|
|
| (33 intermediate revisions by 9 users not shown) |
| Line 2: |
Line 2: |
| '''Original Editors ''' - [[User:Jessica Stevenson|Jessica Stevenson]] from [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | | '''Original Editors ''' - [[User:Jessica Stevenson|Jessica Stevenson]] from [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project.]] |
|
| |
|
| '''Lead Editors''' - Your name will be added here if you are a lead editor on this page. [[Physiopedia:Editors|Read more.]] | | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} |
| </div> | | </div> |
| == Definition/Description <br> == | | == Introduction == |
| | [[File:Cushing's syndrome diag.png|thumb|Cushing's syndrome]] |
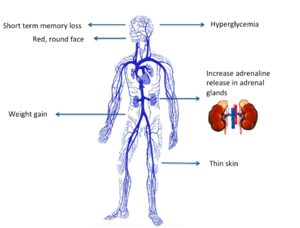
| | Cushing’s syndrome is a general term for increased secretion of cortisol by the [[Adrenal Glands|adrenal]] cortex. |
|
| |
|
| Cushing’s syndrome is a general term for increased secretion of cortisol by the adrenal cortex. When corticosteroids are administered externally, a condition of hypercortisolism called iatrogenic Cushing’s syndrome occurs. <ref name="DD">Goodman CC, Snyder KS. Differential Diagnosis for Physical Therapists: Screening for Referral. Philadelphia : W.B. Saunders Company; 2006: 473-475</ref> When the hypercortisolism results from an oversecretion of ACTH from the pituitary, the condition is called Cushing’s disease. The clinical presentation is the same for all of these conditions. <ref name="Path">Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist 3rd ed. St. Louis: Saunders Elsevier; 2009: 481-483.</ref><br>
| | # When [[Corticosteroid Medication|corticosteroids]] are administered externally, a condition of hypercortisolism called iatrogenic Cushing’s syndrome occurs. |
| | # When the hypercortisolism results from an oversecretion of Adrenocorticotropic hormone (ACTH) from the pituitary, the condition is called Cushing’s disease. |
|
| |
|
| *ACTH: Adrenocorticotropic hormone<br>
| | The clinical presentation is the same for all of these conditions.<ref name="DD">Goodman CC, Snyder KS. Differential Diagnosis for Physical Therapists: Screening for Referral. Philadelphia : W.B. Saunders Company; 2006: 473-475</ref> <ref name="Path">Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist 3rd ed. St. Louis: Saunders Elsevier; 2009: 481-483.</ref> |
| | == Epidemiology == |
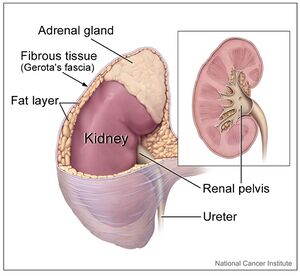
| | [[File:Kidney and adrenal gland.jpeg|right|frameless]] |
| | The actual incidence and prevalence of Cushing syndrome are not known. The prevalence of the disease is highly variable across different ethnic and cultural groups depending upon the frequency and spectrum of the medical conditions requiring steroid-based therapy. |
|
| |
|
| == Prevalence<br> == | | # Of the known cases, iatrogenic hypercortisolism outweighs the endogenous causes, |
| | # Of the endogenous causes, pituitary-mediated ACTH production accounts for up to 80% of cases of hypercortisolism, followed by adrenals, unknown source, and ectopic ACTH production secondary to malignancies<ref name=":0">Chaudhry HS, Singh G. Cushing syndrome. InStatPearls [Internet] 2021 Jul 30. StatPearls Publishing. Available:https://www.ncbi.nlm.nih.gov/books/NBK470218/ (accessed 12.5.2022)</ref> |
|
| |
|
| By far, the single most common cause of Cushing's syndrome today (as many as 12 cases/1 million people) is the use of corticosteroid medications to treat a wide variety of disease states, including rheumatoid arthritis, asthma, and multiple sclerosis. The prevelance of hypercotisolism from all other causes combined is only 13 cases per 1 million people nationally. The overall incidence is estimated as 2 new cases per 1 million persons per year. <ref name="CS 52">Harold J Bruyere: 100 Case Studies in Pathophysiology. Lippincott Williams &amp;amp;amp;amp;amp;amp; Wilkins; October 2008: Case Study 52.</ref>
| | == Etiology == |
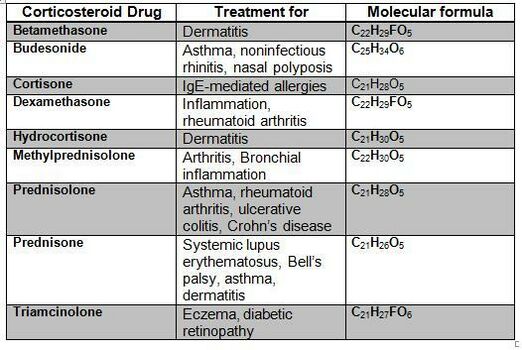
| | [[File:Corticosteroid.jpg|thumb|522x522px|Corticosteroid Medications]] |
| | There are two main etiologies of Cushing syndrome: |
|
| |
|
| Females are eight times more likely than males to develop hypercortisolism from a pituitary tumor and three times more likely to develop a cortisol-secreting adrenal tumor: However, hormone-producing lung tumors that cause hypercortisolism are more common in males. <ref name="CS 52" />
| | # Endogenous hypercortisolism: results from excessive production of cortisol by adrenal glands and can be ACTH-dependent and ACTH-independent. ACTH-secreting pituitary adenomas (Cushing disease) and ectopic ACTH secretion by neoplasms are responsible for ACTH-dependent Cushing. Adrenal hyperplasia, adenoma, and carcinoma are major causes of ACTH-independent Cushing syndrome. |
| | | # Exogenous hypercortisolism: the most common cause of Cushing syndrome, mostly iatrogenic and results from the prolonged use of [[Corticosteroid Medication|glucocorticoids]]<ref name=":0" />. |
| Ninety percent of all cases of Cushing's syndome occur during adulthood. The incidence of Cushing's syndrome in children is estimated at approximately 0.2 cases per 1 million persons per year: The peak incidence of Cushing's syndrome due to an adrenal or pituitary tumor occurs in persons 25-40 years of age. <ref name="CS 52" />
| |
| | |
| Non-iatrogenic Cushing’s syndrome occurs mainly in women, with an average age of onset of 20 to 40 years, although it can be seen in people up to age 60 years. <ref name="Path" />
| |
|
| |
|
| == Characteristics/Clinical Presentation == | | == Characteristics/Clinical Presentation == |
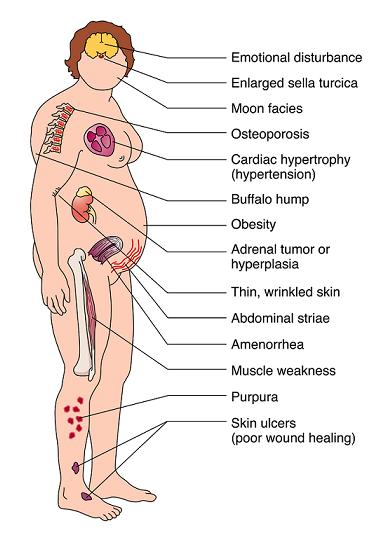
| | [[File:Cushings-syndrome2.jpg|alt=|right]] |
|
| |
|
| Clinical manifestations include “moon” face (very round), buffalo hump (truncal obesity with prominent supraclavicular and dorsal cervical fat pads) <ref name="Merck">Beers MH, Porter RS, Jones TV, Kaplan JL, Berkwits M. The Merck Manual of Diagnosis and Therapy 18th ed. Whitehouse Station:Merck Research Laboratories; 2006: 1212-1214.</ref>, protuberant abdomen with accumulation of fatty tissue and stretch marks with purple striae, muscle wasting and weakness, thin extremities, decreased bone density (especially spine), kyphosis and back pain (secondary to bone loss), easy bruising and poor wound healing due to thin and atrophic skin <ref name="Merck" />, acne, psychiatric or emotional disturbances, impaired reproductive function (decreased libido and changes in menstrual cycle, and diabetes mellitus. In women, masculinizing effects such as hypertrichosis, breast atrophy, voice changes, and other signs of virilism are noted. Cessation of linear growth is characteristic in children. <ref name="DD" /> <ref name="Merck" /> | | Clinical manifestations include: |
| | |
| [[Image:Moon facies in Cushings.jpg|Image:Moon_facies_in_Cushings.jpg]] [[Image:Cushings-syndrome2.jpg]]
| |
| | |
| == Associated Co-morbidities ==
| |
| | |
| Cushing’s syndrome involves the HPA axis causing excess cortisol release from the adrenal glands. When the normal function of the glucocorticoids becomes exaggerated, a wide range of physiologic responses can be triggered. <ref name="Path" />
| |
| | |
| Co-morbidities involved with Cushing’s disease are persistent hyperglycemia, cardiac hypertrophy and hypertension, proximal muscle wasting (protein tissue wasting), osteopenia or osteoporosis, hypokalemia, mental changes and memory loss, depression, renal calculi, increased susceptibility to infection, adrenal hyperplasia and adrenal tumors <ref name="Path" /> <ref name="Merck" /> <ref name="DD" /><br><br>
| |
| | |
| == Medications ==
| |
| | |
| Initially, the patient’s general condition should be supported by high protein intake and appropriate administration of vitamin K. If clinical manifestations are severe, it may be reasonable to block corticosteroid secretion with metyrapone 250 mg to 1 g pot id or ketoconazole 400 mg po once/day, increasing to a maximum of 400 tid. Ketoconazole is more readily available but slower in onset and sometimes hepatatoxic. <ref name="Merck" />
| |
| | |
| Adrenal inhibitors, such as metyrapone 500 mg pot id (and up to a total of 6 g/day) or mitotane 0.5 g po once/day, increasing to a maximum of 3 to 4 g/day, usually control severe metabolic disturbances (eg. Hypokalemia). When mitotane is used, large doses of hydrocortisone or dexamethasone may be needed. Measures of cortisol production may be unreliable, and severe hypercholesterolemia may develop. Ketoconazole 400 to 1200 mg po once/day also blocks corticosteroid synthesis, although it may cause liver toxicity and can cause addisonian symptoms. Alternatively, the corticosteroid receptors can be blocked with mifepristone (RU 486). Mifepristone increases plasma cortisol but blocks effects of the corticosteroid. Sometimes ACTH-secreting tumors respond to long-acting somatostatin analogs, although administration for > 2 years requires close follow-up, because mild gastritis, gall stones, cholangitis, and malabsorption may develop. <ref name="Merck" /><br><br>
| |
| | |
| == Diagnostic Tests/Lab Tests/Lab Values ==
| |
| | |
| Although there is a classic cushingoid appearance in persons with hypercortisolism and diagnosis is usually suspected based on the characteristic symptoms and signs, diagnostic laboratory studies, including hormonal and imaging tests, are used to confirm the diagnosis. <ref name="Path" /> <ref name="Merck" /> Also, reviewing the history of receiving corticosteroids is important.<br>In some centers, testing begins with measurement of urinary free cortisol (UFC), the best assay for urinary excretion. UFC is elevated > 120 µg/24h (>331 nmol/24h) in almost all patients with Cushing’s syndrome. However, many patients with UFC elevations between 100 and 150 µg/24h (276 and 414 nmol/24h) have obesity, depression, or polycystic ovaries but not Cushing’s syndrome. A patient with suspected Cushing’s syndrome with grossly elevated UFC (> 4 times the upper limit of normal) almost certainly has Cushing’s syndrome. Two to three normal collections virtually exclude the diagnosis. Slightly elevated levels generally necessitate further investigation. <ref name="Merck" />
| |
| | |
| If the initial laboratory tests are positive (elevated cortisol levels), then a dexamethasone suppression test may be done to determine the cause. <ref name="Path" /> An amount of 1, 1.5, or 2 mg of dexamethasone is administered po at 11 to 12 PM and plasma cortisol is measured at 8 to 9 AM the next morning. In most normal patients, this drug suppresses morning plasma cortisol to ≤ 1.8 µg/mL (≤ 50 nmol/L), whereas patients with Cushing’s syndrome virtually always have a higher level. A more specific but equally sensitive test is to give dexamethasone 0.5 mg po q 6 h for 2 days (low dose). In general, a clear failure to suppress levels in response to low-dose dexamethasone establishes the diagnosis. <ref name="Merck" />
| |
| | |
| If the results of these tests are indeterminate, the patient is hospitalized for measurement of serum cortisol at midnight, which is more likely to be conclusive. Cortisol normally ranges from 5 to 25 µg/dL (138 to 690 nmol/L) in the early morning (6 to 8 AM) and declines gradually to < 1.8 µg/dL (< 50 nmol/L) at midnight. Patients with Cushing’s syndrome occasionally have a normal morning cortisol level but lack normal diurnal decline in cortisol production, such that midnight plasma cortisol levels are above normal and the total 24-hr cortisol production is elevated. Alternatively, salivary cortisol samples may be collected and stored in the refrigerator at home. Plasma cortisol may be spuriously elevated in patients with congenital increases of corticosteroid-binding globulinor in those receiving estrogen therapy, but diurnal variation is normal in these patients. <ref name="Merck" />
| |
| | |
| Serum ACTH levels help determine whether Cushing’s syndrome is ACTH-dependent (pituitary tumor) or ACTH-independent (adrenal tumor). <ref name="Path" /> Undetectable levels, both basally and particularly in response to corticotrophin-releasing hormone (CRH), suggest a primary adrenal cause. High levels suggest a pituitary cause. If ACTH is detectable (ACTH-dependent Cushing’s syndrome), provocative tests help differentiate Cushing’s disease from ectopic ACTH syndrome, which is rarer. In response to high-dose dexamethasone (2 mg po q 6 h for 48 h), the 9 AM serum cortisol falls by > 50% in most patients with Cushing’s disease but infrequently in those with ectopic ACTH syndrome. Conversely, ACTH and cortisol rise by >50% and 20%, respectively, in response to human or ovine-sequence CRH ( 100 µg IV or 1 µg/kg IV) in most patients with Cushing’s disease but very rarely in those with ectopic ACTH syndrome. An alternative approach to localization, which is more accurate but more invasive, is to catheterize both petrosal veins (which drains the pituitary) and measure ACTH from these veins 5 min after a bolus of CRH 100 µg or 1 µg/kg. A central-to-peripheral ACTH ratio >3 virtually excludes ectopic ACTH syndrome, whereas a ratio <3 suggests a need to seek such a source. <ref name="Merck" />
| |
| | |
| Pituitary imaging is done if ACTH levels and provocative tests suggest a pituitary cause; gadolinium-enhanced MRI is most accurate, but some microadenomas are visible on CT. If testing suggests a nonpituitary cause, imaging includes high-resolution CT of the chest, pancreas, and adrenals; scintiscanning with radiolabeled octreotide; and PET scanning. <ref name="Merck" />
| |
| | |
| X-rays or DEXA scans may be needed to assess for fractures or to rule out osteopenia or osteoporosis, respectively. These tests may be conducted to obtain a baseline measurement of bone density or they may be obtained in response to an individual’s report of musculoskeletal symptoms such as bone pain or backache. <ref name="Path" />
| |
| | |
| In children with Cushing’s disease, pituitary tumors are very small and usually cannot be detected with MRI. Petrosal sinus sampling is particularly useful in this situation. MRI is preferred to CT in pregnant women to avoid fetal exposure to radiation. <ref name="Merck" /><br><br>
| |
| | |
| == Causes ==
| |
| | |
| The primary causes of Cushing’s syndrome are hyperphysiologic doses of adrenocorticosteroids and adrenocortical tumors. <ref name="Path" /> Hyperfunction of the adrenal cortex can be ACTH-dependent or ACTH independent. <ref name="Merck" />
| |
| | |
| ACTH-dependent Cushing’s syndrome may result from hypersecretion of ACTH by the pituitary gland, secretion of ACTH by a nonpituitary tumor, such as small cell carcinoma of the lung or a carcinoid tumor (ectopic ACTH syndrome), or administration of exogenous ACTH. <ref name="Merck" />
| |
| | |
| ACTH-independent Cushing’s syndrome usually results from therapeutic administration of corticosteroids or from adrenal adenomas or carcinomas. Rare causes include primary pigmented nodular adrenal dysplasia (usually in adolescents) and macronodular dysplasia (in older patients). <ref name="Merck" />
| |
| | |
| Pseudo-Cushing’s syndrome occurs when conditions such as depression, alcoholism, estrogen therapy, or eating disorders cause changes similar to those of Cushing’s syndrome. In pseudo-Cushing’s syndrome, the symptoms will go away when the cause is eliminated. <ref name="Path" /><br>
| |
| | |
| == Systemic Involvement ==
| |
| | |
| Cushing’s syndrome involves the HPA axis causing excess cortisol release from the adrenal glands. Cortisol has a key role in glucose metabolism and a lesser part in protein, carbohydrate, and fat metabolism. Cortisol also helps maintain blood pressure and cardiovascular function while reducing the body’s inflammatory responses. Overproduction of cortisol causes liberation of amino acids from muscle tissue with resultant weakning of protein structures (specifically muscle and elastic tissue). The end result may include a protuberant abdomen with purple striae, poor wound healing, thinning of skin, generalized muscle weakness, and marked osteoporosis that is made worse by an excessive loss of calcium in the urine. <ref name="Path" /> <ref name="DD" /> In severe cases of prolonged Cushing’s syndrome, muscle weakness and demineralization of bone may lead to pathological fractures and wedging of the vertebrae, kyphosis, osteonecrosis (especially in femoral head), bone pain, and back pain. <ref name="Path" />
| |
| | |
| The effect of circulating levels of cortisol on the muscles varies from slight to marked. Muscle wasting can be so extensive that the condition simulates muscular dystrophy. Marked weakness of the quadriceps muscle often prevents affected people from rising out of a chair unassisted. <ref name="Path" /> <ref name="DD" />
| |
| | |
| It is important to remember whenever corticosteroids are administered, the increase in serum cortisol levels triggers a negative feedback signal to the anterior pituitary gland to stop its secretion of ACTH. <ref name="DD" /> This decrease in ACTH stimulation of the adrenal cortex results in adrenocortical atrophy during the period of exogenous corticosteroid administration. If these medications are stopped suddenly rather than reduced gradually, the atrophied adrenal gland will not be able to provide the cortisol necessary for physiologic needs. A life-threatening situation known as acute adrenal insufficiency can develop, requiring emergency cortisol replacement. <ref name="Path" />
| |
| | |
| == Medical Management (current best evidence) ==
| |
| | |
| Treatment to restore hormone balance and reverse Cushing’s syndrome or disease may require radiation, drug therapy, or surgery, depending on underlying cause (e.g. resection of tumors). For individuals with muscle wasting or at risk for muscle atrophy, a high-protein diet may be prescribed. Prognosis depends on the underlying cause and ability to control the cortisol excess. Cortisol-secreting tumors can recur, thus follow-up screening is advised. <ref name="Path" />
| |
| | |
| Pituitary tumors that produce excessive ACTH are removed surgical or extirpated with radiation. If no tumor is demonstrated on imaging but a pituitary source is likely, total hypophysectomy may be attempted, particularly in older patients. Younger patients usually receive supervoltage irradiation of the pituitary, delivering 45 Gy. Improvement usually occurs in <1 yr. However, in children, irradiation may reduce secretion of growth hormone and occasionally cause precocious puberty. In special centers, heavy particle beam irradiation, providing about 100 Gy, is often successful, as is a single focused beam of radiation therapy given as a single dose-radiosurgery. Response to irradiation occasionally requires several years, but response is more rapid in children. <ref name="Merck" />
| |
| | |
| Bilateral adrenalectomy is reserved for patients with pituitary hyperadrenocorticism who do not respond to both pituitary exploration (with possible adenomectomy) and irradiation. Adrenalectomy requires life-long corticosteroid replacement. <ref name="Merck" />
| |
| | |
| Adrenocortical tumors are removed surgically. Patients must receive cortisol during the surgical and postoperative periods because their nontumorous adrenal cortex will be atrophic and suppressed. Benign adenomas can be removed laparoscopically. With multinodular adrenal hyperplasia, bilateral adrenalectomy may be necessary. Even after a presumed total adrenalectomy, functional regrowth occurs in few patients. <ref name="Merck" />
| |
| | |
| == Physical Therapy Management (current best evidence) ==
| |
| | |
| Therapists are more likely to treat people who have developed medication-induced Cushing’s syndrome. This condition occurs after these individuals have received a large dose of cortisol (also known as hydrocortisone) or cortisol derivitives. Exogenous steroids are administered for a number of inflammatory and other disorders such as asthma or rheumatoid arthritis. <ref name="DD" />
| |
| | |
| *Because cortisol suppresses the inflammatory response of the body, it can mask early signs of infection. Any unexplained fever without other symptoms should be a warning to the physical therapist of the need for medical follow-up. <ref name="DD" />
| |
| *Consult MD before beginning any exercise program. <ref name="yahoo">Caroline Rea. Cushing's Syndrome. YahooHealth. last updated 4/29/2008. http://health.yahoo.com/hormone-living/cushing-s-syndrome-home-treatment/healthwise--hw71687.html</ref>
| |
| | |
| Get regular exercise to help maintain muscles and bone mass and prevent weight gain. To maintain muscle and bone mass, weight-bearing exercises such as push-ups, sit-ups, or lifting weights are helpful. To prevent weight gain, aerobic exercise is good to increase your heart rate. Examples of aerobic exercise include fast walking, jogging, cycling, and swimming. <ref name="yahoo" />
| |
| | |
| Education on avoiding falls and removing loose rugs and other hazards in the home. Falling may lead to broken bones and other injuries. <ref name="yahoo" />
| |
| | |
| Pay close attention to all wounds. Too much cortisol slows wound healing. Education on proper wound healing and cleansing is important. Clean all wounds immediately with antibacterial soap and use antibiotic ointment and dressings to prevent infection. <ref name="yahoo" />
| |
| | |
| == Alternative/Holistic Management (current best evidence) ==
| |
| | |
| Although there is not much research behind the effectiveness of these interventions, they can improve quality of life. <ref name="Support">Cushing's Syndrome Support Group. http://www.cushings-help.com/cushing-causes.htm</ref>
| |
| | |
| '''Acupuncture'' ''Aromatherapy''
| |
| | |
| ''Ayurveda'' ''Bioenergetics''
| |
| | |
| ''Biofeedback''' '''Bodywork''
| |
| | |
| ''Breathwork''' '''Craniosacral therapy''
| |
| | |
| ''Dance therapy''' '''Feng shui''
| |
| | |
| ''Holistic medicine''' '''Humortherapy''
| |
| | |
| ''Hypnosis Imagery''
| |
| | |
| ''Labyrinth walking Massage''
| |
| | |
| ''Meditation Music therapy''
| |
| | |
| ''Naturopathic medicine Neuro-linguistic programming''
| |
| | |
| ''Polarity therapy Psychotherapy''
| |
| | |
| ''Qigong Reflexology (zone therapy)''
| |
| | |
| ''Reiki Shamanism''
| |
| | |
| ''Spirituality and prayer Support groups''
| |
| | |
| ''Tai Chi '' ''Therapeutic Touch (energy field therapy, biofield therapy)''
| |
| | |
| ''Yoga (hatha yoga) ''<br>
| |
| | |
| == Differential Diagnosis ==
| |
| | |
| Differential diagnoses for Cushing’s syndrome are obesity, diabetes, polycystic ovarian syndrome, other metabolic and endocrine problems. <ref name="DD" />
| |
| | |
| Differentiation of Cushing syndrome from pseudo–Cushing syndrome can sometimes be a challenge. A pseudo-Cushing state is defined as having some of the clinical features and biochemical evidence of Cushing syndrome. However, resolution of the primary condition results in disappearance of the cushingoid features and biochemical abnormalities. <ref name="emedicine">Gail K Adler, MD, PhD, FAHA, Assistant Professor, Department of Medicine, Division of Endocrinology, Diabetes and Hypertension, Brigham and Women's Hospital, Harvard Medical School Cushing Syndrome: Differential Diagnoses &amp;amp;amp;amp;amp;amp; Workup Updated: Oct 1, 2009</ref>
| |
| | |
| In patients who chronically abuse alcohol, clinical and biochemical findings suggestive of Cushing syndrome are often encountered. Discontinuation of alcohol causes disappearance of these abnormalities, and, therefore, this syndrome is often specifically referred to as alcohol-induced pseudo-Cushing syndrome. <ref name="emedicine" />
| |
| | |
| Patients with depression often have perturbation of the HPA axis, with abnormal cortisol hypersecretion. These patients rarely develop clinical Cushing syndrome. Because excess glucocorticoids can lead to emotional liability and depression, distinguishing between depression and mild Cushing syndrome is often a diagnostic challenge. <ref name="emedicine" />
| |
| | |
| == Case Reports ==
| |
| | |
| Click on links below to view case studies of patient's with Cushing's syndrome:
| |
| | |
| [http://www.endocrinology.org/education/resource/EndocrineNurseCourse/ent03/ent03_kie.htm http://www.endocrinology.org/education/resource/EndocrineNurseCourse/ent03/ent03_kie.htm] <ref name="CS 1">N Kieffer. Leicester Royal Infirmary, UHL NHS Trust Endocrine Nurses Training Course 10-12 September 2003: St Aidan's College, University of Durham, Windmill Hill, Durham DH1 3LJ</ref>
| |
| | |
| http://path.upmc.edu/cases/case144.html <ref name="CS 2">Sanja Dacic, MD and Prabha B. Rajan, MD Endocrine Pathology Case Study. Published on-line in April 1998</ref>
| |
| | |
| http://www.medscape.com/viewarticle/547281 <ref name="CS 3">Ashley B Grossman; Philip Kelly; Andrea Rockall; Satya Bhattacharya; Ann McNicol; Tara Balwick[Case Study]: Cushing's Syndrome Caused by an Occult Source: Difficulties in Diagnosis and ManagementPosted: 11/21/2006; Nat Clin Pract Endocrinol Metab. 2006;2(11):642-647. © 2006 Nature Publishing Group</ref>
| |
| | |
| http://www.nature.com/nrendo/journal/v3/n11/full/ncpendmet0665.html <ref name="CS 4">P Gerry Fegan, Derek D Sandeman, Nils Krone, Deborah Bosman, Peter J Wood, Paul M Stewart and Neil A Hanley. Cushing's syndrome in women with polycystic ovaries and hyperandrogenism. J Endocrinol Invest. 2004 Apr;27(4):375-9.</ref>
| |
| | |
| [http://www.ncbi.nlm.nih.gov/pubmed/15233560 http://www.ncbi.nlm.nih.gov/pubmed/15233560] <ref name="CS 5">Tung SC, Wang PW, Huang TL, Lee WC, Chen WJ. Bilateral adrenocortical adenomas causing ACTH-independent Cushing's syndrome at different periods: a case report and discussion of corticosteroid replacement therapy following bilateral adrenalectomy. Department of Internal Medicine, Division of Endocrinology and Metabolism, Kaohsiung Chang Gung Memorial Hospital, Taiwan. [email protected]</ref> | |
| | |
| == Resources <br> ==
| |
| | |
| <u>'''TEXTBOOKS'''</u>
| |
| | |
| 100 Case Studies in Pathophysiology.
| |
|
| |
|
| Differential Diagnosis for Physical Therapists: Screening for Referral.
| | * “moon” face (very round), |
| | * buffalo hump (truncal obesity with prominent supraclavicular and dorsal cervical fat pads) <ref name="Merck">Beers MH, Porter RS, Jones TV, Kaplan JL, Berkwits M. The Merck Manual of Diagnosis and Therapy 18th ed. Whitehouse Station:Merck Research Laboratories; 2006: 1212-1214.</ref>, |
| | * protuberant abdomen with accumulation of fatty tissue and stretch marks with purple striae, |
| | * muscle wasting and weakness, |
| | * thin extremities, |
| | * decreased bone density (especially spine), |
| | * [[kyphosis]] and back pain (secondary to bone loss), |
| | * easy bruising and poor wound healing due to thin and atrophic skin <ref name="Merck" />, |
| | * acne, |
| | * psychiatric or emotional disturbances, |
| | * impaired reproductive function (decreased libido and changes in menstrual cycle, and |
| | * diabetes mellitus. |
|
| |
|
| The Merck Manual of Diagnosis and Therapy 18th edition.
| | In women, masculinizing effects such as hypertrichosis, breast atrophy, voice changes, and other signs of virilism are noted. Cessation of linear growth is characteristic in children. <ref name="DD" /> <ref name="Merck" /> |
| | == Complications == |
|
| |
|
| Pathology: Implications for Physical Therapists 3rd edition.
| | Complications include: |
|
| |
|
| <br> | | * Excess hair growth |
| | * [[Osteoporosis]] |
| | * Susceptibility to infections |
| | * [[Diabetes Mellitus Type 2|Type 2 diabetes]] |
| | * Peptic ulcer disease |
| | * [[Hypertension]]<ref name=":0" /> |
|
| |
|
| <u>'''INTERNET RESOURCES'''</u>
| | == Diagnosis == |
| | Taking glucocorticoid medications is the most common cause of Cushing syndrome. If this is the case other tests are not needed. Cushing syndrome from endogenous cortisol production can be difficult to diagnose because other conditions have similar signs and symptoms. Diagnosing Cushing syndrome can be a long and extensive process. The below tests can help find the cause: |
|
| |
|
| Cushing's Syndrome Support Website ([http://www.cushings-help.com/cushing-causes.htm http://www.cushings-help.com/cushing-causes.htm])
| | * [[Urine]] and [[Blood Tests|blood tests]]: measure [[Hormones|hormone]] levels and show whether person is producing excessive cortisol. The doctor might also recommend other specialized tests that involve measuring cortisol levels before and after using hormone medications to stimulate or suppress cortisol. |
| | * Saliva test. Cortisol levels normally rise and fall throughout the day. In people without Cushing syndrome, levels of cortisol drop significantly in the evening. By analyzing cortisol levels from a small sample of saliva collected late at night, doctors can see if cortisol levels are too high. |
| | * Imaging tests. CT or MRI scans can provide images of the pituitary and adrenal glands to detect abnormalities, eg tumors. |
| | * Petrosal sinus sampling. This test can help determine whether the cause of Cushing syndrome is rooted in the pituitary or somewhere else. For the test, blood samples are taken from the veins that drain the pituitary gland (petrosal sinuses). |
|
| |
|
| E-medicine ([http://emedicine.medscape.com/ http://emedicine.medscape.com/])
| | == Management == |
| | Treatments for Cushing syndrome are designed to lower the high level of cortisol in the body. The best treatment for you depends on the cause of the syndrome. Options include: |
|
| |
|
| Endocrine Pathology case study (http://path.upmc.edu/cases/case144.html)
| | * The best therapy for iatrogenic Cushing syndrome is to taper exogenous steroids'''.''' Chronic exposure to steroids potentially suppresses the function of the adrenal and it can take several months for normal adrenal functioning to recover. Steroids should be slowly tapered allowing adrenal functioning to recover. |
| | * Hypercortisolism due to Cushing disease or adrenal tumor or ectopic tumor is treated with surgical resection. After the operation, cortisol replacement medications are needed to provide the body with the correct amount of cortisol. In most cases eventually normal adrenal hormone production returns. If the surgeon can not totally remove a pituitary tumor, [[Radiation Side Effects and Syndromes|radiation]] therapy as well as surgery will be needed. Additionally, radiation may be used for people who aren't suitable candidates for surgery<ref name=":0" />.<ref>Mayo clinic Cushing Syndrome Available:https://www.mayoclinic.org/diseases-conditions/cushing-syndrome/diagnosis-treatment/drc-20351314 (accessed 13.5.2022)</ref> |
| | * Medications can be used to control cortisol production when surgery and radiation don't work. Medical therapy may not completely improve all of the symptoms of excess cortisol. Medications to control excessive production of cortisol at the adrenal gland include ketoconazole, mitotane (Lysodren) and metyrapone (Metopirone). |
|
| |
|
| Medscape Today from WebMD ([http://www.medscape.com/medscapetoday http://www.medscape.com/medscapetoday])
| | In the management of Cushing syndrome, it is crucial to treat comorbidities such as [[Diabetes Mellitus Type 1|diabetes mellitus]], [[hypertension]], [[osteoporosis]], psychiatric issues, and electrolyte disorders.<ref name=":0" /> |
| | == Physical Therapy Management == |
|
| |
|
| PubMed ([http://www.ncbi.nlm.nih.gov/pubmed http://www.ncbi.nlm.nih.gov/pubmed])
| | Therapists are more likely to treat people who have developed medication-induced Cushing’s syndrome. Exogenous [[Corticosteroid Medication|steroids]] are administered for a number of inflammatory and other disorders eg [[asthma]] or [[Rheumatoid Arthritis|rheumatoid arthritis]]. <ref name="DD" /> |
|
| |
|
| Society for Endocrinology ([http://www.endocrinology.org/ http://www.endocrinology.org/])
| | Educate Clients with regard to: |
|
| |
|
| U.S. National Library of Medicine. National Institute of Health. NCBI ([http://www.nlm.nih.gov/ http://www.nlm.nih.gov/])<br>
| | * Getting regular [[Therapeutic Exercise|exercise]] to help maintain muscles and bone mass and prevent weight gain. To maintain muscle and bone mass, weight-bearing exercises eg [[Pushups|push-ups]], [[Curl-ups|sit-ups]], or lifting weights are helpful. To prevent weight gain, [[Aerobic Exercise|aerobic]] exercise are good. eg fast [[Walking - Muscles Used|walking]], jogging, cycling, and [[Swimming: Freestyle|swimming]]. <ref name="yahoo">Caroline Rea. Cushing's Syndrome. YahooHealth. last updated 4/29/2008. http://health.yahoo.com/hormone-living/cushing-s-syndrome-home-treatment/healthwise--hw71687.html</ref> |
| | * Education on avoiding [[falls]] and removing loose rugs and other hazards in the home. Falling may lead to broken bones and other injuries. <ref name="yahoo" /> |
| | * Pay close attention to all [[Wound Debridement|wounds]]. Too much cortisol slows wound healing. Education on proper wound healing and cleansing is important. Clean all wounds immediately with antibacterial soap and use antibiotic ointment and dressings to prevent infection. <ref name="yahoo" /> |
|
| |
|
| == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/PubMed/ Pubmed]) ==
| |
| <div class="researchbox"><rss>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1BsDMEWA_ZX6DiqehwRMq5vFl03UpgVpZwNHMhgLc-a95ah5iq|charset=UTF-8|short|max=15</rss></div>
| |
| == References == | | == References == |
|
| |
|
| <references /> | | <references /> |
|
| |
|
| [[Category:Bellarmine_Student_Project]] [[Category:Articles]] [[Category:Condition]] | | [[Category:Bellarmine_Student_Project]] |
| | [[Category:Conditions]] |
| | [[Category:Metabolic/Endocrine]] |