroiliac Joint]] and the [https://physio-pedia.com/Lumbar_Radiculopathy?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Lumbar] region. | [[Gluteal Tendinopathy]] is a potential source of deep gluteal pain. The condition has been introduced as a concept very recently in the research compared to other structures that can cause gluteal pain such as [[Sacroiliac Joint Syndrome|Sacroiliac Joint]] and the [https://physio-pedia.com/Lumbar_Radiculopathy?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Lumbar] region. | ||
== Gluteal Tendinopathy == | == Gluteal Tendinopathy == | ||
Gluteal tendinopathy, previously known as Greater Trochanteric Pain Syndrome is the most common lower limb tendinopathy.<ref>Ladurner A, Fitzpatrick J, O’Donnell JM. [https://journals.sagepub.com/doi/epub/10.1177/23259671211016850 Treatment of Gluteal Tendinopathy: A Systematic Review and Stage-Adjusted Treatment Recommendation.] Orthopaedic Journal of Sports Medicine. 2021 Jul 29;9(7):23259671211016850.</ref> It presents with a pain that starts in the greater trochanter region and may radiate to the lateral thigh and/or leg. Trochanteric Pain primarily is caused by the gluteal [[Tendon Biomechanics|tendons]] and a secondary cause of this pain is the bursal inflammation that used to be thought as the main source of pain. Other structures that could be involved in the pathology are the posterior [[Hip Anatomy|hip]] capsule, [[Gemellus Superior|Gemelli's]] and the [[Obturator Externus|Obturators]]<ref name=":2" />. Patients with Gluteal Tendinopathy have been shown to have high levels of anxiety and many of the patients experience pain almost the whole day<ref name=":5">Mest J, Vaughan B, Mulcahy J, Malliaras P. [https://www.researchgate.net/profile/Brett_Vaughan/publication/347390345_The_Prevalence_of_Self-Reported_Psychological_Characteristics_of_Adults_with_Lower_Limb_Tendinopathy/links/5fda865645851553a0c231e6/The-Prevalence-of-Self-Reported-Psychological-Char The Prevalence of Self-Reported Psychological Characteristics of Adults with Lower Limb Tendinopathy]. Muscles, Ligaments & Tendons Journal (MLTJ). 2020 Oct 1;10(4).</ref>. | |||
[[File:Inferior Gemellus - Bigstock Image.jpg|thumb|333x333px|center]] | {| border="1" cellpadding="1" cellspacing="1" | ||
|- | |||
! scope="col" | [[File:Inferior Gemellus - Bigstock Image.jpg|thumb|333x333px|center]]Inferior Gemellus | |||
! scope="col" | [[File:Obturator Externus - Bigstock Images.jpg|thumb|333x333px|center]]Obturator Internus | |||
! scope="col" | [[File:Obturator Internus - Bigstock Images.jpg|thumb|333x333px|center]]Obturator Externus | |||
|} | |||
This condition has a significant impact on [[Sleep: Regulation and Assessment|sleep]] quality, [[Physical Activity|physical activity,]] work participation and the [[Quality of Life|quality of life]] similar to patients waiting for [https://physio-pedia.com/Total_Hip_Replacement?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal a hip replacement] for severe [https://physio-pedia.com/Hip_Osteoarthritis#sts=Primary%20osteoarthritis%20versus%20Secondary%20osteoarthritis?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal hip osteoarthritis.]<ref>Fearon AM, et al. Greater Trochanteric Pain Syndrome Negatively Affects Work, Physical Activity and Quality of Life: A Case Control Study. J Arthroplast. 2014;29(2):383–86.</ref><ref>Castro KM, Silva EN. Evaluation and physiotherapeutic management of the greater major trochanteric pain syndrome: integrative review. BrJP. 2020 Jun 8;3:170-6.</ref>. The pain of Gluteal Tendon origin can refer to the sacroiliac region, the buttock, the groin and into the anterior thigh. This overlap of referral pattern doesn't help in differentiating other pathologies. | |||
Gluteal Tendinopathy is more relevant: in females over 40 years old; believed to be present in 23.5% of women who are at risk of [[Knee Osteoarthritis|knee osteoarthriti]]<nowiki/>s<ref>Segal NA, Felson DT, Torner JC, Zhu Y, Curtis JR, Niu J, et al. Greater trochanteric pain syndrome: epidemiology and associated factors. Arch Phys Med Rehab 2007;88(8):988e92. <nowiki>http://dx.doi.org/10.1016/j.apmr.2007.04.014</nowiki></ref>; 73 percent of the patients are believed to be either [[Menopause|menopausal]] or peri-menopausal, indicating a link between [[Hormones|hormonal]] changes and [https://physio-pedia.com/Tendinopathy?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal tendinopathy]; Certain medications are also shown to influence the tendon structural changes such as quinolone [[antibiotics]], oestrogen inhibitors such as Tamoxifen for patients who had [[Breast Cancer|breast cancer]]<ref name=":2" />. | |||
Most people wait 7.1 weeks to 4.4 years before seeking treatment for their symptoms. <ref>Gomez LP, Childress JM. [https://www.ncbi.nlm.nih.gov/books/NBK557433/ Greater Trochanteric Syndrome (GTS, Hip Tendonitis)]. InStatPearls [Internet] 2020 May 6. StatPearls Publishing.</ref> | |||
'''Other factors''' that were found to affect the presence and prognosis of Tendinopathy are: | '''Other factors''' that were found to affect the presence and prognosis of Tendinopathy are: | ||
* Smoking | * [[Smoking Cessation and Brief Intervention|Smoking]] | ||
* Diabetes | * [[Diabetes]] | ||
* Steriods | * [[Corticosteroid Medication|Steriods]] | ||
* Changes in load either underload or overload | * Changes in load either underload or overload that cause repetitive friction between the ITB and the greater trochanter<ref name=":7">Reid D. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4761624/ The management of greater trochanteric pain syndrome: a systematic literature review]. Journal of orthopaedics. 2016 Mar 1;13(1):15-28.</ref> | ||
'''Risk factors are'''<ref name=":0">Fearon AM, Ganderton C, Scarvell JM, Smith PN, Neeman T, Nash C, Cook JL. Development and validation of a VISA tendinopathy questionnaire for greater trochanteric pain syndrome, the VISA-G. Manual therapy. 2015 Dec 1;20(6):805-13.</ref>''':''' | |||
* Female gender <ref name=":5" /> | |||
* [[Older People Introduction|Older age]]<ref name=":6">Malliaras P, O’Neill S. [https://www.researchgate.net/profile/Peter_Malliaras/publication/318329085_Potential_risk_factors_leading_to_tendinopathy/links/5a0c0980aca2721a23fa4102/Potential-risk-factors-leading-to-tendinopathy.pdf Potential risk factors leading to tendinopathy]. Apunts. Medicina de l'Esport. 2017 Apr 1;52(194):71-7.</ref> | |||
'''Risk factors are'''<ref name=":0">Fearon AM, Ganderton C, Scarvell JM, Smith PN, Neeman T, Nash C, Cook JL. Development and validation of a VISA tendinopathy questionnaire for greater trochanteric pain syndrome, the VISA-G. Manual therapy. 2015 Dec 1;20(6):805-13.</ref>''':''' | |||
* Female gender | |||
* Older age | |||
* Higher BMI | * Higher BMI | ||
* Back pain | * Back pain | ||
* Lower femoral neck angle | * Lower femoral neck angle | ||
* Lipid levels<ref name=":6" /> | |||
* Adiposity<ref name=":6" /> especially in women that carry more fat around the hips<ref>Fearon AM, Stephens S, Cook JL, Smith PN, Neeman T, Cormick W, Scarvell JM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3597182/ The relationship of femoral neck shaft angle and adiposity to greater trochanteric pain syndrome in women]. A case control morphology and anthropometric study. British journal of sports medicine. 2012 Sep 1;46(12):888-92. | |||
</ref> | |||
* Genetics<ref name=":6" /> | |||
= | Factors such as greater psychological stress, poorer quality of life, greater waist girth and a higher BMI were relevant in severe cases. However, these factors might also develop as a result of pain.<ref name=":3">Mellor R, Grimaldi A, Wajswelner H, Hodges P, Abbott JH, Bennell K, Vicenzino B. Exercise and load modification versus corticosteroid injection versus ‘wait and see’for persistent gluteus medius/minimus tendinopathy (the LEAP trial): a protocol for a randomised clinical trial. BMC musculoskeletal disorders. 2016 Dec 1;17(1):196.</ref> But in most cases, pathology is a precursor to pain in tendinopathy. From literature, it seems that factors increasing the risk of developing pain in people with asymptomatic tendinopathy are emotional and cognitive risk factors like anxiety and maladaptive pain beliefs leading to fear avoidance.<ref name=":6" /> | ||
[[Depression]] has also been identified as a significant component of the patient profile of those with severe gluteal tendinopathy , suggesting that clinicians should screen for psychological distress, or the presence of possible depression in patients with lower limb tendinopathies, to better manage these complaints. | |||
Other factors such as depression, kinesiophobia and catastrophisation have been linked in gluteal tendinopathy with increased symptom severity.<ref name=":5" /> Depression is also a major component of patients with severe gluteal tendinopathy which means that therapists should be aware of this and screen for depression or psychological distress to be able to manage their patient's symptoms and refer appropriately when needed. <ref name=":5" /> | |||
The exact mechanism of how these risk factors influence the development of tendinopathy is mostly unknown<ref name=":6" />. Read the recent article by [https://www.researchgate.net/profile/Peter_Malliaras/publication/318329085_Potential_risk_factors_leading_to_tendinopathy/links/5a0c0980aca2721a23fa4102/Potential-risk-factors-leading-to-tendinopathy.pdf Mallarias and O'Neil (2020)] to learn more about the current thoughts on the influence. | |||
FADER or FADER resisted tests ( flexion adduction external rotation position). Pain over the lateral hip region is a positive test and could be diagnostic of gluteal tendinopathy. If the pain was reported in the deep gluteal region it could indicate deep gluteal pain syndrome. When the leg is flexion> 60 degrees, adduction, external rotation, the Piriformis becomes an internal rotator. Also, glute med and glute max swap roles from being an external rotator to being an internal rotator. | == Diagnosis == | ||
There are important measures in diagnosing Gluteal Tendinopathy<ref name=":2" />: | |||
* Patient's history such as gender, BMI, age and history of loading | |||
* Pain location: lateral hip pain. | |||
* Pain severity: usually 4/10 on most days | |||
* Palpation: tenderness over the superior aspect of the greater trochanter (the insertional point of glute medius and glute minimus) | |||
* FADER or FADER resisted tests ( flexion adduction external rotation position). Pain over the lateral hip region is a positive test and could be diagnostic of gluteal tendinopathy. If the pain was reported in the deep gluteal region it could indicate deep gluteal pain syndrome. When the leg is flexion> 60 degrees, adduction, external rotation, the Piriformis becomes an internal rotator. Also, glute med and glute max swap roles from being an external rotator to being an internal rotator. | |||
* A common sign is a reported difficulty in walking after sitting for a period of time often described as<nowiki>'' hobbling''</nowiki>. | |||
To rule out osteoarthritis of the hip, the subjective history of the patient and FADIR (flexion adduction internal rotation test) are used. A positive FADIR test might not rule out OA completely but a negative test is recognised to rule out intra-articular hip pathologies such as OA, [https://physio-pedia.com/Femoroacetabular_Impingement?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal# Femoral Acetabular Impingement] or [https://physio-pedia.com/Overview_of_hip_labral_tears?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Labral tear.] Also, in hip Osteoarthritis hip flexion ROM tends to be reduced. | |||
Hip External Rotator; Gemelli's, Obturators and Quadratus femori have been included in Lateral hip pain pathology<ref>Cox JM, Bakkum BW. Possible generators of retrotrochanteric gluteal and thigh pain: the gemelli–obturator internus complex. Journal of manipulative and physiological therapeutics. 2005 Sep 1;28(7):534-8.</ref>. They are positioned at 90 degrees to the long axis of the hip and serve important functions<ref name=":2" />: | |||
Hip External Rotator; Gemelli's, Obturators and Quadratus femori have been included in Lateral hip pain pathology. | |||
They | |||
* Compress the hip joint and to provide stability at the joint. | * Compress the hip joint and to provide stability at the joint. | ||
* Reinforce the posterior capsule of the hip | * Reinforce the posterior capsule of the hip | ||
== Management of Gluteal Tendinopathy == | |||
'''Patient education''' is considered the most important part of management<ref name=":2" />. Education includes the patient in the management and puts them in control with their treatment plan. | |||
'''Managing associated or provoking factors''' such as hormonal changes, co-morbidities, sleep, smoking and medications should be explained and discussed with the patient. Although some of these factors might not be modifiable however patients should be aware of them<ref name=":4">Bell-Jenje T. Differentiating Buttock Pain (Part 2). Plus Course 2020.</ref>. | |||
Promotion of '''healthy lifestyle changes''' such as quitting smoking and weight loss is integral in the management of Tendinopathy<ref>Cuff A. Tennis Elbow Management. Plus Course 2019.</ref>. | |||
'''Load management''' is used in the management of tendinopathy by gently increasing the load on the tendon and managing the <nowiki>''</nowiki>weekend-warrior exercise<nowiki>''</nowiki> or load and no-load scenario. | |||
People with Gluteal Tendinopathy are shown to have excessive hip adduction<ref name=":2" />. Therefore, adduction or leg movement across the mid-line should be avoided. This can be achieved by avoiding<ref name=":2" />: | |||
* Stretches should be avoided especially Tensor Fascia Lata muscle that compresses the Gluteus medius and minimus tendons | |||
People with | |||
* Stretches should be avoided especially Tensor Fascia Lata muscle | |||
* Crossing the legs especially with the affected leg on top of the non-affected | * Crossing the legs especially with the affected leg on top of the non-affected | ||
* Standing or hanging on one leg | * Standing or hanging on one leg | ||
* Lying on the affected side or non-affected without a firm pillow in between the legs. | * Lying on the affected side or non-affected without a firm pillow in between the legs | ||
* Dynamic valgus (hip adduction and internal rotation) during loading activities as it increases compression and tensile loading on the damaged tendon. | |||
The [https://www.researchgate.net/publication/336533371_VISA_G_scoring_guide_VISA_G_Development_of_the_VISA_G_1 Visa G questionnaire] was validated by Fearon et al <ref name=":0" /> as an outcome measure for disability resulting from lateral hip pain. The questionnaire looks at activities such as lying on the affected side, stairs negotiation and the overall severity of the hip pain. | |||
The | |||
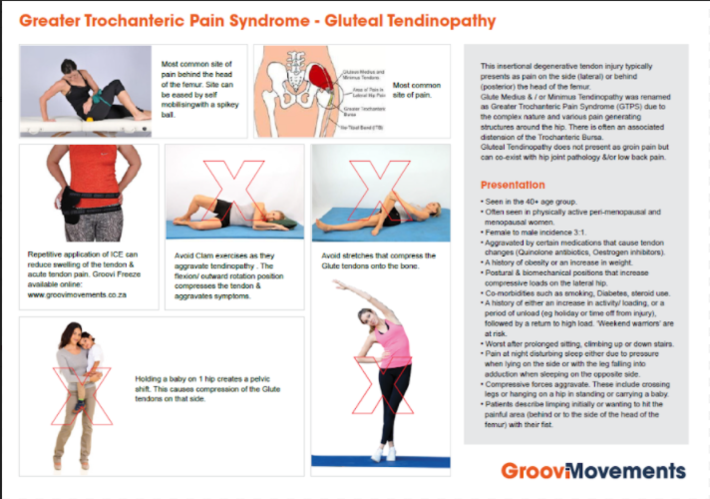
[[File:GT infographic.PNG|thumb|710x710px|none]]Download this patient infographic from Groovi Movements [https://www.groovimovements.co.za/greater-trochanteric-pain-syndrome-patient-info-graphic/ here]. | |||
=== Selection of exercises === | |||
Build up resistance to 4/10. Hold for 30 seconds. repeat 5 times daily<ref name=":2" />. | ==== Principals ==== | ||
* Hip abductor strength is not associated with the severity of the Gluteal tendinopathy<ref name=":3" /> | |||
* Compression forces can aggravate the lateral hip pain. An exercise such as Clam can provoke the tendon pain due to the high compressive force<ref name=":4" /> | |||
* Hip flexion should be avoided as it can negatively affect motor control and optimal muscle activation when Tensor Facia Lata and superficial hip flexors dominate over hip abductors and external rotators | |||
* Exercises should be progressive meaning that load should be increased gradually. The load can be managed by adjusting frequency, repetitions, resistance. | |||
* It is recommended to start the rehabilitation with isometric exercises as it proved to have an analgesic effect on tendon pain and can be used as an entry into rehabilitation and as 'in-season' for athletes to reduce pain and control symptoms<ref name=":1" /> | |||
* Loading should be monitored by observing the pain level following the exercises. A 4/10 pain during the exercise and no worse over 24 hours is ideal. | |||
* Build up the resistance to 4/10 intensity. Hold for 30 seconds. repeat 5 times daily<ref name=":2" />. | |||
* Advice the patients to perform the exercises slowly to stimulate the deep stability system of the muscle. | |||
* Rio et al<ref name=":1">Rio E, Kidgell D, Moseley GL, Gaida J, Docking S, Purdam C, Cook J. Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review. British journal of sports medicine. 2016 Feb 1;50(4):209-15.</ref> recommended the use of external motor control cues such as visual (mirror, video and pressure feedback) auditory (exercise metronome) and mental (mental rehearsing of the task) to stimulate neuroplastic changes | |||
* No pain should be allowed during functional tasks such as lunges, step-ups as it reflects the poor control of optimal alignment and increased compression on the Gluteal Tendon | |||
* Encourage exercises from a neutral lumbar spine. | |||
* An exercise that flares up the patient's symptoms shouldn't necessarily be avoided. Either return to this exercise later in the rehab stages or reduce the load and monitor the symptoms | |||
* French et al <ref>French HP, Woodley SJ, Fearon A, O’Connor L, Grimaldi A. Physiotherapy management of greater trochanteric pain syndrome (GTPS): an international survey of current physiotherapy practice. Physiotherapy. 2020 Dec 1;109:111-20.</ref>indicated, that ITB stretches and target the ITB with manual therapy should not be prescribed, as the evidence exists that an ITB stretch could potentially be provocative. | |||
==== Recommended Exercise Programme<ref name=":4" />: ==== | |||
Recommended Exercise Programme | |||
{| border="1" cellpadding="1" cellspacing="1" | {| border="1" cellpadding="1" cellspacing="1" | ||
|- | |- | ||
| Line 157: | Line 110: | ||
! scope="row" | Week 1 Early | ! scope="row" | Week 1 Early | ||
| Isometric Abduction | | Isometric Abduction | ||
Isometric Extension | |||
| In standing or Lying, against wall, bridging with resisted abduction | | In standing or Lying, against the wall, bridging with resisted abduction | ||
In standing or Lying, against wall, supine into ball | In standing or Lying, against the wall, supine into a ball | ||
| Low effort. Build up resistance slowly to a 4/10 pain max. 30-45 sec hold. 5-8 reps. 1-2 sets throughout the day. | | Low effort. Build up resistance slowly to a 4/10 pain max. 30-45 sec hold. 5-8 reps. 1-2 sets throughout the day. | ||
|- | |- | ||
| Line 166: | Line 119: | ||
Standing Abduction/External Rotation | Standing Abduction/External Rotation | ||
Motor Control | Motor Control | ||
| Modified clam using elastic band to increase resistance | | Modified clam using an elastic band to increase resistance | ||
Bilateral. Starting with light resistance | Bilateral. Starting with light resistance | ||
Glute Max over bed | Glute Max over the bed | ||
| Moderate effort. 8-12 reps. 2 sets once daily | | Moderate effort. 8-12 reps. 2 sets once daily | ||
| Line 177: | Line 130: | ||
Bridge Loading | Bridge Loading | ||
| Fire Hydrant-progress to doing the exercise with resistance | | Fire Hydrant-progress to doing the exercise with resistance | ||
Off-set Bridge, Single Leg Bridge, Hip Drop Bridge | Off-set Bridge, Single-Leg Bridge, Hip Drop Bridge | ||
|High load. 6-8 reps. 1 set.Once Daily | |High load. 6-8 reps. 1 set.Once Daily | ||
10 reps. 1-3 sets | 10 reps. 1-3 sets | ||
| Line 198: | Line 151: | ||
|} | |} | ||
{| border="1" cellpadding="1" cellspacing="1" | |||
|- | |||
! scope="col" | [[File:Static Hip Extension.PNG|thumb|333x333px|center]] Static Hip Extension | |||
! scope="col" | [[File:Resisted hip abduction-band.jpg|thumb|333x333px|center]]Resisted Hip Abduction | |||
! scope="col" | [[File:Abduction Slides.jpg|thumb|333x333px|center]]Abduction Slides | |||
|- | |||
! scope="col" | [[File:Single Leg Squat .jpg|thumb|333x333px|center]]Single Leg Squat | |||
! scope="col" | [[File:Split Lunges .jpg|thumb|333x333px|center]]Split Squat | |||
! scope="col" | [[File:Sidelying abduction .JPG|thumb|333x333px|center]]Sidelying Abduction | |||
|- | |||
! scope="col" | [[File:Bridge with static hip abduction.PNG|thumb|333x333px|center]]Bridge with static hip abduction | |||
! scope="col" | [[File:Modified clam with resistance band.PNG|thumb|333x333px|center]]Modified Clam | |||
! scope="col" | [[File:Optimal glute maximal firing.PNG|thumb|333x333px|center]]Optimal glute maximal firing | |||
|- | |||
! scope="col" | [[File:Pelvic drop and lift from bridge.PNG|thumb|333x333px|center]]Pelvic drop and lift from bridge | |||
! scope="col" | [[File:Resisted bird-dog.PNG|thumb|333x333px|center]]Resisted Bird-dog | |||
! scope="col" | [[File:Static Hip Abduction.PNG|thumb|333x333px|center]]Static Hip Abduction | |||
|} | |||
=== Other conservative options === | |||
'''Non-steroidal anti-inflammatory drugs''' | |||
Some studies show that NSAIDs and topical NSAIDs (for 6 weeks) may play a role in GTPS treatment of chronic tendinopathy.<ref name=":7" /> | |||
'''Extracorporeal Shock Wave Therapy (SWT)''' | |||
SWT has been shown to be effective in GTPS, however, the exact mechanism of the effect on GTPS is unclear. Evidence is however limited. | |||
Low-energy SWT seems to be more effective than cortisone injection at 4 months. Treatment regimens using SWT vary in practice and in research and could not be compared in a literature review by Reid (2016). <ref name=":7" /> | |||
'''Corticosteroid injections''' | |||
In a study in Serbia on 2,217 patients over 6 years in patients with trochanteric bursitis/GTPS showed that local cortisone injection with multimodel physiotherapy it was effective in 49% of patients. Cortisone alone resulted in an improvement of 39%. <ref>Nurkovic J, Jovasevic L, Konicanin A, Bajin Z, Ilic KP, Grbovic V, Skevin AJ, Dolicanin Z. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4968510/ Treatment of trochanteric bursitis: our experience.] Journal of physical therapy science. 2016;28(7):2078-81.</ref> Some studies show an early improvement after injection, lasting up to 3 months, with a peak at 6 weeks, but in the longer term the symptoms of GTPS seam to return.<ref name=":7" /> | |||
=== Surgery Options === | |||
Surgical is indicated when the tendon refracted or the patients are not responding to conservative management. Some surgical options are bursectomy, ITB release, trochanteric reduction [[osteotomy]], gluteal tendon repair, or a combination. Evidence on surgical options for GTPS is of low quality<ref name=":7" />. Recently, endoscopic surgery is being investigated instead of open surgery. <ref name=":7" /> | |||
A case series of 11 patients showed successful following an endoscopic release fo the ITB including a bursectomy. This was done on patients who failed recovery after 1 year of conservative management which included stretching, abductor strengthening, a minimum of one cortisone injections and or ESWT. <ref>Thomassen PJ, Basso T, Foss OA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6588147/ Endoscopic treatment of greater trochanteric pain syndrome-a case series of 11 patient]s. Journal of orthopaedic case reports. 2019 Jan;9(1):6. | |||
</ref> | |||
== References == | == References == | ||
| Line 210: | Line 202: | ||
[[Category:Pelvis - Conditions]] | [[Category:Pelvis - Conditions]] | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Plus Content]] | |||
<references /> | <references /> | ||
Latest revision as of 22:48, 30 October 2022
Original Editors - Mariam Hashem
Top Contributors - Mariam Hashem, Kim Jackson, Tarina van der Stockt, Lucinda hampton and Ewa Jaraczewska
Introduction[edit | edit source]
Deep Gluteal pain is a complex condition that could be the manifestation of different soft tissue pathologies. Due to the complexity of the anatomy the symptoms are overlapping. Scans such as MRI and ultrasound don't rule out the irritating source of pain and the special tests often don't discriminate the underlying structures that contribute to the symptoms[1].
Gluteal Tendinopathy is a potential source of deep gluteal pain. The condition has been introduced as a concept very recently in the research compared to other structures that can cause gluteal pain such as Sacroiliac Joint and the Lumbar region.
Gluteal Tendinopathy[edit | edit source]
Gluteal tendinopathy, previously known as Greater Trochanteric Pain Syndrome is the most common lower limb tendinopathy.[2] It presents with a pain that starts in the greater trochanter region and may radiate to the lateral thigh and/or leg. Trochanteric Pain primarily is caused by the gluteal tendons and a secondary cause of this pain is the bursal inflammation that used to be thought as the main source of pain. Other structures that could be involved in the pathology are the posterior hip capsule, Gemelli's and the Obturators[1]. Patients with Gluteal Tendinopathy have been shown to have high levels of anxiety and many of the patients experience pain almost the whole day[3].
| Inferior Gemellus | Obturator Internus | Obturator Externus |
|---|
This condition has a significant impact on sleep quality, physical activity, work participation and the quality of life similar to patients waiting for a hip replacement for severe hip osteoarthritis.[4][5]. The pain of Gluteal Tendon origin can refer to the sacroiliac region, the buttock, the groin and into the anterior thigh. This overlap of referral pattern doesn't help in differentiating other pathologies.
Gluteal Tendinopathy is more relevant: in females over 40 years old; believed to be present in 23.5% of women who are at risk of knee osteoarthritis[6]; 73 percent of the patients are believed to be either menopausal or peri-menopausal, indicating a link between hormonal changes and tendinopathy; Certain medications are also shown to influence the tendon structural changes such as quinolone antibiotics, oestrogen inhibitors such as Tamoxifen for patients who had breast cancer[1].
Most people wait 7.1 weeks to 4.4 years before seeking treatment for their symptoms. [7]
Other factors that were found to affect the presence and prognosis of Tendinopathy are:
- Smoking
- Diabetes
- Steriods
- Changes in load either underload or overload that cause repetitive friction between the ITB and the greater trochanter[8]
Risk factors are[9]:
- Female gender [3]
- Older age[10]
- Higher BMI
- Back pain
- Lower femoral neck angle
- Lipid levels[10]
- Adiposity[10] especially in women that carry more fat around the hips[11]
- Genetics[10]
Factors such as greater psychological stress, poorer quality of life, greater waist girth and a higher BMI were relevant in severe cases. However, these factors might also develop as a result of pain.[12] But in most cases, pathology is a precursor to pain in tendinopathy. From literature, it seems that factors increasing the risk of developing pain in people with asymptomatic tendinopathy are emotional and cognitive risk factors like anxiety and maladaptive pain beliefs leading to fear avoidance.[10]
Depression has also been identified as a significant component of the patient profile of those with severe gluteal tendinopathy , suggesting that clinicians should screen for psychological distress, or the presence of possible depression in patients with lower limb tendinopathies, to better manage these complaints.
Other factors such as depression, kinesiophobia and catastrophisation have been linked in gluteal tendinopathy with increased symptom severity.[3] Depression is also a major component of patients with severe gluteal tendinopathy which means that therapists should be aware of this and screen for depression or psychological distress to be able to manage their patient's symptoms and refer appropriately when needed. [3]
The exact mechanism of how these risk factors influence the development of tendinopathy is mostly unknown[10]. Read the recent article by Mallarias and O'Neil (2020) to learn more about the current thoughts on the influence.
Diagnosis[edit | edit source]
There are important measures in diagnosing Gluteal Tendinopathy[1]:
- Patient's history such as gender, BMI, age and history of loading
- Pain location: lateral hip pain.
- Pain severity: usually 4/10 on most days
- Palpation: tenderness over the superior aspect of the greater trochanter (the insertional point of glute medius and glute minimus)
- FADER or FADER resisted tests ( flexion adduction external rotation position). Pain over the lateral hip region is a positive test and could be diagnostic of gluteal tendinopathy. If the pain was reported in the deep gluteal region it could indicate deep gluteal pain syndrome. When the leg is flexion> 60 degrees, adduction, external rotation, the Piriformis becomes an internal rotator. Also, glute med and glute max swap roles from being an external rotator to being an internal rotator.
- A common sign is a reported difficulty in walking after sitting for a period of time often described as'' hobbling''.
To rule out osteoarthritis of the hip, the subjective history of the patient and FADIR (flexion adduction internal rotation test) are used. A positive FADIR test might not rule out OA completely but a negative test is recognised to rule out intra-articular hip pathologies such as OA, Femoral Acetabular Impingement or Labral tear. Also, in hip Osteoarthritis hip flexion ROM tends to be reduced.
Hip External Rotator; Gemelli's, Obturators and Quadratus femori have been included in Lateral hip pain pathology[13]. They are positioned at 90 degrees to the long axis of the hip and serve important functions[1]:
- Compress the hip joint and to provide stability at the joint.
- Reinforce the posterior capsule of the hip
Management of Gluteal Tendinopathy[edit | edit source]
Patient education is considered the most important part of management[1]. Education includes the patient in the management and puts them in control with their treatment plan. Managing associated or provoking factors such as hormonal changes, co-morbidities, sleep, smoking and medications should be explained and discussed with the patient. Although some of these factors might not be modifiable however patients should be aware of them[14].
Promotion of healthy lifestyle changes such as quitting smoking and weight loss is integral in the management of Tendinopathy[15].
Load management is used in the management of tendinopathy by gently increasing the load on the tendon and managing the ''weekend-warrior exercise'' or load and no-load scenario.
People with Gluteal Tendinopathy are shown to have excessive hip adduction[1]. Therefore, adduction or leg movement across the mid-line should be avoided. This can be achieved by avoiding[1]:
- Stretches should be avoided especially Tensor Fascia Lata muscle that compresses the Gluteus medius and minimus tendons
- Crossing the legs especially with the affected leg on top of the non-affected
- Standing or hanging on one leg
- Lying on the affected side or non-affected without a firm pillow in between the legs
- Dynamic valgus (hip adduction and internal rotation) during loading activities as it increases compression and tensile loading on the damaged tendon.
The Visa G questionnaire was validated by Fearon et al [9] as an outcome measure for disability resulting from lateral hip pain. The questionnaire looks at activities such as lying on the affected side, stairs negotiation and the overall severity of the hip pain.
Download this patient infographic from Groovi Movements here.
Selection of exercises[edit | edit source]
Principals[edit | edit source]
- Hip abductor strength is not associated with the severity of the Gluteal tendinopathy[12]
- Compression forces can aggravate the lateral hip pain. An exercise such as Clam can provoke the tendon pain due to the high compressive force[14]
- Hip flexion should be avoided as it can negatively affect motor control and optimal muscle activation when Tensor Facia Lata and superficial hip flexors dominate over hip abductors and external rotators
- Exercises should be progressive meaning that load should be increased gradually. The load can be managed by adjusting frequency, repetitions, resistance.
- It is recommended to start the rehabilitation with isometric exercises as it proved to have an analgesic effect on tendon pain and can be used as an entry into rehabilitation and as 'in-season' for athletes to reduce pain and control symptoms[16]
- Loading should be monitored by observing the pain level following the exercises. A 4/10 pain during the exercise and no worse over 24 hours is ideal.
- Build up the resistance to 4/10 intensity. Hold for 30 seconds. repeat 5 times daily[1].
- Advice the patients to perform the exercises slowly to stimulate the deep stability system of the muscle.
- Rio et al[16] recommended the use of external motor control cues such as visual (mirror, video and pressure feedback) auditory (exercise metronome) and mental (mental rehearsing of the task) to stimulate neuroplastic changes
- No pain should be allowed during functional tasks such as lunges, step-ups as it reflects the poor control of optimal alignment and increased compression on the Gluteal Tendon
- Encourage exercises from a neutral lumbar spine.
- An exercise that flares up the patient's symptoms shouldn't necessarily be avoided. Either return to this exercise later in the rehab stages or reduce the load and monitor the symptoms
- French et al [17]indicated, that ITB stretches and target the ITB with manual therapy should not be prescribed, as the evidence exists that an ITB stretch could potentially be provocative.
Recommended Exercise Programme[14]:[edit | edit source]
| Week/Stage | Exercise Type | Examples | Load |
|---|---|---|---|
| Week 1 Early | Isometric Abduction
Isometric Extension |
In standing or Lying, against the wall, bridging with resisted abduction
In standing or Lying, against the wall, supine into a ball |
Low effort. Build up resistance slowly to a 4/10 pain max. 30-45 sec hold. 5-8 reps. 1-2 sets throughout the day. |
| Week 2 | Isotonic:side-lying against gravity
Standing Abduction/External Rotation Motor Control |
Modified clam using an elastic band to increase resistance
Bilateral. Starting with light resistance Glute Max over the bed |
Moderate effort. 8-12 reps. 2 sets once daily
Light effort to activate Glutes Max before hamstrings or back extensor with 10 seconds holds |
| Week 3 | Neuroplastic Training
Bridge Loading |
Fire Hydrant-progress to doing the exercise with resistance
Off-set Bridge, Single-Leg Bridge, Hip Drop Bridge |
High load. 6-8 reps. 1 set.Once Daily
10 reps. 1-3 sets |
| Week 4-6 | Increase loading to incorporate functional high loading with heavy slow resistance | Abduction slides
Proprioception functional loading The Bird Dog Lateral Step Down |
Progressive. Increase resistance.8-12 Reps, 3 sets. 3-4 times weekly. Stop modified clam and optimal Glute Max |
| Week 6-12 Late Rehab | Increase loading. Sports specific exercises | Single-Leg squat
Backward Lunges on ball Contralateral split squat Step-up |
Increase weight-slow and heavy resistance. reduce reps as you increase the weight. 8-12 reps. 3 sets. 3-4 times weekly |
| Static Hip Extension | Resisted Hip Abduction | Abduction Slides |
|---|---|---|
| Single Leg Squat | Split Squat | Sidelying Abduction |
| Bridge with static hip abduction | Modified Clam | Optimal glute maximal firing |
| Pelvic drop and lift from bridge | Resisted Bird-dog | Static Hip Abduction |
Other conservative options[edit | edit source]
Non-steroidal anti-inflammatory drugs
Some studies show that NSAIDs and topical NSAIDs (for 6 weeks) may play a role in GTPS treatment of chronic tendinopathy.[8]
Extracorporeal Shock Wave Therapy (SWT)
SWT has been shown to be effective in GTPS, however, the exact mechanism of the effect on GTPS is unclear. Evidence is however limited.
Low-energy SWT seems to be more effective than cortisone injection at 4 months. Treatment regimens using SWT vary in practice and in research and could not be compared in a literature review by Reid (2016). [8]
Corticosteroid injections
In a study in Serbia on 2,217 patients over 6 years in patients with trochanteric bursitis/GTPS showed that local cortisone injection with multimodel physiotherapy it was effective in 49% of patients. Cortisone alone resulted in an improvement of 39%. [18] Some studies show an early improvement after injection, lasting up to 3 months, with a peak at 6 weeks, but in the longer term the symptoms of GTPS seam to return.[8]
Surgery Options[edit | edit source]
Surgical is indicated when the tendon refracted or the patients are not responding to conservative management. Some surgical options are bursectomy, ITB release, trochanteric reduction osteotomy, gluteal tendon repair, or a combination. Evidence on surgical options for GTPS is of low quality[8]. Recently, endoscopic surgery is being investigated instead of open surgery. [8]
A case series of 11 patients showed successful following an endoscopic release fo the ITB including a bursectomy. This was done on patients who failed recovery after 1 year of conservative management which included stretching, abductor strengthening, a minimum of one cortisone injections and or ESWT. [19]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Bell-Jenje T. Greater Trochanteric Pain Syndrome – Recommended Exercises & Progressions. Part 2. Groovimovements website. (Feb)2020. Available from: https://www.groovimovements.co.za/greater-trochanteric-pain-syndrome-recommended-exercises-progressions/
- ↑ Ladurner A, Fitzpatrick J, O’Donnell JM. Treatment of Gluteal Tendinopathy: A Systematic Review and Stage-Adjusted Treatment Recommendation. Orthopaedic Journal of Sports Medicine. 2021 Jul 29;9(7):23259671211016850.
- ↑ 3.0 3.1 3.2 3.3 Mest J, Vaughan B, Mulcahy J, Malliaras P. The Prevalence of Self-Reported Psychological Characteristics of Adults with Lower Limb Tendinopathy. Muscles, Ligaments & Tendons Journal (MLTJ). 2020 Oct 1;10(4).
- ↑ Fearon AM, et al. Greater Trochanteric Pain Syndrome Negatively Affects Work, Physical Activity and Quality of Life: A Case Control Study. J Arthroplast. 2014;29(2):383–86.
- ↑ Castro KM, Silva EN. Evaluation and physiotherapeutic management of the greater major trochanteric pain syndrome: integrative review. BrJP. 2020 Jun 8;3:170-6.
- ↑ Segal NA, Felson DT, Torner JC, Zhu Y, Curtis JR, Niu J, et al. Greater trochanteric pain syndrome: epidemiology and associated factors. Arch Phys Med Rehab 2007;88(8):988e92. http://dx.doi.org/10.1016/j.apmr.2007.04.014
- ↑ Gomez LP, Childress JM. Greater Trochanteric Syndrome (GTS, Hip Tendonitis). InStatPearls [Internet] 2020 May 6. StatPearls Publishing.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Reid D. The management of greater trochanteric pain syndrome: a systematic literature review. Journal of orthopaedics. 2016 Mar 1;13(1):15-28.
- ↑ 9.0 9.1 Fearon AM, Ganderton C, Scarvell JM, Smith PN, Neeman T, Nash C, Cook JL. Development and validation of a VISA tendinopathy questionnaire for greater trochanteric pain syndrome, the VISA-G. Manual therapy. 2015 Dec 1;20(6):805-13.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 Malliaras P, O’Neill S. Potential risk factors leading to tendinopathy. Apunts. Medicina de l'Esport. 2017 Apr 1;52(194):71-7.
- ↑ Fearon AM, Stephens S, Cook JL, Smith PN, Neeman T, Cormick W, Scarvell JM. The relationship of femoral neck shaft angle and adiposity to greater trochanteric pain syndrome in women. A case control morphology and anthropometric study. British journal of sports medicine. 2012 Sep 1;46(12):888-92.
- ↑ 12.0 12.1 Mellor R, Grimaldi A, Wajswelner H, Hodges P, Abbott JH, Bennell K, Vicenzino B. Exercise and load modification versus corticosteroid injection versus ‘wait and see’for persistent gluteus medius/minimus tendinopathy (the LEAP trial): a protocol for a randomised clinical trial. BMC musculoskeletal disorders. 2016 Dec 1;17(1):196.
- ↑ Cox JM, Bakkum BW. Possible generators of retrotrochanteric gluteal and thigh pain: the gemelli–obturator internus complex. Journal of manipulative and physiological therapeutics. 2005 Sep 1;28(7):534-8.
- ↑ 14.0 14.1 14.2 Bell-Jenje T. Differentiating Buttock Pain (Part 2). Plus Course 2020.
- ↑ Cuff A. Tennis Elbow Management. Plus Course 2019.
- ↑ 16.0 16.1 Rio E, Kidgell D, Moseley GL, Gaida J, Docking S, Purdam C, Cook J. Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review. British journal of sports medicine. 2016 Feb 1;50(4):209-15.
- ↑ French HP, Woodley SJ, Fearon A, O’Connor L, Grimaldi A. Physiotherapy management of greater trochanteric pain syndrome (GTPS): an international survey of current physiotherapy practice. Physiotherapy. 2020 Dec 1;109:111-20.
- ↑ Nurkovic J, Jovasevic L, Konicanin A, Bajin Z, Ilic KP, Grbovic V, Skevin AJ, Dolicanin Z. Treatment of trochanteric bursitis: our experience. Journal of physical therapy science. 2016;28(7):2078-81.
- ↑ Thomassen PJ, Basso T, Foss OA. Endoscopic treatment of greater trochanteric pain syndrome-a case series of 11 patients. Journal of orthopaedic case reports. 2019 Jan;9(1):6.