Deep Gluteal Pain Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| (23 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox">'''Original Editor '''- [[User:Mariam Hashem|Mariam Hashem]] | <div class="editorbox">'''Original Editor '''- [[User:Mariam Hashem|Mariam Hashem]] | ||
| Line 6: | Line 5: | ||
== Introduction == | == Introduction == | ||
The deep buttock area has complicated anatomy and hasn't been explored in-depth in the | The deep buttock area has complicated anatomy and hasn't been explored in-depth in the literature<ref>McCrory P, Bell S (1999) Nerve entrapment syndromes as a cause of pain in the hip, groin and buttock. Sports Med 27(4):261–274</ref>. | ||
Gluteal Pain Syndrome (DGS) is defined as pain or numbness in the buttock<ref>Frank RM, Slabaugh MA, Grumet RC, Virkus WW, Bush-Joseph CA, Nho SJ (2010) Posterior hip pain in an athletic population: differential diagnosis and treatment options. Sports Health 2(3):237–246</ref>, the hip, or the posterior thigh with radiation or radicular pain in the [https://physio-pedia.com/Sciatica?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Sciatic | Deep buttocks pain can arise from compression, inflammation, or injury of one or more of the structures in this area.<ref>Gonzalez-Lomas G. Deep gluteal pain in orthopaedics: a challenging diagnosis. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2021 Dec 15;29(24):e1282-90.</ref> Symptoms of pain and dysfunction in this area can be manifestations of different conditions such as [[Differentiating Buttock Pain and Sacroiliac Joint Disorders|Sacroiliac Joint Dysfunction,]] [[Differentiating Buttock Pain|Gluteal Tendinopathy]], [https://physio-pedia.com/Lumbar_Radiculopathy?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Lumbar Radiculopathy] and [https://physio-pedia.com/Piriformis_Syndrome?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Piriformis Syndrome.] Recent literature has investigated the involvement of various structures in the development of symptoms.<ref name=":7">Hu YW, Ho GW, Tortland PD. [https://journals.lww.com/acsm-csmr/Fulltext/2021/06000/Deep_Gluteal_Syndrome__A_Pain_in_the_Buttock.2.aspx Deep gluteal syndrome: a pain in the buttock.] Current Sports Medicine Reports. 2021 Jun 1;20(6):279-85.</ref> | ||
Gluteal Pain Syndrome (DGS) is defined as pain or numbness in the buttock<ref>Frank RM, Slabaugh MA, Grumet RC, Virkus WW, Bush-Joseph CA, Nho SJ (2010) Posterior hip pain in an athletic population: differential diagnosis and treatment options. Sports Health 2(3):237–246</ref>, the hip, or the posterior thigh with radiation or radicular pain in the [https://physio-pedia.com/Sciatica?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Sciatic nerve distribution]<ref name=":0">Bell-Jenje T. Differentiating Buttock Pain (Part 3). Plus Course 2020 </ref>. This condition is characterized by being<ref name=":5">Kizaki K, Uchida S, Shanmugaraj A, Aquino CC, Duong A, Simunovic N, Martin HD, Ayeni OR. Deep gluteal syndrome is defined as a non-discogenic sciatic nerve disorder with entrapment in the deep gluteal space: a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy. 2020 Apr 3:1-1.</ref>: | |||
# Non-discogenic | # Non-discogenic | ||
# A Sciatic nerve disorder | # A Sciatic nerve disorder | ||
# Nerve entrapment in the deep gluteal space. The most common sites of entrapment are: piriformis muscle (67.8%), sciatic foramen (6%), ischial tunnel (4.7%)<ref name=":4">Filler AG, Haynes J, Jordan SE, et al. Sciatica of nondisc origin and piriformis syndrome: diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment. J Neurosurg Spine 2005; 2: 99–115</ref> | # Nerve entrapment in the deep gluteal space. The most common sites of entrapment are: [[Piriformis|piriformis muscle]] (67.8%), sciatic foramen (6%), ischial tunnel (4.7%)<ref name=":4">Filler AG, Haynes J, Jordan SE, et al. Sciatica of nondisc origin and piriformis syndrome: diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment. J Neurosurg Spine 2005; 2: 99–115</ref> | ||
Gluteal Pain Syndrome is an umbrella of different conditions with similar and overlapping symptoms. | Gluteal Pain Syndrome is an umbrella of different conditions with similar and overlapping symptoms.<ref name=":7" /> | ||
'''Symptoms of Gluteal Pain Syndrome'''<ref name=":0" />''':''' | '''Symptoms of Gluteal Pain Syndrome'''<ref name=":0" />''':''' | ||
| Line 20: | Line 21: | ||
* Pain with prolonged sitting (longer than 20-30 minutes) | * Pain with prolonged sitting (longer than 20-30 minutes) | ||
* Pain with stride into a terminal extension | * Pain with stride into a terminal extension | ||
* Patients could | * Patients could limp with walking | ||
* Neurological sensory changes | * Neurological sensory changes | ||
* Severe night pain with disturbed sleep | * Severe night pain with disturbed sleep | ||
| Line 26: | Line 27: | ||
== '''Anatomy''' == | == '''Anatomy''' == | ||
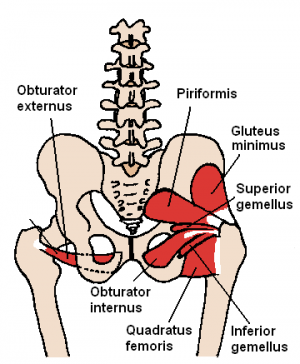
[[File:Piriformis, gemmeli, obturator, quadratus femoris.PNG|thumb]] | [[File:Piriformis, gemmeli, obturator, quadratus femoris.PNG|thumb]] | ||
The deep gluteal space has a unique anatomy. Understanding of its boundaries and contacts | The deep gluteal space has a unique anatomy. Understanding of its boundaries and contacts helps in improving the clinicians' palpation skills as well as the diagnosis of patients symptoms and presentation. | ||
'''The deep gluteal space is bounded by:''' | '''The deep gluteal space is bounded by:''' | ||
| Line 32: | Line 33: | ||
* Anteriorly: the posterior acetabular column, hip joint capsule and proximal femur | * Anteriorly: the posterior acetabular column, hip joint capsule and proximal femur | ||
* Laterally: the lateral lip of linea aspera and gluteal tuberosity | * Laterally: the lateral lip of linea aspera and gluteal tuberosity | ||
* Medially, sacrotuberous ligament and falciform fascia | * Medially, [[Sacrotuberous Ligament|sacrotuberous ligament]] and falciform [[fascia]] | ||
* Superiorly, the inferior margin of the sciatic notch | * Superiorly, the inferior margin of the sciatic notch | ||
* Inferiorly, the proximal origin of the hamstrings at ischial tuberosity<ref name=":2">Martin HD, Shears SA, Johnson JC, et al. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy 2011; 27: 172–81</ref> | * Inferiorly, the proximal origin of the hamstrings at ischial tuberosity<ref name=":2">Martin HD, Shears SA, Johnson JC, et al. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy 2011; 27: 172–81</ref> | ||
The deep | The '''deep six''' are important structures that lie underneath the [[Gluteus Maximus|Glutes Maximus]] and [[Gluteus Medius|Medius.]] The deep six are the Piriformis muscle, the [[Gemellus Superior|Superior Gemelli]], [[Obturator Internus]], [[Obturator Externus]],<ref>Meknas K, Christensen A, Johansen O (2003) The internal obturator muscle may cause sciatic pain. Pain 104(1–2):375–380</ref> Inferior [[Gemellus Inferior|Gemelli]] and [[Quadratus Femoris]]<ref>Vicentini JR, Martinez-Salazar EL, Simeone FJ, Bredella MA, Palmer WE, Torriani M. Kinematic MRI of ischiofemoral impingement. Skeletal Radiology. 2020 Jul 7:1-0.</ref>. The Piriformis and the Quadratus Femoris are the easiest to palpate<ref name=":0" />. | ||
The Sciatic Nerve lies over the Obturator and Gemelli complex<ref>Cox JM, Bakkum BW. Possible generators of retrotrochanteric gluteal and thigh pain: the gemelli-obturator internus complex. J Manipulative Physiol Ther 2005; 28: 534–8</ref> then | The Sciatic Nerve lies over the Obturator and Gemelli complex<ref>Cox JM, Bakkum BW. Possible generators of retrotrochanteric gluteal and thigh pain: the gemelli-obturator internus complex. J Manipulative Physiol Ther 2005; 28: 534–8</ref> it then sits laterally to the Ischial Tuberosity where the [[Biceps Femoris]] attaches. It is bound on the medial side, by the Ischial Tuberosity and on the lateral side, by the lesser trochanter of the femur. | ||
The Sciatic Nerve | The Sciatic Nerve can possibly become trapped underneath the Piriformis muscle <ref name=":1">Aguilera-Bohorquez B, Cardozo O, Brugiatti M, Cantor E, Valdivia N. Endoscopic treatment of sciatic nerve entrapment in deep gluteal syndrome: clinical results. Revista Española de Cirugía Ortopédica y Traumatología (English Edition). 2018 Sep 1;62(5):322-7.</ref> | ||
The nerve kinematics is a crucial aspect of entrapment’s pathophysiology<ref name=":2" />. The sciatic nerve glide across the posterior border of the greater trochanter when the hip moves into deep flexion, abduction and external rotation, Additionally, in the full flexed, abducted externally rotated state, the semimembranosus origin and the posterior edge of the greater trochanter can come into contact<ref name=":0" /> When the knee is flexed, the nerve moves posterolateral and when the knee is extended the nerve moves deep into the tunnel<ref>Martin R, Kivlan B, Martin HD. Greater Trochanter-Ischial Impingement: A Potential Source of Posterior Hip Pain. Rio de Janeiro: International Society for Hip Arthroscopy, 2014.</ref> | The [[Neurone|nerve]] kinematics is a crucial aspect of entrapment’s pathophysiology<ref name=":2" />. The sciatic nerve glide across the posterior border of the greater trochanter when the hip moves into deep flexion, abduction and external rotation, Additionally, in the full flexed, abducted externally rotated state, the [[semimembranosus]] origin and the posterior edge of the greater trochanter can come into contact<ref name=":0" /> When the knee is flexed, the nerve moves posterolateral and when the knee is extended the nerve moves deep into the tunnel<ref>Martin R, Kivlan B, Martin HD. Greater Trochanter-Ischial Impingement: A Potential Source of Posterior Hip Pain. Rio de Janeiro: International Society for Hip Arthroscopy, 2014.</ref> | ||
== Pudendal Nerve Entrapment == | == Pudendal Nerve Entrapment == | ||
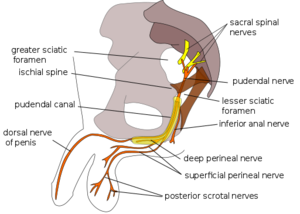
[[File:Pudendal nerve.svg.png|thumb]] | [[File:Pudendal nerve.svg.png|thumb]] | ||
The [https://physio-pedia.com/Sacrotuberous_Ligament?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Sacrotuberous Ligament] comes from the Ischial Tuberosity and inserts onto the sacrum and the coccyx while the Sacrospinous Ligament lies at 90 degrees to it, deep to the Sacrotuberous Ligament and attaches onto the Ischial Spine. The thickness of these ligaments could result in entrapment of the [https://physio-pedia.com/Pudendal_Neuralgia?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Pudendal Nerve], often referred to as Alcock Canal Syndrome or Cyclist Syndrome<ref name=":0" />. | The [https://physio-pedia.com/Sacrotuberous_Ligament?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Sacrotuberous Ligament] comes from the Ischial Tuberosity and inserts onto the sacrum and the coccyx while the Sacrospinous Ligament lies at 90 degrees to it, deep to the Sacrotuberous Ligament and attaches onto the Ischial Spine. The thickness of these ligaments could result in entrapment of the [https://physio-pedia.com/Pudendal_Neuralgia?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Pudendal Nerve], often referred to as Alcock Canal Syndrome or Cyclist Syndrome<ref name=":0" />. This entrapment syndrome is fairly unknown and often misdiagnosed with other pelvic floor diseases.<ref>Luesma MJ, Galé I, Fernando J. Diagnostic and therapeutic algorithm for pudendal nerve entrapment syndrome. Medicina Clínica (English Edition). 2021 Jul 23;157(2):71-8.</ref> | ||
In addition to the buttock pain, symptoms of | In addition to the buttock pain, symptoms of [[Pudendal Neuralgia|pudendal neuralgia]] include sexual dysfunction, rectal pain, faecal incontinence, and urinary incontinence. Pudendal Nerve entrapment can significantly affect the quality of life. | ||
This entrapment can be triggered by prolonged sitting especially on the bike or a recent change of the bike saddle. Usually, the symptoms could be aggravated by sitting, however, sitting on the toilet seat is reported to ease the pain due to the release of pressure off the nerve. | This entrapment can be triggered by prolonged sitting, especially on the bike, or a recent change of the bike saddle. Usually, the symptoms could be aggravated by sitting, however, sitting on the toilet seat is reported to ease the pain due to the release of pressure off the nerve. | ||
== Ischiofemoral Impingement == | == Ischiofemoral Impingement == | ||
Following hip | [[File:Quadratus Femoris - Bigstock Images.jpg|right|frameless]] | ||
Following hip surgeries especially [[Total Hip Replacement|total hip replacement]], some patients were reported to complain of posterior leg and deep buttock ache, especially with hip extension and adduction<ref name=":0" />. Ischiofemoral pain is a rare cause of hip pain first described in three patients after total hip arthroplasty and proximal femoral [[osteotomy]]<ref>Johnson KA. Impingement of the lesser trochanter on the ischial ramus after total hip arthroplasty. Report of three cases. J Bone Joint Surg Am 1977; 59: 268–9.</ref> | |||
The Ischiofemoral space is a very small space bordered by the Ischial Tuberosity and the lesser trochanter. Quadratus Femoris<ref>Taneja AK, Bredella MA, Torriani M. Ischiofemoral impingement. Magn Reson Imaging Clin N Am 2013; 21: 65–73.</ref> tightness/thickness or inflammation such as [[bursitis]] can cause narrowing and impingement on the nociceptive structures in that region. A study linked symptoms to the shortened distance between the bony margins of the ischium and the [[femur]] as measured on axial magnetic resonance imaging ([[MRI Scans|MRI]]) sequences<ref>Gollwitzer H, Banke IJ, Schauwecker J, Gerdesmeyer L, Suren C. How to address ischiofemoral impingement? Treatment algorithm and review of the literature. Journal of Hip Preservation Surgery. 2017 Dec;4(4):289-98.</ref> | |||
Image: Quadratus Femoris | |||
'''Symptoms:''' | '''Symptoms:''' | ||
* Deep-seated buttock pain often described as a deep ache, sometimes radiates to the knee | * Deep-seated buttock pain, often described as a deep ache, sometimes radiates to the knee | ||
* Short strides are often easier than long strides when running. This is due to the narrowing of the Ischiofemoral space with hip extension and adduction increased with the stride length | * Short strides are often easier than long strides when running. This is due to the narrowing of the Ischiofemoral space with hip extension, and adduction increased with the stride length | ||
* Facet type pain at L3-4 | * [[Facet Joints|Facet]] type pain at L3-4 or L4-5 could be confused with a primary lumbar problem. Back pain could be due to the loss of hip extension | ||
* Ischiofemoral Impingement pain is worse with terminal hip extension and adduction | * Ischiofemoral Impingement pain is worse with terminal hip extension and adduction | ||
* Tenderness on palpation of the ischium during passive provocative movement <ref>Wilson MD, Keene JS. Treatment of ischiofemoral impingement: results of diagnostic injections and arthroscopic resection of the lesser trochanter. J Hip Preserv Surg 2016; 3: 146–53</ref> | * Tenderness on palpation of the ischium during passive provocative movement <ref>Wilson MD, Keene JS. Treatment of ischiofemoral impingement: results of diagnostic injections and arthroscopic resection of the lesser trochanter. J Hip Preserv Surg 2016; 3: 146–53</ref> | ||
* Snapping, clicking or locking sensation of the hip joint during long-stride walking caused by the lesser trochanter forcefully bypassing the ischium | * Snapping, clicking or locking sensation of the hip joint during long-stride walking caused by the lesser trochanter forcefully bypassing the ischium | ||
Physical examination findings are not conclusive on the diagnosis of Ischiofemoral Impingement. The combination of passive extension, adducting and external rotation the hip is used to provoke the symptoms<ref>Safran M, Ryu J. Ischiofemoral impingement of the hip: a novel approach to treatment. Knee Surg Sports Traumatol Arthrosc 2014; 22: 781–5.</ref>. | Physical examination findings are not conclusive on the diagnosis of Ischiofemoral Impingement. The combination of passive extension, adducting and external rotation of the hip is used to provoke the symptoms<ref>Safran M, Ryu J. Ischiofemoral impingement of the hip: a novel approach to treatment. Knee Surg Sports Traumatol Arthrosc 2014; 22: 781–5.</ref>. | ||
The long stride walking test (walking with large steps) has a sensitivity of 92% and a specificity of 82% <ref>4. Gomez-Hoyos J, Martin RL, Schroder R et al. Accuracy of 2 clinical tests for ischiofemoral impingement in patients with posterior hip pain and endoscopically confirmed diagnosis. Arthroscopy 2016; 32: 1279–84</ref> | The long stride walking test (walking with large steps) has a sensitivity of 92% and a specificity of 82% <ref>4. Gomez-Hoyos J, Martin RL, Schroder R et al. Accuracy of 2 clinical tests for ischiofemoral impingement in patients with posterior hip pain and endoscopically confirmed diagnosis. Arthroscopy 2016; 32: 1279–84</ref> | ||
| Line 69: | Line 73: | ||
== Hamstring tendinopathy == | == Hamstring tendinopathy == | ||
The insertion point of the Hamstring is on the Ischial Tuberosity, very close to the Sciatic Nerve. [https://physio-pedia.com/Proximal_Hamstring_Tendinopathy?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Proximal hamstring tendinopathy] is common among distance runners and athletes performing sagittal plane (eg, sprinting, hurdling) or change-of-direction activities such as football and hockey drills <ref name=":6">Goom TS, Malliaras P, Reiman MP, Purdam CR. Proximal hamstring tendinopathy: clinical aspects of assessment and management. | The insertion point of the [[Hamstrings|Hamstring]] is on the Ischial Tuberosity, very close to the Sciatic Nerve. [https://physio-pedia.com/Proximal_Hamstring_Tendinopathy?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Proximal hamstring tendinopathy] is common among distance runners and athletes performing sagittal plane (eg, sprinting, hurdling) or change-of-direction activities such as football and hockey drills <ref name=":6">Goom TS, Malliaras P, Reiman MP, Purdam CR. Proximal hamstring tendinopathy: clinical aspects of assessment and management. Journal of orthopaedic & sports physical therapy. 2016 Jun;46(6):483-93.</ref> | ||
'''Signs and Symptoms'''<ref name=":0" />''':''' | '''Signs and Symptoms'''<ref name=":0" />''':''' | ||
* History of repetitive loading in flexion. During flexion movements such as deadlifts and other flexion activities the,proximal | * History of repetitive loading in flexion. During flexion movements such as deadlifts and other flexion activities the, proximal hamstring tendon undergoes tensile loading on the Ischial Tuberosity | ||
* Deep, localised pain in the region of the ischial tuberosity | * Deep, localised pain in the region of the ischial tuberosity | ||
* Pain gets worse with sitting (described as sitting on a boggy mass), driving, picking up boxes and uphill running due to the shear forces between the hamstring attachment and ischial tuberosity with increased hip flexion. During running, the peak force occurs in late swing, with a second peak reported in early stance. | * Pain gets worse with sitting (described as sitting on a boggy mass), driving, picking up boxes and uphill running. This is due to the shear forces between the hamstring attachment and ischial tuberosity with increased hip flexion. During running, the peak force occurs in late swing, with a second peak reported in early stance. | ||
* Positive straight leg raise | * Positive straight leg raise | ||
* Positive slump and neurodynamic test which indicates pressure on the Sciatic Nerve but doesn't rule out Hamstrings Tendinopathy | * Positive [[Slump Test|slump]] and neurodynamic test which indicates pressure on the Sciatic Nerve but doesn't rule out Hamstrings Tendinopathy | ||
* Thickening on palpation around the Ischial Tuberosity lateral to the Ischium | * Thickening on palpation around the Ischial Tuberosity lateral to the Ischium | ||
Pain score should increase with load assessment tests<ref name=":6" />: | Pain score should increase with load assessment tests<ref name=":6" />: | ||
* Progression from the single-leg bent-knee bridge to the long-lever bridge to arabesque as follows: | * Progression from the single-leg bent-knee bridge to the long-lever bridge to arabesque as follows: | ||
[[File:Single_Leg_Long_Lever_Bridge.png| | Single Leg Long Lever Bridge: | ||
[[File:Single_Leg_Long_Lever_Bridge.png|341x341px]][[File:Long lever bridge.gif|thumb|400x400px|none|Long lever bridge]][[File:Arabesque.jpg|thumb|400x400px|left| | |||
Arabesque exercise | |||
]] | |||
* Single-leg deadlift | * Single-leg deadlift | ||
[[File:Single leg dead lift.jpg|none|thumb]] | [[File:Single leg dead lift.jpg|none|thumb|Single leg dead lift]] | ||
* Three passive stretch tests (bent-knee stretch, modified bent-knee stretch, and Puranen-Orava test) have moderate to high validity and high sensitivity and specificity for the diagnosis of PHT: | * Three passive stretch tests (bent-knee stretch, modified bent-knee stretch, and Puranen-Orava test) have moderate to high validity and high sensitivity and specificity for the diagnosis of PHT: | ||
| Line 95: | Line 103: | ||
== Examination == | == Examination == | ||
Lumbar spine pathology should be ruled out first. Physical examination includes palpation, pelvic girdle and Sacroiliac Joint tests Tests such as the March test and the active straight leg raise test. | Lumbar spine pathology should be ruled out first. Physical examination includes palpation, pelvic girdle and Sacroiliac Joint tests Tests such as the March/Gillet test and the active [[Straight Leg Raise Test|straight leg raise test]]. | ||
Patients with sciatic nerve entrapment are often presented with a history of previous trauma, pain with sitting, radicular leg pain and paresthesia<ref>Benson B, Schutzer SF. Posttraumatic Piriformis syndrome: diagnosis and results of operative treatment. J Bone Joint Surg Am 1999; 81: 941–9</ref> | Patients with sciatic nerve entrapment are often presented with a history of previous trauma, pain with sitting, radicular leg pain and paresthesia<ref>Benson B, Schutzer SF. Posttraumatic Piriformis syndrome: diagnosis and results of operative treatment. J Bone Joint Surg Am 1999; 81: 941–9</ref> | ||
A positive March test or active straight leg raise test, indicate poor motor control and failed load transfer, but | A positive March test or active straight leg raise test, indicate poor motor control and failed [[Load and Shift|load]] transfer, but neither differentiates the pathologic structure<ref name=":0" />. | ||
{{#ev:youtube|jxhR5iCpPz0|300}}<ref>Proper Introduction and Gillet's Test on Diamond . Available from:https://www.youtube.com/watch?v=jxhR5iCpPz0[last accessed 22/10/2020]</ref> | |||
A | To rule out [[hip Osteoarthritis]], the total arc of motion and FADIR tests are utilised. A negative FADIR can rule out intra-articular pathology, such as [[Labral Tear|labral]] damage or [https://physio-pedia.com/Hip_Osteoarthritis?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal osteoarthritis of the hip]<ref name=":0" />. | ||
https://www.youtube.com/watch?v= | {{#ev:youtube|PqgPWRqmQ_A|300}}<ref>How to do the FADIR hip impingement test . Available from:https://www.youtube.com/watch?v=PqgPWRqmQ_A[last accessed 22/10/2020]</ref> | ||
<ref> | A positive FABER test provokes Sciatic Nerve symptoms where the nerve glides across the posterior border of the greater trochanter in that position <ref name=":0" />. Applying the same test, the pain felt on the greater trochanter could be due to Gluteal tendinopathy. If the patient felt the pain deep in the buttock it is more likely to be compression or irritation around the Piriformis muscle or some of the deep six. | ||
{{#ev:youtube|v=RMgaRoBg0do|300}}<ref>Ortho EVAL Pal With Paul Marquis PT. FABER/Patrick/Figure 4 Test-How to Perform it and What it Means! 2021 . Available from:https://www.youtube.com/watch?v=RMgaRoBg0do[last accessed 26/10/2022]</ref> | |||
Patients with Deep Gluteal Pain Syndrome can present with altered nerve conduction tests, changes in reflexes, motor weakness<ref>Papadopoulos EC, Khan SN. Piriformis syndrome and low back pain: a new classification and review of the literature. Orthop Clin North Am 2004; 35: 65–71</ref>, and sensation changes which make it difficult in differentiating the lumbar spine from the buttock<ref name=":0" />. | |||
The combination of the seated piriformis stretch test with the piriformis active test has shown a sensitivity of 91% and specificity of 80% for the endoscopic finding of sciatic nerve entrapment<ref>Martin HD, Kivlan BR, Palmer IJ, et al. Diagnostic accuracy of clinical tests for sciatic nerve entrapment in the gluteal region. Knee Surg Sports Traumatol Arthrosc 2014; 22: 882–8.</ref> | |||
{{#ev:youtube|JR1rtQ-PF38|300}}<ref>Piriformis stretch. Available from:https://www.youtube.com/watch?v=JR1rtQ-PF38[last accessed 22/10/2020]</ref> | |||
{{#ev:youtube|iL19XaxMmP4|300}}<ref>Piriformis stretch. Available from:https://www.youtube.com/watch?v=iL19XaxMmP4[last accessed 22/10/2020]</ref> | |||
= | Palpation skills can be useful in differentiating the site of pain and texture of soft tissue<ref name=":0" />. Using the ischial tuberosity as a reference while trying to reproduce the patient's pain with palpation to understand the probable source of symptoms <ref name=":3">Martin HD, Reddy M, Gómez-Hoyos J. Deep gluteal syndrome. Journal of hip preservation surgery. 2015 Jul 1;2(2):99-107. </ref> | ||
{{#ev:youtube|IhvVoKGyl8E|300}}<ref>Physical Examination of the Hip - Hal D. Martin D.O.. Available from:https://www.youtube.com/watch?v=IhvVoKGyl8E[last accessed 22/10/2020]</ref> | |||
=== Differential Diagnosis === | |||
The following table matches the deep gluteal pain conditions with their most likely symptoms<ref name=":0" />: | |||
{| border="1" cellpadding="1" cellspacing="1" | |||
|- | |||
! scope="row" | Condition | |||
! scope="col" | Symptoms | |||
|- | |||
! scope="row" | Reactive hamstring tendon, bursitis | |||
| Uphill running | |||
Deadlifts | |||
Picking up boxes / other loading flexion activity | |||
Feels like is sitting on a boggy mass | |||
|- | |||
! scope="row" | Non-discogenic Sciatic nerve entrapment | |||
| Radicular leg pain with hip flexion | |||
|- | |||
! scope="row" | Pudendal nerve entrapment | |||
| Increased time on the bike or change in saddle | |||
Sitting on a toilet seat eases the pain | |||
|- | |||
! scope="row" |Ischiofemoral Impingement, lumbar facet pain, Sacroiliac Joint pain | |||
| Pain with hip extension or long strides | |||
|- | |||
! scope="row" |Ischiofemoral Impingement | |||
| History of trauma or hip surgery | |||
|- | |||
! scope="row" |Gluteal Tendinopathy, Obturator / Gemelli Tendinopathy | |||
| Limping after prolonged sitting | |||
|} | |||
== Management == | |||
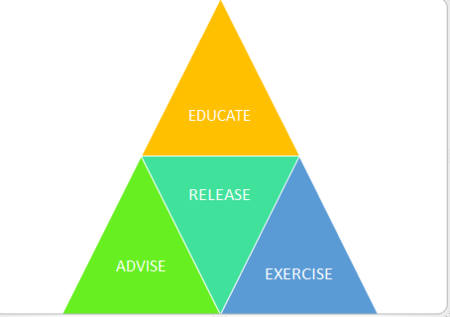
Hamstring tendinopathy: | === Principals: === | ||
* Differentiating the source of pain is recommended by using knowledge and assessment skills | |||
* Educate your patient on the anatomy and causes of symptoms | |||
*[[File:Principals of Deep Gluteal Pain management.PNG|thumb|450x450px]]Address [https://physio-pedia.com/Chronic_Pain?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal chronic pain] factors using the biopsychosocial approach | |||
* Advice [https://physio-pedia.com/Load_Management?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal load management] | |||
'''Hamstring tendinopathy:''' | |||
# Avoid deadlifts and other flexion activities | |||
# Avoid Hamstring stretches such as straightening the leg at 90 degrees of hip flexion | |||
'''Sciatic Nerve involvement:''' | |||
# When driving, move the car seat closer to the steering wheel to ease off that neural tension off the Sciatic Nerve | |||
# For runners, advice them to reduce their stride length to relieve the symptoms | |||
'''Pudendal Nerve type symptoms,''' you may need to refer the patient to a woman or men's health physiotherapist to assist you with the symptoms such as rectal pain, faecal incontinence or urinary incontinence. Refer female patients over 50 to the gynaecologist to assist their hormonal status. Lifestyle changes and weight management advice is also recommended | |||
'''General Advice on the following:''' | |||
* Weight management | |||
* Lifestyle changes | |||
* Sleep hygiene | |||
* Risk factors such as smoking | |||
Myofascial release, manual therapy in conjunction with the appropriate rehabilitation and advice are helpful clinical tools in the management of Deep Gluteal Pain<ref name=":0" />. | |||
Image-guided anaesthetic block or steroid injections might also be effective<ref name=":4" /> | |||
'''Surgical options are:''' | |||
Partial lesser trochanteric plastics for Ischiofemoral Impingement | |||
Arthroscopic or endoscopic releases of adhesions between Hamstring tendons or the Piriformis tendon and the Sciatic Nerve <ref>Kay J, Morrison L, Fejtek E, Simunovic N, Martin HD, Ayeni OR. Surgical management of deep gluteal syndrome causing sciatic nerve entrapment: a systematic review. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2017 Dec 1;33(12):2263-78.</ref><ref name=":1" />. | |||
. | |||
=== Exercises === | === Exercises === | ||
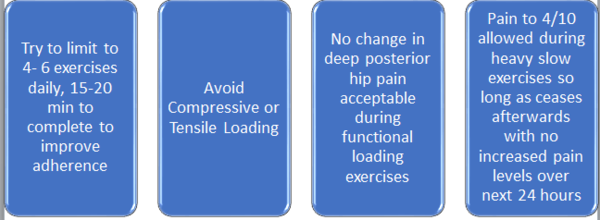
'''Principals of exercise prescription'''<ref name=":0" />''':''' | |||
[[File:Exercise principals DGS.PNG|thumb|600x600px]] | |||
Try and limit the exercises to 15 or 20 minutes a day to improve your compliance and | Try and limit the exercises to 15 or 20 minutes a day to improve your compliance and adherence. | ||
Avoid stretching at the beginning of the treatment of tendinopathy to reduce the tensile loading on the tendon and possibly introduce them later when the pain settles. | |||
When managing [[Tendinopathy]], try to keep the pain below 5/10 and no worse at 24 hours afterwards especially with functional loading exercises such as the step-down, one-legged squat, a dynamic lunge, and a split squat. | |||
When performing Piriformis stretch with the hip at 90 degrees, the hip needs to be in an externally rotated position. Piriformis is a hip abductor and external rotator below 45 to 60 degrees of hip flexion but functions as an internal rotator above 60 degrees of hip flexion | |||
Combine exercises with neurodynamic gliding techniques, such as a Sciatic Nerve slider | |||
Advise gluteal strengthening as bird-dog, split squats, and functional loading exercises | |||
Progressive loading with emphasis on hip extensors, abductors and lateral rotators as a general rule | |||
[[File:Single Leg Squat .jpg|none|thumb|Single Leg Squat ]] | |||
[[File:Resisted bird-dog.PNG|none|thumb|Resisted bird-dog]] | |||
== References == | == References == | ||
| Line 252: | Line 225: | ||
[[Category:Pelvis - Conditions]] | [[Category:Pelvis - Conditions]] | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Plus Content]] | |||
<references /> | <references /> | ||
Latest revision as of 00:21, 31 October 2022
Introduction[edit | edit source]
The deep buttock area has complicated anatomy and hasn't been explored in-depth in the literature[1].
Deep buttocks pain can arise from compression, inflammation, or injury of one or more of the structures in this area.[2] Symptoms of pain and dysfunction in this area can be manifestations of different conditions such as Sacroiliac Joint Dysfunction, Gluteal Tendinopathy, Lumbar Radiculopathy and Piriformis Syndrome. Recent literature has investigated the involvement of various structures in the development of symptoms.[3]
Gluteal Pain Syndrome (DGS) is defined as pain or numbness in the buttock[4], the hip, or the posterior thigh with radiation or radicular pain in the Sciatic nerve distribution[5]. This condition is characterized by being[6]:
- Non-discogenic
- A Sciatic nerve disorder
- Nerve entrapment in the deep gluteal space. The most common sites of entrapment are: piriformis muscle (67.8%), sciatic foramen (6%), ischial tunnel (4.7%)[7]
Gluteal Pain Syndrome is an umbrella of different conditions with similar and overlapping symptoms.[3]
Symptoms of Gluteal Pain Syndrome[5]:
- Buttock and often retro greater trochanter pain
- Bilateral but usually unilateral symptoms
- Pain with prolonged sitting (longer than 20-30 minutes)
- Pain with stride into a terminal extension
- Patients could limp with walking
- Neurological sensory changes
- Severe night pain with disturbed sleep
Anatomy[edit | edit source]
The deep gluteal space has a unique anatomy. Understanding of its boundaries and contacts helps in improving the clinicians' palpation skills as well as the diagnosis of patients symptoms and presentation.
The deep gluteal space is bounded by:
- Posteriorly, the gluteus maximus
- Anteriorly: the posterior acetabular column, hip joint capsule and proximal femur
- Laterally: the lateral lip of linea aspera and gluteal tuberosity
- Medially, sacrotuberous ligament and falciform fascia
- Superiorly, the inferior margin of the sciatic notch
- Inferiorly, the proximal origin of the hamstrings at ischial tuberosity[8]
The deep six are important structures that lie underneath the Glutes Maximus and Medius. The deep six are the Piriformis muscle, the Superior Gemelli, Obturator Internus, Obturator Externus,[9] Inferior Gemelli and Quadratus Femoris[10]. The Piriformis and the Quadratus Femoris are the easiest to palpate[5].
The Sciatic Nerve lies over the Obturator and Gemelli complex[11] it then sits laterally to the Ischial Tuberosity where the Biceps Femoris attaches. It is bound on the medial side, by the Ischial Tuberosity and on the lateral side, by the lesser trochanter of the femur.
The Sciatic Nerve can possibly become trapped underneath the Piriformis muscle [12]
The nerve kinematics is a crucial aspect of entrapment’s pathophysiology[8]. The sciatic nerve glide across the posterior border of the greater trochanter when the hip moves into deep flexion, abduction and external rotation, Additionally, in the full flexed, abducted externally rotated state, the semimembranosus origin and the posterior edge of the greater trochanter can come into contact[5] When the knee is flexed, the nerve moves posterolateral and when the knee is extended the nerve moves deep into the tunnel[13]
Pudendal Nerve Entrapment[edit | edit source]
The Sacrotuberous Ligament comes from the Ischial Tuberosity and inserts onto the sacrum and the coccyx while the Sacrospinous Ligament lies at 90 degrees to it, deep to the Sacrotuberous Ligament and attaches onto the Ischial Spine. The thickness of these ligaments could result in entrapment of the Pudendal Nerve, often referred to as Alcock Canal Syndrome or Cyclist Syndrome[5]. This entrapment syndrome is fairly unknown and often misdiagnosed with other pelvic floor diseases.[14]
In addition to the buttock pain, symptoms of pudendal neuralgia include sexual dysfunction, rectal pain, faecal incontinence, and urinary incontinence. Pudendal Nerve entrapment can significantly affect the quality of life.
This entrapment can be triggered by prolonged sitting, especially on the bike, or a recent change of the bike saddle. Usually, the symptoms could be aggravated by sitting, however, sitting on the toilet seat is reported to ease the pain due to the release of pressure off the nerve.
Ischiofemoral Impingement[edit | edit source]
Following hip surgeries especially total hip replacement, some patients were reported to complain of posterior leg and deep buttock ache, especially with hip extension and adduction[5]. Ischiofemoral pain is a rare cause of hip pain first described in three patients after total hip arthroplasty and proximal femoral osteotomy[15]
The Ischiofemoral space is a very small space bordered by the Ischial Tuberosity and the lesser trochanter. Quadratus Femoris[16] tightness/thickness or inflammation such as bursitis can cause narrowing and impingement on the nociceptive structures in that region. A study linked symptoms to the shortened distance between the bony margins of the ischium and the femur as measured on axial magnetic resonance imaging (MRI) sequences[17]
Image: Quadratus Femoris
Symptoms:
- Deep-seated buttock pain, often described as a deep ache, sometimes radiates to the knee
- Short strides are often easier than long strides when running. This is due to the narrowing of the Ischiofemoral space with hip extension, and adduction increased with the stride length
- Facet type pain at L3-4 or L4-5 could be confused with a primary lumbar problem. Back pain could be due to the loss of hip extension
- Ischiofemoral Impingement pain is worse with terminal hip extension and adduction
- Tenderness on palpation of the ischium during passive provocative movement [18]
- Snapping, clicking or locking sensation of the hip joint during long-stride walking caused by the lesser trochanter forcefully bypassing the ischium
Physical examination findings are not conclusive on the diagnosis of Ischiofemoral Impingement. The combination of passive extension, adducting and external rotation of the hip is used to provoke the symptoms[19].
The long stride walking test (walking with large steps) has a sensitivity of 92% and a specificity of 82% [20]
Hamstring tendinopathy[edit | edit source]
The insertion point of the Hamstring is on the Ischial Tuberosity, very close to the Sciatic Nerve. Proximal hamstring tendinopathy is common among distance runners and athletes performing sagittal plane (eg, sprinting, hurdling) or change-of-direction activities such as football and hockey drills [22]
Signs and Symptoms[5]:
- History of repetitive loading in flexion. During flexion movements such as deadlifts and other flexion activities the, proximal hamstring tendon undergoes tensile loading on the Ischial Tuberosity
- Deep, localised pain in the region of the ischial tuberosity
- Pain gets worse with sitting (described as sitting on a boggy mass), driving, picking up boxes and uphill running. This is due to the shear forces between the hamstring attachment and ischial tuberosity with increased hip flexion. During running, the peak force occurs in late swing, with a second peak reported in early stance.
- Positive straight leg raise
- Positive slump and neurodynamic test which indicates pressure on the Sciatic Nerve but doesn't rule out Hamstrings Tendinopathy
- Thickening on palpation around the Ischial Tuberosity lateral to the Ischium
Pain score should increase with load assessment tests[22]:
- Progression from the single-leg bent-knee bridge to the long-lever bridge to arabesque as follows:
Single Leg Long Lever Bridge:
- Single-leg deadlift
- Three passive stretch tests (bent-knee stretch, modified bent-knee stretch, and Puranen-Orava test) have moderate to high validity and high sensitivity and specificity for the diagnosis of PHT:
Examination[edit | edit source]
Lumbar spine pathology should be ruled out first. Physical examination includes palpation, pelvic girdle and Sacroiliac Joint tests Tests such as the March/Gillet test and the active straight leg raise test.
Patients with sciatic nerve entrapment are often presented with a history of previous trauma, pain with sitting, radicular leg pain and paresthesia[26]
A positive March test or active straight leg raise test, indicate poor motor control and failed load transfer, but neither differentiates the pathologic structure[5].
To rule out hip Osteoarthritis, the total arc of motion and FADIR tests are utilised. A negative FADIR can rule out intra-articular pathology, such as labral damage or osteoarthritis of the hip[5].
A positive FABER test provokes Sciatic Nerve symptoms where the nerve glides across the posterior border of the greater trochanter in that position [5]. Applying the same test, the pain felt on the greater trochanter could be due to Gluteal tendinopathy. If the patient felt the pain deep in the buttock it is more likely to be compression or irritation around the Piriformis muscle or some of the deep six.
Patients with Deep Gluteal Pain Syndrome can present with altered nerve conduction tests, changes in reflexes, motor weakness[30], and sensation changes which make it difficult in differentiating the lumbar spine from the buttock[5].
The combination of the seated piriformis stretch test with the piriformis active test has shown a sensitivity of 91% and specificity of 80% for the endoscopic finding of sciatic nerve entrapment[31]
Palpation skills can be useful in differentiating the site of pain and texture of soft tissue[5]. Using the ischial tuberosity as a reference while trying to reproduce the patient's pain with palpation to understand the probable source of symptoms [34]
Differential Diagnosis[edit | edit source]
The following table matches the deep gluteal pain conditions with their most likely symptoms[5]:
| Condition | Symptoms |
|---|---|
| Reactive hamstring tendon, bursitis | Uphill running
Deadlifts Picking up boxes / other loading flexion activity Feels like is sitting on a boggy mass |
| Non-discogenic Sciatic nerve entrapment | Radicular leg pain with hip flexion |
| Pudendal nerve entrapment | Increased time on the bike or change in saddle
Sitting on a toilet seat eases the pain |
| Ischiofemoral Impingement, lumbar facet pain, Sacroiliac Joint pain | Pain with hip extension or long strides |
| Ischiofemoral Impingement | History of trauma or hip surgery |
| Gluteal Tendinopathy, Obturator / Gemelli Tendinopathy | Limping after prolonged sitting |
Management[edit | edit source]
Principals:[edit | edit source]
- Differentiating the source of pain is recommended by using knowledge and assessment skills
- Educate your patient on the anatomy and causes of symptoms
- Address chronic pain factors using the biopsychosocial approach
- Advice load management
Hamstring tendinopathy:
- Avoid deadlifts and other flexion activities
- Avoid Hamstring stretches such as straightening the leg at 90 degrees of hip flexion
Sciatic Nerve involvement:
- When driving, move the car seat closer to the steering wheel to ease off that neural tension off the Sciatic Nerve
- For runners, advice them to reduce their stride length to relieve the symptoms
Pudendal Nerve type symptoms, you may need to refer the patient to a woman or men's health physiotherapist to assist you with the symptoms such as rectal pain, faecal incontinence or urinary incontinence. Refer female patients over 50 to the gynaecologist to assist their hormonal status. Lifestyle changes and weight management advice is also recommended
General Advice on the following:
- Weight management
- Lifestyle changes
- Sleep hygiene
- Risk factors such as smoking
Myofascial release, manual therapy in conjunction with the appropriate rehabilitation and advice are helpful clinical tools in the management of Deep Gluteal Pain[5].
Image-guided anaesthetic block or steroid injections might also be effective[7]
Surgical options are:
Partial lesser trochanteric plastics for Ischiofemoral Impingement
Arthroscopic or endoscopic releases of adhesions between Hamstring tendons or the Piriformis tendon and the Sciatic Nerve [36][12].
.
Exercises[edit | edit source]
Principals of exercise prescription[5]:
Try and limit the exercises to 15 or 20 minutes a day to improve your compliance and adherence.
Avoid stretching at the beginning of the treatment of tendinopathy to reduce the tensile loading on the tendon and possibly introduce them later when the pain settles.
When managing Tendinopathy, try to keep the pain below 5/10 and no worse at 24 hours afterwards especially with functional loading exercises such as the step-down, one-legged squat, a dynamic lunge, and a split squat.
When performing Piriformis stretch with the hip at 90 degrees, the hip needs to be in an externally rotated position. Piriformis is a hip abductor and external rotator below 45 to 60 degrees of hip flexion but functions as an internal rotator above 60 degrees of hip flexion
Combine exercises with neurodynamic gliding techniques, such as a Sciatic Nerve slider
Advise gluteal strengthening as bird-dog, split squats, and functional loading exercises
Progressive loading with emphasis on hip extensors, abductors and lateral rotators as a general rule
References[edit | edit source]
- ↑ McCrory P, Bell S (1999) Nerve entrapment syndromes as a cause of pain in the hip, groin and buttock. Sports Med 27(4):261–274
- ↑ Gonzalez-Lomas G. Deep gluteal pain in orthopaedics: a challenging diagnosis. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2021 Dec 15;29(24):e1282-90.
- ↑ 3.0 3.1 Hu YW, Ho GW, Tortland PD. Deep gluteal syndrome: a pain in the buttock. Current Sports Medicine Reports. 2021 Jun 1;20(6):279-85.
- ↑ Frank RM, Slabaugh MA, Grumet RC, Virkus WW, Bush-Joseph CA, Nho SJ (2010) Posterior hip pain in an athletic population: differential diagnosis and treatment options. Sports Health 2(3):237–246
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 Bell-Jenje T. Differentiating Buttock Pain (Part 3). Plus Course 2020
- ↑ Kizaki K, Uchida S, Shanmugaraj A, Aquino CC, Duong A, Simunovic N, Martin HD, Ayeni OR. Deep gluteal syndrome is defined as a non-discogenic sciatic nerve disorder with entrapment in the deep gluteal space: a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy. 2020 Apr 3:1-1.
- ↑ 7.0 7.1 Filler AG, Haynes J, Jordan SE, et al. Sciatica of nondisc origin and piriformis syndrome: diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment. J Neurosurg Spine 2005; 2: 99–115
- ↑ 8.0 8.1 Martin HD, Shears SA, Johnson JC, et al. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy 2011; 27: 172–81
- ↑ Meknas K, Christensen A, Johansen O (2003) The internal obturator muscle may cause sciatic pain. Pain 104(1–2):375–380
- ↑ Vicentini JR, Martinez-Salazar EL, Simeone FJ, Bredella MA, Palmer WE, Torriani M. Kinematic MRI of ischiofemoral impingement. Skeletal Radiology. 2020 Jul 7:1-0.
- ↑ Cox JM, Bakkum BW. Possible generators of retrotrochanteric gluteal and thigh pain: the gemelli-obturator internus complex. J Manipulative Physiol Ther 2005; 28: 534–8
- ↑ 12.0 12.1 Aguilera-Bohorquez B, Cardozo O, Brugiatti M, Cantor E, Valdivia N. Endoscopic treatment of sciatic nerve entrapment in deep gluteal syndrome: clinical results. Revista Española de Cirugía Ortopédica y Traumatología (English Edition). 2018 Sep 1;62(5):322-7.
- ↑ Martin R, Kivlan B, Martin HD. Greater Trochanter-Ischial Impingement: A Potential Source of Posterior Hip Pain. Rio de Janeiro: International Society for Hip Arthroscopy, 2014.
- ↑ Luesma MJ, Galé I, Fernando J. Diagnostic and therapeutic algorithm for pudendal nerve entrapment syndrome. Medicina Clínica (English Edition). 2021 Jul 23;157(2):71-8.
- ↑ Johnson KA. Impingement of the lesser trochanter on the ischial ramus after total hip arthroplasty. Report of three cases. J Bone Joint Surg Am 1977; 59: 268–9.
- ↑ Taneja AK, Bredella MA, Torriani M. Ischiofemoral impingement. Magn Reson Imaging Clin N Am 2013; 21: 65–73.
- ↑ Gollwitzer H, Banke IJ, Schauwecker J, Gerdesmeyer L, Suren C. How to address ischiofemoral impingement? Treatment algorithm and review of the literature. Journal of Hip Preservation Surgery. 2017 Dec;4(4):289-98.
- ↑ Wilson MD, Keene JS. Treatment of ischiofemoral impingement: results of diagnostic injections and arthroscopic resection of the lesser trochanter. J Hip Preserv Surg 2016; 3: 146–53
- ↑ Safran M, Ryu J. Ischiofemoral impingement of the hip: a novel approach to treatment. Knee Surg Sports Traumatol Arthrosc 2014; 22: 781–5.
- ↑ 4. Gomez-Hoyos J, Martin RL, Schroder R et al. Accuracy of 2 clinical tests for ischiofemoral impingement in patients with posterior hip pain and endoscopically confirmed diagnosis. Arthroscopy 2016; 32: 1279–84
- ↑ Posterior Hip Impingement Test Video Demonstration . Available from:https://www.youtube.com/watch?v=qobPzFnhRY0[last accessed 22/10/2020]
- ↑ 22.0 22.1 Goom TS, Malliaras P, Reiman MP, Purdam CR. Proximal hamstring tendinopathy: clinical aspects of assessment and management. Journal of orthopaedic & sports physical therapy. 2016 Jun;46(6):483-93.
- ↑ Active Isolated Stretching - Bent Knee Hamstring. Available from:https://www.youtube.com/watch?v=sgbhl1yU3cc[last accessed 22/10/2020]
- ↑ Modified Bent Knee Stretch Test. Available from:https://www.youtube.com/watch?v=5JhQpLt2YZ8[last accessed 22/10/2020]
- ↑ Active Puranen Orava Test (Active Standing Hamstrings Stretch Test) Available from:https://www.youtube.com/watch?v=7e4_MDlsU0w[last accessed 22/10/2020]
- ↑ Benson B, Schutzer SF. Posttraumatic Piriformis syndrome: diagnosis and results of operative treatment. J Bone Joint Surg Am 1999; 81: 941–9
- ↑ Proper Introduction and Gillet's Test on Diamond . Available from:https://www.youtube.com/watch?v=jxhR5iCpPz0[last accessed 22/10/2020]
- ↑ How to do the FADIR hip impingement test . Available from:https://www.youtube.com/watch?v=PqgPWRqmQ_A[last accessed 22/10/2020]
- ↑ Ortho EVAL Pal With Paul Marquis PT. FABER/Patrick/Figure 4 Test-How to Perform it and What it Means! 2021 . Available from:https://www.youtube.com/watch?v=RMgaRoBg0do[last accessed 26/10/2022]
- ↑ Papadopoulos EC, Khan SN. Piriformis syndrome and low back pain: a new classification and review of the literature. Orthop Clin North Am 2004; 35: 65–71
- ↑ Martin HD, Kivlan BR, Palmer IJ, et al. Diagnostic accuracy of clinical tests for sciatic nerve entrapment in the gluteal region. Knee Surg Sports Traumatol Arthrosc 2014; 22: 882–8.
- ↑ Piriformis stretch. Available from:https://www.youtube.com/watch?v=JR1rtQ-PF38[last accessed 22/10/2020]
- ↑ Piriformis stretch. Available from:https://www.youtube.com/watch?v=iL19XaxMmP4[last accessed 22/10/2020]
- ↑ Martin HD, Reddy M, Gómez-Hoyos J. Deep gluteal syndrome. Journal of hip preservation surgery. 2015 Jul 1;2(2):99-107.
- ↑ Physical Examination of the Hip - Hal D. Martin D.O.. Available from:https://www.youtube.com/watch?v=IhvVoKGyl8E[last accessed 22/10/2020]
- ↑ Kay J, Morrison L, Fejtek E, Simunovic N, Martin HD, Ayeni OR. Surgical management of deep gluteal syndrome causing sciatic nerve entrapment: a systematic review. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2017 Dec 1;33(12):2263-78.